Abstract
A negative wealth shock (i.e., a sudden large loss in wealth) represents a stressful life event that threatens older adults' mental health. This study examines whether a negative wealth shock is associated with both 12-month major depressive episodes and 1-week depressive symptoms over time among older adults, compared to positive wealth without a shock. This study also examines whether baseline net worth moderates the association between a negative wealth shock and depressive symptoms. The study utilized a national sample of 15,660 individuals from six waves of the Health and Retirement Study (2008–2018). We estimated mixed-effects models based on respondents’ self-reported wealth and depressive symptoms. A negative wealth shock was defined as a loss of 75 % in total wealth compared to the previous wave. We applied inverse probability weighting to account for potential selection bias. A negative wealth shock was associated with 1.30 times higher odds of having major depressive episodes compared to positive wealth. Both a negative wealth shock (incidence rate ratio [IRR] = 1.30, 95 % Confidence Interval [CI]: 1.06–1.60) and baseline negative wealth (IRR = 1.05, 95 % CI: 1.01–1.09) were associated with a higher rate of depressive symptoms compared to positive wealth. No interaction effects between baseline net worth and a negative wealth shock on depressive symptoms were observed. A negative wealth shock in mid-to-late life has detrimental effects on both 12-month and past-week depressive symptoms, providing implications for mental health programs for older adults at financial risk.
Keywords: Depression, Wealth, Socioeconomic status, Mental health, Older adults
Highlights
-
•
A negative wealth shock is associated with both 12-month major depressive episodes and past-week depressive symptoms.
-
•
Zero/negative wealth at baseline is linked to past-week depressive symptoms, but not related to major depressive episodes.
-
•
No interaction effects between baseline net worth and a negative wealth shock are observed on depression outcomes.
1. Introduction
Wealth is an important social determinant of mental health (Ettman et al., 2020; Hudson et al., 2012; Kourouklis et al., 2020). Individuals with low income and negative wealth (i.e., debt) are more likely to experience mental health symptoms compared to those with more affluent socioeconomic resources (Ettman et al., 2022; Keene et al., 2015; Prati, 2024). In particular, steady income and wealth status can provide economic security and facilitate individuals' access to mental health services and health-promoting resources (Ettman et al., 2022). Conversely, a sudden loss of substantial wealth (i.e., a negative wealth shock) represents a stressful life event that can lead to rapid changes in economic status and leave fewer available economic resources. Previous research has pointed to strong associations between a sudden large loss in wealth and clinically relevant changes in health such as a decline in physiological functioning (Boen & Yang, 2016), psychological stress (Schwandt, 2018), psychiatric morbidity (Pool et al., 2017), and all-cause mortality (Pool et al., 2018). Taken together, a negative wealth shock can be a major stressor that threatens individuals’ physical and psychosocial well-being.
Negative wealth shocks can be particularly detrimental among older adults, who are more likely to have complex health needs and high medical expenditures (Lehnert et al., 2011). A negative wealth shock can occur due to multi-level reasons, including societal-level economic recession and individual-level life events such as marital dissolution and a major illness onset (Cho et al., 2025; Ettman et al., 2022). As older adults are more likely to have multiple chronic conditions and rely on health-promoting products, having steady positive wealth is crucial to financial security and maintaining desired health (Babiarz et al., 2013). While having Medicare enrollment at 65 years of age may be linked to reduced financial strains, recent evidence also shows that unaffordability of medical care is prevalent among Medicare enrollees, especially those with poorer health and having a disability (Madden et al., 2021), which can potentially threaten their financial status. Additionally, a negative wealth shock in middle to late life may permanently lower one's socioeconomic status and even impoverish individuals who have reached retirement due to less opportunities to earn income, rebuild assets, and economically recover from the shock (Butrica et al., 2010). Consequently, a sudden large loss in wealth in late life can be a long-term stressor that dampens older adults' sense of control and threatens retirement security (Butrica et al., 2010; Mejía et al., 2016). Given the distinct nature of a large loss in wealth to older adults, it is important to further understand the mental health consequences of negative wealth changes among this population.
The Stress Process Model provide a useful theoretical explanations for understanding how a negative wealth shock may impact mental health (Pearlin et al., 1981). A wealth shock can constitute a primary stressor that triggers stress response and adversely affects emotional well-being, giving rise to both acute and chronic stress due to declined financial well-being (Drentea & Reynolds, 2014). Also, a sudden loss in wealth may activate long-term physiological dysregulation, which in turn can further link to adverse mental health outcomes. Collectively, a wealth shock can be a stress-inducing event that increases psychological and emotional processes through reducing one's coping competency (Drentea & Reynolds, 2014), threatening late-life health and well-being.
Related to the Stress Process Model, a growing body of evidence suggests that individuals who experience a sudden and substantial depletion of wealth are at increased risk of mental health disorders, including depression (Fowler et al., 2014; Keene et al., 2015; Pool et al., 2017). Depression is the most prevalent mental health syndrome among older adults in the United States as well as globally, with clinically significant depressive symptoms affecting 10 %–15 % of adults aged 55 years or older and major depression affecting 2 % of this population (Kok & Reynolds III, 2017). Prior research shows that a negative shock of total net wealth is related to short-term elevated depressive symptoms, suggesting that a wealth shock can trigger stress response leading to poorer mental health outcomes (Pool et al., 2017). Specifically, a negative wealth shock may chronically activate physiological dysregulation in response to the stressful event, increasing the risk of depressive symptoms among older adults (Kobrosly et al., 2014). Recent evidence based on cross-country comparisons also identified consistent association between a negative wealth shock and depressive symptoms in the United States, England, China, and Mexico, emphasizing the importance of wealth shocks regardless of the economic development levels of the country (Ran et al., 2024).
Similarly, evidence from the Great Recession of 2008 also points to the pathway linking sudden loss of financial resources to elevated depressive symptoms and reduced sense of control among older adults (Butrica et al., 2010; Mejía et al., 2016; Modrek et al., 2014; Wilkinson, 2016). For example, prior research suggests that a financial shock during the Great Recession is associated with increased risk of clinically significant depressive disorder (Swift et al., 2020), highlighting the adverse role of wealth shock in psychological well-being. The consistent evidence on wealth shock and depressive symptoms may also provide an alternative explanation for the relationship between economic recession and suicide (Swift et al., 2020).
Recent evidence also suggests that, as a risk factor of mental health outcomes, financial well-being may be an important intervention point for depression assessment and treatment (Vittengl, 2024). Altogether, a negative wealth shock may be linked to depressive symptoms among older adults, highlighting the harmful effects of a negative wealth shock and warranting further investigation on how a wealth shock influences depression in the long term.
Important gaps remain unaddressed in evidence on negative wealth shocks and depression in older adults. First, extant research on the wealth shock-depression associations has primarily relied on the Center for Epidemiologic Studies Depression (CESD) scale or Patient Health Questionnaire (PHQ) to measure depressive symptoms during the past week (McInerney et al., 2013; Pool et al., 2017; Wilkinson, 2016). However, CESD and PHQ have limitations in capturing depression syndrome and persistent symptoms compared to the Composite International Diagnostic Interview (CIDI), which is often used as the gold standard for identifying major depressive disorder (Dang et al., 2020; Gelaye et al., 2014; Maske et al., 2015). According to a recent review on wealth and depression, no study has utilized the CIDI in examining wealth shock-depression associations (Ettman et al., 2022). Recent evidence suggests that the CESD scale is a less sensitive measure for case identification of depression syndrome than the CIDI (Dang et al., 2020), which may be a clinical and diagnostic instrument for depression that takes into consideration both the intensity and duration of symptoms during the past 12 months (Steffick, 2000; Xiang & Cheng, 2019). It is also suggested that multiple measures of depression should be incorporated to examine the robustness of findings (Dang et al., 2020). For example, cross-sectional findings among a sample of US Afro–Caribbean women show that financial hardship is associated with past-week depressive symptoms, but not lifetime major depressive disorder (Erving, 2021). However, little evidence is available to explain whether a sudden loss in wealth is prospectively related to both depressive symptoms in past week and 12-month major depressive episodes. Given the sudden nature of a negative wealth shock and its potential permanent damage to older adults’ financial resources, it warrants a more in-depth investigation to compare how this stressful experience longitudinally influences both past-week depressive symptoms and 12-month depressive disorder.
Second, previous research on negative wealth shocks and depression lacks comparison with older adults who experience zero or negative wealth, which is defined as individual who have no net worth or have debt equal or larger than their assets (Hawkley et al., 2020; Pool et al., 2017). Sustained exposure to asset poverty may be linked to depressive symptoms via mechanisms that are distinct from a sudden large loss in wealth (Ridley et al., 2020). However, limited research has compared whether a negative wealth shock and baseline negative wealth have differing influence on mental health. It is important to understand whether a wealth shock and negative wealth differentially influence depressive symptoms because adaptations to asset poverty and a sudden loss in wealth may require different types and amount of support to cope with the associated mental health consequences.
Relatedly, the extent to which a negative wealth shock can impact depression may depend on one's wealth status prior to the shock. For example, research shows that household wealth status moderates the relationship between a wealth shock and expectations of a future shock, such that wealthier households are less likely to be affected by a wealth shock due to access to alternative livelihood strategies (Freudenreich & Kebede, 2022). Similarly, earlier research shows that non-housing assets (e.g., stock holdings) moderate the association between a subsequent wealth shock and mental health (McInerney et al., 2013). However, evidence in related research suggests that there is no moderating effects of baseline poverty on income shock and loneliness (Hawkley et al., 2020). Taken together, it remains unclear whether baseline wealth status will moderate a negative wealth shock and depressive symptoms. It is possible that older adults with less wealth at baseline are more prone to adverse mental health outcomes if they experience a sudden large loss in wealth due to lack resources to cope with financial hardships. There is scant evidence on whether older adults' baseline wealth moderates the association between a negative wealth shock and depressive symptoms. Understanding these relationships can better inform mental health interventions for financially at-risk older populations.
To address the gaps in the extant research, our study utilizes longitudinal data from the Health and Retirement Study to examine the following research questions among a national sample of adults aged 51 and older: 1) Compared to individuals with positive wealth without a shock, are those experiencing a negative wealth shock or baseline zero/negative wealth at a higher risk of both depressive symptoms (CESD) and major depressive episodes (CIDI)? 2) Does baseline household wealth moderate the association between a negative wealth shock and depressive symptoms? Our study is among the first to incorporate the CIDI-measured depression syndrome in studying its relation to a negative wealth shock. Our study contributes to a more robust understanding of the interplay of baseline wealth and negative wealth shocks on mental health among older adults over time.
2. Methods
2.1. Study Sample
Data came from the Health and Retirement Study (HRS), an ongoing prospective panel study conducted among a nationally representative sample of middle-aged and older adults aged 51 year or older (Sonnega et al., 2014). The HRS employs a complex multi-stage area probability sampling design and the surveys are conducted biannually among individuals from eligible birth cohorts (Heeringa & Connor, 1995). The first wave of HRS was in 1992. The HRS oversampled Black and Hispanic Americans and residents in Florida. HRS was utilized for the study because it contained detailed data on participants’ wealth information and two measures on depression symptomatology, allowing for testing the study aims. For the present study, all data came from HRS RAND longitudinal data from 2008 to 2018 (Bugliari et al., 2024). This period was chosen because major depressive episodes was measured at each survey wave starting in 2008. In total, 16,784 respondents aged above 50 participated in the HRS survey in 2008. We excluded proxy respondents (n = 1120) because data on depressive symptoms were not collected. We omitted 4 respondents who had missing data on depressive symptoms, resulting in a final sample n = 15,660. This sample was followed up from 2008 to 2018. We implemented listwise deletion to the baseline sample to handle the missing data. The overall attrition rate is 48.7 % and the average follow up time is 6.2 years (approximately 3.1 waves). We used a closed cohort starting with participants with available data in 2006.
2.2. Measures
2.2.1. Negative wealth shock (exposure)
The total net worth was calculated for each survey wave as the sum of all wealth components minus all outstanding debts. Wealth components included net value of house, real estate, vehicles, businesses, individual retirement account, stocks, mutual funds, investment trusts, checking, savings, money market accounts, government savings bonds, treasury bills, bond funds, and all other savings. Debts included mortgages, land contracts, other home loans, and all other debts. All net worth values were adjusted to 2018 US dollars based on the Consumer Price Index. In case the respondents did not report a continuous value on wealth variables, follow-up questions with a bracket method using value ranges were provided to ascertain respondents’ assets in ranges. The brackets of value ranges were then incorporated to nearest-neighbor imputation to handle the missing data on wealth (Hurd et al., 2016). Net worth was defined as the sum of all wealth components minus all debts. A negative wealth shock, defined as a sudden loss of 75 % or more in total household net worth, was computed using two consecutive survey waves. The cut-off point of 75 % was used based on previous evidence that it had a minimal probability of misclassification due to measurement error (Cho et al., 2023; Hawkley et al., 2020; Pool et al., 2017). Consistent with previous literature (Boen & Yang, 2016; Cho et al., 2025; Pool et al., 2018), we created three mutually exclusive categories: 1) positive wealth at baseline without a negative wealth shock; 2) positive wealth at baseline with a negative wealth shock; and (3) no or negative wealth at baseline. Specifically, among participants with positive net worth at wave t-1, a loss of net worth of 75 % or more at wave t was considered a “negative wealth shock”, whereas a loss less than 75 % or positive change in the net worth was considered “positive wealth without a shock”. Participants with zero or negative net worth at wave t-1 were all considered “no or negative wealth at baseline” at wave t regardless of any positive or negative change in wealth from wave t-1 to wave t.
2.2.2. Major depressive episodes (outcome)
Major depressive episodes were measured at each wave with the short-form World Health Organization's Composite International Diagnostic Interview (CIDI-SF). The CIDI-SF is a previously validated screening scale that was developed in an effort to detect possible psychiatric disorders in large population surveys (Kessler et al., 1998). The CIDI-SF can be used to assess a probable diagnosis of major depressive episodes during the last 12 months, as the scale was derived based on criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (American Psychiatric Association, 2013). The CIDI-SF contains 33 questions that assess the major depressive episodes in two domains: dysphoria (sadness) and anhedonia (inability to feel pleasure). Respondents who reported dysphoria and/or anhedonia were presented with subsequent questions to probe the duration and frequency of symptoms. The summary scores of CIDI-SF ranged from 0 to 7. Based on previous evidence, a cut-off score of ≥3 was used to dichotomize the CIDI-SF scores and indicate diagnosis of major depressive episodes (Steffick, 2000; Xiang, 2016).
2.2.3. Depressive symptoms (outcome)
Depressive symptoms were assessed at each wave using an 8-item Center for Epidemiologic Studies Depression Scale (CESD-8), which was derived from the full 20-item CESD scale originally developed as a continuous measure of depressive symptomatology (Radloff, 1977). Respondents were asked whether they experienced any of the eight symptoms in the last week (yes or no), including six negative indicators (i.e., depression, everything is an effort, restless sleep, felt alone, felt sad, and could not get going) and two positive indicators (i.e., felt happy and enjoyed life). The two positive indicators were reverse coded. A summary score was created by counting the number of symptoms, with a possible score ranging from 0 to 8. The CESD-8 scale had a Kuder-Richardson 20 coefficient at 0.81, indicating good internal consistency.
2.2.4. Baseline wealth (Moderator)
Baseline wealth status was measured as the total net worth calculated as the sum of all wealth components minus all debts. Baseline wealth was transformed using the inverse hyperbolic sine transformation approach to handle negative values (Friedline et al., 2015).
2.2.5. Covariates
Covariates were selected based on previous literature on mental health consequences of a negative wealth shock among older adults (Boen & Yang, 2016; Cho et al., 2025; Pool et al., 2017; Ran et al., 2024). Demographic covariates included age (in years), gender (male and female), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, and others), and marital status (married/partnered and unmarried/not partnered). Socioeconomic covariates included education (less than high school, high school graduate, some college but no degree, and college degree or above), labor force participation (employed, not employed, and retired), household net worth, and logarithmically transformed household income that was adjusted to 2018 US dollars using the consumer price index (Bugliari et al., 2024). We adjusted household net worth and income to control for the potential impact of financial means on depressive symptoms.
Baseline Health behaviors were adjusted in all models, including alcohol consumption (no drinking, moderate drinking, and excessive drinking) and smoking status (never smoked, past smoker, and current smoker). A Metabolic Equivalent of Task score was calculated to indicate the level of physical activity intensity and frequency. Additional health-related covariates were hospitalization in the past two years (yes or no), health insurance status (yes or no), comorbid chronic conditions (no condition, one condition, or two or more conditions), difficulty in any activities of daily living (yes or no), and limited ability to work due to impaired health (yes or no). All covariates were time-varying except gender, race, education, baseline net worth, and health behaviors, which were measured at baseline. A detailed description of covariates is presented in Supplemental Table 1.
2.3. Analysis Strategy
Baseline sample characteristics were compared across three categories of wealth status using Kruskal-Wallis rank sum or χ 2 test. Next, we employed a two-stage inverse probability weighting (IPW) adjusted mixed-effects models to address the imbalanced distribution of baseline covariates across three wealth shock groups. In particular, we applied the IPW method to adjust for differential exposures to negative wealth shocks (DuGoff et al., 2014). For example, socially disadvantaged older adults may be more vulnerable to both negative wealth shocks and depression syndrome. Standard regression approaches that adjusted for confounders are inadequate in this context because they fail to address the non-random selection into negative wealth shock conditions, potentially leading to a biased estimation (Petersen et al., 2024). The IPW approach addresses this issue by generating a pseudo-population in which the distribution of individual characteristics is independent of experiencing a wealth shock. The analysis involved two steps. First, we generated propensity scores from a generalized boosted regression tree model (GBM) to predict the probability of exposure to each of the three wealth shock conditions (McCaffrey et al., 2004). GBM is a machine learning, data-adaptive modeling algorithm that allows for the flexible estimation of nonlinear relationships with a large number of covariates (McCaffrey et al., 2004). Detailed information on IPWs calculations is provided in Supplemental Materials. All covariates were included in the GBM model. Diagnostic assessments of covariate balance after applying GBM were conducted utilizing the absolute standardized mean differences and the Kolmogorov-Smirnov statistic. Covariate balance was considered achieved if the effect size was less than 0.1 according to Rubin's rule and the Kolmogorov-Smirnov statistic was non-significant for any baseline covariate (Rubin, 2001). The inverse probability weighting method resulted in satisfactory covariate balance on the baseline variables, and an assessment of extreme values was also conducted to ensure no such values were presented. The final weights were created by multiplying the inverse probability weights by the HRS respondent-level survey weights, which accounted for complex study design (i.e., stratum and cluster), sample selection, and non-response.
Second, we estimated four weighted mixed effects regression models to examine the impact of wealth shocks on depressive symptoms. Weighted mixed-effects logistic regressions were used to examine negative wealth shocks and major depressive episodes (CIDI-SF), and weighted mixed-effects negative binominal regressions were used to examine negative wealth shocks and depressive symptoms (CESD-8), adjusting for all covariates in both models. Of the three categories of a negative wealth shock variable, we used positive wealth without a shock as the reference group. We considered multiple variance covariance structures to identify the model with the best fit. Based on the Bayesian information criterion (BIC), we assumed an unstructured variance-covariance structure to allow all variance and covariance to be distinctly estimated. We applied this doubly robust estimation approach to reduce the risk of estimation bias due to model misspecification (Funk et al., 2011; Yu et al., 2023). The model equation was as follows,
where Yit represents the log odds of depressive symptoms for individual i at wave t. Sit is a wealth shock indicator for individual i at wave t. Depressive symptoms and wealth shock were both time-varying variables. Xit captures both time-variant and time-invariant covariates included in the model. Parameter estimates include β0 as the intercept, β1 as the estimated treatment effect of being in a wealth shock group. Ωp are the coefficients of all covariates. μ0i is the random effect for individual i and μ1i is the random effect for the wave slope. Level 1 intra-individual variance is represented with eit and is assumed to have a bivariate normal distribution. Robust standard errors were estimated to adjust clustering effects. We added an interaction term of “baseline wealth × negative wealth shock” to examine whether the association between a negative wealth shock and depressive symptoms varies by participants' baseline net worth. That is, we tested the interaction term to understand whether baseline wealth moderated the effects of a negative wealth shock on depressive symptoms. We conducted a series of sensitivity analyses to test the robustness of our findings. Data analyses were performed using Stata 18 (StataCorp, 2023) and R Studio (R Core Team, 2021).
2.3.1. Sensitivity analyses
Findings from the sensitivity analyses that tested the robustness of our findings are presented in supplemental materials. First, we estimated generalized mixed effects models without adjusting for selection weights (Supplemental Table 2) and without controlling for health behaviors (Supplemental Table 3). Additionally, the findings were robust to alternative cut points for the negative wealth shock exposure (i.e., a loss of 50 % or more in total net worth) (Supplemental Table 4). We further tested our regression models by testing both CIDI and CESD scores as continuous variables (Supplemental Table 5), adding household size as a control variable (Supplemental Table 6), adding interaction terms between wealth shock with housing vs. non-housing wealth (Supplemental Table 7), adjusting for attrition (Supplemental Table 8), and adding interaction between a negative wealth shock with socio-demographic variables (i.e., age, gender, race, education, and baseline wealth in quintiles) (Supplemental Table 9). Findings from our sensitivity analyses largely conformed to results from the main analyses.
3. Results
Table 1 presents baseline socio-demographic and health characteristics by wealth shock. Among the study sample, 18.1 % of older adults experienced a negative wealth shock. Statistically significant differences in all variables by wealth shock status were observed (p < 0.01). Older adults who experienced a negative wealth shock were more likely to be older, women, White, and with less education compared to those with positive wealth without a shock. Additionally, individuals with a negative wealth shock reported worse health-related outcomes, such as smoking, less physical activity, being hospitalized in the past 2 years, no health insurance, multimorbidity, ADL difficulty, and limited ability to work due to impaired health.
Table 1.
Baseline sample characteristics (N = 15,660).
| Positive wealth without a shock (n = 11,999; 76.6 %) | No or negative wealth at baseline (n = 822; 5.2 %) | Negative wealth shock (n = 2839; 18.1 %) | |
|---|---|---|---|
| CIDI-SF (%) | |||
| No | 93.0 (92.3, 93.5) | 84.0 (80.7, 86.9) | 91.1 (89.2, 92.7) |
| Yes | 7.0 (6.5, 7.7) | 16.0 (13.1, 19.3) | 8.9 (7.3, 10.8) |
| CESD-8 (mean) | 1.3 (1.2, 1.3) | 2.8 (2.6, 3.0) | 1.6 (1.5, 1.7) |
| Age (mean) | 66.9 (66.6, 67.3) | 65.2 (64.2, 66.2) | 67.6 (67.0, 68.1) |
| Gender (%) | |||
| Men | 46.1 (45.3, 46.8) | 39.2 (34.5, 44.0) | 39.2 (37.0, 41.4) |
| Women | 53.9 (53.2, 54.7) | 60.8 (56.0, 65.5) | 60.8 (58.6, 63.0) |
| Race (%) | |||
| White, non-Hispanic | 83.8 (81.6, 85.8) | 48.6 (43.5, 53.6) | 75.8 (72.8, 78.6) |
| Black, non-Hispanic | 7.3 (6.5, 8.2) | 27.8 (24.2, 31.7) | 12.1 (10.4, 14.2) |
| Hispanic | 6.4 (4.8, 8.4) | 21.3 (16.9, 26.5) | 8.8 (6.8, 11.2) |
| Other | 2.5 (1.9, 3.2) | 2.3 (1.3, 4.0) | 3.3 (2.4, 4.4) |
| Education (%) | |||
| Less than high school | 13.7 (12.5, 15.1) | 43.9 (38.7, 49.2) | 20.8 (19.0, 22.9) |
| High school graduate | 34.6 (33.2, 36.1) | 29.3 (24.9, 34.1) | 35.7 (33.6, 37.8) |
| Some college, no degree | 24.0 (22.7, 25.2) | 18.1 (14.6, 22.3) | 25.3 (23.1, 27.7) |
| College degree or above | 27.7 (25.8, 29.6) | 8.7 (5.9, 12.5) | 18.2 (15.8, 20.7) |
| Household net worth a (median, IQR) | 358,360 (125,240, 833,280) | −1860 (−12,003, 0) | 154,380 (31,378, 499,720) |
| Household income b (median, IQR) | 59,964 (30,480, 112,080) | 16,790 (10,498, 36,206) | 42,523 (21,096, 84,156) |
| Marital Status (%) | |||
| Married/partnered | 69.0 (67.7, 70.2) | 31.2 (26.6, 36.2) | 56.5 (54.0, 59.0) |
| Unmarried/no partner | 31.0 (29.8, 32.3) | 68.8 (63.8, 73.4) | 43.5 (41.0, 46.0) |
| Smoking status (%) | |||
| Never smoked | 43.4 (42.0, 44.8) | 34.1 (30.1, 38.3) | 43.3 (41.2, 45.5) |
| Past smokers | 43.8 (42.4, 45.3) | 38.5 (35.0, 42.3) | 40.5 (38.2, 42.9) |
| Current smoker | 12.8 (11.9, 13.7) | 27.4 (23.7, 31.5) | 16.2 (14.2, 18.4) |
| Alcohol consumption (%) | |||
| No drinking | 61.6 (59.7, 63.4) | 75.4 (71.1, 79.3) | 69.8 (67.0, 72.4) |
| Moderate drinking | 25.0 (23.4, 26.7) | 11.9 (9.2, 15.4) | 18.4 (16.4, 20.5) |
| Heavy drinking | 13.5 (12.7, 14.3) | 12.6 (9.8, 16.1) | 11.8 (10.3, 13.6) |
| Metabolic Equivalent of Task score (mean, SE) | 22.6 (22.2, 23.0) | 15.7 (14.2, 17.2) | 20.6 (19.8, 21.4) |
| Hospitalization (%) | |||
| No | 75.8 (74.8, 76.8) | 67.7 (63.6, 71.6) | 72.7 (70.6, 74.7) |
| Yes | 24.2 (23,2, 25.2) | 32.3 (28.4, 36.4) | 27.3 (25.3, 29.4) |
| Having health insurance c (%) | |||
| No | 4.8 (4.1, 5.7) | 14.4 (10.9, 18.7) | 9.6 (8.0, 11.4) |
| Yes | 95.2 (94.3, 95.9) | 85.6 (81.3, 89.1) | 90.4 (88.6, 92.0) |
| Multimorbidity d (%) | |||
| no condition | 16.1 (15.2, 17.1) | 10.6 (8.2, 13.5) | 13.7 (12.1, 15.4) |
| 1 condition | 26.5 (25.6, 27.5) | 19.4 (16.0, 23.2) | 24.9 (22.9, 27.1) |
| ≥ 2 conditions | 57.4 (56.3, 58.4) | 70.1 (66.0, 73.9) | 61.4 (59.1, 63.7) |
| ADL difficulty e (%) | |||
| No | 87.4 (86.7, 88.1) | 66.5 (61.9, 70.8) | 83.7 (82.0, 85.3) |
| Yes | 12.6 (11.9, 13.3) | 33.5 (29.2, 38.1) | 16.3 (14.7, 18.0) |
| Health limits work (%) | |||
| No | 75.5 (74.4, 76.5) | 54.9 (50.8, 58.9) | 72.1 (69.4, 74.6) |
| Yes | 24.5 (23.5, 25.6) | 45.1 (41.1, 49.2) | 27.9 (25.4, 30.6) |
| Labor Force (%) | |||
| Employed | 43.1 (41.7, 44.5) | 31.9 (27.4, 36.7) | 40.9 (38.5, 43.3) |
| Not employed | 9.6 (8.9, 10.4) | 20.3 (17.2, 23.9) | 11.9 (10.6, 13.5) |
| Retired | 47.3 (46.1, 48.5) | 47.8 (42.8, 52.8) | 47.2 (45.0, 49.3) |
Note. 95 % confidence interval in parentheses. IQR = interquartile range. Chi-squared test and Kruskal-Wallis rank sum test were used as appropriate to test bivariate relationships. HRS-provided person-level sampling weights and design factors (i.e., cluster and stratum) were adjusted to generate weighted estimates.
Household income was adjusted to 2018 US dollars using the Consumer Price Index, and was logarithmically transformed using the function log(wealth + 1).
Household net worth was adjusted to 2018 US dollars using the Consumer Price Index. Inverse hyperbolic sine transformation was applied to using the function log(wealth + ).
Health insurance status was based on whether respondents reported any of the insurance plan: Medicare, Medicaid, CHAMPVA/CHAMPUS, private insurance, or employer-provided health insurance.
Multimorbidity was classified based on a count of eight self-reported conditions: heart disease, hypertension, diabetes, stroke, cancer, arthritis, lung disease, and psychiatric problems.
ADL = activities of daily living, including five domains: bathing, eating, dressing, walking across the room, and getting in and out of bed.
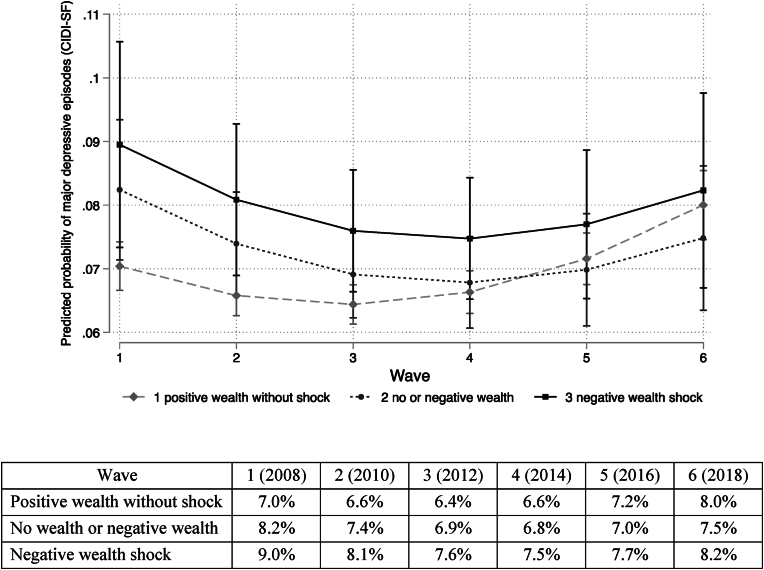
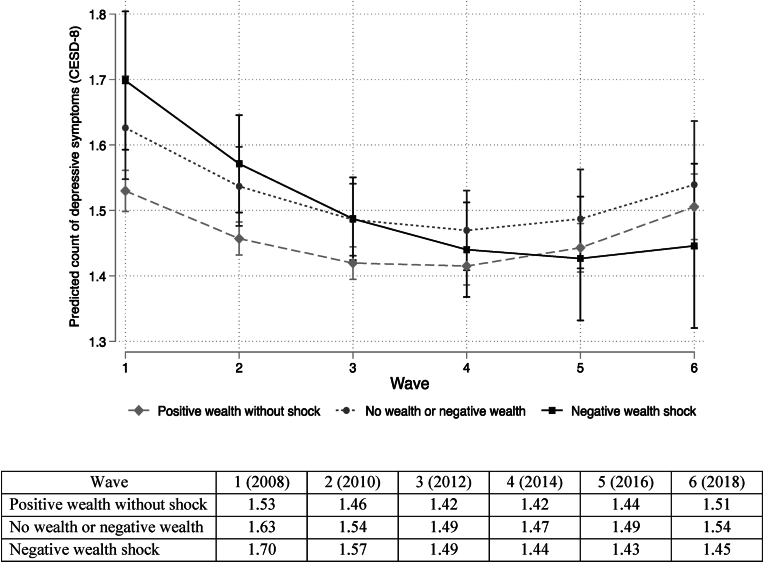
Table 2 presents result from mixed-effects regression models estimated with inverse probability weights. Regarding our first research question on the association between a negative wealth shock and depressive symptoms, Model 1 shows that respondents who experienced a negative wealth shock showed significantly higher odds of having the CIDI-measured major depressive episodes over time (OR = 1.30, 95 % CI: 1.1–1.6, p < 0.05), compared to those who experienced positive wealth without a shock. No statistically significant differences in CIDI-SF were found between individuals with zero or negative wealth and those with positive wealth without a shock. Model 2 shows that, compared to positive wealth without a shock, a negative wealth shock was associated with 1.04 times (95 % CI: 1.01–1.08, p < 0.05) the rate of CESD-measured depressive symptoms over time. Also, zero/negative wealth was associated with 1.05 (95 % CI: 1.01–1.09, p < 0.05) times the rate of CESD-measured depressive symptoms. The predicted probability of a major depressive episode and depressive symptoms by wealth shock are presented in Fig. 1, Fig. 2. Additionally, we present changes in major depressive episodes and depressive symptoms over time in Fig. 3, Fig. 4.
Table 2.
Mixed-effects logistic regression and negative binomial regression of depression by wealth status Among Middle-Aged and Older Adults, HRS, 2008–2018.
| Model 1 CIDI-SF |
Model 2 CESD-8 |
Model 3 CIDI-SF |
Model 4 CESD-8 |
|
|---|---|---|---|---|
| OR (95 % CI) | IRR (95 % CI) | OR (95 % CI) | IRR (95 % CI) | |
| Wealth shock | ||||
| Positive wealth without shock | Reference | Reference | Reference | Reference |
| No or negative wealth | 1.09 (0.92, 1.30) | 1.04 (1.01, 1.08) | 1.15 (0.96, 1.38) | 1.04 (1.01, 1.08) |
| Negative wealth shock | 1.30 (1.06, 1.60) | 1.05 (1.01, 1.09) | 1.02 (0.60, 1.71) | 1.03 (0.95, 1.12) |
| Baseline net worth in 2008 | 0.99 (0.98, 1.00) | 0.98 (0.98, 0.99) | 0.99 (0.98, 1.01) | 0.99 (0.98, 0.99) |
| Wealth shock × Baseline net wealth in 2008 | ||||
| Positive wealth without shock × net worth in 2008 | – | – | Reference | Reference |
| No/negative wealth × net worth in 2008 | – | – | 0.98 (0.97, 1.00) | 1.00 (0.99, 1.00) |
| Negative wealth shock × net worth in 2008 | – | – | 1.02 (0.97, 1.07) | 1.00 (0.99, 1.01) |
| Intercept | 0.41 (0.19, 0.91) | 1.43 (1.16, 1.76) | 0.39 (0.18, 0.86) | 1.44 (1.17, 1.78) |
| Variance of Random Effects | ||||
| Wave slope | 0.21 (0.17, 0.26) | 0.02 (0.02, 0.03) | 0.21(0.17, 0.26) | 0.02 (0.02, 0.03) |
| Intercept | 5.89 (5.06, 6.86) | 1.03 (0.97, 1.10) | 5. 91 (5.07, 6.88) | 1.03 (0.97, 1.10) |
| Variance-covariance | −0.64 (−0.81, −0.47) | −0.06 (−0.07, −0.05) | −0.64 (−0.82, −0.47) | −0.06 (−0.07, −0.05) |
| Number of person-years | 65,954 | 65,956 | 65,954 | 65,956 |
| BIC | 27273 | 184962 | 27291 | 185545 |
Note. OR = odds ratio. IRR = incidence rate ratio. CI = confidence interval. BIC = Bayesian information criterion. Baseline net worth was inverse hyperbolic sine transformed. Inverse probability weights were applied to adjust for participants' conditional probability of experiencing positive wealth, zero/negative wealth, or negative wealth shock. Models controlled for age, gender, race, educational attainment, marital status, alcohol consumption, smoking status, metabolic equivalent of task scores, household income (log transformed), hospitalization in past 2 years, health insurance status, multimorbidity, difficulty in activities of daily living (ADL), health limits the ability to work, labor force participation, and survey wave.
Fig. 1.
Predicted Probability of Major Depressive Episodes by Wealth Status among Middle-Aged and Older Adults. Figure is based on Table 2 Model 1.
Fig. 2.
Predicted Count of Depressive Symptoms by Wealth Status among Middle-Aged and Older Adults. Figure is based on Table 2 Model 2.
Fig. 3.
Predicted Probability of Major Depressive Episodes by Wealth Status, HRS 2008–2018. Note. The predicted probabilities were derived from the mixed-effect logistic regression model of major depressive episodes in Table 1 Model 1. The estimated inverse probability weighting was applied to adjust for selection bias. The marginal effects were significant at p < 0.05 significance level.
Fig. 4.
Predicted Count of Depressive Symptoms by Wealth Status, HRS 2008–2018. Note. The predicted probabilities were derived from the mixed-effect negative binomial regression model of depressive symptoms in Table 1 Model 2. The estimated inverse probability weighting was applied to adjust for selection bias. The marginal effects were significant at p < 0.05 significance level.
Regarding our second research question, we did not observe statistically significant interaction effects between baseline wealth and a negative wealth shock for either the CESD-8 or CIDI-SF. Results from the interaction terms are shown in Model 3 and Model 4.
4. Discussion
Our study is among the first to use CIDI-measured depressive symptoms in studying wealth shock-depression associations. Using longitudinal data from a national sample of adults aged over 50, we examined the associations between a negative wealth shock and depression, including both 12-month major depressive episodes (CIDI-SF) and past-week depressive symptoms (CESD-8). Our study is among the first to use CIDI-SF to capture clinically relevant major depressive episodes in relation to a negative wealth shock. By using two measures of depression, our study contributes to a more granular and robust understanding of how a negative wealth shock may be related to depression, which is important to inform mental health programs for older adults at financial risk. Our findings largely support the Stress Process Model by showing that a negative wealth shock can adversely affect mental health. Three primary findings emerged from this study. First, a negative wealth shock is associated with both 12-month major depressive episodes (CIDI-SF) and past-week depressive symptoms (CESD-8), showing robust association between negative wealth shocks and depression syndrome. Second, similar to a negative wealth shock, having zero or negative wealth is linked to more depressive symptoms measured with CESD-8, but not related to major depressive episodes measured with CIDI-SF. Third, we did not observe interaction effects between baseline wealth and a negative wealth shock for either the CESD-8 or the CIDI-SF, suggesting that a negative wealth shock represents a stressor that can negatively impact older adults’ mental health regardless of whether they have low or high wealth before the shock. Taken together, these findings point to the importance of both sudden loss in wealth and no/negative wealth on mental health outcomes among older adults, and also echoes previous evidence that CESD-8 and CIDI-SF may be tapping into differing construct of depression (Dang et al., 2020).
Our results are consistent with previous evidence (McLaughlin et al., 2012; Pool et al., 2017; Schwandt, 2018) that a sudden large loss in wealth in middle to late life can be a stressful life event that triggers an adverse psychological response, leading to elevated depressive symptoms. It is possible that negative changes in financial resources can inhibit older adults' ability to meet routine life payments and reduce their financial satisfaction, which may heighten their depressive symptoms (Wilkinson, 2016). Our findings are also consistent with related research, particularly the sizable literature documenting negative wealth changes as risk factors for suicide and all-cause mortality among older populations (Almeida et al., 2012; Duberstein et al., 2004). Collectively, our findings demonstrate that a negative wealth shock among adults over 50 represents a major stressor that can adversely impact individuals’ mental health.
We observed complex findings on zero/negative wealth at baseline in association with depression outcomes. Unlike a negative wealth shock, which is related to both past-week depressive symptoms (CESD-8) and 12-month major depressive episodes (CIDI-SF), zero/negative wealth is associated with past-week depressive symptoms, but not the risk of 12-month major depressive episodes. These findings on zero/negative wealth are similar to evidence based on a national sample of US Afro–Caribbean women, which found that financial strain is related to past-week depressive symptoms, but not lifetime major depressive disorder (Erving, 2021). Zero/negative wealth may have less influence on clinically relevant depressive disorder compared to a sudden large loss in wealth. It is possible that older adults living with baseline negative wealth have daily financial struggles but may not perceive their financial situation as an acute and sudden stressful crisis, while individuals who experience a negative wealth shock are more likely to perceive it as a crisis. Additionally, prior evidence suggests that subjective perception of financial stress is a stronger predictor of poorer mental health than objective indicators of wealth (Wilkinson, 2016). Our study focused on objective measures of wealth changes, which may not capture and reflect older adults’ subjective perception of their financial status. Therefore, future research needs to further explore subjective perceptions of wealth changes and depressive symptoms.
An alternative explanation for the difference in major depressive episodes between individuals with a negative wealth shock and those with zero or negative wealth may be due to the difference between the two depression measures, as depression measured by CESD-8 and CIDI-SF are not interchangeable (Dang et al., 2020). Specifically, while CIDI-SF is a clinical diagnostic instrument of depression, CESD-8 taps into a broader construct beyond depression and can detect non-specific psychological distress (Dang et al., 2020; Radloff, 1977). Therefore, our findings suggest that while both negative wealth shock and baseline negative wealth may be linked to adverse mental health, a negative wealth shock is also related to clinically relevant major depressive episodes.
Interestingly, we did not observe an interaction between baseline net worth and a subsequent wealth shock on either measure of depressive symptoms. That is, a negative wealth shock has harmful influence on mental health regardless of older adults' wealth status prior to the shock. In related research, evidence suggests that there is no moderating effects of baseline poverty status on the association between income shock and loneliness (Hawkley et al., 2020). An earlier study focusing on 2008 economic recession reports that baseline wealth may moderate the effects of a wealth shock on mental health if baseline wealth consists of non-housing assets (McInerney et al., 2013), because non-housing financial assets, such as stock holdings, are subject to a higher risk of sudden loss. In our study, we assess wealth encompassing both housing assets and non-housing financial assets, minus debts. Home ownership constitutes an important portion of older adults’ wealth, which may buffer the effects of loss in non-housing wealth. We did not observe significant interaction effects between a negative wealth shock with baseline housing vs. non-housing asset in the supplemental analysis. A possible explanation is that the study by McInerney (2013) utilized two waves of data (2006 and 2008) to capture immediate effects of wealth loss on mental health during the Great Recession. We utilized data from 2008 to 2018, and the interaction effects between a negative wealth shock and non-housing asset may become less revealing over time.
Additionally, while we define a negative wealth shock as a loss of 75 % of wealth, as adopted by prior research (Hawkley et al., 2020; Pool et al., 2017, 2018), it may carry non-equivalent implications for older adults with low and high income. It is possible that a small loss in wealth can substantially impact low-income older adults’ mental health, whereas a larger portion of loss in wealth is needed to detect mental health effects among high-income individuals. Future research is needed to examine a variety of parameters of wealth shock.
The study findings should be interpreted in light of limitations. First, the HRS recruited participants aged 51 years or older. Therefore, it is unknown whether the study participants experienced wealth shocks at a younger age. Individuals who had experienced wealth shocks in early adulthood are likely to be more resilient and prepared to cope with the sudden loss of wealth in late life. Thus, we were not able to control for the effects of previous wealth shocks that may have occurred at participants' younger age, which may lead to an underestimation of the effects of wealth shocks on depressive symptoms. Second, the literature suggests that the influence of a negative wealth event on mental health may depend on individuals' subjective perception of stress about wealth (Ennis et al., 2000), which is not available in the HRS. While baseline net worth can be an indicator of individuals’ economic status, it does not tap into perceived stress about losing wealth. Therefore, future research can further test the potential moderating role of perceived wealth status in the association between a negative wealth shock and mental health. Third, wealth shock was based on changes in wealth from wave t-1 to wave t, and depressive symptoms were assessed in wave t. Due to the limitation in temporality, we cannot determine whether wealth shock caused depressive symptoms or vice versa. Last, the study period spanned from 2008 to 2018, during which the Great Recession in 2008 and the enactment of the Affordable Care Act in 2010 occurred. We were unable to ascertain whether the observed negative wealth shock during 2008–2010 was due to structural or individual reasons, both of which may contribute to elevated depressive symptoms.
5. Conclusions
Using two measures of depressive symptoms, longitudinal national data, and robust empirical methods, this study contributes to a more in-depth understanding of the association between a sudden loss of substantial wealth and depressive symptoms among adults over age 50 in the US. Our findings suggest that a negative wealth shock can be a major stressful life event that is associated with both clinically relevant major depressive episodes and a higher count of depressive symptoms. The high mental health risk of both wealth loss and zero/negative wealth in late life indicates the urgency to provide tailored mental health programs to address mental health needs among older adults – both those with negative wealth and whose who experience a negative wealth shock. Beyond a focus on targeted mental health services, these results demonstrate the continued need to more directly address the economic situations of older adults – addressing asset poverty, reducing the risk of wealth loss (such as those caused by catastrophic medical payments), and supporting those experiencing a wealth shock.
CRediT authorship contribution statement
Weidi Qin: Writing – review & editing, Writing – original draft, Methodology, Investigation, Formal analysis, Conceptualization. Jiao Yu: Writing – original draft, Formal analysis. Belinda L. Needham: Writing – review & editing, Methodology, Conceptualization. Stephanie A. Robert: Writing – review & editing, Methodology, Conceptualization.
Human participant protection
The Health and Retirement Study was approved by the University of Michigan Institutional Review Board under the Protocol Number: HUM00061128. The present study used de-identified secondary data from the Health and Retirement Study, and thus it was exempt from IRB review.
Funding
The preparation of this article was supported in part by the National Institute on Aging of the National Institutes of Health under the grant number T32AG000221 (WQ), P30AG017266 (WQ) and P30AG066613 (JY). The Health and Retirement Study is sponsored by the National Institute on Aging (U01AG009740) and is conducted by the University of Michigan. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Declaration of interest
The authors declare that there is no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2025.101871.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Data availability
We used publicly available and accessible data from the Health and Retirement Study.
References
- Almeida O.P., Draper B., Snowdon J., Lautenschlager N.T., Pirkis J., Byrne G., Sim M., Stocks N., Flicker L., Pfaff J.J. Factors associated with suicidal thoughts in a large community study of older adults. British Journal of Psychiatry. 2012;201(6):466–472. doi: 10.1192/bjp.bp.112.110130. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . 5th ed. 2013. Diagnostic and statistical manual of mental disorders. [DOI] [Google Scholar]
- Babiarz P., Widdows R., Yilmazer T. Borrowing to cope with adverse health events: Liquidity constraints, insurance coverage, and unsecured debt. Health Economics. 2013;22(10):1177–1198. doi: 10.1002/hec.2877. [DOI] [PubMed] [Google Scholar]
- Boen C., Yang Y.C. The physiological impacts of wealth shocks in late life: Evidence from the great recession. Social Science & Medicine. 2016;150:221–230. doi: 10.1016/j.socscimed.2015.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bugliari D., Carroll J., Hayden O., Hayes J., Hurd M., Lee S., Main R., McCullough C., Meijer E., Pantoja P., Rohwedder S. RAND HRS longitudinal file 2020 (V2) documentation. The RAND Center for the Study of Aging. 2024 https://hrsdata.isr.umich.edu/sites/default/files/documentation/other/1715891203/randhrs1992_2020v2.pdf Santa Monica, CA. [Google Scholar]
- Butrica B.A., Smith K.E., Toder E.J. What the 2008 stock market crash means for retirement security. Journal of Aging & Social Policy. 2010;22(4):339–359. doi: 10.1080/08959420.2010.507623. [DOI] [PubMed] [Google Scholar]
- Cho T.-C., Yu X., Adar S.D., Choi H., Langa K.M., Kobayashi L.C. Changes in marital and health status as risk factors for a subsequent negative wealth shock: A population-based longitudinal study in the United States, 1995–2020. Social Science & Medicine. 2025;371 doi: 10.1016/j.socscimed.2025.117905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho T.-C., Yu X., Gross A.L., Zhang Y.S., Lee J., Langa K.M., Kobayashi L.C. Negative wealth shocks in later life and subsequent cognitive function in older adults in China, England, Mexico, and the USA, 2012–18: A population-based, cross-nationally harmonised, longitudinal study. The Lancet Healthy Longevity. 2023;4(9):e461–e469. doi: 10.1016/S2666-7568(23)00113-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dang L., Dong L., Mezuk B. Shades of blue and gray: A comparison of the center for epidemiologic studies depression scale and the composite international diagnostic interview for assessment of depression syndrome in later life. The Gerontologist. 2020;60(4):e242–e253. doi: 10.1093/geront/gnz044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drentea P., Reynolds J.R. Where does debt fit in the stress process model? Society and Mental Health. 2014;5(1):16–32. doi: 10.1177/2156869314554486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duberstein P., Conwell Y., Conner K., Eberly S., Caine E. Suicide at 50 years of age and older: Perceived physical illness, family Discord and financial strain. Psychological Medicine. 2004;34(1):137–146. doi: 10.1017/S0033291703008584. [DOI] [PubMed] [Google Scholar]
- DuGoff E.H., Schuler M., Stuart E.A. Generalizing observational study results: Applying propensity score methods to complex surveys. Health Services Research. 2014;49(1):284–303. doi: 10.1111/1475-6773.12090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ennis N.E., Hobfoll S.E., Schröder K.E.E. Money doesn't talk, it swears: How economic stress and resistance resources impact inner-city women's depressive mood. American Journal of Community Psychology. 2000;28(2):149–173. doi: 10.1023/A:1005183100610. [DOI] [PubMed] [Google Scholar]
- Erving C.L. The effect of stress exposure on depressive symptoms and major depressive episode among US Afro–Caribbean women. Social Psychiatry and Psychiatric Epidemiology. 2021;56(12):2227–2238. doi: 10.1007/s00127-021-02096-8. [DOI] [PubMed] [Google Scholar]
- Ettman C.K., Adam G.P., Clark M.A., Wilson I.B., Vivier P.M., Galea S. Wealth and depression: A scoping review. Brain and Behavior. 2022;12(3) doi: 10.1002/brb3.2486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman C.K., Cohen G.H., Galea S. Is wealth associated with depressive symptoms in the United States? Annals of Epidemiology. 2020;43:25–31.e1. doi: 10.1016/j.annepidem.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler K.A., Gladden R.M., Vagi K.J., Barnes J., Frazier L. Increase in suicides associated with home eviction and foreclosure during the US housing crisis: Findings from 16 national violent death reporting system states, 2005–2010. American Journal of Public Health. 2014;105(2):311–316. doi: 10.2105/AJPH.2014.301945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freudenreich H., Kebede S.W. Experience of shocks, household wealth and expectation formation: Evidence from smallholder farmers in Kenya. Agricultural Economics. 2022;53(5):756–774. doi: 10.1111/agec.12718. [DOI] [Google Scholar]
- Friedline T., Masa R.D., Chowa G.A.N. Transforming wealth: Using the inverse hyperbolic sine (IHS) and splines to predict youth's math achievement. Social Science Research. 2015;49:264–287. doi: 10.1016/j.ssresearch.2014.08.018. [DOI] [PubMed] [Google Scholar]
- Funk M.J., Westreich D., Wiesen C., Stürmer T., Brookhart M.A., Davidian M. Doubly robust estimation of causal effects. American Journal of Epidemiology. 2011;173(7):761–767. doi: 10.1093/aje/kwq439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelaye B., Tadesse M.G., Williams M.A., Fann J.R., Vander Stoep A., Andrew Zhou X.-H. Assessing validity of a depression screening instrument in the absence of a gold standard. Annals of Epidemiology. 2014;24(7):527–531. doi: 10.1016/j.annepidem.2014.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley L.C., Zheng B., Song X. Negative financial shock increases loneliness in older adults, 2006–2016: Reduced effect during the great recession (2008–2010) Social Science & Medicine. 2020;255 doi: 10.1016/j.socscimed.2020.113000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeringa S.G., Connor J.H. Technical description of the health and retirement survey sample design. 1995. https://hrs.isr.umich.edu/publications/biblio/5310
- Hudson D.L., Neighbors H.W., Geronimus A.T., Jackson J.S. The relationship between socioeconomic position and depression among a US nationally representative sample of African Americans. Social Psychiatry and Psychiatric Epidemiology. 2012;47(3):373–381. doi: 10.1007/s00127-011-0348-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurd M.D., Meijer E., Moldoff M., Rohwedder S. RAND Corporation; Santa Monica, CA: 2016. Improved wealth measures in the health and retirement Study: Asset reconciliation and cross-wave imputation. [DOI] [Google Scholar]
- Keene D.E., Cowan S.K., Baker A.C. “when you’re in a crisis like that, you don't want people to know”: Mortgage strain, stigma, and mental health. American Journal of Public Health. 2015;105(5):1008–1012. doi: 10.2105/AJPH.2014.302400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Andrews G., Mroczek D., Ustun B., Wittchen H.-U. The world health organization composite international diagnostic interview short-form (CIDI-SF) International Journal of Methods in Psychiatric Research. 1998;7(4):171–185. doi: 10.1002/mpr.47. [DOI] [Google Scholar]
- Kobrosly R.W., van Wijngaarden E., Seplaki C.L., Cory-Slechta D.A., Moynihan J. Depressive symptoms are associated with allostatic load among community-dwelling older adults. Physiology & Behavior. 2014;123:223–230. doi: 10.1016/j.physbeh.2013.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kok R.M., Reynolds III C.F. Management of depression in older adults: A review. JAMA. 2017;317(20):2114–2122. doi: 10.1001/jama.2017.5706. [DOI] [PubMed] [Google Scholar]
- Kourouklis D., Verropoulou G., Tsimbos C. The impact of wealth and income on the depression of older adults across European welfare regimes. Ageing and Society. 2020;40(11):2448–2479. doi: 10.1017/S0144686X19000679. [DOI] [Google Scholar]
- Lehnert T., Heider D., Leicht H., Heinrich S., Corrieri S., Luppa M., Riedel-Heller S., König H.-H. Review: Health care utilization and costs of elderly persons with multiple chronic conditions. Medical Care Research and Review. 2011;68(4):387–420. doi: 10.1177/1077558711399580. [DOI] [PubMed] [Google Scholar]
- Madden J.M., Bayapureddy S., Briesacher B.A., Zhang F., Ross-Degnan D., Soumerai S.B., Gurwitz J.H., Galbraith A.A. Affordability of medical care among medicare enrollees. JAMA Health Forum. 2021;2(12) doi: 10.1001/jamahealthforum.2021.4104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maske U.E., Busch M.A., Jacobi F., Beesdo-Baum K., Seiffert I., Wittchen H.-U., Riedel-Heller S., Hapke U. Current major depressive syndrome measured with the patient health Questionnaire-9 (PHQ-9) and the composite international diagnostic interview (CIDI): Results from a cross-sectional population-based study of adults in Germany. BMC Psychiatry. 2015;15(1):77. doi: 10.1186/s12888-015-0463-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCaffrey D.F., Ridgeway G., Morral A.R. Propensity score estimation with boosted regression for evaluating causal effects in observational studies. Psychological Methods. 2004;9:403–425. doi: 10.1037/1082-989X.9.4.403. American Psychological Association. [DOI] [PubMed] [Google Scholar]
- McInerney M., Mellor J.M., Nicholas L.H. Recession depression: Mental health effects of the 2008 stock market crash. Journal of Health Economics. 2013;32(6):1090–1104. doi: 10.1016/j.jhealeco.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin K.A., Nandi A., Keyes K.M., Uddin M., Aiello A.E., Galea S., Koenen K.C. Home foreclosure and risk of psychiatric morbidity during the recent financial crisis. Psychological Medicine. 2012;42(7):1441–1448. doi: 10.1017/S0033291711002613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mejía S.T., Settersten J.R.A., Odden M.C., Hooker K. Responses to financial loss during the great recession: An examination of sense of control in late midlife. The Journals of Gerontology: Serie Bibliographique. 2016;71(4):734–744. doi: 10.1093/geronb/gbv054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modrek S., Hamad R., Cullen M.R. Psychological well-being during the great recession: Changes in mental health care utilization in an occupational cohort. American Journal of Public Health. 2014;105(2):304–310. doi: 10.2105/AJPH.2014.302219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin L.I., Menaghan E.G., Lieberman M.A., Mullan J.T. The stress process. Journal of Health and Social Behavior. 1981;22(4):337–356. doi: 10.2307/2136676. [DOI] [PubMed] [Google Scholar]
- Petersen G.L., Jørgensen T.S.H., Mathisen J., Osler M., Mortensen E.L., Molbo D., Hougaard C.Ø., Lange T., Lund R. Inverse probability weighting for self-selection bias correction in the investigation of social inequality in mortality. International Journal of Epidemiology. 2024;53(4) doi: 10.1093/ije/dyae097. [DOI] [PubMed] [Google Scholar]
- Pool L.R., Burgard S.A., Needham B.L., Elliott M.R., Langa K.M., Mendes de Leon C.F. Association of a negative wealth shock with all-cause mortality in middle-aged and older adults in the United States. JAMA. 2018;319(13):1341–1350. doi: 10.1001/jama.2018.2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pool L.R., Needham B.L., Burgard S.A., Elliott M.R., de Leon C.F.M. Negative wealth shock and short-term changes in depressive symptoms and medication adherence among late middle-aged adults. Journal of Epidemiology & Community Health. 2017;71(8):758 LP–763. doi: 10.1136/jech-2016-208347. [DOI] [PubMed] [Google Scholar]
- Prati G. The reciprocal relationships between economic status and mental health: Investigating the between-person and within-person effects in a three-wave longitudinal study. Journal of Affective Disorders. 2024;366:16–24. doi: 10.1016/j.jad.2024.08.169. [DOI] [PubMed] [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2021. R: A language and environment for statistical computing. [Google Scholar]
- Radloff L.S. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Ran G., Zuo C., Liu D. Negative wealth shocks and subsequent depressive symptoms and trajectories in middle-aged and older adults in the USA, England, China, and Mexico: A population-based, multinational, and longitudinal study. Psychological Medicine. 2024;54(14):3888–3895. doi: 10.1017/S0033291724002332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridley M., Rao G., Schilbach F., Patel V. Poverty, depression, and anxiety: Causal evidence and mechanisms. Science. 2020;370(6522) doi: 10.1126/science.aay0214. [DOI] [PubMed] [Google Scholar]
- Rubin D.B. Using propensity scores to help design observational studies: Application to the tobacco litigation. Health Services & Outcomes Research Methodology. 2001;2(3):169–188. doi: 10.1023/A:1020363010465. [DOI] [Google Scholar]
- Schwandt H. Wealth shocks and health outcomes: Evidence from stock market fluctuations. American Economic Journal: Applied Economics. 2018;10(4):349–377. doi: 10.1257/app.20140499. [DOI] [Google Scholar]
- Sonnega A., Faul J.D., Ofstedal M.B., Langa K.M., Phillips J.W.R., Weir D.R. Cohort profile: The health and retirement study (HRS) International Journal of Epidemiology. 2014;43(2):576–585. doi: 10.1093/ije/dyu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp . StataCorp LLC; College Station, TX: 2023. Stata statistical software: Release 18. [Google Scholar]
- Steffick D.E. Institute for Social Research, University of Michigan; Ann Arbor, MI: 2000. Documentation of affective functioning measures in the health and retirement study.https://hrs.isr.umich.edu/sites/default/files/biblio/dr-005.pdf (Survey research center). [Google Scholar]
- Swift S.L., Elfassy T., Bailey Z., Florez H., Feaster D.J., Calonico S., Sidney S., Kiefe C.I., Zeki Al Hazzouri A. Association of negative financial shocks during the great recession with depressive symptoms and substance use in the USA: The CARDIA study. Journal of Epidemiology & Community Health. 2020;74(12):995 LP–1001. doi: 10.1136/jech-2020-213917. [DOI] [PubMed] [Google Scholar]
- Vittengl J.R. Low household income, financial literacy, or financial health: Which is the strongest risk factor and outcome of depressive symptomatology? Journal of Affective Disorders. 2024;344:18–24. doi: 10.1016/j.jad.2023.10.019. [DOI] [PubMed] [Google Scholar]
- Wilkinson L.R. Financial strain and mental health among older adults during the great recession. The Journals of Gerontology: Serie Bibliographique. 2016;71(4):745–754. doi: 10.1093/geronb/gbw001. [DOI] [PubMed] [Google Scholar]
- Xiang X. History of major depression as a barrier to health behavior changes after a chronic disease diagnosis. Journal of Psychosomatic Research. 2016;85:12–18. doi: 10.1016/j.jpsychores.2016.04.001. [DOI] [PubMed] [Google Scholar]
- Xiang X., Cheng J. Trajectories of major depression in middle‐aged and older adults: A population‐based study. International Journal of Geriatric Psychiatry. 2019;34:1506–1514. doi: 10.1002/gps.5161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu J., Qin W., Huang W., Thomas K. Oral health and mortality among older adults: A doubly robust survival analysis. American Journal of Preventive Medicine. 2023;64(1):9–16. doi: 10.1016/j.amepre.2022.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
We used publicly available and accessible data from the Health and Retirement Study.