Abstract
Objective: Screening for mental illness in primary care is widely recommended, but little is known about the evaluation, treatment, and long-term management processes that follow screening. The aim of this study was to examine and describe the quality of mental health care for persons with chronic obstructive pulmonary disease (COPD) and anxiety/depressive disorders, as measured by adherence to practice guidelines.
Method: This retrospective chart review examined data for 102 primary care and mental health care patients with COPD who were diagnosed, using Structured Clinical Interview for DSM-IV criteria, with major depressive disorder, dysthymia, depression not otherwise specified, generalized anxiety disorder, or anxiety not otherwise specified. Data were gathered from primary care progress notes from the year prior to enrollment in a randomized controlled trial (enrollment was from July 2002 to April 2004). We compared the care received by these patients over 1 year with that recommended by practice guidelines. Charts were abstracted using a checklist of recommended practice guidelines for diagnostic evaluation, acute treatment, and long-term management of anxiety and depressive disorders.
Results: Fifty (49%) of the 102 patients were recognized during the review year as having an anxiety or depressive disorder. Eighteen patients were newly assessed for depressive or anxiety disorders during the chart review year. Patients followed in primary care alone, compared with those who were comanaged by mental health care providers, were less likely to have guideline-adherent care.
Conclusion: Depressive and anxiety disorders are recognized in about half of patients; however, guideline-supported diagnostic evaluation, acute treatment (except for medications), and long-term management rarely occur in the primary care setting. To improve the treatment of depressive and anxiety disorders in primary care, the process of care delivery must be understood and changed.
Anxiety and depression are common in the medical setting1 and often appear together.2 Growing evidence suggests that anxiety3 and depression4 occur in those with chronic obstructive pulmonary disease (COPD) at levels above those observed in the general population.5 When these illnesses are not recognized and treated, the physical and social impairments of COPD are impacted negatively, compounding the effects of COPD on activities of daily living, social functioning, psychological functioning, and recreational activities.6–9 Rapid recognition and treatment of depression could be advantageous, as delay may make remission of depression more difficult to attain.10 Unfortunately, mental illnesses are not well recognized, assessed, or treated in patients with COPD.
In 1987, Yellowlees et al.11 looked at 50 consecutive patients with COPD admitted to a respiratory unit. Of these patients, 29 had an Axis I psychiatric diagnosis, and though some had seen a psychiatrist in the past, no patient was being seen by a psychiatrist at the time of evaluation. Similarly, a 1990 study of 50 consecutive COPD patients seen in an outpatient clinic found that none of the patients with a psychiatric diagnosis had a history of psychiatric treatment.12 In 2000, Kim et al.13 showed that less than 25% of patients with recent pulmonary function tests and depression or anxiety were receiving appropriate medications. This limited use of anxiolytics and antidepressants has also been found in nonacute, hospitalized patients with COPD and anxiety or depression.14 None of the aforementioned studies examined adherence to practice guidelines. Previous studies have, however, assessed guideline-based process measures in large non-COPD samples with a primary focus on antidepressant use and duration15 or appropriate medication and counseling.16 These studies found that many patients with depressive or anxiety disorders are undertreated, both within the Veterans Affairs (VA) system15 and in a large national sample.16
We examined the recognition, diagnostic evaluation, acute treatment, and long-term management of depression and anxiety in a sample of primary care patients with COPD and 1 or more of the following anxiety or depressive disorders: generalized anxiety disorder, anxiety not otherwise specified (NOS), depression NOS, dysthymia, or major depressive disorder. The objective of this study was to examine and describe the quality of mental health care, as measured by recognition of anxiety/depression and adherence to practice guidelines, for persons with COPD and anxiety/depressive disorders.
METHOD
This study was conducted within the context of a randomized controlled trial to test the use of cognitive-behavioral therapy for persons with COPD and comorbid anxiety and/or depression. All research subjects participated in informed consent procedures approved by the Baylor College of Medicine Institutional Review Board.
Participants
Participants for this study were recruited in 3 stages: an administrative database search, telephone screening, and in-person interviews. All persons who received care at the Michael E. DeBakey VA Medical Center (Houston, Tex.) in the previous year and had a diagnosis of bronchitis, emphysema, asthma, bronchiectasis, chronic airway obstruction, or respiratory condition not otherwise specified (ICD-9 codes: 466, 490, 491, 492, 493, 494, 496, and 508) were targeted for recruitment using the VA outpatient and inpatient treatment files. The setting from which this sample was drawn includes a nested mental health clinic available for immediate referral for complicated psychiatric patients and for consultation as needed.
Of the 21,796 patients with an ICD-9 code suggesting chronic breathing disorders, 1981 were randomly selected and screened by telephone for presence of breathing difficulties. Then, the 1632 prescreened patients who acknowledged a breathing problem were asked 5 questions from the Primary Care Evaluation of Mental Disorders (PRIME-MD) patient questionnaire17 to screen for depression and anxiety.18
Patients who acknowledged breathing difficulties and answered at least 1 PRIME-MD item positively were recruited for an in-person baseline assessment. At this evaluation (N = 557), depression was assessed using the Beck Depression Inventory-II,19 and anxiety was assessed using the Beck Anxiety Inventory.20 In the patients with clinically significant levels of depression and/or anxiety (N= 444), portable spirometry was administered to confirm COPD (forced expiratory volume in 1 second [FEV1]/forced vital capacity [FVC] < 75% and FEV1 < 70%), and the Mini-Mental State Examination (MMSE)21 was administered to ensure adequate cognitive functioning (defined as an MMSE score ≥ 24). COPD was present in 250 of the 444 patients to whom spirometry was administered. From the 250 patients, 46 were excluded for the following reasons: severely depressed and/or suicidal (N = 12), active psychosis (N = 9), cognitive impairment (N = 8), active substance use disorders (N = 9), and other (N = 8). Of the 204 remaining patients to whom the Structured Clinical Interview for DSM-IV (SCID) was administered, 104 patients met SCID diagnostic criteria for at least 1 of the following depressive or anxiety disorders: major depressive disorder, dysthymia, depression NOS, generalized anxiety disorder, or anxiety NOS. Two of these patients did not see primary care providers during the review year and were excluded, leaving 102 patients in the sample population.
Chart Review
Primary care progress notes from the 12 months prior to study enrollment (enrollment began July 11, 2002, and ended April 30, 2004) were reviewed for the 102 patients identified by the SCID as having a depressive or anxiety disorder. A PGY4 psychiatry resident (K.R.) abstracted all charts in consultation with a board-certified geriatric psychiatrist (M.E.K.).
Practice guidelines were sought as a benchmark for use in evaluating the quality of care in the recognition, diagnostic evaluation, acute treatment, and long-term management of depressive and anxiety disorders. Practice guidelines22–32 for depression and anxiety found in PubMed (language: English; publication type: “Practice Guideline”; keywords: major depressive disorder, dysthymia, generalized anxiety disorder) and National Guideline Clearing-house (keywords: major depressive disorder, dysthymia, generalized anxiety disorder) searches were evaluated using the criteria suggested by Hayward et al.33
Our search revealed that the Veterans Health Administration/Department of Defense (VHA/DoD) had published a practice guideline for depression and dysthymia. This guideline was selected because it was the standard of care for the VA. In addition to having specific guidelines for primary care, the VHA/DoD guideline was rigorous and compared favorably with other guideline options.27 For generalized anxiety disorder and anxiety disorder NOS, the Institute for Clinical Systems Improvement (ICSI) practice guideline was selected.28 The ICSI guideline more explicitly described the process for selecting evidence for the recommendations, had strength of evidence gradation, and had been pilot-tested in the clinical setting.
The clinical guidelines for anxiety and depression followed a common pattern of dividing treatment into 3 components: diagnostic evaluation, acute treatment, and long-term management. The specific evaluation and treatment components were surprisingly similar, and Table 1 lists the recommendations used in our study. Each recommendation was coded as having been completed or not completed. Any reference within the chart to any of the listed components was coded as having met guideline criteria. For example, if the chart stated “not suicidal,” then the reviewer would indicate that the primary care physician had assessed suicide. If the primary care physician documented “I reviewed his medications with him,” this was documented as education, or if the primary care physician listed depression in the problem list with no other mention of depression on the chart, then the reviewer concluded that depression was recognized. Medication adjustments and comments that indicated that the care provider did not need to adjust medications were viewed as appropriate medication management.
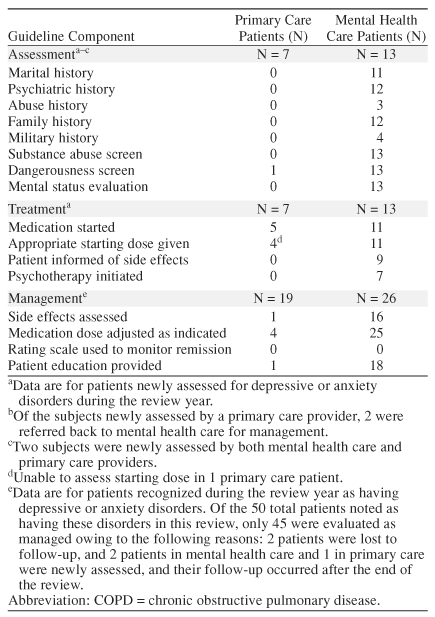
Table 1.
Adherence to Guidelines for the Assessment, Treatment, and Long-Term Management of Anxiety and Depression by Primary Care and Mental Health Care Providers in COPD Patients
RESULTS
Demographics and Diagnoses
The sample of 102 patients with COPD and clinically significant anxiety and/or depression had a mean age of 64.3 years (SD = 11.4) and a mean of 12.7 years of education (SD = 2.9). Men comprised 96% (N = 98) of the sample. Ethnicity was distributed as follows: 75.5% white (N = 77), 17.6% African American (N = 18), 4.9% Hispanic (N = 5), and 2.0% Native American (N = 2). Married patients comprised 53.9% (N = 55) of the sample; 34.3% (N = 35) were divorced/separated, 8.8% (N = 9) were widowed, and 2.9% (N = 3) were never married. The distribution of SCID-based diagnoses among the patients was as follows (the total exceeds 100% because some patients had multiple diagnoses): 45.1% major depressive disorder (N = 46), 27.5% dysthymia (N = 28), 1.0% depression NOS (N = 1), 37.3% generalized anxiety disorder (N = 38), and 23.5% anxiety NOS (N = 24).
Recognition of Patients With Depression and Anxiety
Depressive and/or anxiety disorders were noted by clinicians in the charts of 50 (49%) of the 102 patients (95% CI = 39% to 59%). Thirty-two (64%) of these 50 patients were seen at least once by a mental health care provider. Of the 72 patients with depressive spectrum disorders, 39 (54%) were identified and followed by primary care or mental health care providers (95% CI = 42% to 66%). Twenty-nine (47%) of the 62 patients with anxiety disorders were identified and followed by primary care providers or mental health care providers (95% CI = 35% to 59%).
Diagnostic Assessment and Acute Treatment
During the review year, 20 diagnostic evaluations for depressive or anxiety disorders were performed on 18 subjects (2 subjects were evaluated by both primary care and mental health care providers). Primary care providers completed 7 of these, and mental health care providers completed 13. Table 1 presents data on how frequently primary care and mental health care providers addressed each of the practice guideline evaluation and treatment components.
Primary care documentation of the assessment of dangerousness (suicidal thought) was found in 1 chart. Otherwise, there was no evidence in any primary care diagnostic evaluation chart of other guideline-recommended evaluations, including marital status, psychiatric history, physical abuse history, sexual abuse history, family history, military history, medication history, substance abuse screen, or mental status evaluation. Five (71%) of these 7 patients were started on medications in primary care. There was no documentation of psychotherapy, psychotherapy referral, or information given to patients about medication side effects as recommended in the practice guideline.
Mental health care providers performed 13 diagnostic assessments. Charts frequently documented marital information (85% [N = 11]), psychiatric history (92% [N = 12]), and family history (92% [N = 12]). All charts (100% [N = 13]) documented substance abuse evaluation, assessment of dangerousness (suicidal thought), and a mental status evaluation. Three charts (23%) documented assessment of abuse history, and only 4 charts (31%) documented assessment of military history. Eleven patients (85%) were started on medications, with 9 (69%) being informed of potential side effects. Seven (54%) of the patients' charts documented specific psychotherapeutic interventions.
Long-Term Management
A total of 19 patients received long-term management of depression and/or anxiety from primary care providers during the review year. In reviewing the adherence to practice guidelines for long-term management, it was determined that primary care providers documented medication dose adjustment or dose appropriateness in 4 cases (21%). Side effect monitoring and patient education were noted once each (5%). In no instance was there documentation that primary care providers were monitoring for remission using rating scales, as suggested by the practice guidelines.
Of the 32 patients seen at least once by a mental health care provider, 26 of these patients were managed by mental health care providers during the review year. The other 6 patients were lost to follow-up, returned to primary care, or had their return visit following the initial assessment after the end of the chart review timeframe. Medication dose adjustment or documentation that dose was appropriate was found in 25 instances (96%), and evidence of side effect assessment was evident in 16 charts (62%). Evidence of patient education was present in 18 charts (69%). There was no evidence of monitoring for remission using rating scales.
DISCUSSION
These results provide evidence that depression and anxiety disorders are recognized about 50% of the time in the primary care setting. These results are consistent with one recent primary care study of depression,34 and they suggest improvement compared with studies completed over a decade ago when recognition was only 33% to 36%.35,36
It is difficult to draw conclusions about the assessment and acute treatment process due to the small number of subjects. However, 16 of the 18 patients who were newly recognized during the year were started on treatment with a psychotropic medication. This appears more encouraging than the results of Swindle et al.,37 who found that when primary care physicians were notified of a patient with depression, only 20 of 103 patients identified with depression were started on medication. Any hesitance in prescribing medication should be addressed, given the risks of delaying treatment and the beneficial effects of treatment on breathing in those with COPD.38
Despite the apparent improved recognition and initial treatment by primary care physicians, there appears to be a disparity between primary care and mental health care providers in guideline-based assessment and long-term management. Unfortunately, chart review methodology limits our ability to decipher whether these recommended practices were performed and not documented or simply not performed at all. For example, recently published data suggest that the majority of primary care patients feel adequately informed about their mental health treatment,39 yet we found little evidence of patient education being given to those patients who were treated in primary care alone.
Emerging interventions may help to close the disparity between guideline-recommended care and care in the real world. Primary care time limitations40 were a concern for the International Consensus Group on Depression and Anxiety, which has proposed a time-conscious algorithm for the assessment and acute treatment of depression and anxiety.41 They recommend the following sequence of events: brief screening, then confirmation with a diagnostic checklist and a 1-question suicide screen, followed by treatment. Guideline-driven practice that is accompanied by close consultation with a specialist, such as that used by the Sequenced Treatment Alternatives to Relieve Depression (STAR*D)42 and Re-Engineering Systems for the Primary Care Treatment of Depression (RESPECT) trials,43 may improve primary care delivery by increasing the likelihood of treatment and enhancing long-term management. Better care may also be achieved by integrating mental health care providers into a medicine clinic, as co-location of psychiatric care for geriatric populations led to considerably more engagement in psychiatric care.44 Disease management programs also have a significant effect on depression severity.45
This study has some limitations. This study is set in the VA health care system and uses an all-veteran, mostly male sample. Additionally, veteran beneficiaries have more physical, social, and financial stressors than age-matched nonveteran beneficiary samples,46 which may limit the generalizability of the study to other populations with COPD.
Another important limitation of the study is that patients were excluded if they had severe depression and/or suicidal ideation, which could cause this study to potentially underestimate the detection of mental health conditions by primary care clinicians given that severe depression and suicidal ideation are conditions most likely to result in detection by primary care clinicians.
A simplification of guidelines for a chart review has inherent limitations, as does chart review itself, which cannot capture any physician actions not described in the chart. As a result, this review may underestimate the efforts of primary care in the treatment of anxiety and depression. On the other hand, accuracy of diagnosis was not a focus of this chart review. Care from either guideline set would have probably been appropriate, even with a misdiagnosis due to the similarity of the guidelines.
In our study, we found that primary care physicians recognized depression or anxiety and did not typically use generalized anxiety disorder, dysthymia, or the NOS diagnostic categories. Due to this very general recognition of anxiety and depression, the lack of specific evidence-based guidelines for anxiety and depression NOS appears to be less significant than originally anticipated. It is difficult to draw generalizations because we were only able to review the charts of a small number of patients who received a diagnostic evaluation, acute management, and/or long-term management of anxiety and/or depression.
These findings could also potentially reflect a selection bias, given that patients with more severe mental illnesses may be more likely to be referred to specialists (mental health) who have more active involvement in their disease, while those with milder symptoms may be more likely to be managed in primary care.
Finally, this study did not capture instances in which primary care succeeded in the treatment of depression and anxiety because only patients with active symptoms of depression and/or anxiety were eligible for the study.
The strength of this study of depression and anxiety in persons with COPD is that it captures a snapshot of the quality of care from the point of recognition through long-term management. This study suggests that future interventions to improve quality of care for COPD patients need to address recognition, diagnostic evaluation, acute treatment, and long-term management of anxiety and depression.
Acknowledgments
The authors thank Laura Krishnan, M.S., for invaluable assistance in the preparation of this manuscript.
Pretest and Objectives
Instructions and Posttest
Registration Form
Footnotes
This material is based on work supported by a grant from the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service (IIR 00-097), Washington, D.C. This work was also supported in part by the Houston Center for Quality of Care and Utilization Studies, which is partially funded by the Health Services Research and Development Service, Office of Research and Development, Washington, D.C.; and the South Central MIRECC, Department of Veterans Affairs, Washington, D.C.
In the spirit of full disclosure and in compliance with all ACCME Essential Areas and Policies, the faculty for this CME activity were asked to complete a full disclosure statement. The information received is as follows: Drs. Roundy, Cully, Stanley, Veazey, Souchek, Wray, and Kunik have no significant commercial relationships to disclose relative to this article.
REFERENCES
- Zinbarg RE, Barlow DH, and Liebowitz M. et al. The DSM-IV field trial for mixed anxiety-depression. Am J Psychiatry. 1994 151:1153–1162. [DOI] [PubMed] [Google Scholar]
- Zung WW, Magruder-Habib K, and Velez R. et al. The comorbidity of anxiety and depression in general medical patients: a longitudinal study. J Clin Psychiatry. 1990 51suppl 6. 77–80. [PubMed] [Google Scholar]
- Brenes GA. Anxiety and chronic obstructive pulmonary disease: prevalence, impact, and treatment. Psychosom Med. 2003;65:963–970. doi: 10.1097/01.psy.0000097339.75789.81. [DOI] [PubMed] [Google Scholar]
- van Ede L, Yzermans CJ, Brouwer HJ. Prevalence of depression in patients with chronic obstructive pulmonary disease: a systematic review. Thorax. 1999;54:688–692. doi: 10.1136/thx.54.8.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunik ME, Roundy K, and Veazey C. et al. Surprisingly high prevalence of anxiety and depression in general medical patients: a longitudinal study. Chest. 2005 127:1205–1211. [DOI] [PubMed] [Google Scholar]
- Oga T, Nishimura K, and Tsukino M. et al. Relationship between different indices of exercise capacity and clinical measures in patients with chronic obstructive pulmonary disease. Heart Lung. 2002 31:374–381. [DOI] [PubMed] [Google Scholar]
- Peruzza S, Sergi G, and Vianello A. et al. Chronic obstructive pulmonary disease (COPD) in elderly subjects: impact on functional status and quality of life. Respir Med. 2003 97:612–617. [DOI] [PubMed] [Google Scholar]
- Engstrom CP, Persson LO, and Larsson S. et al. Functional status and well being in chronic obstructive pulmonary disease with regard to clinical parameters and smoking: a descriptive and comparative study. Thorax. 1996 51:825–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prigatano GP, Wright EC, Levin D. Quality of life and its predictors in patients with mild hypoxemia and chronic obstructive pulmonary disease. Arch Intern Med. 1984;144:1613–1619. [PubMed] [Google Scholar]
- Keller MB, Lavori PW, and Mueller TI. et al. Time to recovery, chronicity, and levels of psychopathology in major depression: a 5-year prospective follow-up of 431 subjects. Arch Gen Psychiatry. 1992 49:809–816. [DOI] [PubMed] [Google Scholar]
- Yellowlees PM, Alpers JH, and Bowden JJ. et al. Psychiatric morbidity in patients with chronic airflow obstruction. Med J Aust. 1987 146:305–307. [DOI] [PubMed] [Google Scholar]
- Karajgi B, Rifkin A, and Doddi S. et al. The prevalence of anxiety disorders in patients with chronic obstructive pulmonary disease. Am J Psychiatry. 1990 147:200–201. [DOI] [PubMed] [Google Scholar]
- Kim HF, Kunik ME, and Molinari VA. et al. Functional impairment in COPD patients: the impact of anxiety and depression. Psychosomatics. 2000 41:465–471. [DOI] [PubMed] [Google Scholar]
- Dowson C, Laing R, and Barraclough R. et al. The use of the Hospital Anxiety and Depression Scale (HADS) in patients with chronic obstructive pulmonary disease: a pilot study. N Z Med J. 2001 114:447–449. [PubMed] [Google Scholar]
- Charbonneau A, Rosen AK, and Ash AS. et al. Measuring the quality of depression care in a large integrated health system. Med Care. 2003 41:669–680. [DOI] [PubMed] [Google Scholar]
- Young AS, Klap R, and Sherbourne CD. et al. The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry. 2001 58:55–61. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persoons P, Luyckx K, and Desloovere C. et al. Anxiety and mood disorders in otorhinolaryngology outpatients presenting with dizziness: validation of the self-administered PRIME-MD Patient Health Questionnaire and epidemiology. Gen Hosp Psychiatry. 2003 25:316–323. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, and Brown GK. Manual for Beck Depression Inventory-II. San Antonio, Tex: The Psychological Corporation. 1996 [Google Scholar]
- Beck AT, Steer RA. Beck Anxiety Inventory: Manual. San Antonio, Tex: The Psychological Corporation. 1990 [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Bauer M, Whybrow PC, and Angst J. et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of unipolar depressive disorders, pt 2: maintenance treatment of major depressive disorder and treatment of chronic depressive disorders and subthreshold depressions. World J Biol Psychiatry. 2002 3:69–86. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Practice Guideline for Major Depressive Disorder in Adults. Am J Psychiatry. 1993 150suppl 4. 1–26. [DOI] [PubMed] [Google Scholar]
- Ballenger JC, Davidson JR, and Lecrubier Y. et al. Consensus statement on generalized anxiety disorder from the International Consensus Group on Depression and Anxiety. J Clin Psychiatry. 2001 62suppl 11. 53–58. [PubMed] [Google Scholar]
- Karasu TB, Gelenberg A, and Merriam A. et al. Practice guideline for the treatment of patients with major depressive disorder. Available at: http://www.psych.org/psych_pract/treatg/pg/Depression2e.book.cfm. Accessed March 1, 2004. [Google Scholar]
- Major Depression Workgroup. Major depression in adults for mental health care providers. Available at: http://www.icsi.org/knowledge/detail.asp?catID=29&itemID=179. Accessed Aug 27, 2004. [Google Scholar]
- Major Depressive Disorder Working Group. VHA/DoD clinical practice guideline for the management of major depressive disorder in adults. Available at: http://www.oqp.med.va.gov/cpg/MDD/MDD_Base.htm. Accessed March 1, 2004. [Google Scholar]
- Major Depression, Panic Disorder and Generalized Anxiety Disorder in Primary Care Workgroup. Major depression, panic disorder and generalized anxiety disorder in adults in primary care. Available at: http://www.icsi.org/knowledge/. Accessed March 1, 2004. [Google Scholar]
- Glassman R, Farnan L, and Gharib S. et al. Depression: a guide to diagnosis and treatment. Available at: http://www.brighamandwomens.org/medical/handbookarticles/depression/depression_frame.asp. Accessed March 1, 2004. [Google Scholar]
- US Preventive Services Task Force. Screening for depression: recommendations and rationale. Ann Intern Med. 2002;136:760–764. doi: 10.7326/0003-4819-136-10-200205210-00012. [DOI] [PubMed] [Google Scholar]
- Management of Substance Use Disorders Working Group. VHA/DoD clinical practice guideline for the management of substance use disorders. Available at: http://www.oqp.med.va.gov/cpg/SUD/SUD_Base.htm. Accessed March 1, 2004. [Google Scholar]
- Snow V, Lascher S, Mottur-Pilson C. Pharmacologic treatment of acute major depression and dysthymia. American College of Physicians-American Society of Internal Medicine. Ann Intern Med. 2000;132:738–742. doi: 10.7326/0003-4819-132-9-200005020-00010. [DOI] [PubMed] [Google Scholar]
- Hayward RS, Wilson MC, and Tunis SR. et al. Users' guides to the medical literature, 8: how to use clinical practice guidelines, A: are the recommendations valid? The Evidence-Based Medicine Working Group. JAMA. 1995 274:570–574. [DOI] [PubMed] [Google Scholar]
- Unutzer J, Katon W, and Callahan CM. et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002 288:2836–2845. [DOI] [PubMed] [Google Scholar]
- Coyne JC, Fechner-Bates S, Schwenk TL. Prevalence, nature, and comorbidity of depressive disorders in primary care. Gen Hosp Psychiatry. 1994;16:267–276. doi: 10.1016/0163-8343(94)90006-x. [DOI] [PubMed] [Google Scholar]
- Perez-Stable EJ, Miranda J, and Munoz RF. et al. Depression in medical outpatients: underrecognition and misdiagnosis. Arch Intern Med. 1990 150:1083–1088. [DOI] [PubMed] [Google Scholar]
- Swindle RW, Rao JK, and Helmy A. et al. Integrating clinical nurse specialists into the treatment of primary care patients with depression. Int J Psychiatry Med. 2003 33:17–37. [DOI] [PubMed] [Google Scholar]
- Smoller JW, Pollack MH, and Systrom D. et al. Sertraline effects on dyspnea in patients with obstructive airways disease. Psychosomatics. 1998 39:24–29. [DOI] [PubMed] [Google Scholar]
- Schwenk TL, Evans DL, and Laden SK. et al. Treatment outcome and physician-patient communication in primary care patients with chronic, recurrent depression. Am J Psychiatry. 2004 161:1892–1901. [DOI] [PubMed] [Google Scholar]
- Rost K, Nutting P, and Smith J. et al. The role of competing demands in the treatment provided primary care patients with major depression. Arch Fam Med. 2000 9:150–154. [DOI] [PubMed] [Google Scholar]
- Ballenger JC, Davidson JR, and Lecrubier Y. et al. A proposed algorithm for improved recognition and treatment of the depression/anxiety spectrum in primary care. Prim Care Companion J Clin Psychiatry. 2001 3:44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush AJ, Fava M, and Wisniewski SR. et al. Sequenced Treatment Alternatives to Relieve Depression (STAR*D): rationale and design. Control Clin Trials. 2004 25:119–142. [DOI] [PubMed] [Google Scholar]
- Dietrich AJ, Oxman TE, and Williams JW Jr. et al. Re-engineering systems for the treatment of depression in primary care: cluster randomised controlled trial. BMJ. 2004 329:602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartels SJ, Coakley EH, and Zubritsky C. et al. Improving access to geriatric mental health services: a randomized trial comparing treatment engagement with integrated versus enhanced referral care for depression, anxiety, and at-risk alcohol use. Am J Psychiatry. 2004 161:1455–1462. [DOI] [PubMed] [Google Scholar]
- Neumeyer-Gromen A, Lampert T, and Stark K. et al. Disease management programs for depression: a systematic review and meta-analysis of randomized controlled trials. Med Care. 2004 42:1211–1221. [DOI] [PubMed] [Google Scholar]
- Perlin J, Kazis LE, and Skinner KM. et al. Health Status and Outcomes of Veterans: Physical and Mental Component Summary Scores Veterans SF-36. 1999 Large Survey of Veteran Enrollees. Executive Report. Washington, DC: Department of Veterans Affairs. 2000 [Google Scholar]