Abstract
Background
Advance care planning (ACP) and advance directives (AD) are tools for supporting person-centered decision-making. In dementia care, the progression of cognitive decline, complex family dynamics and variability in healthcare systems pose unique challenges to effective ACP/AD implementation for people with dementia (PWD).
Methods
We conducted a scoping review of the literature related to ACP/AD in dementia care between 2014 and 2024. Studies were screened and thematically analyzed to identify current approaches, gaps and recommendations for dementia-specific ACP/AD. We identified key stakeholders involved in decision-making and highlighted procedural components for ACP/AD according to stakeholder groups.
Results
Forty studies were included. Key stakeholders included healthcare professionals (HCPs); family members and caregivers; PWD; dyads (PWD and their caregivers); the broader public; policymakers; and researchers. Prominent findings included: the role and training of HCPs; educational and decision-support needs; early and ongoing engagement of PWD; development and evaluation of dementia-specific tools; ethical and procedural challenges in end-of-life decision-making; and the importance of outreach and cultural sensitivity. Promising interventions include structured communication models, psychoeducational programs and tools, although few have been fully adapted for dementia.
Conclusion
Dementia-specific ACP/AD require a relational, flexible and ethically grounded approach that evolves with the individual’s condition. While ACP/AD should reflect the autonomous preferences of the PWD, during late-stage dementia, shared decision-making becomes central to providing care that aligns with the person’s goals and preferences. Future research should focus on inclusive tools and training; timing and process facilitation; and public health strategies to improve access and equity.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12877-025-06514-3.
Keywords: Dementia, Advance care planning, Advance directives, Decision-making, Public health
Introduction
Dementia is a progressive condition affecting various cognitive functions, such as memory, language, thinking and decision-making [1]. As dementia advances, individuals often lose the capacity to express their care preferences, including preferences regarding living arrangements, medical treatment and end-of-life decisions [2, 3]. Given this, early engagement in dementia care planning is critical to ensure that future care aligns with an individual’s values and wishes.
In this review, we distinguish between advance care planning (ACP) and advance directives (AD), and care planning more broadly. ACP refers to an ongoing process of communication and reflection in which individuals, their families and healthcare professionals discuss future preferences for care and treatment, ideally before decision-making capacity of the individual is lost [4]. ADs are formal, often legally binding, documents that record these preferences or designate a surrogate decision-maker [5]. They may be the outcome of an ACP process but can also be completed independently. Care planning, by contrast, is a broader term used in this review that encompasses individualized planning of healthcare and support needs across the dementia trajectory, which may or may not include ACP/ADs.
ACP/AD can help reduce uncertainty, improve outcomes, and provide guidance for families and healthcare professionals when critical care decisions arise [6]. For surrogate decision-makers such as family members and formal caregivers, ACP/AD capture the officially expressed wishes of the person with dementia (PWD) to guide decision-making on their behalf [7]. Healthcare professionals (HCPs), including physicians and nurses, contribute to interpreting these documents and applying them to treatment decision-making by providing medical guidance and safeguarding ethical and legal standards [8]. Policymakers influence the broader systems in which ACP/AD are implemented, by setting legal frameworks, directing healthcare funding, and determining institutional protocols [9].
Planning future care is first and foremost the right of the PWD. Involving multiple stakeholders can improve the efficacy of care planning in dementia and is often, eventually, necessary, but it also introduces certain challenges. Different groups bring divergent priorities, expectations, and emotional responses to the decision-making process. For example, family members may prioritize comfort and familiarity [10], whereas HCPs often emphasize clinical outcomes, safety, and resource limitations [11, 12]. These views may, at times, diverge from the PWD’s previously expressed values and preferences, and progressing dementia often limits the person’s ability to self-advocate. There is a risk that the opinions and interests of others may supersede those of the PWD, especially when the PWD’s wishes are not clearly documented or are interpreted differently by different stakeholders, potentially also leading to coercion. ACP/AD can serve as important safeguards.
Despite the recognized importance of ACP and AD in dementia care, there remains no clear consensus on which procedural components, e.g., interactions, tools, and policies, best meet the unique needs of PWD. A central challenge lies in tailoring these directives and processes to the progressive and variable nature of dementia. PWD have distinct cognitive needs that influence their ability to participate in ACP/AD over time. These evolving impairments demand ACP/AD approaches that are both flexible enough to accommodate changing capacities and specific enough to guide care in later stages. As such, dementia-specific tools are essential to ensure that planning processes remain meaningful, inclusive and responsive to the unique trajectory of dementia. This scoping review addresses the question “What are the critical areas of consideration for individuals making advance care decisions in dementia care?” by identifying (1) key stakeholders, and (2) the procedural components required to support their needs and roles while engaging with ACP/AD completion. As a result, this would allow us to determine how best to design tools that are tailored to PWD. By clarifying what makes ACP/AD more effective and efficient and to whom within dementia care, we aim to contribute to more structured and ethical approaches to dementia care planning.
Methods and materials
Overview
The present scoping review was conducted following the methodological framework proposed by Arksey and O’Malley [13] and reported according to the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews) checklist (Additional file 1). The protocol for the review was preregistered on the Open Science Framework registry in January 2025 [14].
Search strategy
A comprehensive list of specific terms relating to care planning and dementia were identified using a web-based search of relevant published research. A search string was developed for databases: Pubmed, EMBASE, Scopus and Cochrane, and a comprehensive search performed first on 09.04.2024 and updated on 31.10.2024. The detailed search strategy and search strings can be found in Additional file 2.
Eligibility criteria
Articles were screened following specified inclusion and exclusion criteria established by all authors. For inclusion, articles must significantly discuss components of ACP or AD, defined here as elements directly related to their design, use or implementation in dementia care. These included, but were not limited to: (1) communication processes between patients, families, caregivers and healthcare professionals; (2) documentation practices such as AD or other written records; (3) decision-making frameworks or models guiding ACP/AD; (4) patient-family-clinician discussions about values, preferences and goals of care; and (5) practical or ethical considerations in implementing ACP/AD. Only original research articles were included, from 2014 to 2024 to capture timely and relevant findings. Articles were excluded if they did not have a specific focus on dementia, ACP, or AD. Editorials, commentaries, book front/back ends, conference proceedings/abstracts, literature reviews, preprints, protocols and articles not in English were also excluded.
The choice to exclude review articles was deliberate, due to the risk of duplicating results and over emphasizing certain findings as the reviewed articles would already be included individually.
Screening, data extraction and analysis
Screening for articles was conducted in two stages: (1) title and abstract screened by one reviewer (RV), (2) full-text review conducted by three reviewers independently (RV, AF and SG). An interrater reliability of 94.38% was obtained, where any disagreements were solved through discussion.
After full-text review, reviewers RV and AF performed data extraction of all eligible articles. Data extracted included: title of article, DOI, authors, year of publication, country of study, aims, study type, study population, inclusion/exclusion criteria of the study itself, sample size, study setting, intervention (if applicable), outcomes measured, key results, focus on AD or ACP and key considerations for decision-making.
A thematic analysis based on full-text review of the included studies was conducted by RV and further consolidated by AF. Coding of included studies only focused on their research findings and discussions. The thematic analysis extracted content related to key considerations in advance care planning for dementia care.
Results
Search findings
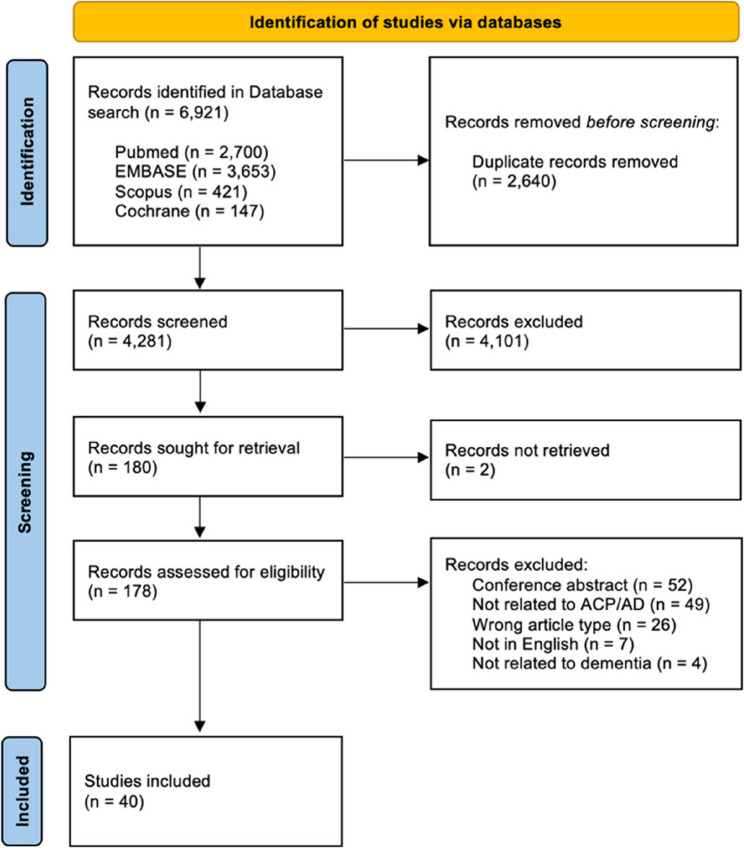
The database search retrieved 6,921 records, of which 2,640 were removed as duplicates. 4,281 records were screened by their title and abstract, of which 180 were determined eligible for full-text review. Of these, 138 articles were excluded and 2 could not be retrieved, resulting in a final pool of 40 reports (see Fig. 1).
Fig. 1.
PRISMA-ScR flowchart showing the study selection. ACP: advance care plan; AD: advance directive
Characteristics of included studies
In this scoping review, 16 of the included studies were conducted in the USA, five in Belgium, three in Germany and Taiwan, two in Australia, Canada and Finland, and one study each in Hong Kong, Israel, Netherlands, New Zealand, Singapore, Switzerland and the United Kingdom. 19 studies were published from 2014 to 2019 and 21 studies from 2020 to 2024.
Of the included studies, 13 were qualitative studies, six were cross-sectional studies, four were cluster RCTs, four were mixed methods studies, four were pilot studies, three were pre-test/post-test interventions, two were retrospective studies, and there was one consensus development, experimental, quasi-experimental and user-centered design study each.
Twenty-five studies focused primarily on ACP, eight on both ACP and AD and seven strictly on AD. A summary of the included studies can be seen in Additional file 3.
Key considerations in dementia care
Based on the included studies, we conducted a thematic analysis structured as follows. First, we identified relevant stakeholders involved in decision-making in dementia care: healthcare professionals (HCPs), caregivers and family members, PWD, dyads (PWD and their caregivers), as well as public, policy and research stakeholders. This specific focus on prioritizing stakeholders allows us to identify how ACP/AD completion takes place across different care contexts by highlighting the distinct roles, needs and interactions of PWD and those supporting their decision-making. Next, we extracted themes specific to each stakeholder group through inductive coding. Data segments were coded iteratively through emerging themes, where three rounds of coding were completed. Two reviewers (RV and AF) went through the final codes and themes of the analyzed studies to ensure reliability and consistency. Table 1 presents these themes along with illustrative examples from the reviewed studies.
Table 1.
Key considerations of the relevant stakeholders in dementia care
| Themes | Examples of key considerations | Studies |
|---|---|---|
| Healthcare professionals (HCPs) | ||
| Role of HCPs | Should involve PWD in ACP, even in advanced stages. | [15] |
| Should determine the timing of ACP and act proactively. | [15, 16] | |
| Should provide more detailed ACP discussions and education, including informal daily conversations. | [15–17] | |
| Should improve communication regarding goals of care and treatment preferences, including context-specific decision-making. | [15, 17] | |
| Should go beyond person-centered care to something more relationship-centered or family-centered care, so it is less medicalized. | [16, 18–21] | |
| Should reduce misconceptions about dementia and ACP. | [22] | |
| Training HCPs | Receiving skill workshops to assess decision-making capacity in PWD. | [23] |
| Receiving training for ACP facilitation in routine clinical practice, for better communication between caregivers and PWD. | [18] | |
| Receiving training for dealing with lack of proxy decision-makers and validity of decisions made close to the time of death. | [24] | |
| Receiving training for recognizing socio-cultural factors which may influence ACP between PWD, family members and caregivers. | [21, 25] | |
| Tools for HCPs | Using clinician-facing tools that are less static and less procedure-oriented. | [26] |
| Using educational interventions to improve ACP documentation. | [27] | |
| Caregivers and family members | ||
| Education and resources | Receiving support for making decisions for the needs of PWD through training materials. | [28] |
| Receiving information regarding context and situation specific treatments and goals of care over the course of the dementia. | [17] | |
| Receiving support in understanding racial differences in care preferences and attitudes towards ACP for formal caregivers. | [29] | |
| Communication with HCPs | Having more frequent contact with HCPs to understand goals of care and treatment decisions. | [30] |
| Receiving nurse-led triadic sessions for ACP, which includes information about dementia and treatments. | [31] | |
| Receiving decision-support interventions for improving communication and goals of care conversations between surrogate decision-makers and HCPs. | [32, 33] | |
| Treatment information | Should be specific to different scenarios and stages of dementia. | [34] |
| Should be provided with the risks and benefits of certain treatments. | [28] | |
| Involvement | Should be included and involved in ACP. | [35] |
| Family dynamics should be considered for creation of ACP, enduring power of attorney and do not resuscitate orders. | [34] | |
| People with dementia (PWD) | ||
| Education | Receiving theoretical interventions for support in selecting hospice and AD completion. | [35] |
| Receiving early and continued education about different stages of dementia, care alternatives, context/scenario specific treatments and medical decisions. | [16, 17, 36] | |
| Receiving assistance with accepting and understanding dementia, anosognosia and reducing stigmas related to dementia. | [16, 17, 20] | |
| Receiving audio-visual information for reducing negative dementia stereotypes and better understanding the impacts on their quality of life. | [37] | |
| Tools for PWD | Access to innovative approaches to will-making for expressing ACP. | [38] |
| Access to educational videos for dementia-specific treatments. | [39] | |
| Using written forms or documents for dementia-specific planning. | [36] | |
| Using ACP videos for aligning between comfort-focused care and ADs (in advanced dementia). | [40] | |
| Outreach | Using public health campaigns to raise awareness of ACP before the onset of dementia. | [23] |
| Improving equitable access to care in underserved communities and providing proactive efforts to reduce social barriers to ACP. | [24] | |
| Identifying community members who are less likely to have ADs and providing support directly to them. | [41] | |
| Dyads (PWD and their caregivers) | ||
| Support | Receiving coaching sessions with HCPs to identify shared values and wishes for care. | [42] |
| Receiving long-term follow-up and support during educational interventions. | [35] | |
| Receiving more regular and continuous communication with HCPs to understand ACP. | [18] | |
| Having a criterion of considerations for HCPs to ensure dyadic concordance (i.e., respect/regard, clarifying processes, trust, affirmative understanding). | [43] | |
| Receiving a holistic, flexible and relational communication process from HCPs when implementing ACP. | [19] | |
| Receiving information from HCPs about the role of surrogate decision-making. | [36] | |
| Resources | Access to ACP manuals and pictures for better understanding the stages of dementia, medical treatments and ACP. | [18] |
| Receiving psychoeducational interventions delivered by a HCP, for PWD, family members/caregivers, following a set criterion of conversations. | [44] | |
| Having an ACP website that can be used by PWD and family members/caregivers with communication tools, testimonials and ACP content. | [45] | |
| Using self-directed interactive workbooks for ACP engagement (i.e., Your Conversation Starter Kit). | [46] | |
| Education | Receiving health education and disease awareness (about dementia). | [42] |
| Support in understanding the reasons to engage in ACP and what are the available resources to do so. | [42] | |
| Public, policymakers and research | ||
| Changes to ACP models | To help in improving the facilitation and guidance of ACP. | [47] |
| To help in the development of process facilitation which incorporates all relevant stakeholders and factors. | [30] | |
| To provide recommendations for HCPs to identify, understand and clarify certain requirements and roles of those involved. | [48] | |
| For establishing meta-directives for end-of-life choices in advanced dementia. | [49] | |
| Changes to dementia care | To better include continuity of care, staff competency and responsibility. | [16] |
| To better dementia-specific ACP guidelines, resources and training of HCPs to deliver these conversations to PWD. | [50] | |
| Research focus | To create a standard for developing ACP interventions for PWD. | [51] |
| Conducting more socio-cultural research to understand gaps, guidance of public health efforts for ACP completion. | [52] | |
| Public outreach | To strengthen public information and education programs for ACP, for PWD. | [53] |
| To better identify and overcome challenges for underserved communities. | [54] | |
Discussion
Principal findings
This scoping review identified dementia-specific procedural components of ACP and AD that are relevant factors for decision-making in such cases. Across the 40 included studies, ACP and AD were explored in relation to HCPs; caregivers and family members; PWD; dyads (PWD and their caregivers); the public; policymakers; and researchers. Key findings highlight the value of structured and consistent ACP, including the use of AD; the specific role of HCPs in facilitating decision-making and how to better prepare them for this role; and the need for resources that support both caregivers and PWD in making informed care and treatment decisions. The following sections provide a more in-depth analysis of findings and implications for future ACP/AD completion.
Key considerations for healthcare professionals (HCPs)
Role of HCPs
HCPs play a vital role in ensuring that PWD are included in ACP/AD decision-making, even in advanced stages of dementia [15]. Their involvement helps reduce misconceptions about dementia or ACP/AD [22] and supports ethical, person-centered care. Meaningful engagement in ACP/AD depends on timely discussions, ideally during admission (particularly in the first weeks/months), during crises and through ongoing informal daily conversations [15, 16]. During these discussions, it is important for HCPs to provide more information, especially towards helping to clarify specific goals of care and treatment preferences, so that patients are able to make fully informed decisions [17]. Finally, a shift towards relationship- or family-centered care may also be necessary, as overly medicalized individualistic approaches may limit participation and shared understanding [16, 18–21].
Training of HCPs
Many HCPs struggle with assessing a patient’s decisional capacity in ethically complex scenarios. Targeted training, such as skill-development workshops or practice through role play, as well as having tools to use with patients and loved-ones can improve confidence and communication [23] Skills for facilitating discussions, incorporating ACP into the routine clinic pathway and engaging in regular communication with PWD and their caregivers are especially important and could help reduce decisional conflicts in ACP/AD planning [18]. Practice addressing ethically complex scenarios, such as the absence of proxy decision-makers or navigating decisions made close to the time of death where documented ADs may not reflect the patient’s self-formulated wishes due to the timing of when they were documented [24], could also be improved through targeted training provided to HCPs. Furthermore, socio-cultural and contextual factors may influence ACP/AD completion between PWD, family members and caregivers [21, 25]; thus, it may be important for HCPs to receive cultural competency training, related to dementia.
Tools for HCPs
Current ACPs are often unable to capture the evolving needs of PWD. Therefore, clinician-facing tools should be enhanced specifically for dementia to better enable ACP for the needs of PWD, where they explore values and explore the caregiver role, which can be done by making the ACP procedure less static and procedure-oriented [26] Educational interventions or decision tools for HCPs could help with improving ACP documentation and communication [27], however the impact of such tools depends on the effectiveness of integrating them into routine care.
In summary, future research should explore how HCPs can be effectively supported in initiating and sustaining ACP conversations with PWD, particularly in the early stages of care and during key transition points such as admission or crisis events. There is a need to develop and evaluate dementia-specific training programs and tools that equip HCPs to navigate the complexities of decision-making capacity, cultural sensitivities, and family dynamics in ACP and AD planning. Further studies should investigate the design and implementation of procedure-oriented ACP tools that move beyond procedural checklists and instead emphasize the evolving values, preferences and social context of PWD and their caregivers [55].
Caregivers and family members
Education and resources
Caregivers and family members are often central to making decisions for PWD, yet many lack the knowledge and support to confidently participate in ACP/AD planning [28]. Here, tailored educational resources are essential [47], ideally including scenario-based guidance that captures the progression of dementia and evolving goals of care [17]. These materials should help caregivers navigate complex treatment decisions over time. For formal caregivers, training should also address cultural variations in care preference, including racial and ethnic attitudes towards ACP/AD and end-of-life decisions [29].
Communication with HCPs
Regular and meaningful communication with healthcare professionals helps caregivers and family members to better understand medical decisions and the broader goals of care [30]. Studies highlight the potential of decision-support interventions to improve this dialogue, especially in facilitating difficult conversations between surrogate decision-makers and clinical teams [32, 33]. Caregivers and family members also reported feeling more engaged when ACP/AD sessions are led by nurses and take place in triadic settings, where the PWD, carers and HCP are all present [31]. These formats foster trust and shared understanding and may reduce the sense of isolation caregivers often report in decision-making processes.
Dementia treatment information and involvement in care planning
Providing information that is tailored to the stage and context of dementia is critical [34]. Caregivers need clarity around the potential risks and outcomes of specific treatments, as well as the practical and ethical implications of decisions such as resuscitation orders or feeding interventions [28, 38]. Involving caregivers and family members in the planning process acknowledges the importance of relational dynamics and promotes decisions that are aligned with the values of both the PWD and their support network [35]. Identifying an enduring power of attorney or health proxy should also be approached as a collaborative and anticipatory process, not just a legal formality [38].
In summary, future research should examine how triadic decision-making models - engaging HCPs, patients and families - used in other chronic illnesses, can inform dementia care planning. Such models could help overcome the challenge of medicalization in dementia-related ACP by fostering trust and shared understanding among all parties involved.
People with dementia (PWD)
Education
Educational support is essential to help PWD better understand their diagnosis, care options and the different medical decisions that they may face [16, 17, 20, 36]. Early and on-going education can improve understanding and acceptance of the condition, and prepare individuals for future care planning [17]. Interventions using audio-visual formats, such as videos about living with dementia, may help reduce stigma, support quality of life discussions and introduce relevant resources [37]. There may be a need for more theory-based educational interventions that guide PWD in considering hospice care and how to complete ADs [35].
Tools for PWD
PWD have expressed interest in more accessible and innovative approaches, such as through digital tools, to write wills that include their ACP/AD [38]. Other innovative approaches may include multimedia and plain-language tools (i.e., like the PREPARE tool [55]), that help users clarify their values, designate proxies and more clearly express care preferences. These tools also help family members in understanding and following the wishes of the PWD. Dementia-specific resources, such as educational videos [39], or structured forms and documents tailored to treatment contexts [36], can make ACP more actionable. For those in advanced stages of dementia, visual aids showing comfort-focused care options may help align decisions with documented ADs [40].
Outreach
A few studies highlight the necessity of supporting outreach around advance care of PWD. For instance, public health campaigns can raise awareness and normalize early planning, particularly before cognitive decline begins [23]. Community-based strategies are needed to reduce social and structural barriers to care planning, especially in underserved communities where ACP/AD engagement is low [24]. Proactive efforts to identify and support community members who are less likely to complete care plans, including culturally targeted outreach and local advocacy, could promote more equitable access [41].
In summary. future research should explore early and continuous educational interventions that help PWD understand their diagnosis, care options and medical decisions. There is a need to develop dementia-specific, digital and context-sensitive tools, such as videos or interactive documents that support PWD in expressing advance care preferences, ideally in collaboration with caregivers. Studies should also assess the effectiveness of outreach strategies, including public health campaigns and community-based efforts, in increasing awareness and equitable access to ACP. Finally, targeted interventions are needed to reach underserved populations who are less likely to engage in ACP/AD.
Dyads (PWD and their caregivers)
Support
Although shared decision-making can support collaborative care planning, it is important to distinguish it from advance decision-making, which prioritizes the autonomy of the person while they still have capacity. However, as the capacity of a PWD declines, shared decision-making is best supported through structured coaching with a HCP where sessions help clarify values and future care preferences [42]. Such interventions should include regular follow-ups to support ongoing communication [18]. Dyads often benefit from guidance on the surrogate’s role and the extent of decision-making leeway they may have [36]. Educational programs aimed at dyads should include long-term support, with content tailored to relational dynamics, achieving dyadic concordance and the evolving nature of dementia [43]. This is particularly important for dyads affected by young-onset dementia, where care planning should especially be holistic, flexible and relational rather than procedural [19].
Resources & education
A range of tools and resources have been developed to support dyads in engaging with ACP/AD, including visual aids [18], interactive websites [45], physical resources [46] and psychoeducational interventions [44]. ACP manuals and pictures can clarify life-sustaining medical procedures and help dyads prepare for end-stage dementia [18]. Online platforms offer structured content, peer testimonials and interactive features, but should allow users to navigate at their own pace [45]. Self-directed workbooks, like Your Conversation Starter Kit, support early ACP engagement by prompting reflection on quality of life, family involvement in decision-making and timing of conversations [46]. Further, psychoeducational interventions delivered by an interventionist, such as SPIRIT [44], which combine education, goal setting and planning support, have also been effective in helping dyads align on goals of care [41].
Overall, dyads require relational, flexible and sustained support to meaningfully engage in dementia-related ACP. Future research should examine how existing tools like PREPARE [55] could be adapted and tested for dyads. Specifically, health education and disease awareness interventions should be tailored to promote joint reflection and shared understanding of the need to engage in ACP processes together, i.e., early in the dementia, providing resources for within the community and contingency planning [42].
Public, policy and research
Changes to ACP models and dementia care
Literature suggests several changes to improve current ACP models. These include better facilitation by HCPs [47] and clearer guidance to ensure all aspects of the ACP process are addressed [30, 48]. When it comes to end-of-life care, or decisions during late-stage dementia, it would be important to include all relevant stakeholders in shared decision-making, to ensure decisions are made according to the PWD’s previous autonomous wishes and current medical assessments. For instance, there is a known challenge when ADs prohibiting life-supporting treatment in late-stage dementia are not followed if the PWD later appears to be “happy” in their dementia [49]. In such conflicts, implementing an explicit meta-directive in the AD, which provides documented instructions for addressing these cases may offer a solution [49].
A synthesis of key recommendations for ACP models includes the following considerations [30, 48]:
Physician’s strategy and ACP initiation: Define timing, whom to involve, discussion topics and context-specific elements.
Patient assessment: Evaluate the patient’s condition and mental capacity.
ACP conversations with PWD: Use communication strategies that involve surrogates, increase disease awareness and explore experiences, needs, fears and care preferences.
Clarify roles of supporters: Understand the willingness, degree of involvement and needs of family members/caregivers, while promoting consensus within the care network.
Non-verbal ACP inclusion: Maximize participation of PWD by attending to non-verbal cues, behaviors and emotions, with caregiver involvement.
Documentation of preferences: Record values, care goals, AD and legal proxies; ensure ACPs are regularly reviewed and communicated to care teams.
End-of-life decision-making: Balance previously expressed wishes with current best interests, in consultation with the broader care team.
Policy support: Develop national frameworks that include HCP training, implementation support and organizational integration of ACP.
Beyond ACP models, restructuring dementia care models more broadly is also needed. This includes clearer care pathways to ensure a continuity of care, role definitions, guidance for ACP implementation, support for professional responsibilities and addressing staff shortages and resource limitations [16, 50].
Research focus
This review identified a limited focus on intervention development [48], with no existing standards for ACP-based dementia interventions [51]. More targeted research is needed to develop, test and refine these tools. In addition, socio-cultural research should explore how ACP is influenced by social norms, beliefs and health system structures [52]. Comparative studies within a country, as well as between countries, can help tailor interventions to different populations [49], reduce stigma and support more inclusive public health strategies [52].
Public outreach
Public education remains a critical factor in increasing engagement with ACP [53]. Strengthening outreach in underserved communities requires more than information alone, but rather relationship-building and community participation. Effective strategies include outreach health programs such as affordable medical clinics in underserved neighborhoods, partnering with trusted local organizations and forming community advisory boards to support culturally relevant outreach [54].
Unaddressed areas within this review and future research avenues
This review highlights that while there is growing recognition of the importance of ACP/AD in dementia care, several gaps remain that limit the effective implementation. Limited public and professional understanding of ACP/AD, unclear roles for surrogate decision-makers and delays in initiating these conversations all contribute to fragmented planning. Furthermore, decision-making is often led by caregivers, especially under high levels of burden, which may inadvertently clash with the wishes of PWD. It should be clarified that while this review highlights the need to initiate dementia-specific ACP/AD completion related activities as soon as dementia is diagnosed, it does not provide evidence in how to initiate conversations, frequency of review or care topics.
Certain questions also could not be answered by this review due to a lack of evidence, including the need for capacity reviews and assessments for cognitive decline – both of which should form necessary considerations for ACP/AD completion. Additionally, the lack of dementia specific ACP/AD forms/tools was striking. While our review emphasizes current effort in educational interventions, future research avenues need to specify what makes dementia-specific ADs a good vehicle for capturing the evolving preferences, values and treatment boundaries of individuals across different stages of cognitive decline. Future research should focus on identifying structural, ethical and contextual components that make dementia-specific ADs clear, actionable and sensitive to the progressive nature of dementia. Co-design approaches that involve PWD, caregivers and HCPs, are especially promising to ensure tools are practical and sensitive to users’ needs.
Designing dementia-specific ACP/AD tools also requires grappling with ethical and legal uncertainties surrounding decisional capacity, influence, and temporal consistency. As in legal assessments of testamentary capacity [56], PWD may experience fluctuating cognitive function, raising critical questions about when and how capacity should be evaluated, and whether a minimal threshold should be defined for making binding decisions [57, 58]. Safeguards, similar to those used to detect undue influence in financial wills, may be needed to ensure that ACP/AD reflect the individual’s authentic wishes rather than those of others [56, 59]. Moreover, ethics literature highlights the tension between prior autonomous choices and current experiential interests, prompting the need for ACP/AD formats that anticipate such conflicts and clarify how the person would want these to be reconciled [60–62]. This calls for dementia-sensitive communication strategies [60] and the inclusion of care preferences that go beyond generic AD templates to address the specific trajectory and care realities of dementia.
Finally, future studies should continue to explore the timeliness and initiation of ACP conversations, building on earlier findings that such discussions often occur too late. Early, ongoing communications that are guided by accessible resources and supported by care teams, may help reduce the burden on caregivers and ensure that planning reflects the true values and preferences of PWD. To ensure ADs continue to be led by autonomous preferences of the PWD, it may also be important for future research to explore how the needs/preferences of caregivers or HCPs may influence their decision-making.
Limitations of this scoping review
This scoping review focuses specifically on a diagnosis of dementia and did not include studies discussing mild cognitive impairments (MCI), subjective cognitive decline (SCD), or other cognitive impairments not meeting the clinical criteria for dementia. The rationale was that while MCI and SCD can be early indicators of dementia, they are distinct conditions where individuals often retain decision-making capacity, which may influence how they engage in ACP conversations. However, due to this criterion, we may have potentially missed a unique context and perspective of early interventions or techniques that may help shape care preferences before dementia progresses.
Conclusion
This scoping review highlights the multidimensional nature of ACP and AD in dementia care, involving healthcare professionals, caregivers and family members, persons with dementia and broader public, policy and research frameworks. While current studies provide foundational insights into ACP/AD implementation, future research should prioritize the creation of dementia-specific, user-friendly tools and the adaptation of existing ACP-supporting frameworks for the dementia context. There is also a critical need for early, ongoing education for PWD, culturally inclusive interventions and scalable public outreach efforts to promote awareness and equitable access. Crucially, advancing ethically grounded approaches require reconciling tensions between autonomy and best-interest judgements in later stages of dementia. Future ACP models must account for this ethical complexity while remaining flexible, inclusive and responsive to relational dynamics in care settings.
Supplementary Information
Additional file 1: PRISMA-ScR checklist.
Additional file 3: Data extraction file of included studies.
Acknowledgements
RV would like to thank the Ethox Centre, University of Oxford and the Caroline Miles Scholarship which allowed her to work on parts of this study during a research visit in November 2024.
Abbreviations
- ACP
Advance care planning
- AD
Advance directive
- HCP
Healthcare professional
- PRISMA-ScR
Preferred reporting items for systematic review and meta-analyses extension for scoing reviews
- PWD
People with dementia
Authors’ contributions
RV and NBA designed the study methodology. RV, AF and SG completed screening and review of all articles. Data extraction and analysis were completed by RV and AF. Manuscript write-up was completed by RV with major contribution from AF and minor contributions from SG and NBA. RV and AF completed manuscript revisions. All authors read and approved the final manuscript.
Funding
Open access funding provided by Swiss Federal Institute of Technology Zurich. This research did not receive any funding.
Data availability
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Alzheimer’s Association. What is Dementia? 2024. https://www.alz.org/alzheimers-dementia/what-is-dementia.
- 2.Givens JL, Kiely DK, Carey K, et al. Healthcare proxies of nursing home residents with advanced dementia: decisions they confront and their satisfaction with decision-making. J Am Geriatr Soc. 2009;57:1149–55. 10.1111/J.1532-5415.2009.02304.X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lamahewa K, Mathew R, Iliffe S, et al. A qualitative study exploring the difficulties influencing decision making at the end of life for people with dementia. Health Expect. 2018;21(1):118–27. 10.1111/HEX.12593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Francesca B, Jox Ralf J, Laura J, et al. Planning ahead with dementia: what role can advance care planning play? A review of opportunities and challenges. Swiss Med Wkly. 2018;148. 10.4414/SMW.2018.14706. [DOI] [PubMed]
- 5.Kollisch DO, Santulli RB, Bernat JL. The limits of advance directives in maintaining autonomy in patients with advanced dementia. Am J Med. 2021;134:963–7. 10.1016/J.AMJMED.2021.02.032. [DOI] [PubMed] [Google Scholar]
- 6.Sampson EL, Burns A. Planning a personalised future with dementia: ‘the misleading simplicity of advance directives.’ Palliat Med. 2013;27:387–8. 10.1177/0269216313484426. [DOI] [PubMed] [Google Scholar]
- 7.Geddis-Regan A, Errington L, Abley C, et al. Enhancing shared and surrogate decision making for people living with dementia: a systematic review of the effectiveness of interventions. Health Expect. 2021;24:19–32. 10.1111/HEX.13167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoffmann TC, Légaré F, Simmons MB, et al. Shared decision making: what do clinicians need to know and why should they bother? Med J Aust. 2014;201:35–9. 10.5694/MJA14.00002. [DOI] [PubMed] [Google Scholar]
- 9.Nakanishi M, Martins Pereira S, Van den Block L, et al. Future policy and research for advance care planning in dementia: consensus recommendations from an international Delphi panel of the European association for palliative care. Lancet Healthy Longev. 2024;5:e370. 10.1016/S2666-7568(24)00043-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pinkert C, Holle B. Home-based care for people living with dementia at the end of life: the perspective of experts. BMC Palliat Care. 2023;22:123. 10.1186/S12904-023-01251-Z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bergmann S, Peper J, Bieber A. The use of formal care for dementia from a professional perspective: a scoping review. BMC Health Serv Res. 2022;22:825. 10.1186/S12913-022-08229-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hall AJ, Manning F, Goodwin V. Qualitative study exploring health care professionals’ perceptions of providing rehabilitation for people with advanced dementia. BMJ Open. 2023;13:e072432. 10.1136/BMJOPEN-2023-072432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. 10.1080/1364557032000119616. [Google Scholar]
- 14.Scoping review of key considerations in decision-making in dementia care. OSF Registry. 2025. https://osf.io/ecy4x/. Accessed 7 Mar 2025.
- 15.Ampe S, Sevenants A, Smets T, et al. Advance care planning for nursing home residents with dementia: policy vs. practice. J Adv Nurs. 2016;72:569–81. 10.1111/JAN.12854. [DOI] [PubMed] [Google Scholar]
- 16.Tetrault A, Nyback MH, Vaartio-Rajalin H, et al. Advance care planning in dementia care: Wants, beliefs, and insight. Nurs Ethics. 2022;29:696–708. 10.1177/09697330211035498. [DOI] [PMC free article] [PubMed]
- 17.Givens JL, Sudore RL, Marshall GA, et al. Advance care planning in community-dwelling patients with dementia. J Pain Symptom Manage. 2018;55:1105–12. 10.1016/J.JPAINSYMMAN.2017.12.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang HL, Lu WR, Liu CL, et al. Advance care planning information intervention for persons with mild dementia and their family caregivers: impact on end-of-life care decision conflicts. PLoS ONE. 2020;15:e0240684. 10.1371/JOURNAL.PONE.0240684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Rickstal R, Vleminck A, De, Engelborghs S, et al. A qualitative study with people with young-onset dementia and their family caregivers on advance care planning: A holistic, flexible, and relational approach is recommended. Palliat Med. 2022;36:964–75. 10.1177/02692163221090385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van Rickstal R, De Vleminck A, Engelborghs S, et al. Experiences with and perspectives on advance care planning in young- and late- onset dementia: a focus group study with physicians from various disciplines. Front Aging Neurosci. 2023;15:1130642. 10.3389/FNAGI.2023.1130642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ali N, Anthony P, Lim WS, et al. Exploring differential perceptions and barriers to advance care planning in dementia among Asian patient–caregiver dyads—a mixed-methods study. Int J Environ Res Public Health. 2021;18:18. 10.3390/IJERPH18137150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bosisio F, Sterie AC, Rubli Truchard E, et al. Implementing advance care planning in early dementia care: results and insights from a pilot interventional trial. BMC Geriatr. 2021;21:1–11. 10.1186/S12877-021-02529-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alam A, Barton C, Prathivadi P, et al. Advance care planning in dementia: a qualitative study of Australian general practitioners. Aust J Prim Health. 2021;28:69–75. 10.1071/PY20307. [DOI] [PubMed] [Google Scholar]
- 24.Naasan G, Boyd ND, Harrison KL, et al. Advance directive and POLST documentation in decedents with dementia at a memory care center: the importance of early advance care planning. Neurol Clin Pract. 2022;12:14–21. 10.1212/CPJ.0000000000001123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chou HH. Exploring the issues of advance directives in patients with mild dementia in Taiwan. Acta Med Okayama. 2020;74:215–20. 10.18926/AMO/59952. [DOI] [PubMed] [Google Scholar]
- 26.Berry CE, Montgomery SH, Santulli R, et al. Adapting the serious illness conversation guide for dementia care. American Journal of Hospice and Palliative Medicine®. 2024;41:942–51. 10.1177/10499091231200214. [DOI] [PubMed] [Google Scholar]
- 27.Cotter VT, Hasan MM, Ahn J, et al. A practice improvement project to increase advance care planning in a dementia specialty practice. American Journal of Hospice and Palliative Medicine®. 2019;36:831–5. 10.1177/1049909119841544. [DOI] [PubMed] [Google Scholar]
- 28.Bonner GJ, Freels S, Ferrans C, et al. Advance care planning for African American caregivers of relatives with dementias: cluster randomized controlled trial. Am J Hospice Palliat Med. 2021;38:547–56. 10.1177/1049909120916127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pettigrew C, Brichko R, Black B, et al. Attitudes toward advance care planning among persons with dementia and their caregivers. Int Psychogeriatr. 2020;32:585–99. 10.1017/S1041610219000784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.van Soest-Poortvliet MC, van der Steen JT, Gutschow G, et al. Advance care planning in nursing home patients with dementia: a qualitative interview study among family and professional caregivers. J Am Med Dir Assoc. 2015;16:979–89. 10.1016/J.JAMDA.2015.06.015. [DOI] [PubMed] [Google Scholar]
- 31.Yeung CCyan, Ho KH man, Chan HY. lai. A dyadic advance care planning intervention for people with early-stage dementia and their family caregivers in a community care setting: a feasibility trial. BMC Geriatr. 2023:23:1–16. 10.1186/S12877-023-03815-3. [DOI] [PMC free article] [PubMed]
- 32.Einterz SF, Gilliam R, Chang Lin F, et al. Development and testing of a decision aid on goals of care for advanced dementia. J Am Med Dir Assoc. 2014;15:251–5. 10.1016/J.JAMDA.2013.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ma H, Kiekhofer RE, Hooper SM, et al. Goals of care conversations and subsequent advance care planning outcomes for people with dementia. J Alzheimers Dis. 2021;83:1767–73. 10.3233/JAD-210720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Volicer L, Stets K. Acceptability of an advance directive that limits food and liquids in advanced dementia. American Journal of Hospice and Palliative Medicine®. 2016;33:55–63. 10.1177/1049909114554078. [DOI] [PubMed] [Google Scholar]
- 35.Chiu wu CH, Perng SJ, Shi CK, et al. Advance care planning and advance directives: a multimedia education program in community-dwelling older adults. J Appl Gerontol. 2020;39:811–9. 10.1177/0733464819831596. [DOI] [PubMed] [Google Scholar]
- 36.Fried TR, Cohen AB, Harris JE, et al. Cognitively impaired older persons’ and caregivers’ perspectives on dementia-specific advance care planning. J Am Geriatr Soc. 2021;69:932–7. 10.1111/JGS.16953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Volhard T, Jessen F, Kleineidam L, et al. Advance directives for future dementia can be modified by a brief video presentation on dementia care: an experimental study. PLoS ONE. 2018;13:e0197229. 10.1371/JOURNAL.PONE.0197229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.de Vries K, Drury-Ruddlesden J. Advance care planning for people with dementia: ordinary everyday conversations. Dementia. 2019;18:3023–35. 10.1177/1471301218764169. [DOI] [PubMed] [Google Scholar]
- 39.Mitchell SL, Shaffer ML, Cohen S, et al. An advance care planning video decision support tool for nursing home residents with advanced dementia: a cluster randomized clinical trial. JAMA Intern Med. 2018;178:961–9. 10.1001/JAMAINTERNMED.2018.1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cohen SM, Volandes AE, Shaffer ML, et al. Concordance between proxy level of care preference and advance directives among nursing home residents with advanced dementia: A cluster randomized clinical trial. J Pain Symptom Manage. 2019;57:37–e461. 10.1016/J.JPAINSYMMAN.2018.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tjia J, Dharmawardene M, Givens JL. Advance directives among nursing home residents with mild, moderate, and advanced dementia. J Palliat Med. 2018;21:16–21. 10.1089/JPM.2016.0473. [DOI] [PubMed] [Google Scholar]
- 42.Vellani S, Puts M, Iaboni A, et al. Acceptability of the voice your values, an advance care planning intervention in persons living with mild dementia using videoconferencing technology. PLoS ONE. 2022;17:e0266826. 10.1371/JOURNAL.PONE.0266826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Clayton JL, Supiano KP, Aruscavage N, et al. Advance care planning in the context of dementia: defining concordance. Gerontologist. 2024. 10.1093/GERONT/GNAE029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Song MK, Ward SE, Hepburn K, et al. Can persons with dementia meaningfully participate in advance care planning discussions? A mixed-methods study of SPIRIT. J Palliat Med. 2019;22:1410–6. 10.1089/JPM.2019.0088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dupont C, Smets T, Monnet F, et al. Defining the content of a website on advance care planning in dementia: a focus group study with family and health professionals. BMC Med Inform Decis Mak. 2023;23:1–9. 10.1186/S12911-023-02359-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sussman T, Lawrence J, Pimienta R. This is how i want it: exploring the use of a workbook with persons with dementia to support advance care planning engagement. Dementia. 2022;21:2601–18. 10.1177/14713012221127358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Blake M, Doray ON, Sinclair C. Advance care planning for people with dementia in Western Australia: an examination of the fit between the law and practice*. Psychiatry Psychol Law. 2018;25:197–218. 10.1080/13218719.2017.1351904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Piers R, Albers G, Gilissen J, et al. Advance care planning in dementia: recommendations for healthcare professionals. BMC Palliat Care. 2018;17:1–17. 10.1186/S12904-018-0332-2/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schoene-Seifert B, Uerpmann AL, Gerß J, et al. Advance (Meta-) Directives for Patients with Dementia who Appear Content: Learning from a Nationwide Survey. J Am Med Dir Assoc. 2016;17:294–9. 10.1016/J.JAMDA.2016.01.014. [DOI] [PubMed]
- 50.Tetrault A, Nyback MH, Vaartio-Rajalin H, et al. Advance care planning in dementia care: wants, beliefs, and insight. Nurs Ethics. 2022;29:696–708. 10.1177/09697330211035498. [DOI] [PMC free article] [PubMed]
- 51.Harrison Dening K, Castle E, Scates C, et al. Advance care plans in dementia: user-centred design. BMJ Support Palliat Care. 2020;10:e38–e38. 10.1136/BMJSPCARE-2018-001700. [DOI] [PubMed]
- 52.Werner P, Ulitsa N, AboJabel H. Exploring the Motivations for Completing Advance Care Directives: A Qualitative Study of Majority/Minority Israeli People Without Dementia. Front Psychiatry. 2022;13:864271. 10.3389/FPSYT.2022.864271. [DOI] [PMC free article] [PubMed]
- 53.Schmidhuber M, Haeupler S, Marinova-Schmidt V, et al. Advance Directives as Support of Autonomy for Persons with Dementia A Pilot Study among Persons with Dementia and Their Informal Caregivers. Dement Geriatr Cogn Dis Extra. 2018;7:328–38. 10.1159/000479426. [DOI] [PMC free article] [PubMed]
- 54.Bonner GJ, Wang E, Wilkie DJ, et al. Advance care treatment plan (ACT-Plan) for African American family caregivers: A pilot study. Dementia. 2014;13:79–95. 10.1177/1471301212449408. [DOI] [PMC free article] [PubMed]
- 55.Sudore RL, Schillinger D, Katen MT, et al. Engaging Diverse English- and Spanish-Speaking Older Adults in Advance Care Planning: The PREPARE Randomized Clinical Trial. JAMA Intern Med. 2018;178:1616–25. 10.1001/JAMAINTERNMED.2018.4657. [DOI] [PMC free article] [PubMed]
- 56.Shulman KI, Cohen CA, Kirsh FC, et al. Assessment of testamentary capacity and vulnerability to undue influence. A J Psychiatry. 2007;164:722–7. 10.1176/AJP.2007.164.5.722/ASSET/IMAGES/R710F2.JPEG. [DOI] [PubMed]
- 57.Grisso Thomas, Appelbaum PS. Assessing Competence to Consent to Treatment: A Guide for Physicians and Other Health Professionals. New York: Oxford University Press 1998.
- 58.Trachsel M, Hermann H, Biller-Andorno N. Cognitive Fluctuations as a Challenge for the Assessment of Decision-Making Capacity in Patients With Dementia. Am J Alzheimers Dis Other Demen. 2015;30:360–3. 10.1177/1533317514539377. [DOI] [PMC free article] [PubMed]
- 59.Trachsel M, Mitchell C, Biller-Andorno N. Decision-making incapacity at the end of life: conceptual and ethical challenges. Bioethica Forum. 2013;6:26–30. doi: 10.5167/UZH-81528
- 60.Dresser R. Dworkin on Dementia: Elegant Theory, Questionable Policy. Hastings Center Report. 1995;25:32–8. 10.2307/3527839. [PubMed]
- 61.Dworkin R. Life’s Dominion: An Argument about Abortion, Euthanasia, and Individual Freedom. New York: Alfred A. Knopf 1993.
- 62.Jaworska A. Respecting the margins of agency: Alzheimer’s patients and the capacity to value. Philos Public Aff. 1999;28:105–38. 10.1111/J.1088-4963.1999.00105.X. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: PRISMA-ScR checklist.
Additional file 3: Data extraction file of included studies.
Data Availability Statement
All data generated or analyzed during this study are included in this published article [and its supplementary information files].