Abstract
Activation of host innate immune responses was studied in severe acute respiratory syndrome coronavirus (SCV)-infected human A549 lung epithelial cells, macrophages, and dendritic cells (DCs). In all cell types, SCV-specific subgenomic mRNAs were seen, whereas no expression of SCV proteins was found. No induction of cytokine genes (alpha interferon [IFN-α], IFN-β, interleukin-28A/B [IL-28A/B], IL-29, tumor necrosis factor alpha, CCL5, or CXCL10) or IFN-α/β-induced MxA gene was seen in SCV-infected A549 cells, macrophages, or DCs. SCV also failed to induce DC maturation (CD86 expression) or enhance major histocompatibility complex class II expression. Our data strongly suggest that SCV fails to activate host cell cytokine gene expression in human macrophages and DCs.
Severe acute respiratory syndrome coronavirus (SCV) (13, 15, 21, 26) causes a severe lung infection that resembles the one caused by the avian influenza virus H5N1, a virus that successfully escapes the antiviral actions of cytokines (2, 27). The epithelial cells of the upper respiratory tract are the primary targets for respiratory viruses, but macrophages and dendritic cells (DCs) are also often infected. Little information is available as to whether SCV infection induces a cytokine response in human macrophages or DCs, the cell types that initially regulate the activation of innate and adaptive immune responses during microbial infections. Alpha/beta interferons (IFN-α/β), the major antiviral cytokines, posses activity against many respiratory viruses (24, 25). However, SCV appears to be somewhat resistant to the antiviral actions of IFNs (5, 30). Here we studied whether SCV can activate cytokine-mediated innate immune responses in human lung epithelial cells or in human monocyte-derived macrophages and DCs.
The SCV Frankfurt-1 isolate (kind gift of H. Rabenau) was propagated in Vero E6 cells (CRL 1586, American Type Culture Collection, Manassas, VA) under BSL-3 conditions (19). The infectivity of the virus was 107 50% tissue culture infective doses/ml. Influenza virus A/Beijing/353/89 (H3N2) and the murine Sendai virus (strain Cantell) served as controls (20, 22). The human lung carcinoma cell line A549 (CCL-185, American Type Culture Collection) and the human hepatoma cell line HuH7 (18) were used in infection and transfection experiments, respectively.
SCV 3a and N genes were PCR amplified (primer sequences available on request) and cloned into the BamHI site of pcDNA 3.1(+) (Invitrogen). The N gene was inserted into pAcYM1 baculovirus expression vector (17), and recombinant SCV N protein was produced in insect cells (7). Guinea pigs were immunized with sodium dodecyl sulfate-polyacrylamide gel electrophoresis-purified SCV N protein (20 μg/immunization/animal), and N protein-specific antibody titers were determined by indirect immunofluorescence staining in SCV N gene-transfected HuH7 cells (17).
Approximately 2.5 × 106 monocytes from healthy blood donors were allowed to bind to plastic six-well plates (Falcon, Becton Dickinson, Franklin Lakes, NJ) and to differentiate into macrophages or immature DCs (20, 22, 32) using granulocyte-macrophage colony-stimulating factor (GM-CSF) or GM-CSF and interleukin-4 (IL-4), respectively. Human leukocyte IFN-α was obtained from the Finnish Red Cross Blood Transfusion Service, and recombinant human IFN-β (Schering-Plough, Espoo, Finland) and IL-29 (ZymoGenetics, Seattle, WA) were obtained from commercial sources.
For indirect immunofluorescence staining or flow cytometric analysis (FACS), cells were infected with SCV, influenza A, or Sendai viruses, fixed, permeabilized, and treated with 2% fetal bovine serum in phosphate-buffered saline. SCV-infected Vero E6 cells and DCs were stained with guinea pig anti-SCV N protein antibodies followed by secondary fluorescein isothiocyanate-labeled antibodies. Virus-infected DCs were stained with fluorescein isothiocyanate-conjugated anti-CD80, anti-CD83, anti-CD86, anti-HLA-DR, or isotype control antibodies (Caltag Laboratories). Influenza A- or Sendai virus-infected DCs were stained with glycoprotein-specific antibodies (20, 22) and secondary antibodies (Caltag Laboratories). Stained cells were analyzed with FACScan using Cellquest software (Becton Dickinson, San Diego, CA).
Northern blot analysis was done as described previously (4, 8). Hybond-N nylon membranes (Amersham Biosciences, Helsinki, Finland) were hybridized with SCV 3a, SCV N, IFN-α2, IFN-β, IL-28B, and IL-29 (29); tumor necrosis factor alpha (TNF-α), CCL5, and CXCL10 (16); and MxA (23) cDNA probes.
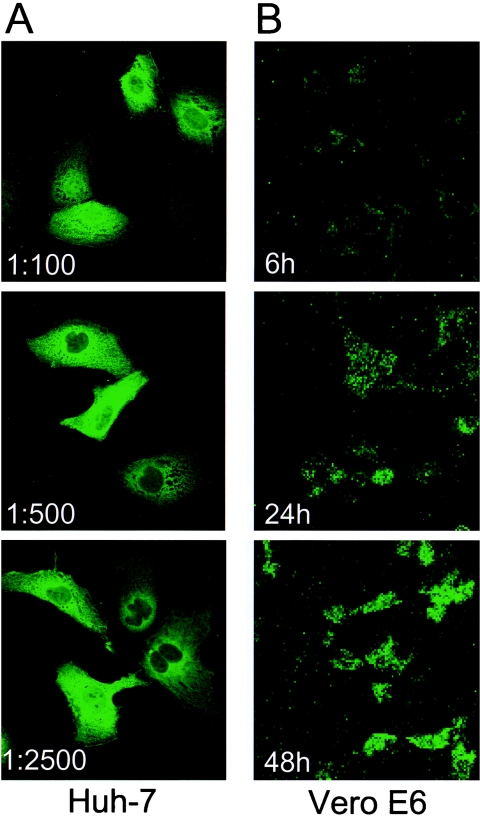
Guinea pig anti-SCV N protein antibodies were highly specific (Fig. 1A), and they were used to study the kinetics of SCV N protein expression in Vero E6 cells, where SCV N protein expression was readily seen at 24 and 48 h after infection (Fig. 1B).
FIG. 1.
Specificity of anti-SCV N protein antibodies and expression of SCV N protein in SCV-infected Vero E6 cells. Guinea pigs were immunized with preparative sodium dodecyl sulfate-polyacrylamide gel electrophoresis-purified SCV N protein, and the specificity and quantity of the antibodies were analyzed by confocal laser microscopy in SCV N gene-transfected HuH7 hepatoma cells. (A) Immunofluorescence staining pattern of guinea pig 3 anti-SCV N antibodies in different dilutions. (B) Immunofluorescence staining pattern of SCV-infected (multiplicity of infection [MOI], 5) Vero E6 cells at 6, 24, and 48 h after infection.
Northern blot analysis of SCV-infected A549 cells revealed SCV 3a and N mRNA-specific signals whose intensity increased from 6 to 24 h after infection (Fig. 2). In A549 cells, SCV N protein expression was not seen even at 5 days after infection (results not shown). IFN-α pretreatment showed some inhibition of SCV mRNA expression 24 h after infection. SCV infection failed to induce IFN-α, IFN-β, IL-28A/B, IL-29, TNF-α, CCL5, CXCL10 (data not shown), or IFN-α/β-induced MxA (Fig. 2) mRNA expression, which is a sensitive marker gene for IFN-α/β (10, 11, 24). IFN-α priming, which provides positive feedback for virus-induced cytokine gene expression (14, 20), did not enhance SCV-induced cytokine mRNA expression in A549 cells (data not shown). Based on Northern blot analysis, SCV-infected DCs expressed SCV N mRNA (Fig. 3A). However, the infection appeared to be self-limiting, since viral mRNA expression was reduced at 24 h of infection. No induction of IFN-α, IFN-β, IL-28A/B, IL-29, TNF-α, CCL5, or CXCL10 mRNAs was seen in SCV-infected DCs (results not shown). MxA mRNA expression was not seen, further suggesting that IFN-α/β was not induced by SCV in DCs. In influenza A or Sendai virus infection, instead, a rapid and strong MxA mRNA expression in DCs was evident (Fig. 3B). Pretreatment of DCs with IFN-α, IFN-β, or IL-29 led to MxA gene induction but not to a detectable reduction in SCV mRNA expression (Fig. 3A) or enhanced cytokine gene expression (data not shown). Also, in macrophages, SCV infection led to the expression of N-specific mRNAs whose expression was not reduced by cytokine pretreatment (Fig. 3C). Like in A549 cells and DCs, SCV failed to induce IFN-α, IFN-β, IL-29, CCL5, or CXCL10 mRNA expression in unprimed or IFN/IL-29-primed macrophages (data not shown), suggesting that SCV does not induce efficient cytokine response in these cells.
FIG. 2.
Expression of SCV mRNA in IFN-α-treated and untreated A549 cells. Untreated or IFN-α-pretreated (100 IU/ml, 24 h) A549 cells were infected with SCV (MOI, 2) for the times indicated. Total cellular RNA was isolated and processed for Northern blot analysis using SCV 3a cDNA (two bands) or T7 RNA polymerase-transcribed SCV N positive-strand-specific cRNA probe (six bands) and host MxA gene-specific random-primed cDNA probe. SCV-specific mRNA species are found especially at 24 h after infection. No IFN-α, IFN-β, IL-28A/B, IL-29, TNF-α, CCL5, or CXCL10 mRNA expression was seen in SCV-infected cells (blots not shown). Ethidium bromide staining for 28S and 18S rRNAs was used to verify equal RNA loading.
FIG. 3.
SCV mRNA is expressed in virus-infected human monocyte-derived dendritic cells and macrophages. Human myeloid DCs (A) or macrophages (C) were infected with SCV (MOIs, 2 and 0.4) for 24 h. Total cellular RNA was isolated and processed for Northern blotting, and the filters were hybridized with SCV N- or host MxA-specific cDNA probes. (B) DCs were also infected with influenza A or Sendai viruses (MOI, 5), cells were collected at the times indicated, total cellular RNA was isolated, and Northern blot analysis was carried out with MxA cDNA. Ethidium bromide staining for 28S and 18S rRNAs was used to verify equal RNA loading.
In spite of clearly detectable expression of SCV-specific subgenomic mRNAs (Fig. 3A), FACS analysis of SCV-infected DCs revealed a complete lack of SCV N protein expression and a lack of enhancement of HLA-DR expression. (Fig. 4A). Similarly, SCV infection failed to induce DC maturation marker CD86, the expression of which was readily enhanced by influenza A and Sendai viruses (Fig. 4B). The latter two viruses replicated well in DCs (Fig. 4C).
FIG. 4.
SCV-infected myeloid DCs fail to express SCV N protein and enhance HLA class II and CD86 expression. Monocyte-derived human DCs were infected with SCV (MOI, 5) followed by fixing of the cells for FACS analysis at different time points after the infection. (A) Cells were permeabilized with 0.1% Triton X-100 (for SCV N protein staining) or left nonpermeabilized (HLA class II staining) and stained with guinea pig anti-SCV N protein antibodies (1:500 dilution) or anti-HLA-DR antibodies. FACS profiles of SCV N protein-stained uninfected and SCV-infected cells are shown in the left panels. The dotted lines represent the cutoff for positive protein expression. FACS profiles of HLA class II DR expression in SCV-infected and control cells are shown in the right panels. The dotted lines represent the geometric mean fluorescence value (20) of uninfected control cells at 6 h. (B) CD86 expression in SCV-, influenza A-, and Sendai virus-infected DCs. Human monocyte-derived DCs were infected with SCV, influenza A H3N2, or Sendai virus (MOI, 5). Cells were fixed at the times indicated and stained for cell surface expression of CD86. SCV failed to induce significant expression of CD86, whereas influenza A virus induced moderate and Sendai virus full DC maturation. The dotted lines represent the geometric mean fluorescence intensities of the uninfected control cells at 6 h. (C) Influenza A- and Sendai virus-infected DCs were stained for cell surface expression of viral glycoproteins. Virtually all influenza A- or Sendai virus-infected DCs were positive for viral glycoprotein staining.
Here we show that SCV can internalize A549 cells, monocyte-derived macrophages, and DCs, since SCV-specific subgenomic mRNAs were expressed. However, the infection was not productive, since SCV (N) protein expression was not taking place. Our results are well in line with those of others (3, 31, 33), who also observed uptake but not efficient replication of SCV in DCs or in A549 cells. The failure of SCV to induce cytokine gene expression in these cell types is likely due to the lack of efficient SCV replication, since the activation of IFN/cytokine gene expression requires virus replication, which triggers the activation of IKKe/TBK1-IRF3/IRF7 and NF-κB signal transduction pathways leading to enhanced IFN/cytokine gene expression.
Contact with bacteria or virus infection stimulates DC maturation, expression of CD80, CD83, CD86, and major histocompatibility complex class II, and the production of proinflammatory cytokines (1, 6, 32). While influenza A and Sendai viruses replicated well in DCs and stimulated the expression of CD86, SCV-infected DCs failed to show enhanced CD86 or HLA class II expression. SCV infection in DCs was also not able to induce IFN-α/β, IL-28A/B, IL-29, TNF-α, CCL5, or CXCL10 gene expression. These genes are readily turned on by infection of DCs with other viruses (1, 6, 12, 16, 20, 28). Indirect evidence for the lack of IFN-α/β production was obtained from the inability of SCV to turn on MxA gene expression. The MxA gene is specifically and sensitively (<1 IU/ml) under the regulation of IFN-α/β (23, 24). It is likely that the inability of SCV to induce cytokine gene expression in human myeloid DCs is due to the abortive nature of SCV infection in these cells.
In Vero E6 cells and macaque type 1 pneumocytes, IFN-α/β has activity against SCV. However, relatively high doses (1,000 IU/ml or higher) of IFN-α/β were required for significant inhibition of SCV replication (5, 9). Other antiviral proteins apart from MxA are likely to be involved in this process (5, 9). Although we used lower IFN-α pretreatment doses (100 IU/ml), some inhibition of SCV mRNA expression was seen in A549 cells but not in DCs or macrophages (Fig. 2 and 3), further supporting the idea that SCV is relatively insensitive to the antiviral effects of IFN-α/β (and IL-29).
Our observations demonstrate that human primary macrophages and DCs are susceptible to SCV. Although early SCV mRNA expression appears to take place, the infection is self-limiting and no evidence for viral protein expression is seen. SCV also completely failed to induce host cell cytokine response. This strongly suggests that macrophages and DCs are not efficiently activated by SCV, which may lead to weak host cell antiviral response and slow initiation of cytokine-mediated adaptive immune responses.
Acknowledgments
We thank Mika Salminen for expert help in the use of the Institute's BSL-3 facilities and Tapani Hovi for critical review of the manuscript.
Financial support for this study was received from the Medical Research Council of the Academy of Finland, the Sigrid Jusélius Foundation, and the Finnish Department of Social Welfare and Health.
REFERENCES
- 1.Cella, M., M. Salio, Y. Sakakibara, H. Langen, I. Julkunen, and A. Lanzavecchia. 1999. Maturation, activation, and protection of dendritic cells induced by double-stranded RNA. J. Exp. Med. 189:821-829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cheung, C. Y., L. L. Poon, A. S. Lau, W. Luk, Y. L. Lau, K. F. Shortridge, S. Gordon, Y. Guan, and J. S. Peiris. 2002. Induction of proinflammatory cytokines in human macrophages by influenza A (H5N1) viruses: a mechanism for the unusual severity of human disease? Lancet 360:1831-1837. [DOI] [PubMed] [Google Scholar]
- 3.Cheung, C. Y., L. L. Poon, I. H. Ng, W. Luk, S. F. Sia, M. H. Wu, K. H. Chan, K. Y. Yuen, S. Gordon, Y. Guan, and J. S. Peiris. 2005. Cytokine responses in severe acute respiratory syndrome coronavirus-infected macrophages in vitro: possible relevance to pathogenesis. J. Virol. 79:7819-7826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chirgwin, J. M., A. E. Przybyla, R. J. MacDonald, and W. J. Rutter. 1979. Isolation of biologically active ribonucleic acid from sources enriched in ribonuclease. Biochemistry 18:5294-5299. [DOI] [PubMed] [Google Scholar]
- 5.Cinatl, J., B. Morgenstern, G. Bauer, P. Chandra, H. Rabenau, and H. W. Doerr. 2003. Treatment of SARS with human interferons. Lancet 362:293-294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coccia, E. M., M. Severa, E. Giacomini, D. Monneron, M. E. Remoli, I. Julkunen, M. Cella, R. Lande, and G. Uze. 2004. Viral infection and Toll-like receptor agonists induce a differential expression of type I and lambda interferons in human plasmacytoid and monocyte-derived dendritic cells. Eur. J. Immunol. 34:796-805. [DOI] [PubMed] [Google Scholar]
- 7.Fagerlund, R., K. Melen, L. Kinnunen, and I. Julkunen. 2002. Arginine/lysine-rich nuclear localization signals mediate interactions between dimeric STATs and importin alpha 5. J. Biol. Chem. 277:30072-30078. [DOI] [PubMed] [Google Scholar]
- 8.Glisin, V., R. Crkvenjakov, and C. Byus. 1974. Ribonucleic acid isolated by cesium chloride centrifugation. Biochemistry 13:2633-2637. [DOI] [PubMed] [Google Scholar]
- 9.Haagmans, B. L., T. Kuiken, B. E. Martina, R. A. Fouchier, G. F. Rimmelzwaan, G. van Amerongen, D. van Riel, T. de Jong, S. Itamura, K. H. Chan, M. Tashiro, and A. D. Osterhaus. 2004. Pegylated interferon-alpha protects type 1 pneumocytes against SARS coronavirus infection in macaques. Nat. Med. 10:290-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Helin, E., R. Vainionpaa, T. Hyypia, I. Julkunen, and S. Matikainen. 2001. Measles virus activates NF-kappa B and STAT transcription factors and production of IFN-alpha/beta and IL-6 in the human lung epithelial cell line A549. Virology 290:1-10. [DOI] [PubMed] [Google Scholar]
- 11.Kim, M. J., A. G. Latham, and R. M. Krug. 2002. Human influenza viruses activate an interferon-independent transcription of cellular antiviral genes: outcome with influenza A virus is unique. Proc. Natl. Acad. Sci. USA 99:10096-10101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kotenko, S. V., G. Gallagher, V. V. Baurin, A. Lewis-Antes, M. Shen, N. K. Shah, J. A. Langer, F. Sheikh, H. Dickensheets, and R. P. Donnelly. 2003. IFN-lambdas mediate antiviral protection through a distinct class II cytokine receptor complex. Nat. Immunol. 4:69-77. [DOI] [PubMed] [Google Scholar]
- 13.Ksiazek, T. G., D. Erdman, C. S. Goldsmith, S. R. Zaki, T. Peret, S. Emery, S. Tong, C. Urbani, J. A. Comer, W. Lim, P. E. Rollin, S. F. Dowell, A. E. Ling, C. D. Humphrey, W. J. Shieh, J. Guarner, C. D. Paddock, P. Rota, B. Fields, J. DeRisi, J. Y. Yang, N. Cox, J. M. Hughes, J. W. LeDuc, W. J. Bellini, and L. J. Anderson. 2003. A novel coronavirus associated with severe acute respiratory syndrome. N. Engl. J. Med. 348:1953-1966. [DOI] [PubMed] [Google Scholar]
- 14.Marie, I., J. E. Durbin, and D. E. Levy. 1998. Differential viral induction of distinct interferon-alpha genes by positive feedback through interferon regulatory factor-7. EMBO J. 17:6660-6669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marra, M. A., S. J. Jones, C. R. Astell, R. A. Holt, A. Brooks-Wilson, Y. S. Butterfield, J. Khattra, J. K. Asano, S. A. Barber, S. Y. Chan, A. Cloutier, S. M. Coughlin, D. Freeman, N. Girn, O. L. Griffith, S. R. Leach, M. Mayo, H. McDonald, S. B. Montgomery, P. K. Pandoh, A. S. Petrescu, A. G. Robertson, J. E. Schein, A. Siddiqui, D. E. Smailus, J. M. Stott, G. S. Yang, F. Plummer, A. Andonov, H. Artsob, N. Bastien, K. Bernard, T. F. Booth, D. Bowness, M. Czub, M. Drebot, L. Fernando, R. Flick, M. Garbutt, M. Gray, A. Grolla, S. Jones, H. Feldmann, A. Meyers, A. Kabani, Y. Li, S. Normand, U. Stroher, G. A. Tipples, S. Tyler, R. Vogrig, D. Ward, B. Watson, R. C. Brunham, M. Krajden, M. Petric, D. M. Skowronski, C. Upton, and R. L. Roper. 2003. The genome sequence of the SARS-associated coronavirus. Science 300:1399-1404. [DOI] [PubMed] [Google Scholar]
- 16.Matikainen, S., J. Pirhonen, M. Miettinen, A. Lehtonen, C. Govenius-Vintola, T. Sareneva, and I. Julkunen. 2000. Influenza A and sendai viruses induce differential chemokine gene expression and transcription factor activation in human macrophages. Virology 276:138-147. [DOI] [PubMed] [Google Scholar]
- 17.Melen, K., R. Fagerlund, J. Franke, M. Kohler, L. Kinnunen, and I. Julkunen. 2003. Importin alpha nuclear localization signal binding sites for STAT1, STAT2, and influenza A virus nucleoprotein. J. Biol. Chem. 278:28193-28200. [DOI] [PubMed] [Google Scholar]
- 18.Nakabayashi, H., K. Taketa, K. Miyano, T. Yamane, and J. Sato. 1982. Growth of human hepatoma cells lines [sic] with differentiated functions in chemically defined medium. Cancer Res. 42:3858-3863. [PubMed] [Google Scholar]
- 19.Ng, M. L., S. H. Tan, E. E. See, E. E. Ooi, and A. E. Ling. 2003. Proliferative growth of SARS coronavirus in Vero E6 cells. J. Gen. Virol. 84:3291-3303. [DOI] [PubMed] [Google Scholar]
- 20.Österlund, P., V. Veckman, J. Sirén, K. M. Klucher, J. Hiscott, S. Matikainen, and I. Julkunen. 2005. Gene expression and antiviral activity of alpha/beta interferons and interleukin-29 in virus-infected human myeloid dendritic cells. J. Virol. 79:9608-9617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peiris, J. S., S. T. Lai, L. L. Poon, Y. Guan, L. Y. Yam, W. Lim, J. Nicholls, W. K. Yee, W. W. Yan, M. T. Cheung, V. C. Cheng, K. H. Chan, D. N. Tsang, R. W. Yung, T. K. Ng, and K. Y. Yuen. 2003. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet 361:1319-1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pirhonen, J., T. Sareneva, M. Kurimoto, I. Julkunen, and S. Matikainen. 1999. Virus infection activates IL-1 beta and IL-18 production in human macrophages by a caspase-1-dependent pathway. J. Immunol. 162:7322-7329. [PubMed] [Google Scholar]
- 23.Ronni, T., S. Matikainen, A. Lehtonen, J. Palvimo, J. Dellis, F. Van Eylen, J. F. Goetschy, M. Horisberger, J. Content, and I. Julkunen. 1998. The proximal interferon-stimulated response elements are essential for interferon responsiveness: a promoter analysis of the antiviral MxA gene. J. Interferon Cytokine Res. 18:773-781. [DOI] [PubMed] [Google Scholar]
- 24.Ronni, T., S. Matikainen, T. Sareneva, K. Melen, J. Pirhonen, P. Keskinen, and I. Julkunen. 1997. Regulation of IFN-alpha/beta, MxA, 2′,5′-oligoadenylate synthetase, and HLA gene expression in influenza A-infected human lung epithelial cells. J. Immunol. 158:2363-2374. [PubMed] [Google Scholar]
- 25.Ronni, T., T. Sareneva, J. Pirhonen, and I. Julkunen. 1995. Activation of IFN-alpha, IFN-gamma, MxA, and IFN regulatory factor 1 genes in influenza A virus-infected human peripheral blood mononuclear cells. J. Immunol. 154:2764-2774. [PubMed] [Google Scholar]
- 26.Rota, P. A., M. S. Oberste, S. S. Monroe, W. A. Nix, R. Campagnoli, J. P. Icenogle, S. Penaranda, B. Bankamp, K. Maher, M. H. Chen, S. Tong, A. Tamin, L. Lowe, M. Frace, J. L. DeRisi, Q. Chen, D. Wang, D. D. Erdman, T. C. Peret, C. Burns, T. G. Ksiazek, P. E. Rollin, A. Sanchez, S. Liffick, B. Holloway, J. Limor, K. McCaustland, M. Olsen-Rasmussen, R. Fouchier, S. Gunther, A. D. Osterhaus, C. Drosten, M. A. Pallansch, L. J. Anderson, and W. J. Bellini. 2003. Characterization of a novel coronavirus associated with severe acute respiratory syndrome. Science 300:1394-1399. [DOI] [PubMed] [Google Scholar]
- 27.Seo, S. H., E. Hoffmann, and R. G. Webster. 2002. Lethal H5N1 influenza viruses escape host anti-viral cytokine responses. Nat. Med. 8:950-954. [DOI] [PubMed] [Google Scholar]
- 28.Sheppard, P., W. Kindsvogel, W. Xu, K. Henderson, S. Schlutsmeyer, T. E. Whitmore, R. Kuestner, U. Garrigues, C. Birks, J. Roraback, C. Ostrander, D. Dong, J. Shin, S. Presnell, B. Fox, B. Haldeman, E. Cooper, D. Taft, T. Gilbert, F. J. Grant, M. Tackett, W. Krivan, G. McKnight, C. Clegg, D. Foster, and K. M. Klucher. 2003. IL-28, IL-29 and their class II cytokine receptor IL-28R. Nat. Immunol. 4:63-68. [DOI] [PubMed] [Google Scholar]
- 29.Siren, J., J. Pirhonen, I. Julkunen, and S. Matikainen. 2005. IFN-alpha regulates TLR-dependent gene expression of IFN-alpha, IFN-beta, IL-28, and IL-29. J. Immunol. 174:1932-1937. [DOI] [PubMed] [Google Scholar]
- 30.Stroher, U., A. DiCaro, Y. Li, J. E. Strong, F. Aoki, F. Plummer, S. M. Jones, and H. Feldmann. 2004. Severe acute respiratory syndrome-related coronavirus is inhibited by interferon-alpha. J. Infect. Dis. 189:1164-1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tseng, C. T., L. A. Perrone, H. Zhu, S. Makino, and C. J. Peters. 2005. Severe acute respiratory syndrome and the innate immune responses: modulation of effector cell function without productive infection. J. Immunol. 174:7977-7985. [DOI] [PubMed] [Google Scholar]
- 32.Veckman, V., M. Miettinen, J. Pirhonen, J. Sirén, S. Matikainen, S. Matikainen, and I. Julkunen. 2004. Streptococcus pyogenes and Lactobacillus rhamnosus differentially induce maturation and production of Th1-type cytokines and chemokines in human monocyte-derived dendritic cells. J. Leukoc. Biol. 75:764-771. [DOI] [PubMed] [Google Scholar]
- 33.Yang, Z.-Y., Y. Huang, L. Ganesh, K. Leung, W.-P. Kong, O. Schwartz, K. Subbarao, and G. J. Nabel. 2004. pH-dependent entry of severe acute respiratory syndrome coronavirus is mediated by the spike glycoprotein and enhanced by dendritic cell transfer through DC-SIGN. J. Virol. 78:5642-5650. [DOI] [PMC free article] [PubMed] [Google Scholar]