Abstract
Objective
To assess the effects of web-based care management on glucose and blood pressure control over 12 months in patients with poorly controlled diabetes mellitus.
Research Design and Methods
104 patients with diabetes mellitus and hemoglobin A1c ≥ 9.0% who received their care at a VA medical center were recruited. All participants completed a diabetes education class and were randomized to continue with usual care (n = 52) or receive web-based care management (n = 52). The care management group received a notebook computer, glucose and blood pressure monitoring devices and access to a care management website. The website provided educational modules, accepted uploads from monitoring devices, and had an internal messaging system for patients to communicate with the care manager.
Results
Participants receiving web-based care management had lower hemoglobin A1c over 12 months (P<0.05) when compared to education and usual care. Persistent website users had greater improvement in hemoglobin A1c when compared to intermittent users (−1.9% vs. −1.2%, P=0.051) or education and usual care (−1.4%, P<0.05). Greater numbers of website data uploads were associated with larger declines in hemoglobin A1c (highest tertile −2.1%, lowest tertile: −1.0%, P<0.02). Hypertensive participants in the web-based care management group had a greater reduction in systolic blood pressure (P<0.01). HDL cholesterol rose and triglycerides fell in the web-based care management group (P<0.05).
Conclusions
Web-based care management may be a useful adjunct in the care of patients with poorly controlled diabetes mellitus.
Diabetes care is facilitated by engagement of patients in a self-management program with the advice and counsel of physicians and allied health professionals (1). Care-management has been advocated in patients with diabetes as a means of facilitating easier, time-efficient communication between clinicians and patients with the goal of improving care and reducing healthcare expenditures.
Healthcare systems have adopted care management for individuals with high-risk diseases and particularly patients with diabetes mellitus (2–5). Scheduling and/or travel may be barriers to engagement with a care provider, limiting uptake and resulting in a failure to maximize the potential health-gains (6). Care management has been studied in patients with diabetes but results have been mixed; some have noted significant improvement in HbA1c (7–9) but a recent study found no effect (10).
Patients are accessing medical content on the Internet with increasing frequency (11–14). In a survey of patients in a primary care practice, 54% reported using the Internet for medical information and 60% felt that the information was the same or better than what they received from their doctors (11). Few studies have examined the effects of web-based interventions that provide an interactive component, that is, delivering content as well as feedback to participants (15–17). Our goal was to test the hypothesis that diabetes care management using a web-based system in individuals with poorly controlled diabetes mellitus would result in significant and sustained improvement in HbA1c and blood pressure.
Research Design and Methods
Study participants
The study was conducted at the Veteran’s Affairs (VA) Boston Healthcare System. The protocol was reviewed and approved by the institutional review board and informed, written consent was obtained from each participant. Eligibility criteria included HbA1c ≥9.0%, age >18 years, ability to understand written and spoken English, and willingness to use a notebook computer, glucose and blood pressure monitoring devices. Participants were required to have a VA-based primary care provider at one of 4 hospital-based clinics or 10 community-based outpatient clinics, and access to a telephone.
Hospital laboratory data were screened monthly for individuals with an HbA1c ≥ 8.8%. Potential participants were sent a letter and/or brochure describing the study and a follow-up telephone call was attempted at least 2 weeks later to solicit participation. In-person screening was provided to interested and potentially eligible subjects between October 2001 and April 2003 (Figure 1). Reasons for non-participation were provided by 353 of the 684 individuals who declined to participate after being reached by phone, and included lack of interest (30%), transportation challenges (25%), poor health (20%), scheduling (9%), and other (16%).
Figure 1.
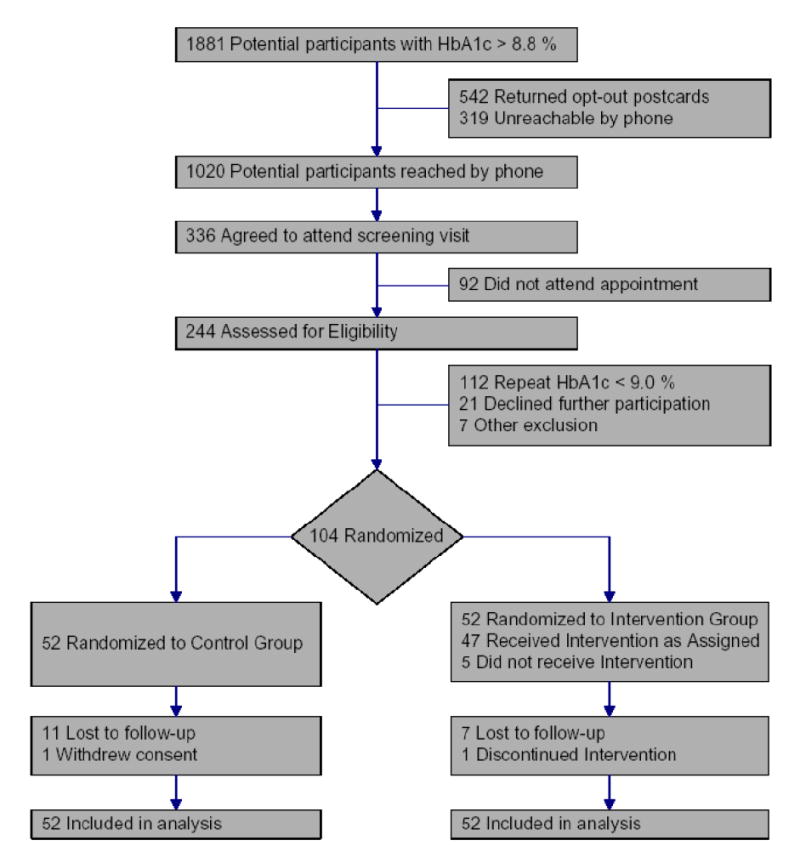
CONSORT diagram of participant flow through the study.
Study Protocol
Eligible participants attended a half-day self-management education session for instruction in diabetes core-content areas as recommended by the American Diabetes Association (18). They met with a nurse, nutritionist and pharmacist, all of whom were certified diabetes educators. Participants were then randomized to one of two study groups through use of a random variables generator and a series of sealed envelopes.
Usual Care
Those randomized to usual care continued with ongoing care by their primary care provider as needed. Study staff had contact with these participants only to arrange follow-up visits for outcome measures.
Web-based care management
Participants randomized to web-based care management also continued with their usual care but additionally received a notebook computer (HP Omnibook, 700 mHz, 128 RAM, running Internet Explorer 5.50), a glucose meter (Accucheck Advantage™, Roche Diagnostics) and a blood pressure monitor (HEM-747-IC IntelliSense™ Automatic BPM, Omron Medical, North Bend, WA). The notebook computer was programmed to connect to a diabetes education and management website (see below) using complimentary toll-free dial-up Internet access. Computer training and support was provided by one of the study staff (S.H.H.) for a mean total of 2.3 hours [range 1.0–6.6 hours] per subject. Home blood pressure monitoring was encouraged at least 3 times weekly; recommendations for home glucose testing were individualized for each patient.
The MyCareTeam™ website (https://mycareteam.georgetown.edu/vaboston) was designed and hosted at the Imaging Science and Information Systems Center at Georgetown University Medical Center. Participants used coded identifiers when interacting with the website, which was accessed using secure socket layer encryption via secure http (i.e. https) to ensure the confidentiality of data transfer. The website accepted uploads from blood pressure and glucose monitoring devices and displayed these data in graphic and tabular form for the participant and care manager to review. An internal messaging system allowed participants to send and receive secure messages to and from the care manager via the website. The care manager responded to queries within one working day during office hours. The website contained web-enabled diabetes educational modules and had links to other web-based diabetes resources. Participants that did not login to the website during a 2 week period were contacted by a study coordinator by telephone to encourage website usage.
An advanced practice nurse and certified diabetes educator (H.E.G.) reviewed participant data from the website and, using treatment algorithms for glucose and hypertension management, provided recommendations to the primary care provider and participants. The care manager and primary care providers communicated predominantly via the hospital email system; the physician entered medication changes suggested by the care manager directly into the pharmacy’s electronic ordering system. The care manager and participants had contact through the website’s internal messaging system and occasionally through telephone contact.
Outcome measures
The primary outcome measures were HbA1c, systolic and diastolic blood pressure. Measurements were collected at baseline, 3, 6, 9 and 12 months after randomization. For measurement of HbA1c, the hemoglobin components were separated using HPLC with measurement of the six fractions of hemoglobin, including the HbA1c component (Tosoh Bioscience, Inc., South San Francisco, CA). Blood pressure was measured in the seated position after 5 minutes rest with the same automatic blood pressure device used by study participants. Two readings were taken 1 min apart and the average of the readings was recorded. Hypertension was defined as a systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg measured at baseline. Secondary outcome measures (fasting triglycerides, LDL and HDL cholesterol) were obtained at baseline and 12 months and measured with standard laboratory techniques. Research staff recording outcome measures were not masked to study group assignment.
The protocol pre-specified an evaluation of outcomes in the web-based care management group based on the frequency and persistence of website interactions. During the study, website logins and data uploads were counted and time stamped. The number of data uploads over the 12 months of follow-up was separated into tertiles representing medians of 1, 18, and 31 uploads. Persistence with the web-based care management over time was assessed by defining individuals as “Persistent users,” those who had at least one website login every 3 months (n = 30), and “Intermittent users” (n = 22), who had intervals > 3 months during the study when no website logins were recorded.
Statistical Analyses
A sample size of 50 participants in each group was determined to have 80% power (alpha = 0.05) to detect a between group difference of 0.8% for HbA1c, 6 mm Hg for systolic blood pressure and 5 mm Hg for diastolic blood pressure. Categorical data are presented as percentages and continuous data are presented as means ± SD unless otherwise noted. All analyses compared subjects according to their status at randomization and were conducted in an intention-to-treat manner, with the last value carried forward for missing data. Baseline characteristics were compared using the chi-squared analysis for categorical variables, and the independent groups’ t-test for continuous variables. Differences between baseline and follow-up for continuous variables were assessed using a mixed linear model incorporating the grouping variable (i.e. randomization or persistence group) as a fixed effect and repeated measures analysis to specify covariance structures for repeated measurements on subjects over time. All tests were two-tailed. For all analyses, an alpha of 0.05 was used to define statistical significance. Statistical analysis was performed using SAS version 8.02 (SAS Institute, Cary, NC).
Results
Baseline characteristics of the 104 randomized participants divided by study group are presented in Table 1. The mean age was 63 years; nearly all were males. More than half of the study participants had attended college; approximately one-third had prior Internet access.
Table 1.
Baseline Characteristics
| Parameter | Web-based care management (n = 52) | Usual Care (n = 52) |
|---|---|---|
| Age (years) | 64 ± 7 | 63 ± 7 |
| Sex (% male) | 99% | 100% |
| BMI (kg/m2) | 32.3 ± 5.6 | 34.1 ± 7.0 |
| Education | ||
| College or above | 59% | 67% |
| High school graduate | 22% | 19% |
| Some high school | 12% | 6% |
| Below high school | 6% | 2% |
| Prior Internet access | 31% | 27% |
| Duration of Diabetes (years) | 12.4 | 12.2 |
| Diabetes Medication (n,%) | ||
| Oral medication only | 27 (52%) | 26 (50%) |
| Insulin | 25 (48%) | 26 (50%) |
| HbA1c (mean %) | 10.0 ± 0.8 | 9.9 ± 0.8 |
| Blood Pressure (mm Hg) | ||
| Systolic | 141 ± 21 | 139 ± 20 |
| Diastolic | 81± 7 | 80 ± 7 |
| Lipids (mg/dl) | ||
| LDL cholesterol | 100 ± 35 | 97 ± 21 |
| HDL cholesterol | 43 ± 14 | 40 ± 8 |
| Triglycerides | 178 ± 112 | 204 ± 140 |
Changes in HbA1c
There was a significant decrease in HbA1c compared to baseline in both groups (P< 0.001) at all serial points of measurement (Figure 2). There was a greater decline in HbA1c over time in the web-based care management group when compared to the education and usual care group (P<0.05). At one year, the reduction from baseline in HbA1c was −1.2 ± 1.4% in the education and usual care group and −1.6 ± 1.4% in the web-based care management group.
Figure 2.
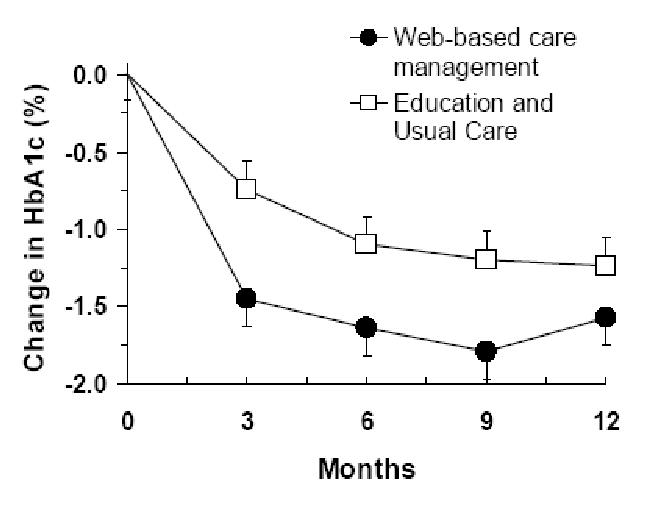
Changes in HbA1c over 12 months in the education and usual care and web-based care management groups. Participants in the web-based care management group had significantly greater change in HbA1c over time (P<0.05) when compared to the education and usual care group. Data shown are mean ± SE
Individuals who had greater adherence with the intervention had more improvement in HbA1c. Participants in the web-based care management group who had more data uploads or regular website interactions had greater improvements in HbA1c. Persistent users tended to have a greater change in HbA1c when compared to Intermittent users (−1.9 ± 1.2% vs. −1.2 ± 1.4%, P=0.051) or to the education and usual care group (P<0.05) that persisted over time (Figure 3A). Similarly, there was a progressive decline in HbA1c with increasing number of website data uploads (Figure 3B). Those in the highest tertile for data uploads had a significantly greater decline in HbA1c than those in the lowest tertile (−2.1 ± 1.1% vs. −1.1 ± 1.7%, P<0.05). Persistent and Intermittent users and those who had greater or fewer data uploads did not differ with regard to baseline demographic and biochemical parameters.
Figure 3.
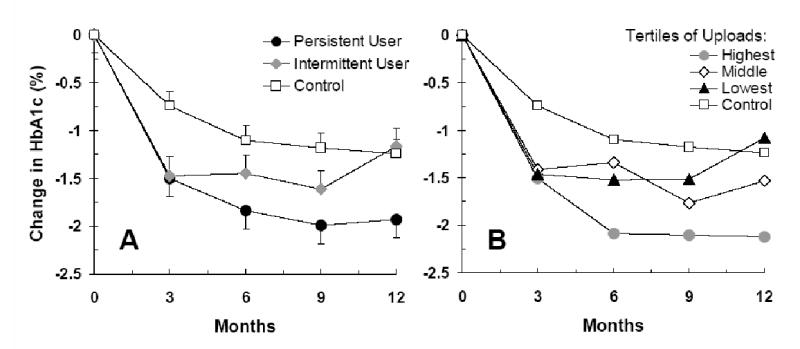
Effects of engagement with web-based care management and outcome.
A: Changes in HbA1c in the web-based care management group who were Persistent and Intermittent users in comparison to the education and usual care group. Persistent users had a substantially greater fall in HbA1c in comparison to Intermittent users and a significantly greater effect versus those receiving education and usual care. Data shown are mean ± SE.
B: Changes in HbA1c in the web-based care management group by tertiles of website data uploads during the study. (Median number of uploads for each tertile: Lowest = 1 upload; Middle = 18 uploads; Highest = 31 uploads.) Greater numbers of data uploads were associated with larger declines in HbA1c.
Similar numbers of participants in each group experienced severe hypoglycemia during the study, which was defined as an episode of hypoglycemia that required assistance from another person (web-based care management: 46 events in 13 participants [median: 3 per participant]; education and usual care: 33 events in 11 participants [median: 2 per participant]).
Changes in blood pressure
Treatment for hypertension was targeted by the web-based care management intervention. Hypertensive participants in the web-based care management group (n = 37) had a significantly greater decline in systolic blood pressure after 12 months when compared to the education and usual care group (n = 35) (web-based care management: -10 ± 17 mm Hg; education and usual care: −7 ± 21 mm Hg, P<0.01). Diastolic blood pressure declined similarly in both groups (web-based care management: −5 ± 13 mm Hg, P= 0.053 vs. baseline; education and usual care: −6 ± 11 mm Hg, P=0.058 vs. baseline). The frequency of website logins or data uploads was not a predictor for change in blood pressure over time. At the end of the trial there were fewer hypertensive participants in the web-based care management group (n = 28) then in the education and usual care group (n = 37).
Changes in lipid profiles
LDL cholesterol was analyzed as a secondary endpoint and did not change in either group (web-based care management: −6 ± 12 mg/dl; education and usual care: −5 ± 11 mg/dl). However, web-based care management was associated with a significant increase in HDL cholesterol (3 ± 6 mg/dl; P<0.05 vs. baseline) and a significant decrease in triglyceride levels (−38 ± 99 mg/dl; P<0.01 vs. baseline) which did not change in the education and usual care group (1 ± 6 mg/dl and −2 ± 60 mg/dl, respectively).
Conclusions
More than most chronic diseases, diabetes mellitus often requires behavioral and medication changes supported by frequent feedback and support from care providers. We and others have previously shown that self-management education alone can result in significant improvement in HbA1c in patients with poorly controlled diabetes mellitus (19–21). In this study we used broad eligibility criteria to produce potentially generalizable findings. Most of our study participants had no prior computer experience and/or Internet access. Among these subjects with elevated HbA1c, self-management education coupled with internet access, technology training, and web-based care management resulted in significant improvements in HbA1c over 12 months when compared to education and usual care. Individuals who persisted with website usage and regular data uploads were more likely to achieve and maintain reductions in HbA1c. Additional improvements were seen in lipid profiles and systolic blood pressure in hypertensive participants. Thus, these findings support a role for web-based care management in patients with elevated HbA1c as a tool to improve diabetes care.
Several factors should be considered in interpreting the results of this feasibility study. Not every clinical practice setting has access to a care manager with similar training and experience, although such allied health professionals are likely to be increasingly prevalent. We were able to provide Internet access and computer training to study participants: this may not be available to some patients. There was a low prevalence of women recruited by this study, reflecting the relatively smaller number of women cared for in the VA healthcare system. Prior studies (7,8) with more balanced enrollment of men and women receiving care management showed similar outcomes between men and women. The study question necessitated an open-label design which may be subject to the Hawthorne effect and confounding. That degree of improvement in HbA1c correlated with interactivity with the website could reflect the underlying change in motivation of the participants rather than utilization of the care program per se. Consequently, though the evidence linking utilization and outcome is noteworthy, the mechanism through which the care management program achieved its success remains speculative.
There was significant improvement in HbA1c among those randomized to education and usual care. The VA healthcare system has progressively improved its diabetes care program through a series of successful initiatives (22, 23). Additionally, the laboratory results obtained for this study were available on the VA electronic medical record and could have resulted in targeted care that might not have been offered in its absence.
Care management has been embraced for patients with high risk/high cost medical conditions such as diabetes with claims of significant cost savings (2,3). However, the cost-effectiveness of care management in diabetes is still a matter of debate. Indeed, an analysis of potential interventions in patients with diabetes concluded that care management has unclear economic impact (24). Nevertheless, care management has been recommended by the Task Force on Community Preventive Services from the Centers for Disease Control and Prevention (25). While a detailed economic analysis is clearly warranted, our study shows the effectiveness of such an approach, particularly among individuals interested in engaging with the technology.
The Internet has clearly become the gateway to limitless health information (11–14). However, few studies have evaluated the clinical benefit of using web-based education and/or healthcare provider feedback. Access to an interactive asthma education website resulted in a significant increase in asthma knowledge and reduced numbers of symptom-days, ER visits, and inhaled corticosteroid doses (26). In a trial linking web-based education with health care provider feedback, overweight and obese adults randomized to either web-based behavioral counseling vs. basic Internet access achieved significantly greater weight loss when receiving web-based provider feedback intervention (15).
Major advantages of a web-based care management program are the ability to post professionally vetted material on secure websites, offer 24 hour accessibility, and be available to individuals in their home without regard to the distance from their site of healthcare. Our results support the development and greater study of this increasingly ubiquitous portal in the management of patients. Patients with poorly controlled diabetes who adopt such a system and regularly exchange information with their healthcare providers are likely to derive important clinical benefits.
Acknowledgments
The authors express their gratitude to Nancy Fraser, Ann Marie Leikauskas and Fang Fang, M.S.
The views expressed in this article are those of the authors and do not necessarily reflect the position and policy of the United States Federal Government, the Department of Veterans Affairs or the Department of Defense. No official endorsement should be inferred. This project was supported by grants from the Department of the Army Cooperative Agreement # DAMD 17-98-2-8017, Department of Veterans Affairs- Health Services Research and Development Program (TEL-02-100) and NIH K24-DK06321.
References
- 1.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288:2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 2.Steffens B. Cost-effective management of type 2 diabetes: providing quality care in a cost-constrained environment. Am J Manag Care. 2000;6:S697–703. [PubMed] [Google Scholar]
- 3.Sidorov J, Shull R, Tomcavage J, Girolami S, Lawton N, Harris R. Does diabetes disease management save money and improve outcomes? A report of simultaneous short-term savings and quality improvement associated with a health maintenance organization-sponsored disease management program among patients fulfilling health employer data and information set criteria. Diabetes Care. 2002;25:684–689. doi: 10.2337/diacare.25.4.684. [DOI] [PubMed] [Google Scholar]
- 4.Genrich SJ, Neatherlin JS. Case manager role. A content analysis of published literature. Care Manag J. 2001;3:14–19. [PubMed] [Google Scholar]
- 5.Petryshen PR, Petryshen PM. The Case Management Model: an innovative approach to the delivery of patient care. J Adv Nurs. 1992;17:1188–1194. doi: 10.1111/j.1365-2648.1992.tb01834.x. [DOI] [PubMed] [Google Scholar]
- 6.Karter AJ, Parker MM, Moffet HH, et al. Missed appointments and poor glycemic control: an opportunity to identify high-risk diabetic patients. Med Care. 2004;42:110–115. doi: 10.1097/01.mlr.0000109023.64650.73. [DOI] [PubMed] [Google Scholar]
- 7.Taylor CB, Miller NH, Reilly KR, et al. Evaluation of a nurse-care management system to improve outcomes in patients with complicated diabetes. Diabetes Care. 2003;26:1058–1063. doi: 10.2337/diacare.26.4.1058. [DOI] [PubMed] [Google Scholar]
- 8.Aubert RE, Herman WH, Waters J, et al. Nurse case management to improve glycemic control in diabetic patients in a health maintenance organization. A randomized controlled study Ann Int Med. 1998;129:605–612. doi: 10.7326/0003-4819-129-8-199810150-00004. [DOI] [PubMed] [Google Scholar]
- 9.Piette JD, Weinberger M, Kraemer FB, McPhee SJ. Impact of automated calls with nurse follow-up on diabetes treatment outcomes in a Department of Veterans Affairs Health Care System: a randomized controlled trial. Diabetes Care. 2001;24:202–208. doi: 10.2337/diacare.24.2.202. [DOI] [PubMed] [Google Scholar]
- 10.Krein SL, Klamerus ML, Vijan S, et al. Case management for patients with poorly controlled diabetes: a randomized trial. Am J Med. 2004;116:732–739. doi: 10.1016/j.amjmed.2003.11.028. [DOI] [PubMed] [Google Scholar]
- 11.Diaz JA, Griffith RA, Ng JJ, Reinert SE, Friedmann PD, Moulton AW. Patients’ use of the Internet for medical information. J Gen Int Med. 2002;17:180. doi: 10.1046/j.1525-1497.2002.10603.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Silberg WM, Lundberg GD, Musacchio RA. Assessing, controlling, and assuring the quality of medical information on the Internet: Caveant lector et viewor--Let the reader and viewer beware. JAMA. 1997;277:1244–1245. [PubMed] [Google Scholar]
- 13.Bower H. Internet sees growth of unverified health claims. BMJ. 1996;313:381. doi: 10.1136/bmj.313.7054.381. [DOI] [PubMed] [Google Scholar]
- 14.Ullrich PF, Jr, Vaccaro AR. Patient education on the internet: opportunities and pitfalls. Spine. 2002;27:E185–188. doi: 10.1097/00007632-200204010-00019. [DOI] [PubMed] [Google Scholar]
- 15.Tate DF, Jackvony EH, Wing RR. Effects of internet behavioral counseling on weight loss in adults at risk for type 2 diabetes. JAMA. 2003;289:1833–1836. doi: 10.1001/jama.289.14.1833. [DOI] [PubMed] [Google Scholar]
- 16.Lenert L, Munoz RF, Stoddard J, Sansod A, Skoczen S, Perez-Stable EJ. Design and pilot evaluation of an internet smoking cessation program. J Am Med Inform Assoc. 2003;10:16–20. doi: 10.1197/jamia.M1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kwon HS, Cho JH, Kim HS, et al. Establishment of Blood Glucose Monitoring System Using the Internet. Diabetes Care. 2004;27:478–483. doi: 10.2337/diacare.27.2.478. [DOI] [PubMed] [Google Scholar]
- 18.Mensing C, Boucher J, Cypress M, et al. National Standards for Diabetes Self-Management Education. Diabetes Care. 2004;27:S143–150. doi: 10.2337/diacare.27.2007.s143. [DOI] [PubMed] [Google Scholar]
- 19.Raji A, Gomes H, Beard JO, MacDonald P, Conlin PR. A randomized trial comparing intensive and passive education in patients with diabetes mellitus. Arch Int Med. 2002;162:1301–1304. doi: 10.1001/archinte.162.11.1301. [DOI] [PubMed] [Google Scholar]
- 20.Izquierdo RE, Knudson PE, Meyer S, Kearns J, Ploutz-Snyder R, Weinstock RS. A comparison of diabetes education administered through telemedicine versus in person. Diabetes Care. 2003;26:1002–1007. doi: 10.2337/diacare.26.4.1002. [DOI] [PubMed] [Google Scholar]
- 21.Polonsky WH, Earles J, Smith S, et al. Integrating medical management with diabetes self-management training: a randomized control trial of the Diabetes Outpatient Intensive Treatment program. Diabetes Care. 2003;26:3048–3053. doi: 10.2337/diacare.26.11.3048. [DOI] [PubMed] [Google Scholar]
- 22.Kerr EA, Gerzoff RB, Krein SL, et al. Diabetes care quality in the Veterans Affairs Health Care System and commercial managed care: the TRIAD study. Ann Intern Med. 2004;141(4):272–81. doi: 10.7326/0003-4819-141-4-200408170-00007. [DOI] [PubMed] [Google Scholar]
- 23.Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs Health Care System on the quality of care. N Engl J Med. 2003;348:2218–27. doi: 10.1056/NEJMsa021899. [DOI] [PubMed] [Google Scholar]
- 24.Klonoff Dc, Schwartz DM. An economic analysis of interventions for diabetes. Diabetes Care. 2000;23:390–404. doi: 10.2337/diacare.23.3.390. [DOI] [PubMed] [Google Scholar]
- 25.Strategies for reducing morbidity and mortality from diabetes through health-care system interventions and diabetes self-management education in community settings. Morb Mortal Wkly Rep 2001 Sep 28; 50: 1–15. [PubMed]
- 26.Krishna S, Francisco BD, Balas EA, Graff GR, Madsen RW. Internet-enabled interactive multimedia asthma education program: a randomized trial. Pediatrics. 2003;111:503–510. doi: 10.1542/peds.111.3.503. [DOI] [PubMed] [Google Scholar]


