Abstract
In a study of occupational exposure to Bacillus thuringiensis, 20 exposed greenhouse workers were examined for Bacillus cereus-like bacteria in fecal samples and on biomonitoring filters. Bacteria with the following characteristics were isolated from eight individuals: intracellular crystalline inclusions characteristic of B. thuringiensis, genes for and production of B. cereus enterotoxins, and positivity for cry11 as determined by PCR. DNA fingerprints of the fecal isolates were identical to those of strains isolated from the commercial products used. Work processes (i.e., spraying) correlated with the presence of B. thuringiensis in the fecal samples (102 to 103 CFU/g of feces). However, no gastrointestinal symptoms correlated with the presence of B. thuringiensis in the fecal samples.
Bacillus thuringiensis is a gram-positive, facultatively anaerobic, endospore-forming bacterium. It is characterized by its ability to form parasporal crystalline inclusions toxic to larvae of different insect orders. These proteinaceous inclusions are the basis for the commercial use of B. thuringiensis as an insecticide, and since the beginning of the 1950s, this bacterium has been used increasingly against various insect pests. However, in recent years, the close relationship between B. thuringiensis and the bacterium Bacillus cereus, one bacterial species responsible for food poisoning, has been confirmed (4, 11, 37, 48). Despite the widespread use of B. thuringiensis, only few clinical case reports of illness related to the use of B. thuringiensis have been published (18, 21, 34, 40, 45).
Neither medical practice nor the methods used for detection of food pathogens (19) discriminate between B. thuringiensis and B. cereus as causative agents in connection with food contamination or gastroenteritis (41). Therefore, the true proportion of B. thuringiensis involvement in gastroenteritis thought to be caused by B. cereus is not known. However, one study exists in which B. thuringiensis has been shown to be involved in an outbreak of gastroenteritis in four persons (27). In this study, the bacteria initially identified as B. cereus were later found to be B. thuringiensis.
Much research has been aimed at identifying the virulence factors in B. cereus. At least four enterotoxins have been reported to be involved in causing gastroenteritis (32). The three-component hemolysin BL (HBL) complex has been well characterized and has been suggested to be a primary virulence factor in B. cereus diarrhea (6). Recently, the sequence of another three-component enterotoxin, the nonhemolytic enterotoxin (NHE), was published (20). Earlier, Agata et al. reported the identification of a single enterotoxin protein (BceT) (1). Lastly, a gene from B. cereus FM (entFM) has been isolated (3) whose product is implicated in the development of gastroenteritis. Most of these genes and gene products have been found as frequently in strains of B. thuringiensis as in strains of B. cereus (14, 15, 25). Additionally, some strains of B. cereus are known to produce an emetic toxin (2) but this toxin has not been associated with B. thuringiensis isolates.
To our knowledge, no information regarding the level of airborne B. thuringiensis originating from commercial insecticides in enclosed environments, such as greenhouses, has been previously published. Also, exposure in many studies has been measured indirectly; i.e., individuals exposed were defined as persons residing or working in areas sprayed with B. thuringiensis (8, 34). Therefore, a major aim of this study was to determine whether a correlation exists among individual exposure, gastrointestinal symptoms, work processes, and intestinal carriage of B. thuringiensis.
In the present study, we have isolated and characterized B. thuringiensis from fecal samples from greenhouse workers. Individual exposure levels were monitored with a personal bioaerosol sampling device, and the work processes and gastrointestinal symptoms were described.
MATERIALS AND METHODS
Materials.
The study involved 20 volunteers. Four males and 16 females (mean age, 41.0 [range, 27 to 61] years) working in four different greenhouses where B. thuringiensis-based insecticides were used agreed to donate fecal samples for microbial analysis. The insecticides used (Vectobac and Bactimos) were both based on B. thuringiensis subsp. israelensis, and the spraying was performed on the day of monitoring. Individuals with a known medical history were recruited among participants in a 3-year follow-up study of greenhouse workers in 31 different enterprises on Funen Island in Denmark. The data on each person were supplemented with questionnaire-generated data related to gastrointestinal symptoms the day before, on the same day, and the day after fecal samples were taken. The insecticides used (Vectobac and Bactimos) were both based on B. thuringiensis subsp. israelensis, and spraying against fungus gnats (Bradysia sp.) in ornamentals was performed on the day of monitoring. The Scientific Ethical Committee of Vejle and Funen Counties approved the study.
Design.
Bioaerosol sampling was performed on the day of B. thuringiensis spraying, and fecal samples were taken on days 0 to 5.
Collection of samples.
The participants were equipped with a personal bioaerosol sampler (IOM personal sampler; SKC Inc.) with a sterilized MultiDust Foam Disk and polycarbonate filter (pore size, 4 μm) (31). The individuals performing the spraying were not wearing facemasks or taking other precautionary measures to prevent inhalation exposure. Participants who were not spraying were typically working in the vicinity, i.e., in the same greenhouse, within 10 m of the spraying zone. The sampler was operated at 2 liters/min. The sampling device was mounted in the breathing zone, and the participants were instructed not to cover the sampler during the sampling procedure. The airflow rate was checked and calibrated three times during the 8-h sampling period. After exposure, the sampling devices were dismounted and filters were washed within 4 h after sampling in accordance with the method of Würtz et al. (50) and serial dilutions were spread on B. cereus selective agar (33) (Oxoid Ltd., Hampshire, United Kingdom). From each sampling device, 10 single colonies were randomly picked for further characterization, 5 colonies from the MultiDust filter sample (collection of thoracic particle fractions with a 10-μm cutoff point) and 5 colonies from the polycarbonate filter sample (collection of respirable particle fractions with a 4-μm cutoff point). As a negative control, one blank field sample was collected at each sampling site while the sampler was not in operation. Furthermore, the participants donated fecal samples for microbial analysis 0 to 5 days after exposure measurement. For storage, the fecal samples were mixed with an equal volume of brain heart infusion medium (39) containing 34% glycerol and stored at −80°C.
Isolation of B. cereus-like bacteria.
One gram of fecal material was combined with 9 ml of saline dilution liquid (0.9% [wt/vol] NaCl, 0.1% [wt/vol] peptone) and homogenized by using doublet bags and a Stomacher 400 (Ceward Ltd., London, United Kingdom) for 1 min. Serial dilutions (10−2, 10−3, and 10−4) were plated in duplicate directly on B. cereus selective medium and incubated at 30 and 37°C, respectively. Controls comprising B. cereus-negative fecal samples alone or the addition of a known number of B. thuringiensis cells were included and tested in parallel. Furthermore, heat treatment of fractions of the fecal samples (80°C, 15 min) was performed prior to dilution and plating on B. cereus selective medium. The controls showed that more than 80% of the added B. thuringiensis cells could be reisolated from feces after storage at −80°C for approximately 6 weeks. For the strains used as controls of insecticidal toxin genes, ribosomal organization, enterotoxin-related loci, and enterotoxin production see Table 3, where isolates from commercial insecticides used in Danish greenhouses and isolates from fecal samples from greenhouse workers are also listed.
TABLE 3.
Characterization of fecal isolates
| ID no.a | Parasporal inclusions | cry11 | cyt | hblA (Oxoid + PCR) | bceT | NHE (Tecra + PCR [nheA]) | Phospholipase C |
|---|---|---|---|---|---|---|---|
| B. cereus ATCC 10987 | − | − | − | − | NDb | + | + |
| B. cereus ATCC 10876 | − | − | − | + | ND | + | + |
| B. thuringiensis subsp. israelensis 4Q2 | + | + | + | + | + | + | + |
| Dipel | + | − | − | + | + | + | + |
| Vectobac | + | + | + | + | + | + | + |
| Bactimos | + | + | + | + | + | + | + |
| 457-1 | + | + | + | + | + | + | + |
| 457-2 | + | + | + | + | + | + | + |
| 457-3 | + | + | + | + | + | + | + |
| 457-4 | + | + | + | + | + | + | + |
| 457-5 | + | + | + | + | + | + | + |
| 457-6 | + | + | + | + | + | + | + |
| 457-7 | + | + | + | + | + | + | + |
| 302-1 | + | + | + | + | + | + | + |
| 302-2 | + | + | + | + | + | + | + |
| 302-3 | + | + | + | + | + | + | + |
| 302-4 | + | + | + | + | + | + | + |
| 302-5 | − | − | − | + | + | + | + |
| 302-6 | + | + | + | + | + | + | + |
| 171-1 | + | + | + | + | + | + | + |
| 171-2 | + | + | + | + | + | + | + |
| 171-3 | + | + | + | + | + | + | + |
| 171-4 | + | + | + | + | + | + | + |
| 171-5 | + | + | + | + | + | + | + |
| 421-1 | + | + | + | + | + | + | + |
| 421-2 | + | + | + | + | + | + | + |
| 421-3 | − | − | − | − | − | + | + |
| 421-4 | − | − | − | − | − | + | + |
| 459-1 | + | + | + | + | + | + | + |
| 459-2 | + | + | + | + | + | + | + |
| 459-3 | + | + | + | + | + | + | + |
| 573-1 | + | + | + | + | + | + | + |
| 573-2 | + | + | + | + | + | + | + |
| 507-1 | + | + | + | + | + | + | + |
| 244-1 | + | + | + | + | + | + | + |
ID,identification. The first three digits identify the origin of the strain (see sample code, Table 1) followed by a number for the individual strain.
ND, not determined.
DNA manipulations.
Total DNA was isolated by the method of Boe et al. (9). Preparation of large plasmids was performed as described previously (30). All PCR amplifications were performed with a PTC-100 programmable thermal controller (MJ Research Inc.) as previously described (29). DNA was analyzed by horizontal gel electrophoresis (6 to 10 V/cm) in 0.5 to 1.0% agarose (SeaKem GTG) with 1× Tris-borate-EDTA buffer (39) for 1.5 to 2 h. After electrophoresis, the gel was stained in 1 mg of ethidium bromide per ml for 5 to 10 min and destained in water. Where faint or indefinite bands were recovered, PCR amplifications were repeated with new DNA preparations. DNA was blotted from the agarose gel to Hybond N+ (pore size, 0.45 μm; Amersham International plc, Buckinghamshire, United Kingdom) by the method of Southern (43). For DNA fingerprinting, purified DNA samples (2 to 3 μg) were digested with AccI and analyzed by gel electrophoresis and subsequently blotted to Hybond N+ membranes. The probe for hybridization experiments was generated by using the primers GP-1 and GP-2 (36) (see Table 2) and 100 ng of template DNA from B. cereus reference strain ATCC 10987. Probe labeling with fluorescein, DNA hybridization, and washing steps were performed with the Gene Images random prime labeling module and the Gene Images CDP-Star detection module from Amersham. Restriction enzymes were purchased from New England Biolabs Inc. (Beverly, Mass.) or GIBCO-BRL and used as specified by the suppliers.
TABLE 2.
PCR primers used to characterize isolates from fecal samples and commercial insecticides
| Target(s) and primer pair | Primer sequence (5′ to 3′) | Amplicon size(s) (bp) | Reference |
|---|---|---|---|
| Insecticidal genes | |||
| Cry1a | CTG-GAT-TTA-CAG-GTG-GGG-ATA-T | 543-594 | 10 |
| Cry1b | TGA-GTC-GCT-TCG-CAT-ATT-TGA-CT | ||
| Cry3a | TTA-ACC-GTT-TTC-GCA-GAG-A | 652-718 | 12 |
| Cry3b | TCC-GCA-CTT-CTA-TGT-GTC-CAA-G | ||
| Cry11a | TTA-GAA-GAT-ACG-CCA-GAT-CAA-GC | 305 | 10 |
| Cry11b | CAT-TTG-TAC-TTG-AAG-TTG-TAA-TCC-C | ||
| Cyta | AAC-CCC-TCA-ATC-AAC-AGC-AAG-G | 522-525 | 10 |
| Cytb | GGT-ACA-CAA-TAG-ATA-ACG-CCA-CC | ||
| 16S-23S spacer region | |||
| G1 | GAA-GTC-GTA-ACA-AGG | 240, 460, 530, 650 | 13 |
| G2 | CAA-GGC-ATC-CAC-CGT | ||
| 23S internal fragment | |||
| GP1 | GGC-TCG-TCC-GCT-CAG-GG | 508 | 36 |
| GP2 | AAC-CTT-CCA-GCA-CCG-GG | ||
| Phospholipase C | |||
| plc1 | TGA-ATG-GCG-TAC-GGA-GTT-AGA | 415 | This study |
| plc2 | CCG-CTC-CAT-GAA-TCC-ACT-C | ||
| Enterotoxin gene | |||
| NheA1S | ATT-AAG-GTA-AAT-GCG-ATG-AG | 671 | This study |
| NheA1A | GCT-TCA-GTT-TGT-GAT-AAC-TT | ||
| HblA3 | ACG-AAC-AAT-GGA-GAT-ACG-GC | 1,017 | 46 |
| HblA4 | ATT-TTT-GTG-GAG-TAA-CAG-TTT-CTA-C | ||
| BceT3 | TTA-CAT-TAC-CAG-GAC-GTG-CTT | 427 | 46 |
| BceT4 | TGT-TTG-TGA-TTG-TAA-TTC-AGG |
Microscopy and taxonomy.
The isolates were streaked on agar starch medium (BD Biosciences) and inspected in a phase-contrast microscope after 2- and 3-day incubations at 30°C for parasporal inclusions characteristic of B. thuringiensis. Four general primer sets designed to detect various groups of insecticide toxin genes from B. thuringiensis (see Table 2) were employed. To examine whether the strains isolated from fecal samples belonged to the B. cereus group, rRNA typing with primers for the 16S-23S spacer region was performed (13). Furthermore, oligonucleotide primers GP1 and GP2 (see Table 2) were used to PCR amplify a 508-bp region within the 23S rRNA gene. This PCR product was used as a probe in a Southern blot with AccI-digested chromosomal DNA to give a DNA fingerprint of the strains.
Detection of enterotoxins.
Two commercial kits were used for detection of enterotoxins, the Oxoid BCET-RPLA kit (Unipath Ltd., Hampshire, United Kingdom) and the Tecra BDE-VIA kit (Tecra Diagnostics, Reading, United Kingdom). Overnight cultures originating from single colonies were diluted 1:100 in fresh Luria-Bertani broth and incubated for 12 h at 30°C with moderate shaking (200 rpm). The supernatant was isolated by centrifugation and subjected to enterotoxin immunoassays in accordance with the manufacturers' instructions. The Oxoid kit is reported to detect the L2 component of HBL (7), and the Tecra kit is reported to detect a component of the NHE complex (32). Finally, the presence of the bceT gene, which is reported to encode an enterotoxic protein (1, 35), was tested for by PCR assay with bceT-specific primers (see Table 2).
RESULTS
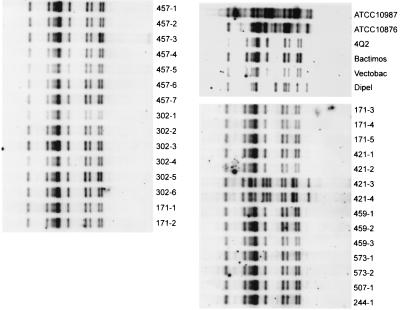
B. thuringiensis bacteria were isolated from the feces of 8 of the 20 participants. The results of the exposure study are shown in Table 1. The number of CFU isolated from the fecal samples gives an estimate in the range of 102 to 103 B. thuringiensis bacteria per g of feces (Table 1). On the basis of the numbers of CFU counted before and after heat treatment of the dilutions prior to plating on B. cereus selective agar, it is estimated that approximately 10% of the CFU originated from spores (data not shown). To verify that the strains isolated from both the fecal samples and the filters belonged to the B. cereus group, rRNA typing with primers for the 16S-23S spacer region was performed. Except for two isolates, 421-3 and 421-4 (see Table 3), all of the isolates gave rise to the four-band pattern characteristic of the B. cereus group (13) (data not shown). The DNA fingerprints in Fig. 1 show the results of digestion of genomic DNA with AccI, followed by hybridization of the 508-bp PCR fragment with the 23S rRNA gene (see Materials and Methods) (36). The DNA fingerprints (Fig. 1) of strains from Vectobac and Bactimos are identical to those of all of the fecal isolates (except isolates 421-3 and 421-4) and to that of reference strain B. thuringiensis subsp. israelensis 4Q2. B. cereus reference strains ATCC 10987 and ATCC 10876 and a B. thuringiensis subsp. kurstaki isolate from the commercial product Dipel all had individual rRNA typing patterns different from the patterns of the fecal isolates (Fig. 1).
TABLE 1.
Results of biomonitoring, questionnaire, and work processes
| Sample code | Work process(es) | No. of B. cereus-like CFUa
|
Presence of symptomsd
|
|||
|---|---|---|---|---|---|---|
| Biomonitoring | Feces | Before monitoring | On day of monitoring | Day after monitoring | ||
| 171 | Watering with VectoBac | 8.5 × 103b,c 6.5 × 103 | 103 | − | − | − |
| 166 | Packing | 0, 8.0 × 103 | − | − | − | |
| 507 | Packing | 0, 0 | 102 | + | + | + |
| 565 | Watering with VectoBac | 2.3 × 103, 2.7 × 103 | − | − | − | |
| 302 | Packing (working in Vectobac-sprayed area sprayed day before) | 1.9 × 104, 2.2 × 104 | 103 | − | − | − |
| 410 | Handling cuttings | <103, 1.9 × 104 | − | − | + | |
| 412 | Planting cactus | 2.4 × 104, 8.3 ×103 | + | + | + | |
| 413 | Handling cuttings | 1.0 × 103, <103 | + | + | + | |
| 419 | Handling cuttings | 3.5 × 103, <103 | + | + | + | |
| 421 | Watering with VectoBac | 4.0 × 104, 5.5 × 103 | 102 | + | + | + |
| 429 | Handling cuttings, moving plants | <103, <103 | + | + | + | |
| 457 | Watering with VectoBac | 1.1 × 104, 2.2 × 104 | 103 | − | − | − |
| 459 | Watering with VectoBac | 2.5 × 104, 1.9 × 104 | 102 | − | − | − |
| 223 | Handling cuttings | 0, 5.3 × 103 | − | − | − | |
| 573 | Handling cuttings, moving plants | 5.8 × 103, 0 | 102 | + | + | + |
| 526 | Watering with Bactimos | 1.5 × 105, 1.4 × 104 | − | − | − | |
| 244 | Watering with VectoBac | 1.5 × 103, 2.5 × 103 | 102 | − | − | − |
| 246 | Packing | <103, 2.5 × 103 | − | − | − | |
| 525 | Cutting, packing | 2.0 × 103, 2.5 × 103 | − | − | − | |
| 524 | Cutting, packing | 0, 1.6 × 104 | − | − | − | |
Determined on B. cereus selective substrate as mentioned in Materials and Methods.
Monitoring data are listed with the CFU count from the filter, followed by the CFU count from the MultiDust foam disk from each individual.
To get an estimate of the concentration of B. cereus bacilli in the air (CFU per liter), multiply the number by 195 (2 liters/min × 60 min/h × 7.5 h).
+, symptoms present; −, symptoms absent.
FIG. 1.
DNA fingerprints of strains from fecal samples and commercial products. Total DNA was digested with AccI and then subjected to hybridization with a fluorescein-labeled 508-bp fragment from the 23S rRNA gene of B. cereus reference strain ATCC 10987.
Additionally, the isolates were characterized by PCR with four general primer sets designed to detect various groups of insecticide toxin genes from B. thuringiensis (listed in Table 2). All isolates from the filters gave signals with primer sets against cry11 and cyt (data not shown). Commercial strains and all fecal isolates, except for isolates 421-3, 421-4, and 302-5, also gave signals with primer sets against cry11 and cyt, a finding that is further substantiated by the absence of parasporal inclusions (Table 3). The presence of enterotoxin genes was verified by PCR with the primers listed in Table 2. Primers NheA1S and NheA1 amplify a 671-bp product within the nheA gene (accession no. Y19005). Primers plc1 and plc2 amplify a 415-bp product within the plc gene (accession no. X12854). All air sample isolates were positive for these primer sets, and the results obtained with the fecal isolates are also summarized in Table 3. Furthermore, the expression of enterotoxins from the fecal isolates was detected by using the commercial kits and the results are listed in Table 3. Because of limitations on resources, the 200 environmental isolates were not tested for the expression of enterotoxins.
Although the study only included 20 participants, a positive correlation between the work process (i.e., spraying) and the presence of B. thuringiensis in the feces of workers (Fisher P-exact value, <0.05) can be observed. However, no health complaints (stomachache, loose stomach, nausea, or vomiting) correlated with exposure to B. thuringiensis as measured by biomonitoring or isolation from feces.
DISCUSSION
In recent years, the close relationship between B. thuringiensis and B. cereus has been further substantiated (11, 22, 23, 49). In reality, it is only the insect-toxic effect that differentiates the two species. The genes coding for insect toxins are found primarily on large plasmids in B. thuringiensis (5), and in the laboratory, these plasmids can be lost or transferred horizontally to other bacilli (16, 17, 28, 30, 47); hence, a B. thuringiensis strain can be transformed into a B. cereus strain and vice versa. We have previously isolated B. thuringiensis from the feces of exposed persons (29), and in this study, we have shown that commercial preparations of B. thuringiensis subsp. israelensis contain the genes for and produce enterotoxins characteristic of B. cereus. Additionally, we have shown that all of the B. thuringiensis isolates from the fecal samples of greenhouse workers also contained genes for and produced enterotoxins. Furthermore, except for the obvious discrepancies among isolates 421-3, 421-4, and 302-5, it was not possible to distinguish among the fecal isolates of B. thuringiensis from the greenhouse workers, the airborne isolates, and the commercial products used in the greenhouses by using any of the techniques employed in this study.
A high frequency of gastrointestinal problems has previously been reported for waste collectors, and Ivens et al. (26) have shown an exposure-response relationship among diarrhea, endotoxins, and microorganisms. In a study carried out in 1999 involving 48 exposed farm workers, Bernstein et al. failed to demonstrate occupationally related symptoms caused by B. thuringiensis (8). However, an increased immune response was detected in the exposed farm workers. Tayabali and Seligy have argued that if a spore-containing B. thuringiensis-based insecticide were to affect the body severely, it would be the result of an extremely rare scenario only made possible by the occurrence of an unfortunate combination of high spore concentrations and exposed individuals with impaired or weakened immune defense systems (44). It is known that the infective dose of B. cereus in food is typically greater than 105 CFU/g of food (38). The CFU counts measured in this survey during an entire workday did not amount to the numbers characteristic of infective doses. Hernandez et al. have mentioned that farm workers spraying with B. thuringiensis-based insecticides during a flu epidemic may constitute a potential risk group (24). Even with limited statistical material (n = 20), our study shows that there is a positive correlation between the work process (i.e., spraying or mixing) and the occurrence of B. thuringiensis in fecal samples. However, it was not possible to correlate this with any gastrointestinal symptoms. This is further substantiated by the fact that the amounts of B. thuringiensis isolated from fecal samples were sporadic and did not produce gastrointestinal symptoms.
In an examination of the safety of B. thuringiensis subsp. israelensis for mammals, Siegel et al. found that the strain examined seemed to be cleared from the (mouse) host as inert particles (42). In our study, only 10% of the isolates from fecal samples were insensitive to heat treatment. These data indicate that the majority of excreted cells were in the vegetative stage, meaning that the ingested spores could have germinated in the gastrointestinal tract. It remains to be clarified whether B. thuringiensis is able to colonize the intestine or if the vegetative cells isolated from the exposed individuals were spores that had germinated immediately prior to shedding in the feces.
In conclusion, we have shown that spraying with a B. thuringiensis-based insecticide correlates with the presence of B. thuringiensis in the feces of workers. We have been able to isolate B. thuringiensis from fecal samples from five of seven persons spraying with B. thuringiensis. Additionally, with the methods employed in this study, the B. thuringiensis isolates from the filter samples and fecal samples were indistinguishable from the B. thuringiensis strains isolated from the commercial insecticides used. Importantly, however, there was no evidence that the presence of B. thuringiensis in feces was correlated with any ill effects on the workers evaluated in this study.
Acknowledgments
This work was supported by a grant from the Danish Working Environment Fund and the Danish National Working Environment Authority.
REFERENCES
- 1.Agata, N., M. Ohta, Y. Arakawa, and M. Mori. 1995. The bceT gene of Bacillus cereus encodes an enterotoxic protein. Microbiology 141:983-988. [DOI] [PubMed] [Google Scholar]
- 2.Andersson, M. A., R. Mikkola, J. Helin, M. C. Andersson, and M. SalkinojaSalonen. 1998. A novel sensitive bioassay for detection of Bacillus cereus emetic toxin and related depsipeptide ionophores. Appl. Environ. Microbiol. 64:1338-1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Asano, S.-I., Y. Nukumizu, H. Bando, T. Iizuka, and T. Yamamoto. 1997. Cloning of novel enterotoxin genes from Bacillus cereus and Bacillus thuringiensis. Appl. Environ. Microbiol. 63:1054-1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ash, C., J. A. E. Farrow, M. Dorsch, E. Stackebrandt, and M. D. Collins. 1991. Comparative analysis of Bacillus anthracis, Bacillus cereus, and related species on the basis of reverse transcriptase sequencing of 16S rRNA. Int. J. Syst. Bacteriol. 41:343-346. [DOI] [PubMed] [Google Scholar]
- 5.Baum, J. A., and T. Malvar. 1995. Regulation of insecticidal crystal protein production in Bacillus thuringiensis. Mol. Microbiol. 18:1-12. [DOI] [PubMed] [Google Scholar]
- 6.Beecher, D. J., J. L. Schoeni, and A. C. L. Wong. 1995. Enterotoxic activity of hemolysin BL from Bacillus cereus. Infect. Immun. 63:4423-4428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beecher, D. J., and A. C. L. Wong. 1994. Identification and analysis of the antigens detected by two commercial Bacillus cereus diarrheal enterotoxin immunoassay kits. Appl. Environ. Microbiol. 60:4614-4616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bernstein, I. L., J. A. Bernstein, M. Miller, D. I. Bernstein, Z. Lummus, M. K. Selgrade, D. L. Doerfler, and V. L. Seligy. 1999. Immune responses in farm workers after exposure to Bacillus thuringiensis pesticides. Environ. Health Perspect. 107:575-582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boe, L., M. F. Gros, H. te Riele, S. D. Ehrlich, and A. Gruss. 1989. Replication origins of single-stranded-DNA plasmid pUB110. J. Bacteriol. 171:3366-3372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bravo, A., S. Sarabia, L. Lopez, H. Ontiveros, C. Abarca, A. Ortiz, M. Ortiz, L. Lina, F. J. Villalobos, G. Pena, M. E. NunezValdez, M. Soberon, and R. Quintero. 1998. Characterization of cry genes in a Mexican Bacillus thuringiensis strain collection. Appl. Environ. Microbiol. 64:4965-4972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carlson, C. R., D. A. Caugant, and A.-B. Kolstø. 1994. Genotypic diversity among Bacillus cereus and Bacillus thuringiensis strains. Appl. Environ. Microbiol. 60:1719-1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ceron, J., A. Ortiz, R. Quintero, L. Guereca, and A. Bravo. 1995. Specific PCR primers directed to identify cryI and cryIII genes within a Bacillus thuringiensis strain collection. Appl. Environ. Microbiol. 61:3826-3831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Daffonchio, D., S. Borin, A. Consolandi, D. Mora, P. L. Manachini, and C. Sorlini. 1998. 16S-23S rRNA internal transcribed spacers as molecular markers for the species of the 16S rRNA group I of the genus Bacillus. FEMS Microbiol. Lett. 163:229-236. [DOI] [PubMed] [Google Scholar]
- 14.Damgaard, P. H. 1995. Diarrhoeal enterotoxin production by strains of Bacillus thuringiensis isolated from commercial Bacillus thuringiensis-based insecticides. FEMS Immunol. Med. Microbiol. 12:245-249. [DOI] [PubMed] [Google Scholar]
- 15.Damgaard, P. H., H. D. Larsen, B. M. Hansen, J. Bresciani, and K. Jørgensen. 1996. Enterotoxin-producing strains of Bacillus thuringiensis isolated from food. Lett. Appl. Microbiol. 23:146-150. [DOI] [PubMed] [Google Scholar]
- 16.González, J. M., Jr., B. J. Brown, and B. C. Carlton. 1982. Transfer of Bacillus thuringiensis plasmids coding for δ-endotoxin among strains of Bacillus thuringiensis and Bacillus cereus. Proc. Natl. Acad. Sci. USA 79:6951-6955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.González, J. M., Jr., and B. C. Carlton. 1984. A large transmissible plasmid is required for crystal toxin production in Bacillus thuringiensis variety israelensis. Plasmid 11:28-38. [DOI] [PubMed] [Google Scholar]
- 18.Gordon, R. E. 1977. Some taxonomic observations on the genus Bacillus, p. 67-82. In J. B. Briggs (ed.), Biological regulations of vectors: the saprophytic and aerobic bacteria and fungi. U.S. Department of Health, Education, and Welfare, Washington, D.C.
- 19.Granum, P. E. 1997. Bacillus cereus determination in food. NMKL method no. 67, 4th ed. National Veterinary Institute, Oslo, Norway.
- 20.Granum, P. E., K. O'Sullivan, and T. Lund. 1999. The sequence of the non-haemolytic enterotoxin operon from Bacillus cereus. FEMS Microbiol. Lett. 177:225-229. [DOI] [PubMed] [Google Scholar]
- 21.Green, M., M. Heumann, R. Sokolow, L. R. Foster, R. Bryant, and M. Skeels. 1990. Public health implications of the microbial pesticide Bacillus thuringiensis: an epidemiological study, Oregon, 1985-86. Am. J. Public Health 80:848-852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Helgason, E., D. A. Caugant, I. Olsen, and A. B. Kolsto. 2000. Genetic structure of population of Bacillus cereus and B. thuringiensis isolates associated with periodontitis and other human infections. J. Clin. Microbiol. 38:1615-1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Helgason, E., O. A. Okstad, D. A. Caugant, H. A. Johansen, A. Fouet, M. Mock, I. Hegna, and A.-B. Kolstø. 2000. Bacillus anthracis, Bacillus cereus, and Bacillus thuringiensis—one species on the basis of genetic evidence. Appl. Environ. Microbiol. 66:2627-2630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hernandez, E., F. Ramisse, P. Gros, and J. Cavallo. 2000. Super-infection by Bacillus thuringiensis H34 or 3a3b can lead to death in mice infected with the influenza A virus. FEMS Immunol. Med. Microbiol. 29:177-181. [DOI] [PubMed] [Google Scholar]
- 25.Hsieh, Y. M., S. J. Sheu, Y. L. Chen, and H. Y. Tsen. 1999. Enterotoxigenic profiles and polymerase chain reaction detection of Bacillus cereus group cells and B. cereus strains from foods and food-borne outbreaks. J. Appl. Microbiol. 87:481-490. [DOI] [PubMed] [Google Scholar]
- 26.Ivens, U. I., N. O. Breum, N. Ebbehoj, B. H. Nielsen, O. M. Poulsen, and H. Wurtz. 1999. Exposure-response relationship between gastrointestinal problems among waste collectors and bioaerosol exposure. Scand. J. Work Environ. Health 25:238-245. [DOI] [PubMed] [Google Scholar]
- 27.Jackson, S. G., R. B. Goodbrand, R. Ahmed, and S. Kasatiya. 1995. Bacillus cereus and Bacillus thuringiensis isolated in a gastroenteritis outbreak investigation. Lett. Appl. Microbiol. 21:103-105. [DOI] [PubMed] [Google Scholar]
- 28.Jensen, G. B., L. Andrup, A. Wilcks, L. Smidt, and O. M. Poulsen. 1996. The aggregation-mediated conjugation system of Bacillus thuringiensis subsp. israelensis: host range and kinetics. Curr. Microbiol. 33:228-236. [DOI] [PubMed] [Google Scholar]
- 29.Jensen, G. B., P. Larsen, B. L. Jacobsen, B. Madsen, A. Wilcks, L. Smidt, and L. Andrup. 2002. Isolation and characterization of Bacillus cereus-like bacteria from faecal samples from greenhouse workers who are using Bacillus thuringiensis-based insecticides. Int. Arch. Occup. Environ. Health 75:191-196. [DOI] [PubMed] [Google Scholar]
- 30.Jensen, G. B., A. Wilcks, S. S. Petersen, J. Damgaard, J. A. Baum, and L. Andrup. 1995. The genetic basis of the aggregation system in Bacillus thuringiensis subsp. israelensis is located on the large conjugative plasmid pXO16. J. Bacteriol. 177:2914-2917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kenny, L. C., J. D. Stancliffe, B. Crook, S. Stagg, W. D. Griffiths, I. W. Stewart, and S. J. Futter. 1998. The adaptation of existing personal inhalable aerosol samplers for bioaerosol sampling. Am. Ind. Hyg. Assoc. J. 59:831-841. [DOI] [PubMed] [Google Scholar]
- 32.Lund, T., and P. E. Granum. 1997. Comparison of biological effect of the two different enterotoxin complexes isolated from three different strains of Bacillus cereus. Microbiology 143:3329-3336. [DOI] [PubMed] [Google Scholar]
- 33.Mossel, D. A., M. J. Koopman, and E. Jongerius. 1967. Enumeration of Bacillus cereus in foods. Appl. Microbiol. 15:650-653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Noble, M. A., P. D. Riben, and G. J. Cook. 1992. Microbial and epidemiological surveillance programme to monitor the health effects of Foray 48B BTK spray. Ministry of Forests, Vancouver, British Columbia, Canada.
- 35.Ombui, J. N., H. Schmeiger, M. M. Kagiko, and S. M. Arimi. 1997. Bacillus cereus may produce two or more diarrheal enterotoxins. FEMS Microbiol. Lett. 149:245-248. [DOI] [PubMed] [Google Scholar]
- 36.Patra, G., A. Fouet, J. Vaissaire, J.-L. Guesdon, and M. Mock. 2002. Variation in rRNA operon number as revealed by ribotyping of Bacillus anthracis strains. Res. Microbiol. 3:139-148. [DOI] [PubMed] [Google Scholar]
- 37.Priest, F. G., D. A. Kaji, Y. B. Rosato, and V. P. Canhos. 1994. Characterization of Bacillus thuringiensis and related bacteria by ribosomal RNA gene restriction fragment length polymorphisms. Microbiology 140:1015-1022. [DOI] [PubMed] [Google Scholar]
- 38.Rusul, G., and N. H. Yaacob. 1995. Prevalence of Bacillus cereus in selected foods and detection of enterotoxin using TECRA-VIA and BCET-RPLA. Int. J. Food Microbiol. 25:131-139. [DOI] [PubMed] [Google Scholar]
- 39.Sambrook, J., E. F. Fritsch, and T. Maniatis. 1989. Molecular cloning: a laboratory manual, 2nd ed. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, N.Y.
- 40.Samples, J. R., and H. Buettner. 1983. Ocular infection caused by a biological insecticide. J. Infect. Dis. 148:614. [DOI] [PubMed] [Google Scholar]
- 41.Shinagawa, K. 1990. Analytical methods for Bacillus cereus and other Bacillus species. Int. J. Food Microbiol. 10:125-141. [DOI] [PubMed] [Google Scholar]
- 42.Siegel, J. P., J. A. Shadduck, and J. Szabo. 1987. Safety of the entomopathogen Bacillus thuringiensis var. israelensis for mammals. J. Econ. Entomol. 80:717-723. [DOI] [PubMed] [Google Scholar]
- 43.Southern, E. 1975. Detection of specific sequences among DNA fragments separated by gel electrophoresis. J. Mol. Biol. 98:503-517. [DOI] [PubMed] [Google Scholar]
- 44.Tayabali, A. F., and V. L. Seligy. 2000. Human cell exposure assays of Bacillus thuringiensis commercial insecticides: production of Bacillus cereus-like cytolytic effects from outgrowth of spores. Environ. Health Perspect. 108:919-930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Warren, R. E., D. Rubenstein, D. J. Ellar, J. M. Kramer, and R. J. Gilbert. 1984. Bacillus thuringiensis var. israelensis: protoxin activation and safety. Lancet i:678-679. [DOI] [PubMed] [Google Scholar]
- 46.Wencheng, Z. 1998. Study of the bceT and hblA genes and the hemolysin BL of Bacillus thuringiensis group. Chin. J. Microbiol. Immunol. 18:428-433. [Google Scholar]
- 47.Wilcks, A., N. Jayaswal, D. Lereclus, and L. Andrup. 1998. Characterization of plasmid pAW63, a second self-transmissible plasmid in Bacillus thuringiensis subspecies kurstaki HD-73. Microbiology 144:1263-1270. [DOI] [PubMed] [Google Scholar]
- 48.Wunschel, D., K. F. Fox, G. E. Black, and A. Fox. 1995. Discrimination among the B. cereus group, in comparison to B. subtilis, by structural carbohydrate profiles and ribosomal RNA spacer region PCR. Syst. Appl. Microbiol. 17:625-635. [Google Scholar]
- 49.Wunschel, D. S., D. C. Muddiman, K. F. Fox, A. Fox, and R. D. Smith. 1998. Heterogeneity in Bacillus cereus PCR products detected by ESI-FTICR mass spectrometry. Anal. Chem. 70:1203-1207. [DOI] [PubMed] [Google Scholar]
- 50.Würtz, H., J. Kildesø, H. W. Meyer, and J. B. Nielsen. 1999. A pilot study on airborne microorganisms in Danish classrooms, p. 316-321. In G. Raw, C. Aizlewood, and P. Warren (ed.), Indoor air 1999. Proceedings of the 8th International Conference on Indoor Air and Climate, vol. 1. [Google Scholar]