Abstract
Three-quarters of a century after the introduction of Mycobacterium bovis BCG, the first tuberculosis vaccine, new vaccines for tuberculosis are finally entering clinical trials. This breakthrough is based not only on advances in proteomics and genomics which have made the construction of new vaccines possible, but also on a greatly expanded knowledge of the immunology of tuberculosis. Here we review our current understanding of how Mycobacterium tuberculosis subverts or survives the host's immune response to cause disease and why the current vaccination strategy, which relies on BCG, is only partially successful in countering the pathogen. This provides a background for describing the new generation of vaccines designed to supplement or replace the current vaccine and the different approaches they take to stimulate immunity against M. tuberculosis.
INTRODUCTION
Tuberculosis (TB) is a disease rich in paradoxes. It was one of the first diseases for which the causative agent (Mycobacterium tuberculosis) was identified, and one of the first for which a vaccine was developed (20, 80). Antibiotics effective against M. tuberculosis have been widely available for a half century (72). Yet it remains one of the great killers, causing between 2 and 3 million deaths, and an estimated 8 to 10 million new infections a year (4). Most recently, the human immunodeficiency virus epidemic has caused the number of new TB cases to explode (1). Although the disease is currently only endemic in developing countries (4), epidemics in the developed world are only prevented by ceaseless monitoring for infection and treatment of potentially exposed individuals. Thus, in addition to the mortality and morbidity it causes, M. tuberculosis inflicts a significant economic cost on the developed and developing world alike. This situation has arisen largely because of the complicated immunology of M. tuberculosis infection and has led to increasing interest in developing new and better vaccines.
At the end of the 19th century, Robert Koch discovered M. tuberculosis as the causative agent of TB and attempted to develop a therapy using a sterile filtrate from in vitro cultures of the pathogen. This was tested in TB patients and was spectacularly unsuccessful. Not only did it fail to provide protection against the virulent organism, but the inflammatory immune responses induced in individuals with active disease were severe. Known as the Koch phenomenon, this necrotic reaction appears to be due to overproduction of several proinflammatory cytokines, but in particular of tumor necrosis factor (TNF-α) (131). Even in Koch's time, it was thought that successful protection against TB required an inflammatory response (a supposition now known to be true) and the fact that tuberculin induced such a strong inflammatory response in the skin (the so-called delayed-type hypersensitivity response) was taken as an indication of its activity. Therefore, Koch's failure illustrates an important point for TB vaccine development: the same immune responses involved in protection against infection with M. tuberculosis are also involved in the pathology underlying the disease. Stimulating the first without worsening the second is the goal of current attempts to develop novel TB vaccines.
VACCINATION AND CONTROL OF TUBERCULOSIS
The first people to succeed in this task were Albert Calmette and Camille Guérin of the Pasteur Institute, who attenuated a mycobacterium related to M. tuberculosis (Mycobacterium bovis bacillus Calmette-Guérin [BCG]) by growing it in on culture medium for 13 years, monitoring its decrease in virulence in animals through this period (20). In 1921, the newly developed BCG vaccine was administered to infants in France, where it proved a resounding success, reducing mortality by approximately 90%. In the intervening decades BCG has become one of the most widely used of all vaccines, being both cheap and safe. Unfortunately, despite early success, the BCG vaccine has had limited effect against the epidemic of TB in the developing world. The reasons for this have been a matter of debate, and this uncertainty has hindered the development of new vaccines. It is only recently that we have begun to understand the limitations of BCG, which are in large part due to the relationships between M. tuberculosis, BCG, and other, nonpathogenic, mycobacteria. The first part of the puzzle has been a better understanding of TB and M. tuberculosis infection.
Immunopathology and M. tuberculosis Infection
M. tuberculosis normally enters the host via the mucosal surface of the lung after inhalation of infectious droplets from an infected individual. The droplets are deposited in the alveolar spaces, where the bacteria are taken up by phagocytic cells. Ingestion of the bacteria induces a rapid inflammatory response which results in the accumulation of a variety of immune cells and, with time, the formation of a granuloma, characterized by a relatively small number of infected phagocytes surrounded by activated monocytes/macrophages and, farther out, activated lymphocytes (55). If the infection is successfully contained, the granuloma shrinks and may eventually calcify. If however, the immune response does not successfully control the bacterial replication, the granulomas increase in size and cellularity. Eventually, cell death in the hypoxic center of the granuloma leads to necrosis. If the granuloma is close to the surface of the lung, the tissue destruction caused by necrosis can breach the mucosal surface, giving rise to the prototypic symptom of TB, a persistent cough with blood in the sputum, a process referred to as cavitation. At this point the patient is highly infectious, spreading the bacteria by aerosol.
Tissue destruction in TB is not mediated by the activities of the bacteria alone; it is immunopathological in nature, and the crucial point to understand is that it is critical for the survival of both the host and the bacteria. The outer surface of M. tuberculosis contains a number of molecules that bind to the host's pathogen-associated molecular pattern receptors, the best characterized of which are the Toll-like receptor (TLR) family, although others certainly play a role (81). Thus, although engagement of TLRs appears to be a crucial initial step for antimycobacterial immune responses (125, 157), all clinical strains of M. tuberculosis express a number of molecules (both expressed on the bacteria's surface and secreted) which trigger these pathways. Interestingly, the majority of these molecules do not seem to be crucial to mycobacterial viability, and as this pathogen has a long coevolutionary history with humanity (16, 17), it suggests that their conservation serves another important function.
The simplest explanation is that M. tuberculosis depends on the immunopathology that promotes cavitation for spread to new hosts. A failure to stimulate inflammatory immune responses is an evolutionary dead end for the bacteria. At the same time, the same immune responses are essential for the host to control bacterial replication. This balance is clearly illustrated by the course of tuberculosis in human immunodeficiency virus-infected individuals, whose immune deficiency renders them simultaneously more susceptible to fatal bacteremia and less infectious than normal, since they cavitate less frequently than people with an intact immune response (1).
Thus, since it cannot evade the induction of cell-mediated immunity, M. tuberculosis has evolved to survive it. And survive it does; even if the initial infection is successfully controlled, many (perhaps all) infected individuals develop a latent infection that can persist for decades (1, 27, 69, 88, 91, 94, 114, 133).
Immunology of M. tuberculosis Infections
The nature of the cells responding to M. tuberculosis infection and how their relative contribution changes over time is an area of obvious importance for rational vaccine development. Animal models suggest that CD4 T cells are the most important aspect of the protective response in primary infection (126). These cells remain important in chronic infection as well, as indicated by animal studies (22, 174) and the high risk of disease reactivation in patients coinfected with human immunodeficiency virus (1). The main effector function of CD4 T cells is mediated by their cytokine production and immunity to mycobacterial infection clearly requires a Th1 response; genetic defects in either gamma interferon (IFN-γ) or interleukin-12 (IL-12) pathways are associated with extreme susceptibility to infection (30, 33, 76). However, IFN-γ production alone is no guarantee of protection against M. tuberculosis (2). Most, if not all, individuals respond to mycobacterial infection by producing IFN-γ, at least initially. The IFN-γ produced by both conventional (CD4 and CD8) and unconventional (γδ, NK, and CD-1-restricted) (82) T cells serves to activate antigen-presenting cells, boosting expression of major histocompatibility complex (MHC) and costimulatory molecules and amplifying IL-12 and IL-18 production, resulting in a positive feedback loop for IFN-γ production (Fig. 1).
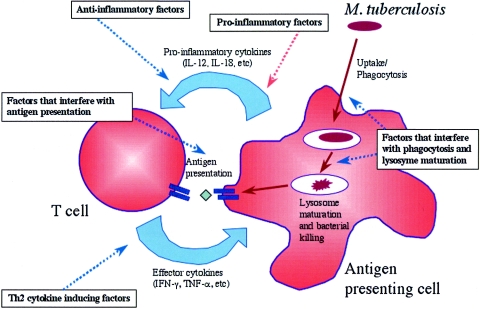
FIG. 1.
Schematic representation of the normal immune response and the different steps where M. tuberculosis intervenes. The Th1 immune response to M. tuberculosis is central to immunity to the pathogen, and the IFN-γ and IL-12 pathway stimulated by proinflammatory factors induced by mycobacterial cell wall lipids is essential for macrophage activation, resulting in lysosome maturation and bacterial killing. M. tuberculosis counteracts this by manipulating the cytokine response through induction of inhibitory Th2 cytokines (IL-4 and IL-10), affecting production of IL-12 themselves, and by modulating the activity of receptor-associated transcription factors such as Stat1. The immune response is also modulated by factors that interfere with antigen-specific responses (by either blocking presentation of antigen or, conversely, promoting immune responses to nonprotective antigens). At the same time, M. tuberculosis deploys an impressive armory of genes to interfere with phagocytosis and lysozyme maturation and function of antigen-presenting cells.
The clear role for IFN-γ-dependent anti-M. tuberculosis effects shown by the effect of genetic defects in this feedback loop (30, 33, 76) has been shown to be due to a variety of factors. Those which have been well studied include induction of reactive nitrogen derivatives (especially nitric oxide) (5, 111, 147) which are directly toxic, alteration of phagocytic vesicle tracking/control by molecules such as LRG-47 (98), which augment lymphocyte responsiveness in response to IFN-γ after M. tuberculosis infection (45), and a general inhibition of the inflammatory cascade which would otherwise lead to increased production of cytokines such as tumor necrosis factor alpha (Fig. 1).
While CD4 T cells apparently contribute more to the early IFN-γ response, CD8 T cells are thought to become more important in the later phases of disease (143, 174), possibly via cytotoxic activity (156) and IFN-γ production (143, 144). The effector function of cytolytic CD8 T cells is disputed but their primary role has been suggested to be the elimination of “old” nonactive phagocytic cells resulting in release of mycobacteria that can then be taken up by newly recruited macrophages with increased antibacterial activity. This may reflect the situation in which the immune system in individuals who had controlled the acute infection attempts to respond to the changing antigenic repertoire and growth pattern of the bacteria in the chronic phase.
The model fits well with data indicating that in animal models, a deficiency in MHC class II (and therefore lack of CD4 T cells) greatly impaired the response to acute infection while a deficiency in MHC class I, was less pronounced during the acute stage but had an influence during the more chronic stages of TB (83, 130, 155) Recent studies, however, indicate that the reality is more complicated. The CD4 T-cell population includes both effector and regulatory subsets, and evidence is beginning to accumulate that the failure of immunity to primary infection may be associated with an accumulation of CD25+ regulatory T cells. These cells are normally associated with down-regulation of the immune response (66) and it is not yet clear whether their increase is a natural host reaction to a growing inflammatory response, or a bacterial product-driven “trick” to evade immunity. The former is suggested by the association of more severe disease manifestations in TB patients, with decreased proportions of CD25+ cells in both the CD4+ and CD8+ T-cell subsets (119). Thus, it appears that the outcome of infection relies on a balance between antigen-specific inflammatory and regulatory T cells in both the MHC I- and MHC II-restricted T-cell compartments.
Adding to the complexity of the immune response, it has long been known that populations of T cells restricted by unconventional presentation molecules (γδ T cells and CD1-restricted T cells) are also expanded during M. tuberculosis infection, (170). The expanded populations of these types of cells appear to be antigen-specific, but the antigens that they respond to are nonpeptidic (for example, lipids and long-chain glycoproteins) thus increasing the number of cues that the host immune system can respond to (9, 31, 110). Like CD8+ T cells, the exact role of these subsets has been controversial, in part because the data from genetic knockout models have been much less impressive than those from studies in which conventional MHC molecules have been removed (78, 83, 84). Ordway and colleagues suggest that both cytokine production and cytotoxic functions may play a role (119), but that cytotoxicity by TCR+ γδ T cells may be their primary function, consistent with earlier studies (38) whereas noncognate cytokine production in the early phases of infection by TCR-γδ T cells may amplify antigen-presenting cell function (37).
Finally, CD1-restricted cells appear to primarily recognize the glycolipids abundant in mycobacterial cell walls and to distinguish these from self-derived lipids (132). Since their receptors are far less variable than those of T cells restricted by conventional MHC I and II molecules, it has been hypothesized that they serve as a bridge between the innate and adaptive immune systems by providing the initial IFN-γ production to start the inflammatory cascade (139, 171). But just as for MHC I-restricted cells, precisely how these T cells acquire their antigen has been a hotly debated topic. It has now been suggested that they respond to products liberated by the apoptotic process (189).
Interaction of M. tuberculosis and the Host Immune System
If the normal immunological process, as described above, was allowed to develop undisturbed, the infection would be eliminated without the need to boost the immune system by vaccination. However, mycobacteria have evolved a very extensive battery of factors to counteract the normal immunological mechanism. The schematic (Fig. 1) provides an outline of the core pathways involved in killing of M. tuberculosis by phagocytic cells and known factors that interfere with this process. These interactions are discussed below but it should be stressed that a detailed accounting is beyond the scope of this review: more interactions are being defined all the time and it is quite likely that different mechanisms are involved at different stages of the infection. What is known is that M. tuberculosis interferes with this process at almost every stage.
Proinflammatory factors.
The cell wall of M. tuberculosis expresses many long-chain fatty acids, the best studied of which are the mycolic acids (13, 81, 125), which strongly stimulate host inflammatory responses, leading to granuloma formation (161), upregulation of antigen presentation and subsequent NK and T-cell responses (136). It has recently been demonstrated that the best-characterized mycolate, trehalose dimycolate, or cord factor, selectively induces a Th1 cytokine response through STAT4 signaling (115). In addition, some of these long-chain fatty acids strongly influence the survival or death by apoptosis of infected macrophages and can promote expression of a complex mixture of cytokines in addition to those that promote IFN-γ production (113, 135). The outcome of these interactions is harder to predict, since the different combinations of factors induced by stimulation of multiple TLRs is nearly infinite and can have both positive and negative outcomes, as discussed below.
Anti-inflammatory factors.
Although a crucial mediator (and proxy marker) of protection, the induction of a strong IFN-γ response may not be enough by itself (2) to kill the bacteria. The mechanism remains unknown, but live bacteria or M. tuberculosis cell wall extracts can inhibit some of the downstream effects of IFN-γ, by reducing STAT-1 binding to transcriptional activators, providing a potential solution: IFN-γ is produced, but its effects are modulated to the bacteria's advantage (164). Production of IFN-γ also varies markedly during the infectious process. Many groups have reported that in vitro IFN-γ recall responses are reduced in patients with advanced TB (36, 40, 176) and the observation that these responses recover in most patients during therapy suggests that this unresponsive state is directly related to the disease (75, 102, 166), though again the precise mechanism has not been described.
One potential candidate for this role is the immunosuppressive cytokine IL-10. It is known that lipoarabinomannan, a major cell wall component of M. tuberculosis, can bind to the DC-Sign molecule, expressed on the surface of dendritic cells. DC-Sign is crucial to dendritic cell maturation, and lipoarabinomannan binding inhibits this process, decreases IL-12 production, and induces dendritic cells to secrete IL-10 (54). Consistent with this, recent studies have found that expression of IL-10 is significantly elevated in TB patients with active disease (36, 116).
Th2 cytokine-inducing factors.
Recent work also suggests that M. tuberculosis may interfere with the balance between IFN-γ and IL-4. Naturally, given the clear importance of Th1 responses in the control of M. tuberculosis infection, the hypothesis that there is a change in the Th1/Th2 balance during the development of disease or protective immunity has been an attractive one. Evidence for increased IL-4 expression in TB was suggested by the finding of elevated IgE or soluble CD30 in TB patients compared to community controls in a TB-endemic region (90). This suggestion was confirmed by intracellular fluorescence-activated cell sorting analysis and reverse transcription-PCR analyses (141, 142, 173). Other factors also point to an important role for IL-4 in the development of tuberculosis.
Differences in T-cell proliferative responses to M. tuberculosis antigens are associated with polymorphisms in the IL-4 receptor (186), while increased production of a splice variant (IL-4δ2) that antagonizes IL-4 activity appears to be characteristic of individuals who are controlling TB in its latent stage (in other words, with protection after natural infection) (36). The observation that IL-4 remains elevated in latently infected individuals, suggests that elevated levels of its antagonist, IL-4δ2 in healthy, latently infected individuals may be a way of coping with IL-4 production driven by the bacteria even during latent infection (48). It also implies that the balance of IFN-γ and IL-4 (and its antagonistic splice variant) is more informative with regard to disease progression than the absolute levels of any single factor by itself, a conclusion supported by studies in the cattle model of TB (185). Most interestingly, the level of IL-4 gene expression appears to correlate both with disease severity (in TB patients) (73, 74) and with risk of clinical disease in individuals who have been exposed but are still healthy (118). This result supports the hypothesis that increased IL-4 expression is not merely coincident with TB but may play a causative role. A potential mechanism has been suggested by recent studies indicating that lipids or lipoproteins from the cell wall of epidemic Beijing strains of M. tuberculosis may specifically induce higher levels of IL-4 and IL-13 in human cells than nonepidemic strains and that one such glycolipid is associated in animal models with inhibition of cell-mediated immunity (101, 129).
Factors that interfere with antigen-specific responses.
Recent data suggest that M. tuberculosis attempts to avoid the consequences of the immune response induced, by expressing “decoy” molecules, which stimulate a Th1 immune response which is antigen specific, but ultimately ineffective. For example, immune responses to the 27-kDa lipoprotein of M. tuberculosis are characterized by strong IFN-γ secretion, but in animal models at least, these responses are not protective, and in fact, appear to promote bacterial growth (68). The highly polymorphic PE-PGRS and PPE/MPTR gene families have also been suggested as a source of antigenic variation in M. tuberculosis (27). Certainly, TB patients mount immune responses to PGRS proteins (e.g., Rv1759c [44]; Rv3367 [149]) and vaccination of mice with one member of the PE-PGRS family (Rv1818c) resulted in a strong but ineffective immune response against M. tuberculosis infection. Interestingly, vaccination with just a fragment of the same gene (lacking the highly polymorphic region) was protective (35).
A more direct intervention is the effect of the 19-kDa lipoprotein of M. tuberculosis, which has a negative effect on immunity to the bacterium (191), interacts with host antigen-presenting cells via TLR1 and TLR2 (162), leading to inhibition in cytokine production, antigen processing, and MHC II expression (49, 112, 120), turning what is normally regarded as a proinflammatory pathway into an anti-inflammatory one. Since TLR2 is implicated in the inflammatory response to mycobacteria (105, 172), it has been suggested that inhibition of antigen presentation and response to IFN-γ by the 19-kDa molecule may allow the bacteria to evade immune surveillance during the latent phase of infection (53, 112, 120), while still allowing the initiation of immune responses during acute infection.
Certainly, when tested as a vaccine in animal models, the 19-kDa antigen appeared to have an antiprotective effect (191) implying that some M. tuberculosis-derived proteins could have long-lasting negative effects on the development of protective immune responses. While there is no empirical evidence to suggest it is a problem in human disease, the presence of the 19-kDa gene—and other possibly antiprotective proteins—in live mycobacterial vaccines remains a concern. At the very least, such proteins are of dubious value as vaccine candidates (127, 191). Taken in total, these studies indicate that M. tuberculosis is able to interfere with almost every stage of the host's immune response (Fig. 1) and give some insight into why it is such an effective pathogen. Countering these complex strategies in the design of novel vaccines is a daunting task.
Factors that interfere with phagocytosis and lysozyme maturation.
A major component of M. tuberculosis's success as a pathogen rests on its ability to survive within macrophages. The various means used to interfere with the immune system have already been briefly discussed, but in addition the pathogen is also able to disrupt the maturation of the phagosome containing it, creating an intracellular compartment that resembles an endosome rather than a lysosome, and lacking the acidic, hydrolytic environment needed to kill the bacteria. However, fusion with other vesicles and membrane remodeling and trafficking still occur, allowing M. tuberculosis to acquire necessary nutrients and export its own proteins (134). A wide range of genes are involved in this process. The functions of some are as yet unknown, but putative transporters, iron-scavenging molecules, and lipid-synthesizing molecules are all apparently important (122) in preventing normal phagosome maturation.
This interaction starts with the very first contact between phagocytes and M. tuberculosis. Bacterial surface molecules (as yet unidentified, but presumably mannose derivatives) from pathogenic (but not nonpathogenic) mycobacteria inhibit phagocytosis by some types of macrophages (159) and therefore potentially allow the pathogen to target cell types more susceptible to infection. Invasion of phagocytes which are not already activated is important for the bacteria's survival: exposure of macrophages to IFN-γ and/or tumor necrosis factor alpha before but not after infection decreases the ability of pathogenic mycobacteria to inhibit phagosome maturation and function (140, 182). This maturation is reflected in the alteration of divalent and trivalent cations (especially iron) within the vacuole, a process which appears to depend on the accumulation of ATPases and GTPases in the vacuole (79, 140). Accumulation of ATPases also seems to be essential for the decrease in pH needed to kill the bacteria (160).
The number of ways in which M. tuberculosis interferes with this process attests to its importance to the survival of the bacteria. Blocking GTPase accumulation appears to depend on the bacteria having access to sufficient iron (79). By holding the phagosome in a “nonmaturing state” M. tuberculosis prevents fusion with late endosomal/lysosomal vesicles while retaining access to early endosomal vesicles, a process dependant at least to some extent on the blocking of calmodulin-dependant Ca2+ flux by lipoarabinomannan, though it is not the only molecule involved (100, 177, 178). Other lipids such as trehalose dimycolate, a potent stimulator of inflammatory responses and granuloma formation, can also prevent phagosome maturation (71). Interestingly, other lipids, including mannose-capped lipoarabinomannan (52) seem to be mimics of host phosphatidylinositols. Their presence presumably interferes with the coordinated expression of phosphatidylinositols on the surface of the vacuole, by which it signifies its maturation state (23, 24). The expression inside the phagosome by M. tuberculosis of a eukaryotic-like serine/threonine protein kinase G that can inhibit phagosome-lysosome fusion and which is crucial for intracellular survival of mycobacteria suggests that mimicking host signal transduction mechanisms to modulate intracellular trafficking may be a general survival strategy for pathogenic mycobacteria (183).
VACCINE DESIGN FOR M. TUBERCULOSIS
The ability of M. tuberculosis to manipulate the host's immune response is not, of course exclusively one-sided and the host can respond effectively, as proved by the fact that most individuals infected with the bacteria do not succumb to the disease. More encouragingly, increasing the host's immune response by vaccination is also possible, as shown by the partial success of BCG vaccination. The use of the word “partial” to describe BCG's effect is based on its very variable efficacy in different trials (46, 47). In the developed world, BCG has generally shown very high and consistent efficacy, and it is often credited with helping end the TB epidemics in Europe and Japan (60). In contrast, its effect in developing countries has been far less consistent (in some studies, the vaccine had no measurable effect on TB incidence at all). The reasons for this may have more to do with vaccine trial design and the local environment than the vaccine itself (47, 188).
It now seems clear that BCG gives significant protection, but only for a limited period of time, and in addition, it is not effective in populations already sensitized to mycobacterial antigens (whether by prior BCG vaccination, exposure to environmental mycobacteria, or latent TB infection) (15, 26). This means that while BCG seems to be effective at reducing the rate of pediatric TB if given to infants (who have no prior immunity to interfere with the vaccination), that period of immunity extends at best 10 to 20 years (28, 61, 158) so that neonatal vaccination has had little effect on the rate of TB in adults (3, 15, 25).
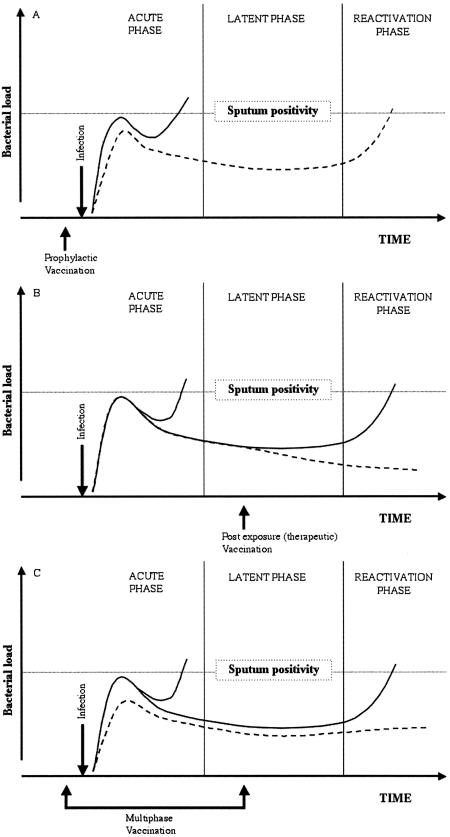
The implications of this for vaccine design are clear: if BCG vaccination at birth can give only short-lived immunity, the options are either to replace BCG with a vaccine that gives a longer duration of protection or to design a vaccine that can be given at a later time point to boost existing immunity and provide protection in adults. Both of these approaches have advantages and disadvantages, and the vaccines now entering clinical trials include proponents of both approaches. However, one important caveat of administering the vaccine at late time points (referred to as the late booster strategy) is the fact that in highly TB-endemic regions such a vaccine will in many cases be given to already latently infected individuals. It is therefore necessary not only to develop such a vaccine as a BCG booster vaccine but also as a postexposure vaccine -an approach that brings its own set of problems and challenges. Eventually it is possible that the only practical outcome might be a hybrid approach, what can be termed a multiphase vaccine that can be administered regardless of the infectious status of the individual and with activity both in naïve and already-infected individuals (Fig. 2).
FIG. 2.
Schematic model of the effect of preexposure, postexposure, and multiphase vaccination. The course of infection with M. tuberculosis (black line) is characterized by an increase in bacterial load until the cognate immune response develops, at which point bacterial growth is reversed. In a minority of individuals (3 to 5%), the bacteria escape control and begin to expand again, resulting in clinical TB and sputum positivity. Preexposure vaccination hastens the development of this initial immune response, leading to earlier arrest of bacterial growth and preventing the infection from becoming symptomatic (A). However, in the majority of infected individuals, the initial infection may be controlled but sterile immunity is not achieved. Instead, M. tuberculosis establishes a latent infection which can later reactivate, causing clinical TB. Postexposure vaccination aims to strengthen immune surveillance to prevent this reactivation (B), but it cannot prevent those cases that arise during acute infection. A hypothetical multiphase vaccine will not only inhibit the infection from becoming symptomatic but will also prevent later reactivation (C). An important consequence of preventing reactivation is that if bacterial load is reduced, not only is disease prevented in the recipient, but the cycle of transmission is broken.
Replacing BCG (Priming Vaccines)
Replacing BCG will not be an easy task; it is perhaps the most used vaccine in the world, and despite its limitations, is cheap, safe, and well established. As mentioned above, neonatal vaccination with BCG seems to consistently provide significant protection against the most severe childhood manifestations of the disease, such as TB meningitis. However, most studies have reported that the efficacy of BCG lasts for no more than 10 to 20 years (28, 61, 158). In Europe, where BCG vaccination was combined with campaigns to identify and isolate adults with TB in sanatoria (or once chemotherapy was developed, to treat them), this appears to have been enough to cause a rapid decrease in incidence. However, in much of the world where TB remains endemic, the resources to track and isolate or treat new cases are lacking and BCG vaccination alone has proven unable to decrease the number of cases in adults. Thus, in hyperendemic regions such as crowded shantytowns and urban slums, the incidence is so high (in the worst cases, reaching 1,000 per 100,000) that most adults are continually exposed to infection. In such an environment, any individual without solid immunity would soon be infected. To prevent this with vaccination alone requires the stimulation of an immune response that persists for decades.
It remains unclear if this is a realistic goal. Animal models (and current research funding paradigms) are ill suited to measure vaccine efficacy over years or even decades. That means that what is most often attempted prior to human trials is to exceed the efficacy of BCG in short-term experiments, in the hope that a stronger primary immune response will also lead in turn to a longer-lasting memory response. In contrast to its record in human trials, BCG has generally provided high levels of protection in animal models (in particular in the guinea pig model) of TB (152) and although considerable progress has been made in the development of efficient subunit vaccines, there is still no reported evidence for efficacies exceeding that of BCG in naïve individuals. Therefore, by this measure, the vaccines that have showed most promise so far as a replacement for BCG are to be found among the live mycobacterial vaccines.
The first of these to enter the clinic, the rBCG30 vaccine, has recently passed phase I clinical trials (67). This vaccine was derived from a vaccine strain of BCG, which has been genetically modified to overexpress the immunodominant antigen Ag85B (67). The idea behind this vaccine was to improve BCG by expressing higher levels of an antigen that had already been shown to be protective. Furthermore, based on the observation that BCG appeared to perform well in the earliest recorded trials but poorly in later trials (25, 26), it was suggested that “modern” strains of BCG were overattenuated and had reduced immunogenicity due to a continued loss of genes from the vaccine stock (10). This may help explain the long period of protection afforded by BCG found on reanalysis of early vaccination campaigns (6).
While it could be argued that variations in efficacy could be explained by the fact that later trials were done under different circumstances and in different populations from the earlier trials, two lines of research support the “attenuation” hypothesis. The first is the rBCG30 vaccine itself: it was reported as having a clearly improved efficacy compared to the parental vaccine strain (67). The improved efficacy of rBCG30 came as something of a surprise, since BCG possesses a functional gene for Ag85B. However, recent work has shown that overexpression of genes can alter the immune response to the antigens they encode (127), reminding us that the mere presence of a gene tells us little about its expression in vivo and that a gene's effects may be modulated by the presence or absence of other genes.
The second piece of supporting evidence is the observation that new vaccines based on attenuation of Mycobacterium bovis (the parental strain of BCG) are both more virulent and give greater protective efficacy than BCG (34). In addition, highly attenuated mutants of M. tuberculosis, though still protective when used as vaccines, have proven less virulent—and less protective—than BCG (137). These results are compatible with the contention that BCG has become “too attenuated.” Building on the same concept, BCG into which the RD1 locus was reintroduced (allowing it to secrete the ESAT-6-CFP10 complex) was reported to be both more virulent but also more protective than the parental BCG strain (124). Interestingly, this vaccine strain (designated BCG::RD1) has recently been shown to trigger an immune response that is qualitatively more similar to that of M. tuberculosis than BCG. Specifically, vaccination with BCG::RD1 induced the recruitment of activated/effector T cells and dendritic cells to the lungs of subsequently infected mice far more efficiently than the parental BCG strain (99). This suggests that antigens encoded by RD1 (and lost during the attenuation of BCG) can significantly modify the type of immune response generated by a mycobacterial vaccine or that a certain level of virulence (perhaps more than that of current vaccine strains) is necessary for the optimal induction of strong immune responses by live vaccines. Efficiency aside, it is questionable if such hypervirulent vaccine strains would have the safety profile necessary for mass vaccination, especially in areas of high human immunodeficiency virus incidence (77).
The last of the BCG-based vaccines which is near clinical testing takes a different and more technically sophisticated approach. The rBCG::ΔureC-llo+ vaccine is a urease-deficient BCG mutant which expresses the listeriolysin O gene from Listeria monocytogenes. These bacteria are unable to arrest phagosome maturation, due to the urease deficiency, and are less virulent than wild-type BCG in immunodeficient scid mice. This may make it safer in populations where human immunodeficiency virus infection is widespread (which, of course, also tend to be the areas where TB incidence is highest), and where the BCG vaccine can cause occasional cases of disseminated BCGosis (21). In addition, the decreased pH in the maturing phagosome provides optimal conditions for the listeriolysin, which is thought to damage the phagosome membrane, allowing leakage into the cytosol and potentially increasing the amount of bacterially derived antigen available for presentation to CD8 T cells via the cytosolic scavenger pathways as previously described (29, 57).
Other groups have attempted to make new vaccines by attenuating M. tuberculosis instead of augmenting gene expression in BCG, reasoning that this would give the closest simulation of natural immunity occurring after M. tuberculosis infection. However, as noted above, M. tuberculosis is remarkably adept at escaping eradication by the immune response; even a cured natural M. tuberculosis infection does not necessarily confer life-long protection (32). It should also be noted that (in animal models) the protection induced by a cured M. tuberculosis infection is not always superior to that from BCG vaccination of a naïve recipient (108). Nonetheless, at least two TB vaccines based on attenuated M. tuberculosis are under development. One of the most important issues such a strategy needs to address is the risk that a vaccine strain based on M. tuberculosis could revert to a virulent form, and obviously the question of how much attenuation is sufficient (18).
The preferred approach has been to make mutations in two crucial genes to reduce the potential for reversion to a virulent form. One such vaccine, developed at the Albert Einstein Hospital in New York, a PanD− Leu− auxotroph of M. tuberculosis (137, 138), has demonstrated both safety in immunodeficient scid mice and protective efficacy in the highly susceptible guinea pig infection model. It is hoped that this vaccine will enter clinical trials within the next 12 months. The ΔphoP/R mutant, in which the phoP virulence factor is inactivated by the insertion of an antibiotic gene, is another vaccine that has showed significant promise in animal models (128a). The hope is that these vaccines will generate better, perhaps longer-lasting immune responses than BCG, but with the possibility of boosting that immunity at a later stage, if necessary. However, if boosting is necessary, these vaccines are unlikely to be successful in that role.
Like BCG, all of these vaccines are intended to be given to immunologically naïve recipients (essentially, that restricts their use to neonates in developing country settings). Boosting BCG-generated immunity by a second dose of BCG given at a later time point has repeatedly failed to show any beneficial effect (89). This failure is consistent with results from animal studies, which have shown that BCG (and therefore presumably any mycobacterial live vaccine) requires a period of multiplication and dissemination in the host to stimulate a protective immune response. If this is blocked by chemotherapy shortly after vaccination (51, 148), then the protective effect of vaccination is abrogated. An existing immune response (whether due to prior BCG vaccination or cross-reactive immune responses arising from exposure to other mycobacteria in the environment) appears to have the same effect, leading to the rapid clearance of BCG (11, 19, 96). This may explain both the demonstrated effect of BCG vaccination in neonates and in adult populations where skin-test-positive individuals have been excluded (25) and its failure in trials where adult (mycobacterially sensitized) individuals were included. If, as anticipated, new mycobacterial vaccines are unable to stimulate life-long immunity, neonatal vaccination may need to be augmented by nonmycobacterial vaccines, so-called booster vaccines.
Augmenting BCG (Late Booster Vaccines or Postexposure Vaccines)
In contrast to vaccines designed to replace BCG, late booster vaccines aim to take advantage of the widespread use of BCG by boosting immunity in young adults already primed by earlier vaccination in childhood. Approximately 3 billion people, half the world's population, have received BCG (153), and most of these live in areas where TB is endemic. Even if the protective effect of the new vaccines lasts no longer than that induced by BCG, it would still greatly reduce the number of new TB cases by reducing incidence over the peak age for TB (25 to 35 years). The “priming/boosting” dichotomy is slightly misleading. Even in areas where BCG vaccination is routine, not every person will be BCG vaccinated and not every vaccinee will have effective immunological memory. So booster vaccines will also need to be able to stimulate effective primary responses as well. However, the requirements are slightly different from those for vaccines intended to replace or compete with BCG for neonatal vaccination.
Whereas a vaccine intended to replace BCG needs to demonstrate superior efficacy to BCG to be seriously considered, booster vaccines are often no more effective than BCG at generating primary immune responses (42, 150, 187). However, they have the additional requirement that they need to be effective in sensitized as well as in naïve recipients, a test which BCG signally fails (11). Furthermore, with the high prevalence of latent TB in TB-endemic areas, the vaccines need to be designed with their potential activity in already infected individuals in mind (postexposure vaccines). This may demand the inclusion of a completely different set of gene products to target the genes that may be upregulated by the mycobacteria in response to long-term exposure to the hostile environment of the activated macrophage. This will be dealt with later in this review.
A variety of live vaccines have been developed as booster vaccines, including a recombinant adenovirus (179) and a recombinant strain of Shigella designed to act as a delivery system for a DNA vaccine (50). These vaccines are still in the developmental stage and it is not clear when they will be ready for clinical trials. However, one live booster vaccine is now in clinical trials (104). This is MVA-85A, a recombinant, replication-deficient vaccinia virus expressing the strongly immunogenic antigen 85A from M. tuberculosis (56). The vaccine has performed well in animal models (56) and now data from the first clinical trials show that it is immunogenic and apparently safe in humans (104).
Also among the first wave of new TB vaccines entering clinical trials are products based on recombinant proteins. In the past, recombinant protein vaccines have not been terribly successful at stimulating strong Th1 responses, due to the lack of adjuvants suitable for generating strong cell-mediated immunity responses in humans without generating unacceptable side effects (58, 92). For many years, the only adjuvant approved for human use was alum, which was only effective for vaccines that required a humoral response (e.g., diphtheria, tetanus, and hepatitis B vaccines). Indeed, since this adjuvant biases the immune response towards the Th2 pole (14) it has actually been shown to decrease the protection generated by vaccination against M. tuberculosis (92). More recently, MF59 was approved for human use, but this adjuvant has so far also been restricted to vaccines where generating humoral responses is key, such as influenza (123).
However, new adjuvants are now entering the clinic (Table 1) and several of these generate strong Th1 responses, making them good candidates for vaccines against M. tuberculosis. These new vaccines owe their success in animal models to an improved understanding of the activation of the immune system in response to conserved molecules on pathogens (41, 63, 64, 93, 121, 169) being built around bacterially derived lipids, bacterial toxins, or analogues of these molecules. In some cases (monophosphoryl lipid A, for example) the receptors are known and are part of the Toll-like receptor family. In other words, we are starting to use some of the same techniques to manipulate the immune responses that M. tuberculosis uses which were described above. We can expect to see more vaccines using this approach in the future, since both recombinant antigens and the adjuvants can easily be synthesized on a large scale, lending themselves to vaccine production.
TABLE 1.
Adjuvants for use with human subunit vaccinesa
| Type | Adjuvant | Characteristics |
|---|---|---|
| Adjuvants suitable for use with subunit vaccines, already registered for human use | Alum (aluminum hydroxide) | The first human adjuvant, alum promotes a strong humoral response and is widely used in viral vaccines; however, it generates strongly Th2-polarized responses and is not suitable for use as a TB vaccine (14, 92) |
| MF59 | An oil-in-water emulsion composed of 5% squalene, 0.5% Tween 80, and 0.5% Span 85; like alum, it generates primarily humoral immunity and is used in influenza vaccines (123) | |
| Virosomes | Similar in structure to liposomes, virosomes are differentiated by containing viral proteins embedded in their membrane, which are delivered into host cells by membrane fusion; currently used in vaccines against viral targets such as influenza and hepatitis A, where humoral immunity is most important (70) | |
| Adjuvants suitable for use with subunit vaccines, in or approaching clinical trials | CAP (calcium phosphate nanoparticles) | Currently in early clinical trials, CAP has been used to generate humoral responses, but the lower levels of IgE induced suggest it may not be as polarized towards the Th2 pole of the immune response as alum (62) |
| LTK63 | A modified and detoxified heat-labile toxin from Escherichia coli tested in human volunteers as an influenza vaccine; generates strongly Th1-polarized responses and is therefore being considered for vaccines against M. tuberculosis and HIV (121) | |
| Lipovac | A stable emulsion containing the cationic surfactant dimethyl dioctadecyl ammonium bromide and the synthetic mycobacterial cord factor trehalose dibehenate (64); has shown good efficacy in animal models and a good safety profile in toxicity studies; currently planned for clinical trials in a TB vaccine in 2006-2007 | |
| AS2 | An oil-in-water emulsion containing 3-deacylated monophosphoryl lipid A (a detoxified form of lipid A from Salmonella enterica serovar Minnesota), and a purified fraction of Quillaria saponaria, known as Quil A; currently in early clinical trials as a TB vaccine; a synthetic analogue of monophosphoryl lipid A called RC-529 is in clinical trials in an HIV vaccine; generates strongly Th1-polarized responses (163) | |
| IC31 | A mixture of oligodeoxynucleotides and polycationic amino acids; generates strong Th1 responses and will enter phase I clinical trials in 2005 as part of a TB vaccine (93, 103) | |
| Montanide | A water-oil emulsion, two variants exist, based on mineral and non-mineral oil; tested initially as a cancer immunotherapeutic agent, Montanide has now been through a variety of clinical trials through to phase III; it generates a mixed-cell-mediated and humoral response, which may render it less attractive for a TB vaccine (7) | |
| ISCOM | A formulation of Quillaja saponins, cholesterol, phospholipids, and protein, typically self-assembling into small icosahedral cage-like particles; used initially for veterinary vaccines, immunostimulatory complexes have recently shown promise in late-phase human clinical trials for viral vaccines; their potential for M. tuberculosis vaccines remains unknown, as they generate a mixed humoral and cell-mediated response (109) | |
| OM-174 | A modified and detoxified lipid A from Escherichia coli (diphosphate triacyl); synthetic analogues also exist; currently in early clinical trials for cancer immunotherapy and suggested for TB vaccine use; generates strongly Th1-polarized responses (107) |
The adjuvants listed are those which are already in or about to enter clinical trials. Many of these adjuvants are also being tested as platforms; that is, the basic delivery system is being tested together with other immunodulating agents (such as ISCOMs being used with mycobacterial lipids) or vice versa (monophosphoryl lipid A [MPL-A] derivatives are finding their way into many adjuvants, and MF59 is being augmented with oligodinucleotides) and so on. These variants are in general, however, less developed with regard to clinical use.
The first of these subunit TB vaccines to enter clinical trials is the 72f vaccine (150), jointly developed by Corixa and GSK. This vaccine is a fusion molecule comprised of two proteins, with the PPE family member Rv1196 inserted into the middle of the putative serine protease Rv0125, which is thus present as two fragments. The adjuvant used contains the saponin derivative QS21 mixed with the TLR4 ligand monophosphoryl lipid A (150). In addition to its activity for priming, this vaccine has also been demonstrated to have a BCG booster effect (12). The second recombinant protein, although developed independently by the Statens Serum Institute, is very similar in its design philosophy. It is a fusion molecule comprised of two immunodominant, secreted proteins from M. tuberculosis (ESAT-6 and Ag85B) and has proven highly efficacious in animal models ranging from mice to primates, more effective in fact, than the single antigens (42, 117, 184). The vaccine has also proven effective as a booster for BCG and augments its efficacy even though the ESAT-6 component of the vaccine is not present in BCG (authors' unpublished data).
The Ag85B-ESAT-6 fusion protein is slated for two clinical trials in 2005-2006. The first of these will test the vaccine in a conventional parenteral vaccination strategy, using a mixture of oligodeoxynucleotides and polycationic amino acids as the adjuvant (93). The second trial, running in parallel, will test the same antigen by the nasal route, using LTK63, a modified, heat-labile enterotoxin from Escherichia coli as an adjuvant (121). ESAT-6 is currently also being applied as a diagnostic tool to detect cell-mediated immunity responses that specifically signal the presence of ongoing infection (40, 87, 128, 175). New fusion molecules that do not contain ESAT-6 are therefore the subject of ongoing research and interestingly, the only antigen so far found which may be able to replace ESAT-6 is also a member of the same small gene family but is, in contrast to ESAT-6, present in BCG (39, 93, 121, 151).
In some ways these two recombinant vaccines can be viewed as M. tuberculosis in miniature—they contain two immunodominant antigens and use as adjuvants modified molecules derived from human pathogens that stimulate Th1 responses. This minimalist approach offers certain advantages. By choosing a limited number of carefully tested immunodominant antigens, we should generate a strong protective response, while avoiding the possibility of inducing unwanted modulation of the response or of antigen presentation. By using adjuvant molecules (slightly modified to decrease their toxicity) derived from human pathogens, we should generate exactly the type of inflammatory response the body normally invokes to deal with a bacterial infection.
Postexposure Vaccination
All of the vaccines described above are prophylactic vaccines, intended to be given to individuals prior to M. tuberculosis infection, and hopefully prior to exposure to the disease. It is not clear whether they will be efficacious or even safe if given to individuals already infected with M. tuberculosis. For booster vaccines this is a serious issue, since in TB-endemic areas, the target population can be expected to include many latently infected subjects. What few data are available from animal studies do not suggest that the leading vaccine candidates induce a Koch phenomenon-like effect in infected recipients, but neither do they suggest these vaccines are effective against the latent phase of the disease (167; authors' unpublished work). It is likely that handling the billions who are potentially latently infected with M. tuberculosis will require a combined strategy, using a multiphase vaccine effective against both acute and latent infection (Fig. 2).
The acute phase of M. tuberculosis infection is characterized by rapid bacterial growth and the development of an immune response targeted towards bacterial antigens actively secreted in the first growth phase, such as ESAT-6 (154). The vaccines so far developed against these acute-phase antigens can reduce the severity of the initial bacteremia and disease but they do not prevent the establishment of infection (42, 117). However, as M. tuberculosis adapts to the hypoxic and hostile environment of host macrophages, it has been shown to undergo a dramatic change in gene transcription thought to be characteristic of latency (65, 106) and this change in gene expression may enable the pathogen to persist in the face of strong memory immune responses. This latent stage of infection is normally associated with a few bacteria surviving in a so-called “dormant state” with low or altered metabolic activity.
When grown in vitro under conditions mimicking those thought to exist in vivo, M. tuberculosis up-regulates overlapping, characteristic sets of genes (145, 181, 192). Increased expression of genes such as HspX (also called α-crystallin, Rv2031c, etc.) during the stationary growth phase (192) appears to be crucial for the survival of the organism (193). In agreement with these in vitro observations it has been demonstrated that the transcription of a number of genes is down-regulated while others are strongly up-regulated after the initiation of a strong immune response in infected animals (146). Together with the abundance of regulatory proteins in the M. tuberculosis genome (27), this indicates the importance of the pathogen's being able to adapt to different environments during infection. This regulatory flexibility may underlie its ability to shift between acute progressive disease and long-lived latent infection.
In addition to the experimental evidence described above, studies in humans are beginning to offer evidence to support the hypothesis that immune responses in healthy but latently infected individuals are targeted to different antigens than the response to an acute infection (Demissie et al., submitted; Klein et al., submitted). It is hoped that vaccinating with other antigens, such as HspX, identified by the in vitro methods described above may promote an immune response that will help prevent reactivation of disease. There is some evidence that such an approach may indeed work. Lowrie and colleagues successfully employed an HSP65-based DNA vaccine in latently infected mice (95), but this finding has been somewhat controversial (168) and emphasizes the need for more research in this field, in particular, the need for rigorously validated animal models.
One area attracting such interest is the “resuscitation-promoting factor” or rpf genes. Micrococcus luteus expresses an rpf gene whose product is required to resuscitate the growth of dormant cultures of Micrococcus luteus and which is essential for the growth of this organism. It has recently been demonstrated that M. tuberculosis has at least five rpf homologues (43, 165), again suggestive of the importance of latency and resuscitation to the survival of M. tuberculosis. Given that they appear to be essential for recovery from the dormant state and are immunogenic, secreted antigens, they make tempting targets for vaccination (190).
The postexposure vaccination area is now being intensively pursued, and although a vaccine is still in the future, it offers the possibility of a multiphase vaccine that induces responses both against acute phase antigens, thus providing protection if the recipient is subsequently infected, and against latency-associated antigens, so that disease is held in remission even if the vaccine recipient is already infected.
INTO THE CLINIC: THE ROAD AHEAD
TB vaccines are only now entering the clinic, but the path for testing is already well laid out: the risk of inducing a severe reaction in already-infected individuals and the high rate of TB and human immunodeficiency virus coincidence in many areas mean that vaccines are first tested for safety and immunogenicity in immunologically naïve individuals (neither BCG vaccinated nor skin test positive) before proceeding into human immunodeficiency virus-positive and latently TB-infected individuals. Concurrent with this, booster vaccines will need to be tested in BCG-vaccinated subjects to see if existing immune responses can be boosted. The first of the new booster vaccine candidates will start this phase in 2005. Given the extensive testing that has already been done in animal models, including primates, it is unlikely that safety problems will arise. That leaves two major hurdles for new vaccines to face.
The first is the question of efficacy. The older TB vaccine trials based on BCG measured efficacy using a simple clinical endpoint: how many cases of TB in the vaccine group compared to a placebo or unvaccinated group. TB develops slowly, and even in high-incidence areas, the case rate is typically much less than 1%. This means that to obtain reliable data, efficacy studies have taken decades and involved very large numbers of participants (typically in excess of 100,000) (8). That is a costly exercise and unattractive to both vaccine developers and public health systems trying to deal with millions of cases annually. Priming vaccines such as recombinant BCG and attenuated M. tuberculosis must be used in immunologically naïve populations, as discussed above, so ultimately their effect on adult pulmonary TB will only be detectable after decades.
However, a quicker route to determining their efficacy in humans will be to examine the effect on TB in infants compared to standard BCG vaccination. Though such a study will necessarily be large, it could be completed in only a few years, and this is the course most likely to be adopted at first. Booster vaccines have a shorter duration between vaccination and the peak years for adult TB incidence, as they are likely to be given to young adults in their teenage years. However, this still means a wait of approximately a decade before any effect can be expected to be clearly detectable. Thus, even late booster vaccines may be tested first against pediatric TB, simply to demonstrate that they are effective in humans.
Recent progress in the TB diagnostic field may turn out to be a very important tool in future clinical trials. The number of M. tuberculosis infections is much greater than the number of clinical cases, and recent improvements in diagnostic tools, based on measuring immune responses to M. tuberculosis virulence factors (such as ESAT-6, which is not expressed in BCG or most environmental mycobacteria), have shown promise at detecting subclinical and latent TB (40, 59, 85, 86, 128, 175). Recent data indicate that the magnitude of the ESAT-6 response may reflect the severity of infection (97, 180) and may predict later breakdown with disease (40) so that measuring the rate of incipient disease (and high ESAT-6 reactivity) rather than the rate of subsequent breakdown may offer the possibility of a far more rapid assessment of vaccine efficacy and the ability to use much smaller cohorts. Before it can be used, however, this approach needs to be validated, and studies to that purpose are ongoing.
The second question is what effect even an improved vaccine will have on TB incidence, given the vast reservoir of latent TB that already exists. Mathematical modeling suggests that a postexposure vaccine effective at preventing disease in latently infected individuals would cause a significant decrease in the number of new cases in the short term, but that over time a preexposure vaccine would have larger effect (194). The ideal approach would therefore be a single multiphase vaccine that was effective against both acute and latent infection, but no such vaccine currently exists. Thus, although we have come a long way in TB vaccine development in the last decade, there are still significant gaps in our knowledge that we need to fill before we can truly hope to control M. tuberculosis through a novel vaccination strategy.
REFERENCES
- 1.Aaron, L., D. Saadoun, I. Calatroni, O. Launay, N. Memain, V. Vincent, G. Marchal, B. Dupont, O. Bouchaud, D. Valeyre, and O. Lortholary. 2004. Tuberculosis in HIV-infected patients: a comprehensive review. Clin. Microbiol. Infect. 10:388-398. [DOI] [PubMed] [Google Scholar]
- 2.Agger, E. M., and P. Andersen. 2001. Tuberculosis subunit vaccine development: on the role of interferon-gamma. Vaccine 19:2298-2302. [DOI] [PubMed] [Google Scholar]
- 3.Anonymous 1999. Fifteen year follow up of trial of BCG vaccines in south India for tuberculosis prevention. Indian J. Med. Res. 110:56-69. [PubMed] [Google Scholar]
- 4.Anonymous 2005. Global tuberculosis control - surveillance, planning, financing W.H.O./HTM/TB/2005. World Health Organization, Geneva, Switzerland.
- 5.Arias, M., M. Rojas, J. Zabaleta, J. I. Rodriguez, S. C. Paris, L. F. Barrera, and L. F. Garcia. 1997. Inhibition of virulent Mycobacterium tuberculosis by Bcg(r) and Bcg(s) macrophages correlates with nitric oxide production. J Infect. Dis. 176:1552-1558. [DOI] [PubMed] [Google Scholar]
- 6.Aronson, N. E., M. Santosham, G. W. Comstock, R. S. Howard, L. H. Moulton, E. R. Rhoades, and L. H. Harrison. 2004. Long-term efficacy of BCG vaccine in American Indians and Alaska Natives: A 60-year follow-up study. JAMA. 291:2086-2091. [DOI] [PubMed] [Google Scholar]
- 7.Aucouturier, J., L. Dupuis, S. Deville, S. Ascarateil, and V. Ganne. 2002. Montanide ISA 720 and 51: a new generation of water in oil emulsions as adjuvants for human vaccines. Expert Rev. Vaccines 1:111-118. [DOI] [PubMed] [Google Scholar]
- 8.Baily, G. V. 1980. Tuberculosis prevention Trial, Madras. Indian J. Med. Res. 72(Suppl.):1-74. [PubMed] [Google Scholar]
- 9.Behar, S. M., C. C. Dascher, M. J. Grusby, C. R. Wang, and M. B. Brenner. 1999. Susceptibility of mice deficient in CD1D or TAP1 to infection with Mycobacterium tuberculosis. J. Exp. Med. 189:1973-1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Behr, M. A. 2001. Correlation between BCG genomics and protective efficacy. Scand. J. Infect. Dis. 33:249-252. [DOI] [PubMed] [Google Scholar]
- 11.Brandt, L., J. Feino Cunha, A. Weinreich Olsen, B. Chilima, P. Hirsch, R. Appelberg, and P. Andersen. 2002. Failure of the Mycobacterium bovis BCG vaccine: some species of environmental mycobacteria block multiplication of BCG and induction of protective immunity to tuberculosis. Infect. Immun. 70:672-678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brandt, L., Y. A. Skeiky, M. R. Alderson, Y. Lobet, W. Dalemans, O. C. Turner, R. J. Basaraba, A. A. Izzo, T. M. Lasco, P. L. Chapman, S. G. Reed, and I. M. Orme. 2004. The protective effect of the Mycobacterium bovis BCG vaccine is increased by coadministration with the Mycobacterium tuberculosis 72-kilodalton fusion polyprotein Mtb72F in M. tuberculosis-infected guinea pigs. Infect. Immun. 72:6622-6632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brennan, P. J. 2003. Structure, function, and biogenesis of the cell wall of Mycobacterium tuberculosis. Tuberculosis (Edinburgh) 83:91-97. [DOI] [PubMed] [Google Scholar]
- 14.Brewer, J. M., M. Conacher, C. A. Hunter, M. Mohrs, F. Brombacher, and J. Alexander. 1999. Aluminium hydroxide adjuvant initiates strong antigen-specific Th2 responses in the absence of IL-4- or IL-13-mediated signaling. J. Immunol. 163:6448-6454. [PubMed] [Google Scholar]
- 15.Brewer, T. F. 2000. Preventing tuberculosis with bacillus Calmette-Guerin vaccine: a meta-analysis of the literature. Clin. Infect. Dis. 31(Suppl. 3):S64-67. [DOI] [PubMed] [Google Scholar]
- 16.Brosch, R., S. V. Gordon, M. Marmiesse, P. Brodin, C. Buchrieser, K. Eiglmeier, T. Garnier, C. Gutierrez, G. Hewinson, K. Kremer, L. M. Parsons, A. S. Pym, S. Samper, D. van Soolingen, and S. T. Cole. 2002. A new evolutionary scenario for the Mycobacterium tuberculosis complex. Proc. Natl. Acad. Sci. USA 99:3684-3689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brosch, R., A. S. Pym, S. V. Gordon, and S. T. Cole. 2001. The evolution of mycobacterial pathogenicity: clues from comparative genomics. Trends Microbiol. 9:452-458. [DOI] [PubMed] [Google Scholar]
- 18.Brown, N., M. Jacobs, S. K. Parida, T. Botha, A. Santos, L. Fick, B. Gicquel, M. Jackson, V. Quesniaux, and B. Ryffel. 2005. Reduced local growth and spread but preserved pathogenicity of a ΔpurC Mycobacterium tuberculosis auxotrophic mutant in gamma interferon receptor-deficient mice after aerosol infection. Infect. Immun. 73:666-670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buddle, B. M., B. J. Wards, F. E. Aldwell, D. M. Collins, and G. W. de Lisle. 2002. Influence of sensitisation to environmental mycobacteria on subsequent vaccination against bovine tuberculosis. Vaccine 20:1126-1133. [DOI] [PubMed] [Google Scholar]
- 20.Calmette, A., and H. Plotz. 1929. Protective inoculation against tuberculosis with BCG. Am. Rev. Tuberc. 19:567-572. [Google Scholar]
- 21.Campos, J. M., J. P. Simonetti, M. V. Pone, L. A. Carvalho, A. C. Pereira, and J. R. Garrido. 1996. Disseminated Bacillus Calmette-Guerin infection in HIV-infected children: case report and review. Pediatr. AIDS HIV Infect. 7:429-432. [PubMed] [Google Scholar]
- 22.Caruso, A. M., N. Serbina, E. Klein, K. Triebold, B. R. Bloom, and J. L. Flynn. 1999. Mice deficient in CD4 T cells have only transiently diminished levels of IFN-gamma, yet succumb to tuberculosis. J. Immunol. 162:5407-5416. [PubMed] [Google Scholar]
- 23.Chua, J., and V. Deretic. 2004. Mycobacterium tuberculosis reprograms waves of phosphatidylinositol 3-phosphate on phagosomal organelles. J. Biol. Chem. 279:36982-36992. [DOI] [PubMed] [Google Scholar]
- 24.Chua, J., I. Vergne, S. Master, and V. Deretic. 2004. A tale of two lipids: Mycobacterium tuberculosis phagosome maturation arrest. Curr. Opin. Microbiol. 7:71-77. [DOI] [PubMed] [Google Scholar]
- 25.Colditz, G. A., C. S. Berkey, F. Mosteller, T. F. Brewer, M. E. Wilson, E. Burdick, and H. V. Fineberg. 1995. The efficacy of bacillus Calmette-Guerin vaccination of newborns and infants in the prevention of tuberculosis: meta-analyses of the published literature. Pediatrics 96:29-35. [PubMed] [Google Scholar]
- 26.Colditz, G. A., T. F. Brewer, C. S. Berkey, M. E. Wilson, E. Burdick, H. V. Fineberg, and F. Mosteller. 1994. Efficacy of BCG vaccine in the prevention of tuberculosis. Meta-analysis of the published literature. JAMA 271:698-702. [PubMed] [Google Scholar]
- 27.Cole, S. T., R. Brosch, J. Parkhill, T. Garnier, C. Churcher, D. Harris, S. V. Gordon, K. Eiglmeier, S. Gas, C. E. Barry, 3rd, F. Tekaia, K. Badcock, D. Basham, D. Brown, T. Chillingworth, R. Connor, R. Davies, K. Devlin, T. Feltwell, S. Gentles, N. Hamlin, S. Holroyd, T. Hornsby, K. Jagels, A. Krogh, J. Mclean, S. Moule, L. Murphy, K. Oliver, J. Osborne, M. A. Quail, M.-A. Rajandream, J. Rogers, S. Rutter, K. Seeger, J. Skelton, R. Squares, S. Squares, J. E. Sulston, K. Taylor, S. Whitehead, and B. G. Barrel. 1998. Deciphering the biology of Mycobacterium tuberculosis from the complete genome sequence. Nature 393:537-544. [DOI] [PubMed] [Google Scholar]
- 28.Comstock, G. W., S. F. Woolpert, and V. T. Livesay. 1976. Tuberculosis studies in Muscogee County, Georgia. Twenty-year evaluation of a community trial of BCG vaccination. Public Health Rep. 91:276-280. [PMC free article] [PubMed] [Google Scholar]
- 29.Conradt, P., J. Hess, and S. H. Kaufmann. 1999. Cytolytic T-cell responses to human dendritic cells and macrophages infected with Mycobacterium bovis BCG and recombinant BCG secreting listeriolysin. Microbes Infect. 1:753-764. [DOI] [PubMed] [Google Scholar]
- 30.Cooper, A. M., D. K. Dalton, T. A. Stewart, J. P. Griffin, D. G. Russell, and I. M. Orme. 1993. Disseminated tuberculosis in interferon gamma gene-disrupted mice. J. Exp. Med. 178:2243-2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dascher, C. C., and M. B. Brenner. 2003. CD1 antigen presentation and infectious disease. Contrib. Microbiol. 10:164-182. [DOI] [PubMed] [Google Scholar]
- 32.de Boer, A. S., and D. van Soolingen. 2000. Recurrent tuberculosis due to exogenous reinfection. N. Engl. J. Med. 342:1050-1051. [PubMed] [Google Scholar]
- 33.de Jong, R., F. Altare, I. A. Haagen, D. G. Elferink, T. Boer, P. J. van Breda Vriesman, P. J. Kabel, J. M. Draaisma, J. T. van Dissel, F. P. Kroon, J. L. Casanova, and T. H. Ottenhoff. 1998. Severe mycobacterial and Salmonella infections in interleukin-12 receptor-deficient patients. Science 280:1435-1438. [DOI] [PubMed] [Google Scholar]
- 34.de Lisle, G. W., B. J. Wards, B. M. Buddle, and D. M. Collins. 2005. The efficacy of live tuberculosis vaccines after presensitization with Mycobacterium avium. Tuberculosis (Edinburgh) 85:73-79. [DOI] [PubMed] [Google Scholar]
- 35.Delogu, G., and M. J. Brennan. 2001. Comparative immune response to PE and PE_PGRS antigens of Mycobacterium tuberculosis. Infect. Immun. 69:5606-5611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Demissie, A., M. Abebe, A. Aseffa, G. Rook, H. Fletcher, A. Zumla, K. Weldingh, I. Brock, P. Andersen, and T. M. Doherty. 2004. Healthy individuals that control a latent infection with Mycobacterium tuberculosis express high levels of Th1 cytokines and the IL-4 antagonist IL-4delta2. J. Immunol. 172:6938-6943. [DOI] [PubMed] [Google Scholar]
- 37.Dieli, F., N. Caccamo, S. Meraviglia, J. Ivanyi, G. Sireci, C. T. Bonanno, V. Ferlazzo, C. La Mendola, and A. Salerno. 2004. Reciprocal stimulation of gammadelta T cells and dendritic cells during the anti-mycobacterial immune response. Eur. J. Immunol. 34:3227-3235. [DOI] [PubMed] [Google Scholar]
- 38.Dieli, F., J. Ivanyi, P. Marsh, A. Williams, I. Naylor, G. Sireci, N. Caccamo, C. Di Sano, and A. Salerno. 2003. Characterization of lung gamma delta T cells following intranasal infection with Mycobacterium bovis bacillus Calmette-Guerin. J. Immunol. 170:463-469. [DOI] [PubMed] [Google Scholar]
- 39.Dietrich, J., C. Aagaard, R. Leah, A. W. Olsen, A. Stryhn, T. M. Doherty, and P. Andersen. 2005. Exchanging ESAT6 with TB10.4 in an Ag85B Fusion Molecule-Based Tuberculosis Subunit Vaccine: Efficient Protection and ESAT6-Based Sensitive Monitoring of Vaccine Efficacy. J. Immunol. 174:6332-6339. [DOI] [PubMed] [Google Scholar]
- 40.Doherty, T. M., A. Demissie, J. Olobo, D. Wolday, S. Britton, T. Eguale, P. Ravn, and P. Andersen. 2002. Immune responses to the Mycobacterium tuberculosis-specific antigen ESAT-6 signal subclinical infection among contacts of tuberculosis patients. J. Clin. Microbiol. 40:704-706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Doherty, T. M., A. W. Olsen, L. van Pinxteren, and P. Andersen. 2002. Oral vaccination with subunit vaccines protects animals against aerosol infection with Mycobacterium tuberculosis. Infect. Immun. 70:3111-3121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Doherty, T. M., A. W. Olsen, J. Weischenfeldt, K. Huygen, S. D'Souza, T. K. Kondratieva, V. V. Yeremeev, A. S. Apt, B. Raupach, L. Grode, S. H. E. Kaufmann, and P. Andersen. 2004. Comparative analysis of different vaccine constructs expressing defined antigens from Mycobacterium tuberculosis. J. Infect. Dis. In Press. [DOI] [PubMed]
- 43.Downing, K. J., V. V. Mischenko, M. O. Shleeva, D. I. Young, M. Young, A. S. Kaprelyants, A. S. Apt, and V. Mizrahi. 2005. Mutants of Mycobacterium tuberculosis lacking three of the five rpf-like genes are defective for growth in vivo and for resuscitation in vitro. Infect. Immun. 73:3038-3043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Espitia, C., J. P. Laclette, M. Mondragon-Palomino, A. Amador, J. Campuzano, A. Martens, M. Singh, R. Cicero, Y. Zhang, and C. Moreno. 1999. The PE-PGRS glycine-rich proteins of Mycobacterium tuberculosis: a new family of fibronectin-binding proteins? Microbiology. 145:3487-3495. [DOI] [PubMed] [Google Scholar]
- 45.Feng, C. G., C. M. Collazo-Custodio, M. Eckhaus, S. Hieny, Y. Belkaid, K. Elkins, D. Jankovic, G. A. Taylor, and A. Sher. 2004. Mice deficient in LRG-47 display increased susceptibility to mycobacterial infection associated with the induction of lymphopenia. J. Immunol. 172:1163-1168. [DOI] [PubMed] [Google Scholar]
- 46.Fine, P. E. 1998. Vaccines, genes and trials. Novartis Found Symp. 217:57-69; discussion 69-72. [DOI] [PubMed] [Google Scholar]
- 47.Fine, P. E. 1995. Variation in protection by BCG: implications of and for heterologous immunity. Lancet 346:1339-1345. [DOI] [PubMed] [Google Scholar]
- 48.Fletcher, H. A., P. Owiafe, D. Jeffries, P. Hill, G. A. Rook, A. Zumla, T. M. Doherty, and R. H. Brookes. 2004. Increased expression of mRNA encoding interleukin (IL)-4 and its splice variant IL-4delta2 in cells from contacts of Mycobacterium tuberculosis, in the absence of in vitro stimulation. Immunology. 112:669-673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fortune, S. M., A. Solache, A. Jaeger, P. J. Hill, J. T. Belisle, B. R. Bloom, E. J. Rubin, and J. D. Ernst. 2004. Mycobacterium tuberculosis inhibits macrophage responses to IFN-gamma through myeloid differentiation factor 88-dependent and -independent mechanisms. J. Immunol. 172:6272-6280. [DOI] [PubMed] [Google Scholar]
- 50.Fouts, T. R., A. L. DeVico, D. Y. Onyabe, M. T. Shata, K. C. Bagley, G. K. Lewis, and D. M. Hone. 2003. Progress toward the development of a bacterial vaccine vector that induces high-titer long-lived broadly neutralizing antibodies against HIV-1. FEMS Immunol. Med. Microbiol. 37:129-134. [DOI] [PubMed] [Google Scholar]
- 51.Francis, J. 1956. Natural and experimental tuberculosis in monkeys; with observations on immunization and chemotherapy. J Comp. Pathol. 66:123-135. [DOI] [PubMed] [Google Scholar]
- 52.Fratti, R. A., J. Chua, I. Vergne, and V. Deretic. 2003. Mycobacterium tuberculosis glycosylated phosphatidylinositol causes phagosome maturation arrest. Proc. Natl. Acad. Sci. USA 100:5437-5442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fulton, S. A., S. M. Reba, R. K. Pai, M. Pennini, M. Torres, C. V. Harding, and W. H. Boom. 2004. Inhibition of major histocompatibility complex II expression and antigen processing in murine alveolar macrophages by Mycobacterium bovis BCG and the 19-kilodalton mycobacterial lipoprotein. Infect. Immun. 72:2101-2110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Geijtenbeek, T. B., S. J. Van Vliet, E. A. Koppel, M. Sanchez-Hernandez, C. M. Vandenbroucke-Grauls, B. Appelmelk, and Y. Van Kooyk. 2003. Mycobacteria target DC-SIGN to suppress dendritic cell function. J Exp. Med. 197:7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gonzalez-Juarrero, M., O. C. Turner, J. Turner, P. Marietta, J. V. Brooks, and I. M. Orme. 2001. Temporal and spatial arrangement of lymphocytes within lung granulomas induced by aerosol infection with Mycobacterium tuberculosis. Infect. Immun. 69:1722-1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Goonetilleke, N. P., H. McShane, C. M. Hannan, R. J. Anderson, R. H. Brookes, and A. V. Hill. 2003. Enhanced immunogenicity and protective efficacy against Mycobacterium tuberculosis of bacille Calmette-Guerin vaccine using mucosal administration and boosting with a recombinant modified vaccinia virus Ankara. J. Immunol. 171:1602-1609. [DOI] [PubMed] [Google Scholar]
- 57.Grode, L., M. Kursar, J. Fensterle, S. H. Kaufmann, and J. Hess. 2002. Cell-mediated immunity induced by recombinant Mycobacterium bovis Bacille Calmette-Guerin strains against an intracellular bacterial pathogen: importance of antigen secretion or membrane-targeted antigen display as lipoprotein for vaccine efficacy. J. Immunol. 168:1869-1876. [DOI] [PubMed] [Google Scholar]
- 58.Gupta, R. K., and G. R. Siber. 1995. Adjuvants for human vaccines-current status, problems and future prospects. Vaccine 13:1263-1276. [DOI] [PubMed] [Google Scholar]
- 59.Harboe, M., T. Oettinger, H. G. Wiker, I. Rosenkrands, and P. Andersen. 1996. Evidence for occurrence of the ESAT-6 protein in Mycobacterium tuberculosis and virulent Mycobacterium bovis and for its absence in Mycobacterium bovis BCG. Infect. Immun. 64:16-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hart, P. D. 1967. Efficacy and applicability of mass BCG vaccination in tuberculosis control. Br. Med. J. 1:587-592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hart, P. D., and I. Sutherland. 1977. BCG and vole bacillus vaccines in the prevention of tuberculosis in adolescence and early adult life. Br Med. J. 2:293-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.He, Q., A. R. Mitchell, S. L. Johnson, C. Wagner-Bartak, T. Morcol, and S. J. Bell. 2000. Calcium phosphate nanoparticle adjuvant. Clin. Diagn. Lab Immunol. 7:899-903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hogarth, P. J., K. J. Jahans, R. Hecker, R. G. Hewinson, and M. A. Chambers. 2003. Evaluation of adjuvants for protein vaccines against tuberculosis in guinea pigs. Vaccine 21:977-982. [DOI] [PubMed] [Google Scholar]
- 64.Holten-Andersen, L., T. M. Doherty, K. S. Korsholm, and P. Andersen. 2004. Combination of the cationic surfactant dimethyl dioctadecyl ammonium bromide and synthetic mycobacterial cord factor as an efficient adjuvant for tuberculosis subunit vaccines. Infect. Immun. 72:1608-1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Honer zu Bentrup, K., and D. G. Russell. 2001. Mycobacterial persistence: adaptation to a changing environment. Trends Microbiol. 9:597-605. [DOI] [PubMed] [Google Scholar]
- 66.Hori, S., and S. Sakaguchi. 2004. Foxp3: a critical regulator of the development and function of regulatory T cells. Microbes Infect. 6:745-751. [DOI] [PubMed] [Google Scholar]
- 67.Horwitz, M. A., and G. Harth. 2003. A new vaccine against tuberculosis affords greater survival after challenge than the current vaccine in the guinea pig model of pulmonary tuberculosis. Infect. Immun. 71:1672-1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hovav, A. H., J. Mullerad, L. Davidovitch, Y. Fishman, F. Bigi, A. Cataldi, and H. Bercovier. 2003. The Mycobacterium tuberculosis recombinant 27-kilodalton lipoprotein induces a strong Th1-type immune response deleterious to protection. Infect. Immun. 71:3146-3154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hsu, T., S. M. Hingley-Wilson, B. Chen, M. Chen, A. Z. Dai, P. M. Morin, C. B. Marks, J. Padiyar, C. Goulding, M. Gingery, D. Eisenberg, R. G. Russell, S. C. Derrick, F. M. Collins, S. L. Morris, C. H. King, and W. R. Jacobs, Jr. 2003. The primary mechanism of attenuation of bacillus Calmette-Guerin is a loss of secreted lytic function required for invasion of lung interstitial tissue. Proc. Natl. Acad. Sci. USA 100:12420-12425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Huckriede, A., L. Bungener, T. Daemen, and J. Wilschut. 2003. Influenza virosomes in vaccine development. Methods Enzymol. 373:74-91. [DOI] [PubMed] [Google Scholar]
- 71.Indrigo, J., R. L. Hunter, Jr., and J. K. Actor. 2003. Cord factor trehalose 6,6′-dimycolate (TDM) mediates trafficking events during mycobacterial infection of murine macrophages. Microbiology. 149:2049-2059. [DOI] [PubMed] [Google Scholar]
- 72.Iseman, M. D. 2002. Tuberculosis therapy: past, present and future. Eur. Respir. J. Suppl. 36:87s-94s. [DOI] [PubMed] [Google Scholar]
- 73.Jalapathy, K. V., C. Prabha, and S. D. Das. 2004. Correlates of protective immune response in tuberculous pleuritis. FEMS Immunol. Med. Microbiol. 40:139-145. [DOI] [PubMed] [Google Scholar]
- 74.Jimenez-Martinez, M. C., M. Linares, R. Baez, L. F. Montano, S. Martinez-Cairo, P. Gorocica, R. Chavez, E. Zenteno, and R. Lascurain. 2004. Intracellular expression of interleukin-4 and interferon-gamma by a Mycobacterium tuberculosis antigen-stimulated CD4+ CD57+ T-cell subpopulation with memory phenotype in tuberculosis patients. Immunology. 111:100-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jo, E. K., J. K. Park, and H. M. Dockrell. 2003. Dynamics of cytokine generation in patients with active pulmonary tuberculosis. Curr. Opin. Infect. Dis. 16:205-210. [DOI] [PubMed] [Google Scholar]
- 76.Jouanguy, E., F. Altare, S. Lamhamedi, P. Revy, J. F. Emile, M. Newport, M. Levin, S. Blanche, E. Seboun, A. Fischer, and J. L. Casanova. 1996. Interferon-gamma-receptor deficiency in an infant with fatal bacille Calmette-Guerin infection. N. Engl. J. Med. 335:1956-1961. [DOI] [PubMed] [Google Scholar]
- 77.Kamath, A. T., U. Fruth, M. J. Brennan, R. Dobbelaer, P. Hubrechts, M. M. Ho, R. E. Mayner, J. Thole, K. B. Walker, M. Liu, and P. H. Lambert. 2005. New live mycobacterial vaccines: the Geneva consensus on essential steps towards clinical development. Vaccine 23:3753-3761. [DOI] [PubMed] [Google Scholar]
- 78.Kaufmann, S. H., and C. H. Ladel. 1994. Role of T-cell subsets in immunity against intracellular bacteria: experimental infections of knock-out mice with Listeria monocytogenes and Mycobacterium bovis BCG. Immunobiology. 191:509-519. [DOI] [PubMed] [Google Scholar]
- 79.Kelley, V. A., and J. S. Schorey. 2003. Mycobacterium's arrest of phagosome maturation in macrophages requires Rab5 activity and accessibility to iron. Mol. Biol Cell. 14:3366-3377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Koch, R. 1982. Classics in infectious diseases. The etiology of tuberculosis: Robert Koch. Berlin, Germany 1882. Rev. Infect. Dis. 4:1270-1274. [PubMed] [Google Scholar]
- 81.Korf, J., A. Stoltz, J. Verschoor, P. De Baetselier, and J. Grooten. 2005. The Mycobacterium tuberculosis cell wall component mycolic acid elicits pathogen-associated host innate immune responses. Eur. J. Immunol. 35:890-900. [DOI] [PubMed] [Google Scholar]
- 82.Ladel, C. H., C. Blum, A. Dreher, K. Reifenberg, and S. H. Kaufmann. 1995. Protective role of gamma/delta T cells and alpha/beta T cells in tuberculosis. Eur. J. Immunol. 25:2877-2881. [DOI] [PubMed] [Google Scholar]
- 83.Ladel, C. H., S. Daugelat, and S. H. Kaufmann. 1995. Immune response to Mycobacterium bovis bacille Calmette Guerin infection in major histocompatibility complex class I- and II-deficient knock-out mice: contribution of CD4 and CD8 T cells to acquired resistance. Eur. J. Immunol. 25:377-384. [DOI] [PubMed] [Google Scholar]
- 84.Ladel, C. H., J. Hess, S. Daugelat, P. Mombaerts, S. Tonegawa, and S. H. Kaufmann. 1995. Contribution of alpha/beta and gamma/delta T lymphocytes to immunity against Mycobacterium bovis bacillus Calmette Guerin: studies with T-cell receptor-deficient mutant mice. Eur. J. Immunol. 25:838-846. [DOI] [PubMed] [Google Scholar]
- 85.Lalvani, A., P. Nagvenkar, Z. Udwadia, A. A. Pathan, K. A. Wilkinson, J. S. Shastri, K. Ewer, A. V. Hill, A. Mehta, and C. Rodrigues. 2001. Enumeration of T cells specific for RD1-encoded antigens suggests a high prevalence of latent Mycobacterium tuberculosis infection in healthy urban Indians. J. Infect. Dis. 183:469-477. [DOI] [PubMed] [Google Scholar]
- 86.Lalvani, A., A. A. Pathan, H. Durkan, K. A. Wilkinson, A. Whelan, J. J. Deeks, W. H. Reece, M. Latif, G. Pasvol, and A. V. Hill. 2001. Enhanced contact tracing and spatial tracking of Mycobacterium tuberculosis infection by enumeration of antigen-specific T cells. Lancet 357:2017-2021. [DOI] [PubMed] [Google Scholar]
- 87.Lalvani, A., A. A. Pathan, H. McShane, R. J. Wilkinson, M. Latif, C. P. Conlon, G. Pasvol, and A. V. Hill. 2001. Rapid detection of Mycobacterium tuberculosis infection by enumeration of antigen-specific T cells. Am. J. Respir. Crit. Care Med. 163:824-828. [DOI] [PubMed] [Google Scholar]
- 88.Lee, R. E., P. J. Brennan, and G. S. Besra. 1996. Mycobacterium tuberculosis cell envelope. Curr. Top. Microbiol. Immunol. 215:1-27. [DOI] [PubMed] [Google Scholar]
- 89.Leung, C. C., C. M. Tam, S. L. Chan, M. Chan-Yeung, C. K. Chan, and K. C. Chang. 2001. Efficacy of the BCG revaccination programme in a cohort given BCG vaccination at birth in Hong Kong. Int J. Tuberc. Lung Dis. 5:717-723. [PubMed] [Google Scholar]
- 90.Lienhardt, C., A. Azzurri, A. Amedei, K. Fielding, J. Sillah, O. Y. Sow, B. Bah, M. Benagiano, A. Diallo, R. Manetti, K. Manneh, P. Gustafson, S. Bennett, M. M. D'Elios, K. McAdam, and G. Del Prete. 2002. Active tuberculosis in Africa is associated with reduced Th1 and increased Th2 activity in vivo. Eur. J. Immunol. 32:1605-1613. [DOI] [PubMed] [Google Scholar]
- 91.Lillebaek, T., A. Dirksen, I. Baess, B. Strunge, V. O. Thomsen, and A. B. Andersen. 2002. Molecular evidence of endogenous reactivation of Mycobacterium tuberculosis after 33 years of latent infection. J. Infect. Dis. 185:401-404. [DOI] [PubMed] [Google Scholar]
- 92.Lindblad, E. B., M. J. Elhay, R. Silva, R. Appelberg, and P. Andersen. 1997. Adjuvant modulation of immune responses to tuberculosis subunit vaccines. Infect. Immun. 65:623-629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lingnau, K., A. Egyed, C. Schellack, F. Mattner, M. Buschle, and W. Schmidt. 2002. Poly-L-arginine synergizes with oligodeoxynucleotides containing CpG-motifs (CpG-ODN) for enhanced and prolonged immune responses and prevents the CpG-ODN-induced systemic release of pro-inflammatory cytokines. Vaccine 20:3498-3508. [DOI] [PubMed] [Google Scholar]
- 94.Long, R., and M. Gardam. 2003. Tumour necrosis factor-alpha inhibitors and the reactivation of latent tuberculosis infection. Cmaj. 168:1153-1156. [PMC free article] [PubMed] [Google Scholar]
- 95.Lowrie, D. B., R. E. Tascon, V. L. Bonato, V. M. Lima, L. H. Faccioli, E. Stavropoulos, M. J. Colston, R. G. Hewinson, K. Moelling, and C. L. Silva. 1999. Therapy of tuberculosis in mice by DNA vaccination. Nature 400:269-271. [DOI] [PubMed] [Google Scholar]
- 96.Lozes, E., O. Denis, A. Drowart, F. Jurion, K. Palfliet, A. Vanonckelen, J. De Bruyn, M. De Cock, J. P. Van Vooren, and K. Huygen. 1997. Cross-reactive immune responses against Mycobacterium bovis BCG in mice infected with non-tuberculous mycobacteria belonging to the MAIS-Group. Scand. J. Immunol. 46:16-26. [DOI] [PubMed] [Google Scholar]
- 97.Lyashchenko, K., A. O. Whelan, R. Greenwald, J. M. Pollock, P. Andersen, R. G. Hewinson, and H. M. Vordermeier. 2004. Association of tuberculin-boosted antibody responses with pathology and cell-mediated immunity in cattle vaccinated with Mycobacterium bovis BCG and infected with M. bovis. Infect. Immun. 72:2462-2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.MacMicking, J. D., G. A. Taylor, and J. D. McKinney. 2003. Immune control of tuberculosis by IFN-gamma-inducible LRG-47. Science 302:654-659. [DOI] [PubMed] [Google Scholar]
- 99.Majlessi, L., P. Brodin, R. Brosch, M. J. Rojas, H. Khun, M. Huerre, S. T. Cole, and C. Leclerc. 2005. Influence of ESAT-6 secretion system 1 (RD1) of Mycobacterium tuberculosis on the interaction between mycobacteria and the host immune system. J. Immunol. 174:3570-3579. [DOI] [PubMed] [Google Scholar]
- 100.Malik, Z. A., S. S. Iyer, and D. J. Kusner. 2001. Mycobacterium tuberculosis phagosomes exhibit altered calmodulin-dependent signal transduction: contribution to inhibition of phagosome-lysosome fusion and intracellular survival in human macrophages. J. Immunol. 166:3392-3401. [DOI] [PubMed] [Google Scholar]
- 101.Manca, C., M. B. Reed, S. Freeman, B. Mathema, B. Kreiswirth, C. E. Barry, 3rd, and G. Kaplan. 2004. Differential monocyte activation underlies strain-specific Mycobacterium tuberculosis pathogenesis. Infect. Immun. 72:5511-5514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Marchant, A., A. Amedei, A. Azzurri, J. Vekemans, M. Benagiano, C. Tamburini, C. Lienhardt, T. Corrah, K. P. McAdam, S. Romagnani, M. M. D'Elios, and G. Del Prete. 2001. Polarization of PPD-specific T-cell response of patients with tuberculosis from Th0 to Th1 profile after successful antimycobacterial therapy or in vitro conditioning with interferon-alpha or interleukin-12. Am. J. Respir. Cell Mol. Biol. 24:187-194. [DOI] [PubMed] [Google Scholar]
- 103.Mattner, F., J. K. Fleitmann, K. Lingnau, W. Schmidt, A. Egyed, J. Fritz, W. Zauner, B. Wittmann, I. Gorny, M. Berger, H. Kirlappos, A. Otava, M. L. Birnstiel, and M. Buschle. 2002. Vaccination with poly-l-arginine as immunostimulant for peptide vaccines: induction of potent and long-lasting T-cell responses against cancer antigens. Cancer Res. 62:1477-1480. [PubMed] [Google Scholar]
- 104.McShane, H., A. A. Pathan, C. R. Sander, S. M. Keating, S. C. Gilbert, K. Huygen, H. A. Fletcher, and A. V. Hill. 2004. Recombinant modified vaccinia virus Ankara expressing antigen 85A boosts BCG-primed and naturally acquired antimycobacterial immunity in humans. Nat. Med. 10:1240-1244. [DOI] [PubMed] [Google Scholar]
- 105.Means, T. K., S. Wang, E. Lien, A. Yoshimura, D. T. Golenbock, and M. J. Fenton. 1999. Human toll-like receptors mediate cellular activation by Mycobacterium tuberculosis. J. Immunol. 163:3920-3927. [PubMed] [Google Scholar]
- 106.Mehrotra, J., and W. R. Bishai. 2001. Regulation of virulence genes in Mycobacterium tuberculosis. Int. J. Med. Microbiol. 291:171-182. [DOI] [PubMed] [Google Scholar]
- 107.Meraldi, V., R. Audran, J. F. Romero, V. Brossard, J. Bauer, J. A. Lopez, and G. Corradin. 2003. OM-174, a new adjuvant with a potential for human use, induces a protective response when administered with the synthetic C-terminal fragment 242-310 from the circumsporozoite protein of Plasmodium berghei. Vaccine 21:2485-2491. [DOI] [PubMed] [Google Scholar]
- 108.Mollenkopf, H. J., M. Kursar, and S. H. Kaufmann. 2004. Immune response to postprimary tuberculosis in mice: Mycobacterium tuberculosis and Miycobacterium bovis bacille Calmette-Guerin induce equal protection. J Infect. Dis. 190:588-597. [DOI] [PubMed] [Google Scholar]
- 109.Morein, B., M. Villacres-Eriksson, J. Ekstrom, K. Hu, S. Behboudi, and K. Lovgren-Bengtsson. 1999. ISCOM: a delivery system for neonates and for mucosal administration. Adv. Vet. Med. 41:405-413. [DOI] [PubMed] [Google Scholar]
- 110.Morita, C. T., Y. Tanaka, B. R. Bloom, and M. B. Brenner. 1996. Direct presentation of non-peptide prenyl pyrophosphate antigens to human gamma delta T cells. Res. Immunol. 147:347-353. [DOI] [PubMed] [Google Scholar]
- 111.Nathan, C., and M. U. Shiloh. 2000. Reactive oxygen and nitrogen intermediates in the relationship between mammalian hosts and microbial pathogens. Proc. Natl. Acad. Sci. USA 97:8841-8848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Noss, E. H., R. K. Pai, T. J. Sellati, J. D. Radolf, J. Belisle, D. T. Golenbock, W. H. Boom, and C. V. Harding. 2001. Toll-like receptor 2-dependent inhibition of macrophage class II MHC expression and antigen processing by 19-kDa lipoprotein of Mycobacterium tuberculosis. J. Immunol. 167:910-918. [DOI] [PubMed] [Google Scholar]
- 113.Nuzzo, I., M. Galdiero, C. Bentivoglio, R. Galdiero, and C. Romano Carratelli. 2002. Apoptosis modulation by mycolic acid, tuberculostearic acid and trehalose 6,6′-dimycolate. J. Infect. 44:229-235. [DOI] [PubMed] [Google Scholar]
- 114.O'Regan, A., and M. Joyce-Brady. 2001. Latent tuberculosis may persist for over 40 years. Br. Med. J. 323:635. [PMC free article] [PubMed] [Google Scholar]
- 115.Oiso, R., N. Fujiwara, H. Yamagami, S. Maeda, S. Matsumoto, S. Nakamura, N. Oshitani, T. Matsumoto, T. Arakawa, and K. Kobayashi. 2005. Mycobacterial trehalose 6,6′-dimycolate preferentially induces type 1 helper T-cell responses through signal transducer and activator of transcription 4 protein. Microb. Pathog. 39:35-43. [DOI] [PubMed] [Google Scholar]
- 116.Olobo, J. O., M. Geletu, A. Demissie, T. Eguale, K. Hiwot, G. Aderaye, and S. Britton. 2001. Circulating TNF-alpha, TGF-beta, and IL-10 in tuberculosis patients and healthy contacts. Scand. J. Immunol. 53:85-91. [DOI] [PubMed] [Google Scholar]
- 117.Olsen, A. W., A. Williams, L. M. Okkels, G. Hatch, and P. Andersen. 2004. Protective effect of a tuberculosis subunit vaccine based on a fusion of antigen 85B and ESAT-6 in the aerosol guinea pig model. Infect. Immun. 72:6148-6150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ordway, D. J., L. Costa, M. Martins, H. Silveira, L. Amaral, M. J. Arroz, F. A. Ventura, and H. M. Dockrell. 2004. Increased interleukin-4 production by CD8 and gammadelta T cells in health-care workers is associated with the subsequent development of active tuberculosis. J. Infect. Dis. 190:756-766. [DOI] [PubMed] [Google Scholar]
- 119.Ordway, D. J., L. Pinto, L. Costa, M. Martins, C. Leandro, M. Viveiros, L. Amaral, M. J. Arroz, F. A. Ventura, and H. M. Dockrell. 2005. Gamma delta T-cell responses associated with the development of tuberculosis in health care workers. FEMS Immunol. Med. Microbiol. 43:339-350. [DOI] [PubMed] [Google Scholar]
- 120.Pai, R. K., M. E. Pennini, A. A. Tobian, D. H. Canaday, W. H. Boom, and C. V. Harding. 2004. Prolonged toll-like receptor signaling by Mycobacterium tuberculosis and its 19-kilodalton lipoprotein inhibits gamma interferon-induced regulation of selected genes in macrophages. Infect. Immun. 72:6603-6614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Peppoloni, S., P. Ruggiero, M. Contorni, M. Morandi, M. Pizza, R. Rappuoli, A. Podda, and G. Del Giudice. 2003. Mutants of the Escherichia coli heat-labile enterotoxin as safe and strong adjuvants for intranasal delivery of vaccines. Expert Rev. Vaccines 2:285-293. [DOI] [PubMed] [Google Scholar]
- 122.Pethe, K., D. L. Swenson, S. Alonso, J. Anderson, C. Wang, and D. G. Russell. 2004. Isolation of Mycobacterium tuberculosis mutants defective in the arrest of phagosome maturation. Proc. Natl. Acad. Sci. USA 101:13642-13647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Podda, A., and G. Del Giudice. 2003. MF59-adjuvanted vaccines: increased immunogenicity with an optimal safety profile. Expert Rev. Vaccines 2:197-203. [DOI] [PubMed] [Google Scholar]
- 124.Pym, A. S., P. Brodin, L. Majlessi, R. Brosch, C. Demangel, A. Williams, K. E. Griffiths, G. Marchal, C. Leclerc, and S. T. Cole. 2003. Recombinant BCG exporting ESAT-6 confers enhanced protection against tuberculosis. Nat. Med. 9:533-539. [DOI] [PubMed] [Google Scholar]
- 125.Quesniaux, V., C. Fremond, M. Jacobs, S. Parida, D. Nicolle, V. Yeremeev, F. Bihl, F. Erard, T. Botha, M. Drennan, M. N. Soler, M. Le Bert, B. Schnyder, and B. Ryffel. 2004. Toll-like receptor pathways in the immune responses to mycobacteria. Microbes Infect. 6:946-959. [DOI] [PubMed] [Google Scholar]
- 126.Rahemtulla, A., W. P. Fung-Leung, M. W. Schilham, T. M. Kundig, S. R. Sambhara, A. Narendran, A. Arabian, A. Wakeham, C. J. Paige, R. M. Zinkernagel, et al. 1991. Normal development and function of CD8+ cells but markedly decreased helper cell activity in mice lacking CD4. Nature 353:180-184. [DOI] [PubMed] [Google Scholar]
- 127.Rao, V., N. Dhar, and A. K. Tyagi. 2003. Modulation of host immune responses by overexpression of immunodominant antigens of Mycobacterium tuberculosis in bacille Calmette-Guerin. Scand. J. Immunol. 58:449-461. [DOI] [PubMed] [Google Scholar]
- 128.Ravn, P., A. Demissie, T. Eguale, H. Wondwosson, D. Lein, H. A. Amoudy, A. S. Mustafa, A. K. Jensen, A. Holm, I. Rosenkrands, F. Oftung, J. Olobo, F. von Reyn, and P. Andersen. 1999. Hum. T-cell responses to the ESAT-6 antigen from Mycobacterium tuberculosis. J. Infect. Dis. 179:637-645. [DOI] [PubMed] [Google Scholar]
- 128a.Raynaud, C., C. Guilhot, J. Rauzier, Y. Bordat, V. Pelicic, R. Manganelli, I. Smith, B. Gicquel, and M. Jackson. 2002. Phospholipases C are involved in the virulence of Mycobacterium tuberculosis. Mol. Microbiol. 45:203-217. [DOI] [PubMed] [Google Scholar]
- 129.Reed, M. B., P. Domenech, C. Manca, H. Su, A. K. Barczak, B. N. Kreiswirth, G. Kaplan, and C. E. Barry 3rd. 2004. A glycolipid of hypervirulent tuberculosis strains that inhibits the innate immune response. Nature 431:84-87. [DOI] [PubMed] [Google Scholar]
- 130.Rolph, M. S., B. Raupach, H. H. Kobernick, H. L. Collins, B. Perarnau, F. A. Lemonnier, and S. H. Kaufmann. 2001. MHC class Ia-restricted T cells partially account for beta2-microglobulin-dependent resistance to Mycobacterium tuberculosis. Eur. J. Immunol. 31:1944-1949. [DOI] [PubMed] [Google Scholar]
- 131.Rook, G. A., and J. L. Stanford. 1996. The Koch phenomenon and the immunopathology of tuberculosis. Curr. Top. Microbiol. Immunol. 215:239-262. [DOI] [PubMed] [Google Scholar]
- 132.Roura-Mir, C., and D. B. Moody. 2003. Sorting out self and microbial lipid antigens for CD1. Microbes Infect. 5:1137-1148. [DOI] [PubMed] [Google Scholar]
- 133.Russell, D. G. 2001. Mycobacterium tuberculosis: here today, and here tomorrow. Nat. Rev. Mol. Cell. Biol. 2:569-577. [DOI] [PubMed] [Google Scholar]
- 134.Russell, D. G., J. Dant, and S. Sturgill-Koszycki. 1996. Mycobacterium avium- and Mycobacterium tuberculosis-containing vacuoles are dynamic, fusion-competent vesicles that are accessible to glycosphingolipids from the host cell plasmalemma. J. Immunol. 156:4764-4773. [PubMed] [Google Scholar]
- 135.Ryll, R., Y. Kumazawa, and I. Yano. 2001. Immunological properties of trehalose dimycolate (cord factor) and other mycolic acid-containing glycolipids-a review. Microbiol. Immunol. 45:801-811. [DOI] [PubMed] [Google Scholar]
- 136.Ryll, R., K. Watanabe, N. Fujiwara, H. Takimoto, R. Hasunuma, Y. Kumazawa, M. Okada, and I. Yano. 2001. Mycobacterial cord factor, but not sulfolipid, causes depletion of NKT cells and upregulation of CD1d1 on murine macrophages. Microbes Infect. 3:611-619. [DOI] [PubMed] [Google Scholar]
- 137.Sambandamurthy, V. K., S. C. Derrick, K. V. Jalapathy, B. Chen, R. G. Russell, S. L. Morris, and W. R. Jacobs, Jr. 2005. Long-term protection against tuberculosis following vaccination with a severely attenuated double lysine and pantothenate auxotroph of Mycobacterium tuberculosis. Infect. Immun. 73:1196-1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Sampson, S. L., C. C. Dascher, V. K. Sambandamurthy, R. G. Russell, W. R. Jacobs, Jr., B. R. Bloom, and M. K. Hondalus. 2004. Protection elicited by a double leucine and pantothenate auxotroph of Mycobacterium tuberculosis in guinea pigs. Infect. Immun. 72:3031-3037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Schaible, U. E., and S. H. Kaufmann. 2000. CD1 molecules and CD1-dependent T cells in bacterial infections: a link from innate to acquired immunity? Semin. Immunol. 12:527-535. [DOI] [PubMed] [Google Scholar]
- 140.Schaible, U. E., S. Sturgill-Koszycki, P. H. Schlesinger, and D. G. Russell. 1998. Cytokine activation leads to acidification and increases maturation of Mycobacterium avium-containing phagosomes in murine macrophages. J. Immunol. 160:1290-1296. [PubMed] [Google Scholar]
- 141.Seah, G. T., and G. A. Rook. 2001. High levels of mRNA encoding IL-4 in unstimulated peripheral blood mononuclear cells from tuberculosis patients revealed by quantitative nested reverse transcriptase-polymerase chain reaction; correlations with serum IgE levels. Scand. J. Infect. Dis. 33:106-109. [DOI] [PubMed] [Google Scholar]
- 142.Seah, G. T., G. M. Scott, and G. A. Rook. 2000. Type 2 cytokine gene activation and its relationship to extent of disease in patients with tuberculosis. J. Infect. Dis. 181:385-389. [DOI] [PubMed] [Google Scholar]
- 143.Serbina, N. V., and J. L. Flynn. 2001. CD8+ T cells participate in the memory immune response to Mycobacterium tuberculosis. Infect. Immun. 69:4320-4328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Shams, H., B. Wizel, S. E. Weis, B. Samten, and P. F. Barnes. 2001. Contribution of CD8+ T cells to gamma interferon production in human tuberculosis. Infect. Immun. 69:3497-3501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Sherman, D. R., M. Voskuil, D. Schnappinger, R. Liao, M. I. Harrell, and G. K. Schoolnik. 2001. Regulation of the Mycobacterium tuberculosis hypoxic response gene encoding alpha-crystallin. Proc. Natl. Acad. Sci. USA 98:7534-7539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Shi, L., Y. J. Jung, S. Tyagi, M. L. Gennaro, and R. J. North. 2003. Expression of Th1-mediated immunity in mouse lungs induces a Mycobacterium tuberculosis transcription pattern characteristic of nonreplicating persistence. Proc. Natl. Acad. Sci. USA 100:241-246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Shiloh, M. U., and C. F. Nathan. 2000. Reactive nitrogen intermediates and the pathogenesis of Salmonella and mycobacteria. Curr. Opin. Microbiol. 3:35-42. [DOI] [PubMed] [Google Scholar]
- 148.Siebenmann, C. O. 1951. Effect of BCG vaccination and chemotherapy on experimental tuberculosis in mice. J. Immunol. 67:137-149. [PubMed] [Google Scholar]
- 149.Singh, K. K., X. Zhang, A. S. Patibandla, P. Chien, Jr., and S. Laal. 2001. Antigens of Mycobacterium tuberculosis expressed during preclinical tuberculosis: serological immunodominance of proteins with repetitive amino acid sequences. Infect. Immun. 69:4185-4191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Skeiky, Y. A., M. R. Alderson, P. J. Ovendale, J. A. Guderian, L. Brandt, D. C. Dillon, A. Campos-Neto, Y. Lobet, W. Dalemans, I. M. Orme, and S. G. Reed. 2004. Differential immune responses and protective efficacy induced by components of a tuberculosis polyprotein vaccine, Mtb72F, delivered as naked DNA or recombinant protein. J. Immunol. 172:7618-7628. [DOI] [PubMed] [Google Scholar]
- 151.Skjot, R. L., I. Brock, S. M. Arend, M. E. Munk, M. Theisen, T. H. Ottenhoff, and P. Andersen. 2002. Epitope mapping of the immunodominant antigen TB10.4 and the two homologous proteins TB10.3 and TB12.9, which constitute a subfamily of the ESAT-6 gene family. Infect. Immun. 70:5446-5453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Smith, D. W. 1985. Protective effect of BCG in experimental tuberculosis. Adv. Tuberc. Res. 22:1-97. [PubMed] [Google Scholar]
- 153.Smith, P. G. 1994. BCG vaccination, p. 297-310. In P. D. O. Davies (ed.), Clinical tuberculosis, 1st ed. Chapman and Hall Medical, London, England.
- 154.Sorensen, A. L., S. Nagai, G. Houen, P. Andersen, and A. B. Andersen. 1995. Purification and characterization of a low-molecular-mass T-cell antigen secreted by Mycobacterium tuberculosis. Infect. Immun. 63:1710-1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Sousa, A. O., R. J. Mazzaccaro, R. G. Russell, F. K. Lee, O. C. Turner, S. Hong, L. Van Kaer, and B. R. Bloom. 2000. Relative contributions of distinct MHC class I-dependent cell populations in protection to tuberculosis infection in mice. Proc. Natl. Acad. Sci. USA 97:4204-4208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Stenger, S. 2001. Cytolytic T cells in the immune response to mycobacterium tuberculosis. Scand. J. Infect. Dis. 33:483-487. [DOI] [PubMed] [Google Scholar]
- 157.Stenger, S., and R. L. Modlin. 2002. Control of Mycobacterium tuberculosis through mammalian Toll-like receptors. Curr. Opin. Immunol. 14:452-457. [DOI] [PubMed] [Google Scholar]
- 158.Sterne, J. A., L. C. Rodrigues, and I. N. Guedes. 1998. Does the efficacy of BCG decline with time since vaccination? Int. J. Tuberc. Lung Dis. 2:200-207. [PubMed] [Google Scholar]
- 159.Stokes, R. W., R. Norris-Jones, D. E. Brooks, T. J. Beveridge, D. Doxsee, and L. M. Thorson. 2004. The glycan-rich outer layer of the cell wall of Mycobacterium tuberculosis acts as an antiphagocytic capsule limiting the association of the bacterium with macrophages. Infect. Immun. 72:5676-5686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Sturgill-Koszycki, S., P. H. Schlesinger, P. Chakraborty, P. L. Haddix, H. L. Collins, A. K. Fok, R. D. Allen, S. L. Gluck, J. Heuser, and D. G. Russell. 1994. Lack of acidification in Mycobacterium phagosomes produced by exclusion of the vesicular proton-ATPase. Science 263:678-681. [DOI] [PubMed] [Google Scholar]
- 161.Sugawara, I., T. Udagawa, S. C. Hua, M. Reza-Gholizadeh, K. Otomo, Y. Saito, and H. Yamada. 2002. Pulmonary granulomas of guinea pigs induced by inhalation exposure of heat-treated BCG Pasteur, purified trehalose dimycolate and methyl ketomycolate. J. Med. Microbiol. 51:131-137. [DOI] [PubMed] [Google Scholar]
- 162.Takeuchi, O., S. Sato, T. Horiuchi, K. Hoshino, K. Takeda, Z. Dong, R. L. Modlin, and S. Akira. 2002. Cutting edge: role of Toll-like receptor 1 in mediating immune response to microbial lipoproteins. J. Immunol. 169:10-14. [DOI] [PubMed] [Google Scholar]
- 163.Tiberio, L., L. Fletcher, J. H. Eldridge, and D. D. Duncan. 2004. Host factors impacting the innate response in humans to the candidate adjuvants RC529 and monophosphoryl lipid A. Vaccine 22:1515-1523. [DOI] [PubMed] [Google Scholar]
- 164.Ting, L. M., A. C. Kim, A. Cattamanchi, and J. D. Ernst. 1999. Mycobacterium tuberculosis inhibits IFN-gamma transcriptional responses without inhibiting activation of STAT1. J. Immunol. 163:3898-3906. [PubMed] [Google Scholar]
- 165.Tufariello, J. M., W. R. Jacobs, Jr., and J. Chan. 2004. Individual Mycobacterium tuberculosis resuscitation-promoting factor homologues are dispensable for growth in vitro and in vivo. Infect. Immun. 72:515-526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Turner, J., T. Corrah, S. Sabbally, H. Whittle, and H. M. Dockrell. 2000. A longitudinal study of in vitro IFNgamma production and cytotoxic T-cell responses of tuberculosis patients in the Gambia. Tuberc. Lung Dis. 80:161-169. [DOI] [PubMed] [Google Scholar]
- 167.Turner, J., E. R. Rhoades, M. Keen, J. T. Belisle, A. A. Frank, and I. M. Orme. 2000. Effective preexposure tuberculosis vaccines fail to protect when they are given in an immunotherapeutic mode. Infect. Immun. 68:1706-1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Turner, O. C., A. D. Roberts, A. A. Frank, S. W. Phalen, D. M. McMurray, J. Content, O. Denis, S. D'Souza, A. Tanghe, K. Huygen, and I. M. Orme. 2000. Lack of protection in mice and necrotizing bronchointerstitial pneumonia with bronchiolitis in guinea pigs immunized with vaccines directed against the hsp60 molecule of Mycobacterium tuberculosis. Infect. Immun. 68:3674-3679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Ulrich, J. T., and K. R. Myers. 1995. Monophosphoryl lipid A as an adjuvant. Past experiences and new directions. Pharm. Biotechnol. 6:495-524. [PubMed] [Google Scholar]
- 170.Ulrichs, T., D. B. Moody, E. Grant, S. H. Kaufmann, and S. A. Porcelli. 2003. T-cell responses to CD1-presented lipid antigens in humans with Mycobacterium tuberculosis infection. Infect. Immun. 71:3076-3087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Ulrichs, T., and S. A. Porcelli. 2000. CD1 proteins: targets of T-cell recognition in innate and adaptive immunity. Rev. Immunogenet. 2:416-432. [PubMed] [Google Scholar]
- 172.Underhill, D. M., A. Ozinsky, K. D. Smith, and A. Aderem. 1999. Toll-like receptor-2 mediates mycobacteria-induced proinflammatory signaling in macrophages. Proc. Natl. Acad. Sci. USA 96:14459-14463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.van Crevel, R., E. Karyadi, F. Preyers, M. Leenders, B. J. Kullberg, R. H. Nelwan, and J. W. van der Meer. 2000. Increased production of interleukin 4 by CD4+ and CD8+ T cells from patients with tuberculosis is related to the presence of pulmonary cavities. J. Infect. Dis. 181:1194-1197. [DOI] [PubMed] [Google Scholar]
- 174.van Pinxteren, L. A., J. P. Cassidy, B. H. Smedegaard, E. M. Agger, and P. Andersen. 2000. Control of latent Mycobacterium tuberculosis infection is dependent on CD8 T cells. Eur. J. Immunol. 30:3689-3698. [DOI] [PubMed] [Google Scholar]
- 175.van Pinxteren, L. A. H., P. Ravn, E. M. Agger, J. M. Pollock, and P. Andersen. 2000. Diagnosis of tuberculosis based on the two specific antigens ESAT-6 and CFP10. Clin. Diagn. Lab Immunol. 7:155-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Vekemans, J., C. Lienhardt, J. S. Sillah, J. G. Wheeler, G. P. Lahai, M. T. Doherty, T. Corrah, P. Andersen, K. P. McAdam, and A. Marchant. 2001. Tuberculosis contacts but not patients have higher gamma interferon responses to ESAT-6 than do community controls in the Gambia. Infect. Immun. 69:6554-6557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Vergne, I., J. Chua, and V. Deretic. 2003. Tuberculosis toxin blocking phagosome maturation inhibits a novel Ca2+/calmodulin-PI3K hVPS34 cascade. J Exp. Med. 198:653-659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Vergne, I., R. A. Fratti, P. J. Hill, J. Chua, J. Belisle, and V. Deretic. 2004. Mycobacterium tuberculosis phagosome maturation arrest: mycobacterial phosphatidylinositol analog phosphatidylinositol mannoside stimulates early endosomal fusion. Mol. Biol. Cell 15:751-760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Vogels, R., D. Zuijdgeest, R. van Rijnsoever, E. Hartkoorn, I. Damen, M. P. de Bethune, S. Kostense, G. Penders, N. Helmus, W. Koudstaal, M. Cecchini, A. Wetterwald, M. Sprangers, A. Lemckert, O. Ophorst, B. Koel, M. van Meerendonk, P. Quax, L. Panitti, J. Grimbergen, A. Bout, J. Goudsmit, and M. Havenga. 2003. Replication-deficient human adenovirus type 35 vectors for gene transfer and vaccination: efficient human cell infection and bypass of preexisting adenovirus immunity. J. Virol. 77:8263-8271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Vordermeier, H. M., M. A. Chambers, P. J. Cockle, A. O. Whelan, J. Simmons, and R. G. Hewinson. 2002. Correlation of ESAT-6-specific gamma interferon production with pathology in cattle following Mycobacterium bovis BCG vaccination against experimental bovine tuberculosis. Infect. Immun. 70:3026-3032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Voskuil, M. I., D. Schnappinger, K. C. Visconti, M. I. Harrell, G. M. Dolganov, D. R. Sherman, and G. K. Schoolnik. 2003. Inhibition of respiration by nitric oxide induces a Mycobacterium tuberculosis dormancy program. J Exp. Med. 198:705-713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Wagner, D., J. Maser, B. Lai, Z. Cai, C. E. Barry, 3rd, K. Honer Zu Bentrup, D. G. Russell, and L. E. Bermudez. 2005. Elemental analysis of Mycobacterium avium-, Mycobacterium tuberculosis-, and Mycobacterium smegmatis-containing phagosomes indicates pathogen-induced microenvironments within the host cell's endosomal system. J. Immunol. 174:1491-1500. [DOI] [PubMed] [Google Scholar]
- 183.Walburger, A., A. Koul, G. Ferrari, L. Nguyen, C. Prescianotto-Baschong, K. Huygen, B. Klebl, C. Thompson, G. Bacher, and J. Pieters. 2004. Protein kinase G from pathogenic mycobacteria promotes survival within macrophages. Science 304:1800-1804. [DOI] [PubMed] [Google Scholar]
- 184.Weinrich Olsen, A., L. A. van Pinxteren, L. Meng Okkels, P. Birk Rasmussen, and P. Andersen. 2001. Protection of mice with a tuberculosis subunit vaccine based on a fusion protein of antigen 85B and ESAT-6. Infect. Immun. 69:2773-2778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Welsh, M. D., R. T. Cunningham, D. M. Corbett, R. M. Girvin, J. McNair, R. A. Skuce, D. G. Bryson, and J. M. Pollock. 2005. Influence of pathological progression on the balance between cellular and humoral immune responses in bovine tuberculosis. Immunology 114:101-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Wiart, A., A. Jepson, W. Banya, S. Bennett, H. Whittle, N. G. Martin, and A. V. Hill. 2004. Quantitative association tests of immune responses to antigens of Mycobacterium tuberculosis: a study of twins in West Africa. Twin Res. 7:578-588. [DOI] [PubMed] [Google Scholar]
- 187.Williams, A., G. J. Hatch, S. O. Clark, K. E. Gooch, K. A. Hatch, G. A. Hall, K. Huygen, T. H. Ottenhoff, K. L. Franken, P. Andersen, T. M. Doherty, S. H. Kaufmann, L. Grode, P. Seiler, C. Martin, B. Gicquel, S. T. Cole, P. Brodin, A. S. Pym, W. Dalemans, J. Cohen, Y. Lobet, N. Goonetilleke, H. McShane, A. Hill, T. Parish, D. Smith, N. G. Stoker, D. B. Lowrie, G. Kallenius, S. Svenson, A. Pawlowski, K. Blake, and P. D. Marsh. 2005. Evaluation of vaccines in the EU TB Vaccine Cluster using a guinea pig aerosol infection model of tuberculosis. Tuberculosis (Edinburgh) 85:29-38. [DOI] [PubMed] [Google Scholar]
- 188.Wilson, M. E., H. V. Fineberg, and G. A. Colditz. 1995. Geographic latitude and the efficacy of bacillus Calmette-Guerin vaccine. Clin. Infect. Dis. 20:982-991. [DOI] [PubMed] [Google Scholar]
- 189.Winau, F., S. H. Kaufmann, and U. E. Schaible. 2004. Apoptosis paves the detour path for CD8 T-cell activation against intracellular bacteria. Cell. Microbiol. 6:599-607. [DOI] [PubMed] [Google Scholar]
- 190.Yeremeev, V. V., T. K. Kondratieva, E. I. Rubakova, S. N. Petrovskaya, K. A. Kazarian, M. V. Telkov, S. F. Biketov, A. S. Kaprelyants, and A. S. Apt. 2003. Proteins of the Rpf family: immune cell reactivity and vaccination efficacy against tuberculosis in mice. Infect. Immun. 71:4789-4794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Yeremeev, V. V., I. V. Lyadova, B. V. Nikonenko, A. S. Apt, C. Abou-Zeid, J. Inwald, and D. B. Young. 2000. The 19-kD antigen and protective immunity in a murine model of tuberculosis. Clin. Exp. Immunol. 120:274-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Yuan, Y., D. D. Crane, and C. E. Barry 3rd. 1996. Stationary-phase-associated protein expression in Mycobacterium tuberculosis: function of the mycobacterial alpha-crystallin homolog. J. Bacteriol. 178:4484-4492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Yuan, Y., D. D. Crane, R. M. Simpson, Y. Q. Zhu, M. J. Hickey, D. R. Sherman, and C. E. Barry 3rd. 1998. The 16-kDa alpha-crystallin (Acr) protein of Mycobacterium tuberculosis is required for growth in macrophages. Proc. Natl. Acad. Sci. USA 95:9578-9583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Ziv, E., C. L. Daley, and S. Blower. 2004. Potential public health impact of new tuberculosis vaccines. Emerg. Infect. Dis. 10:1529-1535. [DOI] [PMC free article] [PubMed] [Google Scholar]