Abstract
The use of tympanic thermometry is attractive in primary care, but a recent systematic review highlighted the paucity of data comparing tympanic thermometry with conventional methods. We report a study of 94 preschool children presenting to primary care in the United Kingdom (UK) with acute cough in whom tympanic infrared and axillary mercury thermometry are compared. Infrared thermometry showed poor agreement, poor sensitivity and high specificity. Infrared thermometry is too insensitive to be used as a screening test for fever, but when fever is already suspected, for example by touch, it may be useful as a ‘rule in’ test.
Keywords: body temperature, children, cough, fever, preschool, thermometers
Introduction
THE presence of fever has implications for the diagnosis,1 prognosis2,3 and treatment2 of patients, although there are little data on how widespread the use of thermometry is in primary care.4 Mercury-in-glass thermometers are likely to be phased out as environmental pressure to reduce the use of mercury increases. Some European countries have already imposed bans.5 Infrared ear thermometry is both convenient and acceptable compared with mercury thermometry, which takes too much time, and rectal thermometry, which is unacceptable to patients and clinicians.
A recent systematic review and meta-analysis of evidence comparing infrared ear thermometry with rectal temperature measurement in children suggests the mean difference (rectal − ear = 0.29°C, 95% limits of agreement = −0.7°C to 1.3°C) is too large to justify the widespread use of infrared thermometry.6 However, the authors only presented the mean difference, which is a measure of the systematic difference between the methods. This does not assess the diagnostic value of infrared thermometry for the detection of fever. In addition, only two of the 44 studies included were conducted in primary care.7,8
When assessing a new test, two types of comparison are possible; agreement and accuracy. The first investigates the extent to which the results of one test resemble another, while the second addresses the extent to which a test will successfully detect the target disorder, in this case fever.9 Agreement makes no assumptions about which is better, while accuracy holds one measure, known as the ‘gold standard’, superior to the other. In reality, it may not be known whether one test really is a gold standard, but making this assumption allows the generation of useful data, particularly with respect to the clinical question about the detection of fever.
Therefore, the aim of this study was to use both approaches to compare infrared tympanic and mercury axillary thermometry in children presenting to primary care.
Method
We compared thermometry in a cohort of 116 preschool children presenting with acute cough to eight practices during one winter. The ‘gold standard’ temperature was measured using a standard mercury thermometer placed in the axilla for 5 minutes.10 The tympanic membrane temperature was measured according to the manufacturer's instructions using an Omron Gentle TempTM (model MC-509-E) calibrated by the manufacturer prior to the study onset. The ‘ear tug’ technique was used to straighten the curvature of the canal.
For agreement, the tympanic membrane reading was subtracted from the axillary reading and then the method comparison techniques described by Bland and Altman were used to investigate the possible levels of individual differences between the measurement approaches and the overall (mean) systematic bias between them.9 Specifically, the mean and standard deviation of the differences, the ‘limits of agreement’ (that is, the 95% reference range for individual differences) and 95% confidence intervals (CIs) for the limits of agreement and for the mean itself, were calculated. For accuracy, a contingency table was constructed, and sensitivity, specificity and likelihood ratios (with 95% CI)11 were calculated using a cut-off for fever of temperatures higher than 37.0°C. The likelihood ratios were used to calculate the post-test probability of fever.12
HOW THIS FITS IN
What do we know?
Mercury is a hazardous substance and there is environmental pressure to reduce its use. Its convenience makes infrared thermometry an attractive alternative in primary care.
What does this paper add?
Infrared thermometry shows poor agreement, poor sensitivity and high specificity compared with established methods for the detection of fever in primary care.
Results
We had complete thermometry data for 94 (81%) children recruited to the cohort. Mean mercury and infrared temperatures were 36.7°C (range = 34.9–38.5°C) and 35.7°C (range = 33.3–39.3°C), respectively. The mean (standard deviation) difference between the axillary and tympanic measures was 1.18°C (0.96°C), and the limits of agreement were therefore −0.73 to 3.09°C. The 95% CI for the limits of agreement were −0.39 to −1.07, and 2.75 to 3.43, respectively. The 95% CI for the mean difference was 0.98 to 1.76. The figure suggests that agreement tended to deteriorate with falling temperatures. Table 1 shows that 20 (21%) of the children were febrile as judged by the gold standard method and four (4%) by infrared thermometry. Table 2 shows the sensitivity, specificity likelihood ratios and post-test probabilities of fever.
Table 1.
Contingency table comparing fever detection by mercury (gold standard) and infrared thermometry.
| Thermometer | Mercury (gold standard) | |||
|---|---|---|---|---|
| Raised | Normal | Total | ||
| Infrared | Raised | 3 | 1 | 4 |
| Normal | 17 | 73 | 90 | |
| Total | 20 | 74 | 94 | |
Table 2.
Sensitivity, specificity, likelihood ratios and post-test probabilities of fever.
| Test parameter | Result (95% CI) |
|---|---|
| Sensitivity (%) | 15.0 (3.2 to 37.9) |
| Specificity (%) | 98.6 (92.7 to 99.9) |
| Positive likelihood ratio | 11.1 (1.2 to 101) |
| Negative likelihood ratio | 0.86 (0.71 to 1.04) |
| Pre-test probability of fever | 0.21 (0.13 to 0.31) |
| Post-test probability of fever with positive result | 0.75 (0.25 to 0.96) |
| Post-test probability of fever with negative result | 0.19 (0.16 to 0.22) |
Discussion
The mean difference and limits of agreement are too large for this tympanic thermometer to replace the mercury thermometer in normal clinical practice. Given that the mean temperature differences found in previous systematic reviews suggest that rectal thermometry reads higher than axillary (by 0.25°C)13 and tympanic thermometry (by 0.29°C),6 we might have expected to find a small mean temperature difference, in the region of 0.04°C. Therefore, the mean difference found in our study is surprisingly large, at 1.18°C. Possible explanations for this include meta-analytic pooling of results in the two systematic reviews decreasing larger, more extreme results from single studies; differences in the method used to measure temperature; the instrument model used; or that children attending primary care may have less severe fevers (lower temperatures were associated with lower levels of agreement). We found some infrared temperatures that were lower than normal body temperature. This may be due to an insufficiently straightened ear canal or earwax obstructing the path of heat radiating from the tympanic membrane.
Our study shows that infrared thermometry was poor at detecting febrile children (sensitivity = 15%), but a positive test meant fever was usually present (post-test probability of 0.75). The precision of the estimates for some of the test parameters are poor, reflecting the small number of children with fever.
Our findings add further evidence to support the conclusion of the systematic review.6 On the evidence available to date, infrared thermometry does not show sufficient agreement to replace established methods in primary care. If clinicians wish to detect all children with fever in their surgeries, then infrared thermometry is too insensitive, and will miss 85% of febrile children. On the other hand, if fever is already clinically suspected, for example through the use of touch,14 then infrared thermometry may be useful to ‘rule in’ fever. Even so, clinicians need to be aware that an elevated infrared measurement is correct in only three-quarters of children.
Further research is needed to examine when and how temperature is measured in primary care and to examine the accuracy of infrared and other measures in patients in whom fever is clinically suspected.
Figure 1.
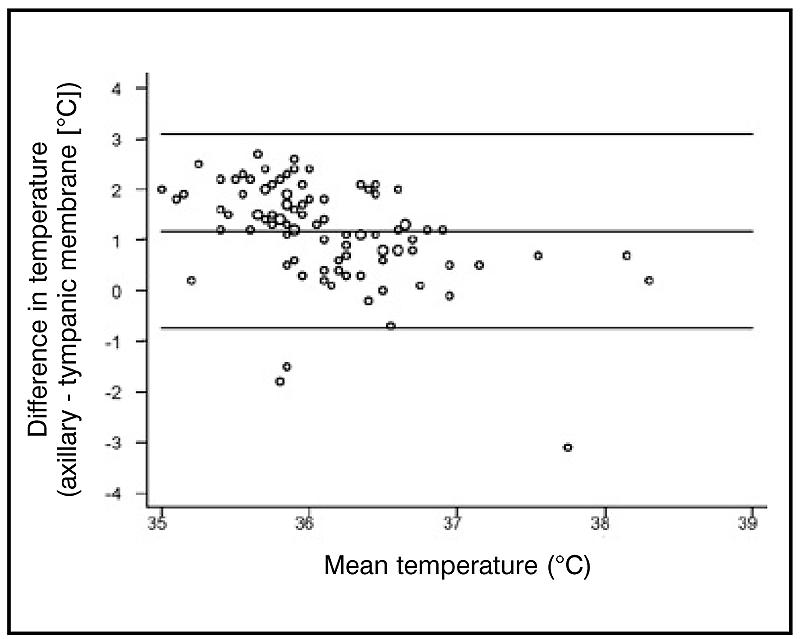
Plot of the difference between axillary and tympanic temperature readings against their mean.
Acknowledgments
We wish to thank OMRON Healthcare (UK) Limited, who supplied the infrared thermometer, the Trent Focus Collaborative Research Network, the eight Leicestershire practices, and the patients who participated in this study. The study was supported by a grant from the Department of General Practice and Primary Health Care, University of Leicester.
References
- 1.Stocks N, Fahey T. Labelling of acute respiratory illness: evidence of between-practitioner variation in the UK. Fam Pract. 2002;19:375–377. doi: 10.1093/fampra/19.4.375. [DOI] [PubMed] [Google Scholar]
- 2.Little P, Gould C, Moore M, et al. Predictors of poor outcome and benefits from antibiotics in children with acute otitis media: pragmatic randomised trial. BMJ. 2002;325:22. doi: 10.1136/bmj.325.7354.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hay AD, Fahey T, Peters TJ, Wilson AD. Predicting complications from acute cough in preschool children in primary care: a prospective cohort study. Br J Gen Pract. 2004;54:9–14. [PMC free article] [PubMed] [Google Scholar]
- 4.Clarke S. Use of thermometers in general practice. BMJ. 1992;304:961–963. doi: 10.1136/bmj.304.6832.961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Medical Devices Agency. Medical devices containing mercury — current position in the UK and Europe. London: Medical Devices Agency; 2003. [Google Scholar]
- 6.Craig JV, Lancaster GA, Taylor S, et al. Infrared ear thermometry compared with rectal thermometry in children: a systematic review. Lancet. 2002;360:603–609. doi: 10.1016/S0140-6736(02)09783-0. [DOI] [PubMed] [Google Scholar]
- 7.Petersen-Smith A, Barber N, Coody D, et al. Comparison of aural infrared with traditional rectal temperatures in children from birth to age three years. J Pediatr. 1994;125:83–85. doi: 10.1016/s0022-3476(94)70129-6. [DOI] [PubMed] [Google Scholar]
- 8.Wilshaw R, Beckstrand R, Waid D, Schaalje GB. A comparison of the use of tympanic, axillary, and rectal thermometers in infants. J Pediatr Nurs. 1999;14:88–93. doi: 10.1016/S0882-5963(99)80042-6. [DOI] [PubMed] [Google Scholar]
- 9.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 10.Coggon DN, Vessey MP. Errors in using clinical thermometers. BMJ. 1976;1:692. doi: 10.1136/bmj.1.6011.692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simel DL, Samsa GP, Matchar DB. Likelihood ratios with confidence: sample size estimation for diagnostic test studies. J Clin Epidemiol. 1991;44:763–770. doi: 10.1016/0895-4356(91)90128-v. [DOI] [PubMed] [Google Scholar]
- 12.Sackett DL, Haynes R, Guyatt GH, Tugwell P. Clinical epidemiology: a basic science for clinical medicine. Boston: Little, Brown and Company; 1991. [Google Scholar]
- 13.Craig JV, Lancaster GA, Williamson PR, Smyth RL. Temperature measured at the axilla compared with rectum in children and young people: systematic review. BMJ. 2000;320:1174–1178. doi: 10.1136/bmj.320.7243.1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Whybrew K, Murray M, Morley C. Diagnosing fever by touch: observational study. BMJ. 1998;317:321–330. doi: 10.1136/bmj.317.7154.321. [DOI] [PMC free article] [PubMed] [Google Scholar]


