Abstract
Background
The UK Colorectal Cancer Screening Pilot has recently been completed to evaluate the feasibility of screening using the faecal occult blood test. Screening will be phased in over the next several years, and it is important to consider the impact on the NHS workforce.
Aim
To determine the impact of the UK Colorectal Cancer Screening Pilot on primary care workload.
Design of study
A retrospective survey and prospective audit of general practice staff.
Setting
General practice.
Method
Workload impact was assessed using a postal questionnaire and a prospective audit of activity in participating practices. Questionnaires were sent to practices that had been involved in the Pilot between 6 weeks and 1 year previously. They were sent to a random sample of 59 practices in Scotland and 60 practices in England between February 2001 and March 2002. Audit forms were sent prospectively to 60 practices involved in the Pilot between May 2001 and September 2002.
Results
Sixty-seven per cent of GPs, 82% of practice managers, 69% of practice nurses, and 70% of receptionists responded to the questionnaire. Of 60 practices contacted to take part in the workload audit, 38 returned completed ‘workload impact audit’ forms. Most practice staff indicated they spent 2% or less of their time during the screening period on Pilot-related activities. Forty per cent of GPs thought that a national colorectal cancer screening programme would substantially impact on the workload in primary care. However, there were variations by country: practice staff in Scotland were more likely to think that it would substantially impact on workload than practice staff in England (44.7% versus 26.6%).
Conclusions
The surveys and audit demonstrate that the Pilot has had a discernible, albeit modest, impact on workload in primary care. Workload of particular significance to primary care personnel includes increases in paperwork, administration, and information provision to patients. The majority of primary care staff support the introduction of a colorectal cancer screening programme. However, there is a strong perception, particularly among GPs, that a national programme of faecal occult blood test screening will impact significantly on workload in primary care, and that primary care-based activities generated through screening should be adequately resourced and remunerated.
Keywords: cancer screening, primary health care, workload, evaluation
INTRODUCTION
Colorectal cancer is the second most common cause of cancer-related death in the Western world. Each year there are over 30 000 new cases of colorectal cancer in the UK with an average 5-year survival of 40%.1,2 The rationale and evidence in support of colorectal screening is strong; screening tests can detect cancers at an earlier stage, while randomised controlled trial and case-control evidence suggest that removal of adenomatous polyps reduces the incidence of colorectal cancer, and that mortality can be reduced by detection of early-stage tumours.3–9
The UK's four Departments of Health have recently completed a UK Colorectal Cancer Screening Pilot to determine the feasibility of screening for colorectal cancer in the UK population using the faecal occult blood test. Invitations were sent to approximately 480 000 people via mail from dedicated screening centres in Rugby and Dundee. We undertook the study reported here as part of an independent, multidisciplinary evaluation of the UK Colorectal Cancer Screening Pilot, commissioned by the Department of Health. The main outputs of the evaluation of this UK Pilot have been reported elsewhere.10 Taking into account the findings of this evaluation report on the UK Colorectal Cancer Screening Pilot, the UK Department of Health has re-affirmed their commitment to introduce a national colorectal cancer screening programme subject to advice from the UK National Screening Committee. The planning and phasing in of the screening programme is expected to take around 5 years and will include consideration of a range of issues including any findings from a trial examining flexible sigmoidoscopy screening.11,12
A national faecal occult blood test screening programme will have a workload impact well beyond the immediate services resourced through the programme. The introduction of a national programme will need to carefully examine existing capacity and potential to accommodate increased activity, at both a national and regional level.
One of the key tasks of our evaluation has been to determine the impact of faecal occult blood test screening on primary and hospital acute services, both directly and indirectly. This article focuses on primary care issues (particularly workload impact). Primary care provides support to the screening process, even when recruitment and follow-up are undertaken outside of primary care — as was the case in this UK Colorectal Cancer Screening Pilot. Although in the UK, cancer screening programmes are coordinated by central NHS screening offices, tasks such as invitation, provision of screening, and information provision are shared between these central units and primary care providers.13,14 One of the concerns of the Pilot was that the workload impact of a screening programme on primary care would be excessive.
METHOD
The UK Pilot screened for colorectal cancer, practice by practice; all eligible patients (those aged 50–69 years) in a practice were invited for screening over a finite time period — usually 1–2 weeks. There were minor but important organisational differences between England and Scotland; for example, patients in Scotland went back to the GP for results of their colonoscopy, while in England they returned to the colonoscopy clinic to get their results. We sought in this study to investigate the impact on primary care of such differences in procedure.
We measured workload impact using a postal questionnaire and a prospective audit of activity in participating practices. Questionnaires and audit sheets were developed and piloted with the assistance of a primary care reference group comprising primary care, public health and screening unit personnel, and a local GP research network.
To identify sampling frames for both the questionnaire survey and the audit, the practice manager in each surgery was contacted by a member of the evaluation team. Lists of GPs and other staff present during the period of practice involvement were confirmed. Part-time GPs and GP registrars were included, but the practice manager was asked to make a judgement in excluding other staff whose appointments were fractional, or whose level of involvement in Pilot-related activities would, for any reason, be expected to be minimal. For example, no receptionists working less than a quarter of full-time equivalent (FTE) hours were included.
How this fits in
Although evidence from randomised controlled trials indicates that screening for colorectal cancer using the faecal occult blood test can reduce mortality, there has so far been little information available on how primary care could accommodate a new cancer screening programme. Existing evidence suggests that the involvement of primary care can improve uptake of screening, and any new programme would need to take account of current capacity and incentives within primary care. The surveys and audit reported here demonstrate that the Pilot has had a discernible, albeit modest, impact on workload in primary care. Aspects of this increased workload that appear to be of particular significance to primary care personnel include increases in paperwork, administration, and information provision to patients. There is a strong feeling, from GPs in particular, that a national programme of faecal occult blood test screening will have a significant impact on the workload of those engaged in primary care, and that remuneration and resources should be adjusted accordingly. There are regional differences on workload impact between England and Scotland. These could relate to the organisational differences between the two sites.
Questionnaires were sent to practices that had been involved in the Pilot between 6 weeks and no more than 1 year previously. They were sent to a random sample of 59 practices in Scotland (23% of total practices involved in the Pilot) and 60 practices in England (42% of English practices) between February 2001 and March 2002. The questionnaires were sent to GPs, practice nurses, receptionists, and practice managers (slightly different versions were sent to each staff group).
The audit relied on prospective documentation of activity by primary care staff in a 1-week period, after the invitations for faecal occult blood test screening had been sent out. It was conducted in practices as they were recruited to the Pilot, between May 2001 and September 2002. Where possible, all practices involved in the Pilot during this time period (n = 60), were invited to take part in the audit. Letters were sent in advance to all GPs and the practice manager telling them about the audit. Two weeks before the audit was due to commence, the practice manager was contacted to identify the number of staff for each different staff group. Colour-coded forms (for different types of practice staff) were placed in the reception areas, treatment rooms, and GP offices; staff were asked to note any enquiries or activities resulting from the Pilot, as they occurred. Activities of interest were enquiries from patients (including date, time, mode, and nature of the enquiry), organisational activities, discussions with staff, queries from the Pilot unit, and time spent with patients undergoing further investigations.
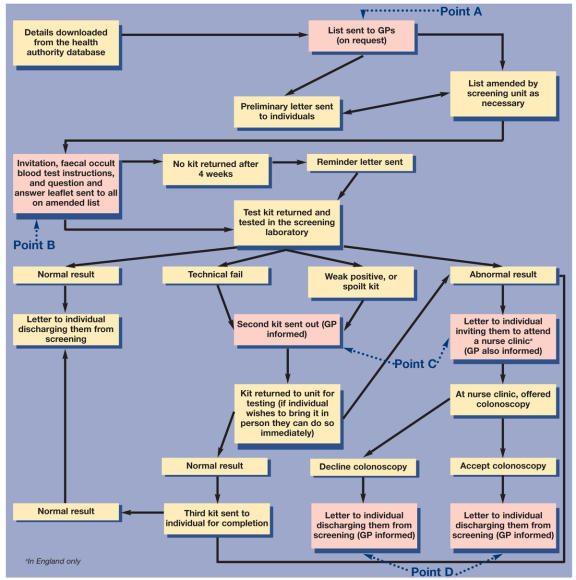
Figure 1 shows the pathway for colorectal cancer screening that was used in the UK Pilot and points to where primary care staff become involved. The audit focused on assessing the workload impact at point B (when invitations were sent out). The questionnaires asked practice staff primarily about checking the prior-notification lists (point A) and the busiest week following the sending out of invitations (point B). However, responders also had the opportunity to comment on the workload impact around points C and D. Types of activities undertaken by practice staff at each of these points are outlined in Table 1. The content of the questionnaires and audit is summarised in Box 1. Data were analysed using SPSS and SAS statistical packages. Free-text comments were coded and key concepts and themes were identified, using a content analysis approach.15
Figure 1.
Pathway for colorectal cancer screening using the faecal occult blood test.
Table 1.
Activities undertaken within primary care and the impact on primary care staff.
| Points where primary care is involved in screening activities | Activities undertaken within primary care process | Potential impact on primary care staff |
| Point A | ||
| Lists of potential participants (prior-notification lists) sent to general practices | Checking of prior notification lists for accuracy and completeness and the exclusion of patients for whom invitation for faecal occult blood tests would be clinically inappropriate | Increase in workload for one or more type of practice staff (for example, practice managers and GPs) |
| Point B | ||
| Invitations and faecal occult blood test kits sent out | Providing information on the test and screening programme | Increase in workload for receptionists (handling calls), and GPs and nurses (responding to enquiries). There may be a need for increased training |
| Point C | ||
| Results have been processed and associated correspondence sent | Filing of positive faecal occult blood tests | Increase in workload for administrative staff |
| Providing information to people on the meaning of their test result | Increase in consultations and or consultation time for GPs and/or nurses | |
| Providing counselling, advice, and support to people referred for further investigations | Increase in consultations and/or consultation time for GPs and/or nurses | |
| Point D | ||
| Ongoing treatment and surveillance | Filing of results/letters | Increase in workload for administrative staff |
| Providing ongoing support and counselling to people undergoing treatment | Increase in consultations for GPs | |
Box 1. Content of questionnaires and audit.
Questionnaires
Questionnaires included both structured and free-text fields.
▸ Views on workload issues related to colorectal cancer screening, for example, workload impact of a national programme.
▸ Pre-screening checking of patient lists.
▸ Workload impact, for example, telephone enquiries, consultations, discussions with staff, paperwork.
▸ Nature of the enquiries.
▸ Views on colorectal cancer screening.
▸ Demographic details.
Audit forms
Audit sheets were sent to individual GPs and practice managers. Receptionists and practice nurses filled out a collective form or individual ones on request.
▸ Nature of the enquiries.
▸ Other activities arising from the Colorectal Cancer Screening Pilot, for example, meetings, organisational activities.
RESULTS
A total of 856 questionnaires were returned (347 from Scottish practices and 509 from English practices). giving with an overall response rate of 70%. Sixty-seven per cent of GPs, 82% of practice managers, 69% of practice nurses, and 70% of practice receptionists responded to the questionnaire.
Of 60 practices contacted for the workload audit, 41 agreed to take part. Of these, 38 returned completed ‘workload impact audit’ forms; the total number of returned audit forms was 195.
Impact on workload from faecal occult blood test screening
Out of 290 GPs, 236 (81%) indicated they spent ‘2% or less’ of their time during the screening period on Pilot-related activities; this reported time commitment was similar in other staff categories. From the prospective audit we determined that the average length of time spent responding to enquiries over a 1-week period (when this was documented) was 4.2 minutes (standard deviation [sd]: 3.7 minutes, range 0.5–20 minutes). The mean length of time spent on ‘other activities’ (for example, administrative tasks, meetings) was 7.6 minutes over the 1-week period (sd: 11.3 minutes, range 0.3–60 minutes).
A major theme arising from the analysis of the free-text comments related to administrative tasks, such as checking patient lists before screening began, and filing results and associated correspondence for those patients with a positive faecal occult blood test. However, some practices reported no increase in administrative tasks, while others reported a significant increase.
Nature of enquiries
Among GPs, the most common enquiries were about whether or not to participate, concerns over positive results, and questions about bowel symptoms prompted by the Pilot (Table 2). Less common were advice on how to perform the test, confusion over information provided by the Pilot site, questions about the risks and benefits of screening, and explanation about subsequent stages in the screening process. A predominant theme in the analysis of free-text comments was the additional time involved with patients who were anxious following a test result, and awaiting further tests or results.
Table 2.
Nature of enquiries about faecal occult blood test screening.
| GP frequency (%) | Practice nurse frequency (%) | |||||
|---|---|---|---|---|---|---|
| Nature of enquiry | Very often | Often | Sometimes | Very often | Often | Sometimes |
| Instructions on how to perform the test | 2 (1.9) | 15 (13.9) | 91 (84.3) | 4 (5.5) | 18 (24.7) | 51 (69.9) |
| Advice on whether or not to participate | 14 (5.9) | 51 (21.5) | 172 (72.6) | 6 (7.5) | 19 (23.8) | 55 (68.8) |
| Concern/fear arising from positive results | 15 (6.3) | 55 (23.2) | 167 (70.5) | 3 (6.0) | 11 (22.0) | 36 (72.0) |
| Questions about bowel symptoms | 7 (4.7) | 35 (23.3) | 108 (72.0) | 4 (10.0) | 10 (25.0) | 26 (65.0) |
| Questions about the risks and benefits of screening | 3 (2.2) | 22 (15.9) | 113 (81.9) | 0 (0.0) | 16 (30.8) | 36 (69.2) |
| Explanation about the next stage | 6 (2.8) | 44 (20.9) | 161 (76.3) | 1 (2.7) | 4 (10.8) | 32 (86.5) |
There was a broadly similar pattern for practice nurses, although they were more likely to become involved in discussions over how to perform the test.
The self-reports of impact on personal workload from the Pilot were supplemented with views on the likely impact on workload, should faecal occult blood test screening be rolled out (Table 3). Forty per cent of GPs thought that a national colorectal cancer screening programme would substantially impact on the workload in primary care. The percentage was markedly lower among practice nurses (25%).
Table 3.
Views on whether a national programme would substantially impact on workload in primary care.
| Area | Response | GP frequency (%) | Practice nurse frequency (%) | All frequency (%) |
|---|---|---|---|---|
| Scotland | Yes | 88 (47.1) | 14 (34.2) | 102 (44.7) |
| No | 75 (40.1) | 22 (53.7) | 97 (42.5) | |
| Not sure | 24 (12.8) | 5 (12.2) | 29 (12.8) | |
| England | Yes | 40 (30.8) | 15 (19.5) | 55 (26.6) |
| No | 73 (56.2) | 44 (57.1) | 117 (56.5) | |
| Not sure | 17 (13.1) | 18 (23.4) | 35 (16.9) | |
| All | Yes | 128 (40.4) | 29 (24.6) | 157 (37.0) |
| No | 148 (46.7) | 66 (55.9) | 214 (49.2) | |
| Not sure | 41 (12.9) | 23 (19.5) | 64 (14.8) |
There were variations by country: practice staff members in Scotland were more likely to think that it would substantially impact on workload than practice staff in England: 44.7% (95% confidence interval [CI] = 20.6% to 32.6% ) versus 26.6% (95% CI = 38.3% to 51.2%) in Scotland.
Among GPs, a majority (55%) felt that general practice should be remunerated for this additional workload. The most common theme to emerge when asked about remuneration was the impact on workload and resources. In particular, practice staff members were concerned that they would not have the resources available to cope. Several responders commented on the need for additional human resources, such as nurses or clerical staff.
DISCUSSION
The role of primary care in a national screening programme for colorectal cancer has not yet been clarified. However, colorectal cancer screening presents unique challenges to primary care and further evidence on ways to improve the delivery and uptake of such a programme is required. Such effort is likely to be worthwhile, as evidence suggests that primary care can significantly improve important measures of colorectal cancer screening such as uptake.16 To consolidate this important role for primary care, a sustainable model of screening will be required that does not place an unrealistic burden on primary care.
Our results are partly based on self-reports in postal questionnaires sent to primary care personnel. It is difficult to validate responses; our concern is that they may have been based on impressions of workload impact rather than actual activity. Nevertheless, the results of the survey and the audit are broadly consistent. Further, as a means of enhancing the validity of responses, the questionnaire was developed with input from GPs who were participating in the Pilot, and these same GPs also examined survey responses and compared them with their own experiences. Similarly, the audit depended upon accurate and complete documentation of activity by practice personnel, without members of our study team present. Although we took all possible measures to raise awareness of the audit among staff in participating practices, there is no ‘gold standard’ validity check we can use on these data. Nevertheless, the Pilot itself was well-publicised among the practices, and staff were engaged in the process by visits from screening unit personnel and other within-practice promotional activities — this should, in theory motivate staff to provide accurate data. There were no particular incentives to either over- or underestimate activity in either the questionnaire surveys or audit.
Our results suggest that faecal occult blood test screening has a modest yet discernible impact on workload; although primary care has not been responsible for recruitment and delivery of screening in the UK Colorectal Cancer Screening Pilot, this evaluation indicates that extra work has been generated for primary care staff. This extra work has mainly been in the form of checking prior notification lists, filing letters and reports generated by the screening unit, and responding to the information needs of invitees.
We noted variations between England and Scotland in some key issues relating to workload impact. Indeed, more practice staff in Scotland than England thought that a programme would substantially impact on primary care. The difference in workload impact between England and Scotland is possibly due to differences in procedures for provision of results of investigations, scheduling arrangements for nurse visits in each of the two sites, and other organisational differences. These variations may provide important clues on strategies to reduce primary care impact. Many primary care personnel, particularly GPs, hold strong views about the capacity of primary care to accommodate a further form of cancer screening without additional dedicated resources.
As outlined in Table 1, a national screening programme for colorectal cancer impacts on primary care at four main points. However, it was difficult from this study to assess at which point primary care staff had the greatest workload. For some practices, checking of the prior-notification lists caused the most work. For others it was filing and responding to patient enquiries. The size of the practice and staffing levels (for example, some practices did not have practice managers) may affect the workload impact.
Our study shows that primary care staff act as information providers in faecal occult blood test screening. In the initial screening pathway, primary care staff were not intended to be involved at this point (information is sent to screening invitees by the screening unit). If general practice is overburdened with the task of information provision, then the screening programme may need to review its information strategy for screening invitees. Importantly, the majority of the workload impact of this screening Pilot on general practice is only for a finite period; screening takes place practice by practice over a 2-year cycle.
If general practice can accommodate a significant role in information provision, then it is in a position to increase informed choice in colorectal cancer screening. The National Screening Committee (which advises all four UK Departments of Health), now advises that individuals should make an informed choice over whether to be screened or not, and that limitations as well as the benefits of screening are made explicit to people who are participating in screening.17 In addition, recent guidance from the General Medical Council states that doctors must ensure that anyone considering whether to consent to screening can make a properly informed decision.18
The UK Pilot of Colorectal Cancer Screening has tested the feasibility of faecal occult blood test screening in the population. Results suggest that uptake rates of approximately 60% would be likely to be achieved in a national programme, and reductions in mortality seen in the randomised controlled trials would be replicated. An effective colorectal cancer screening programme requires the support of primary care; further evidence on ways to enhance and sustain the role of primary care in the delivery and uptake of such a programme is required.
Planning for UK-wide programmes of colorectal cancer screening is underway, although the timing of its introduction and the details of the programme in each of the four countries of the UK is still to be decided. Our paper adds weight to arguments in favour of addressing the issue of primary care involvement in cancer screening programmes. General practice in the UK is undergoing a period of significant change; new NHS contracts for consultant and general medical services over the next 2–3 years, and other elements of health service reform are likely to alter incentives and patterns of health service provision. Planning for a national programme needs to take into account this complex health service environment and the specific issues relating to primary care.
Funding body and reference number
This work was commissioned by the R&D Directorate, UK Department of Health
Ethics committee and reference number
MREC/00/0/26
Competing interests
None
Acknowledgments
The evaluation team received valuable input from the Department of Health's Advisory Group for the Pilot evaluation, and worked closely with the Executive and Steering Groups of the UK Pilot. The authors gratefully acknowledge the assistance of the GP practices and screening units involved in this work.
REFERENCES
- 1.Office of Population Censuses and Surveys. Cancer statistics. Registration 1989. England and Wales. London: HMSO; 1994. (Series MBI; No 22) [Google Scholar]
- 2.Sharp LS, Black RJ, Harkness EF, et al. Cancer registration statistics. Scotland 1981–90. Edinburgh: Information and Statistics Division; 1995. [Google Scholar]
- 3.Hardcastle JD, Chamberlain JO, Robinson MH, et al. Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet. 1996;348:1472–1477. doi: 10.1016/S0140-6736(96)03386-7. [DOI] [PubMed] [Google Scholar]
- 4.Kronborg O, Fenger C, Olsen J, et al. Randomised study of screening for colorectal cancer with faecal-occult-blood test. Lancet. 1996;348:1467–1471. doi: 10.1016/S0140-6736(96)03430-7. [DOI] [PubMed] [Google Scholar]
- 5.Selby JV, Friedman GD, Quesenberry CP, Jr, Weiss NS. A case-control study of screening sigmoidoscopy and mortality from colorectal cancer. N Engl J Med. 1992;326:653–657. doi: 10.1056/NEJM199203053261001. [DOI] [PubMed] [Google Scholar]
- 6.Mandel JS, Church TR, Bond JH, et al. The effect of fecal occult-blood screening on the incidence of colorectal cancer. N Engl J Med. 2000;343:1603–1607. doi: 10.1056/NEJM200011303432203. [DOI] [PubMed] [Google Scholar]
- 7.Scholefield JH, Moss S, Sufi F, et al. Effect of faecal occult blood screening on mortality from colorectal cancer: results from a randomised controlled trial. Gut. 2002;50:840–844. doi: 10.1136/gut.50.6.840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jorgensen OD, Kronborg O, Fenger C. A randomised study of screening for colorectal cancer using faecal occult blood testing: results after 13 years and seven biennial screening rounds. Gut. 2002;50:29–32. doi: 10.1136/gut.50.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Towler B, Irwig L, Glasziou P, et al. A systematic review of the effects of screening for colorectal cancer using the faecal occult blood test, Hemoccult. BMJ. 1998;317:559–565. doi: 10.1136/bmj.317.7158.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weller D, Alexander F, Orbell S, et al. Evaluation of the UK Colorectal Cancer Screening Pilot. A report for the UK Department of Health. London: Department of Health; 2003. www.cancerscreening.nhs.uk/colorectal/finalreport.pdf (accessed 8 Nov 2004) [Google Scholar]
- 11.Rhodes JM. Colorectal cancer screening in the UK: Joint Position Statement by the British Society of Gastroenterology, The Royal College of Physicians, and The Association of Coloproctology of Great Britain and Ireland. Gut. 2000;46:746–748. doi: 10.1136/gut.46.6.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Atkin WS, Edwards R, Wardle J, et al. Design of a multicentre randomised trial to evaluate flexible sigmoidoscopy in colorectal cancer screening. J Med Screen. 2001;8:137–144. doi: 10.1136/jms.8.3.137. [DOI] [PubMed] [Google Scholar]
- 13.Patnick J. Cervical cancer screening in England. Eur J Cancer. 2000;36:2205–2208. doi: 10.1016/s0959-8049(00)00310-5. [DOI] [PubMed] [Google Scholar]
- 14.Moss SM, Brown J, Garvican L, et al. Routine breast screening for women aged 65–69: results from evaluation of the demonstration sites. Br J Cancer. 2001;85:1289–1294. doi: 10.1054/bjoc.2001.2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bryman A. Social research methods. Oxford: Oxford University Press; 2001. [Google Scholar]
- 16.Cole SR, Young GP, Byrne D, et al. Participation in screening for colorectal cancer based on a faecal occult blood test is improved by endorsement by the primary care practitioner. J Med Screen. 2002;9:147–152. doi: 10.1136/jms.9.4.147. [DOI] [PubMed] [Google Scholar]
- 17.National Screening Committee. Second report of the National Screening Committee, 2000. www.nsc.nhs.uk/library/lib_ind.htm (accessed 25 Nov 2004)
- 18.General Medical Council. Seeking patients' consent: the ethical considerations. London: General Medical Council; 1999. [Google Scholar]