Abstract
Complexity theory has attracted considerable attention in recent years, both within medicine and in the wider world. Its themes of uncertainty and non-linearity resonate deeply with the experience of working in general practice. Describing the consultation as a complex, adaptive system provides a coherent theoretical basis for understanding the consultation, which has so far been lacking. Understanding the consultation as a complex, adaptive system offers insights into the consultation of that may prove to be of practical use to clinicians.
Keywords: chaos, complexity theory, consultation
INTRODUCTION
Theories are integral to the understanding and practice of medicine.1 They powerfully influence the way in which we collect, analyse, understand, and use information; as such, they deserve to be both acknowledged and researched.
For the last 300 years scientific thinking has been dominated by the influence of Newtonian science. The central idea here is of mechanism, and the dominant metaphor is the machine. Using Newton's theories, problems can be broken into their parts to be understood, and cause and effect are tightly linked by causal relationships. Although such a theoretical approach can be helpful in some areas of clinical practice, it fits less comfortably in the world of general practice where, using an approach informed by the seminal work of individuals such as Balint,2 Fry,3 and McWhinney,4 individuals and families are the focus.
Many different academic disciplines have brought their perspective to bear on what happens in consultations between doctors and patients. Medical models of the consultation are doctor-centred with diagnosis and disease at their core. Sociologists, on the other hand, have been interested in the interactions between doctors and patients in terms of social structures, roles, norms, and values, and how these are played out in the consultation.5–7 Anthropologists extend this analysis to consider illness and health-seeking behaviour across cultures.8,9 Psychological and psychoanalytical models have brought yet another different perspective to bear.2,10–14 By the late 1970s there was an increasingly held view that illness was the result of the interaction of biological, social, and psychological factors, as proposed by Engel.15 In the 1980s, several GPs16,17 developed consultation models integrating the academic approaches of other disciplines with the experience of general practice. Although all of these approaches have offered insights from their particular perspective, none has provided a unified theory for the consultation. However, in the last few years there has been a developing interest in complexity theory as a way of understanding what happens in health and health care.18–22
Dean has suggested that complexity completes our understanding of Engel's bio–psycho–social model by providing a coherent explanation of the interaction between the parts of the model.23 Is it possible to consider the consultation in terms of complexity and, if so, what advantages are there in so doing? This article discusses complexity theory and how it relates to general practice consultations, then explores the nature of the consultation in terms of the characteristics of complex systems. This analysis highlights skills needed for working within complex consultations.
COMPLEXITY THEORY
Complexity theory is concerned with the study of complex, adaptive systems, examples of which include such disparate phenomena as ecosystems, termite colonies, and any organisation of people — including the primary healthcare team. Whereas the machine is a metaphor of Newton's world, an ecosystem (such as woodland) is a metaphor of a complex, adaptive system.
How this fits in
There has been an increasing interest in complexity theory in recent years and its implications, in particular, for the organisation of care. However, relatively little has been written about complexity theory and clinical practice. Complexity theory offers a coherent explanation of consultation dynamics that goes beyond current models used in teaching consultation skills. This explanation also provides a framework for positive strategies for working in the uncertain world of primary care.
Complex systems are composed of networks of agents. These agents can be regarded as the building blocks of the system, which, through their interaction, contribute to its overall pattern. For example, in the brain these agents are nerve cells and in an ecosystem they are species. The environment of each agent is shaped by both itself and the other agents in the complex system, through constant interaction. Small changes within, or external to, the system can lead to major changes to the overall system, while large changes can make very little difference. For example, adding a new antihypertensive agent to a patient's drug regime might make very little difference to the blood pressure, or cause a disabling fall. This non-linear effect results from the modulation of interaction and feedback within the system. Such a complex system is constantly adapting and changing, sometimes in very small ways that may be difficult to detect, sometimes in such major ways that the complex system is transformed.
These ideas about complexity have been developed from diverse disciplines. For example, systems thinking has taken ideas from the non-linear mathematics of chaos theory24 as a source domain. Theories of dissipative structures25 draw on chemistry and theories of complex, adaptive systems;26 complex, responsive processes27 draw on diverse scientific disciplines, particularly organisational science.
CONSULTATIONS AND COMPLEXITY
All consultations may be analysed in terms of complexity. However, in the pragmatic world of day-to-day general practice, some consultations are straightforward and such an analysis is not needed to help our understanding of them, for example, consultations concerned with matters where actions and intended outcomes are easily agreed between patients and doctors.
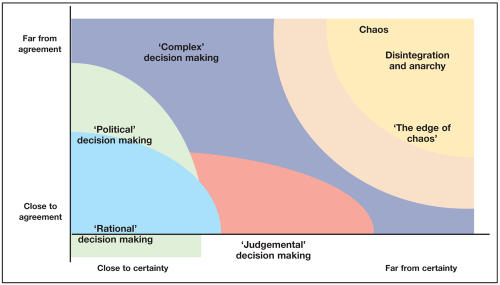
Figure 1 shows a conceptual framework for considering where complexity can help us most with understanding consultations.28–30 Along one axis we move from being close to certainty to being far from certainty; the other similarly describes agreement. At a point close to certainty and close to agreement, cause and effect relationships are most clearly seen by both doctor and patient and a consensus on action is relatively easily achieved. A patient with a cataract who wants treatment would be an example. In the area of ‘political’ decision making the evidence may be clear, but agreement may be difficult to achieve, such as with the current debate in the UK about the MMR (measles, mumps, and rubella) immunisation. Aspects of palliative care involve ‘judgmental’ decision making, where the evidence base is poorly developed. As we move further towards a point far from certainty and far from agreement the consultation may break down. In this anarchic region there is neither certainty nor agreement and no progress can be made. Between the zone of technically rational decisions and anarchy the consultation may be complex — this is where much of the clinical activity of general practice takes place. Links between cause and effect are unclear, and there is uncertainty about the way forward. Undifferentiated problems are presented and symptoms are frequently vague. These problems are the most difficult to help, but can also be the most rewarding. Fatigue, chronic pain, somatisation, and a range of mental health disorders occupy this zone but, realistically, any clinical problem might at some point come to rest here either as a result of its circumstances or evolution.
Figure 1.
The Stacey matrix: complexity and the consultation.28
Complexity theory argues that complex systems are relatively robust, adapting to internal interactions and to external influences but remaining essentially similar. However, metaphor from mathematical ‘chaos’ theory describes a state known as the ‘edge of chaos’ where a complex system is unstable and small changes within or external to the system may precipitate a radical change. Some consultations have this form of instability. Indeed, a doctor or patient may move a consultation to the ‘edge of chaos’ as a deliberate strategy to achieve greater creativity.
DIVERSITY OF AGENTS WITHIN A CONSULTATION
Diversity is the key to understanding complex systems. It can be seen in the many agents or influences that may effect a consultation. Some agents are physically present in the consultation including the doctor, patient, and others, such as a nurse or relative. Helman31 has suggested the manager, lawyer, statistician, journalist, and computer have agency within a consultation. Their agency is through those individuals physically present.
The doctor will be aware of the development of more managed health care in the UK, particularly as primary care trusts become established. The influence of the lawyer hovering in the background is inevitable with increasing complaints and litigation. An impact of this has been a shift to more defensive patterns of practice. The statistician comes to the consultation through measurement of everything from prescribing to cervical cytology, and through evidence-based medicine. The role of the media in consultations is familiar and is one of the ‘cues to action’ in Rosenstock's health belief model.10 Most UK general practices have become computerised,32 and many are paperless.33 Computers deliver high quality notes, data, and audit but they also influence the consultation.34,35 They compete for eye contact and may even reinforce a mechanical, non-human view of the self.36
Through narrative a patient may convey the richness of his/her story and implore the doctor to consider the dangers inherent in reducing that story to the level of a technical description. Stacey described themes emerging from that narrative as having agency within what he prefers to describe as a complex, responsive process rather than a complex, adaptive system.28 He also described organising themes that are experiences that mould the way we are and the way we respond; these too can act as agents. An example of an organising theme might be the experience of a patient who seeks advice about earache and is prescribed an antibiotic. When that patient next experiences similar symptoms he/she may quite reasonably assume that the appropriate course of action is to go to the doctor for antibiotics.
Free-flowing conversation allows the space of possibilities to be explored.28 Where conversation is constrained in consultations, important information and perspectives cannot emerge. Imperfections in communication akin to the mistakes and repairs identified and explicated by conversation analysis37,38 may act as agents in the consultation, changing its direction. A doctor needs to enable free-flowing conversation within the consultation, while remaining sensitive to its imperfections and where these may lead: perhaps to new insights; perhaps impeding understanding.
Various local contextual agents also act in the consultation. For example, the physical environment of the waiting room and the consulting room, and the organisation of the practice may exert their own influences. The amount of time within any one consultation is constrained; this constraint can act as an agent in its own right, significantly affecting what happens. Wider sociocultural influences, whether they be religious, social, or economic, can also act as agents.
CO-EVOLUTION WITHIN A CONSULTATION
Complex adaptive systems change over time and the agents within them co-evolve. Each agent changes in response to the changing context, which includes changes in the other agents in the system. Patient and doctor embark on a consultation with prior perspectives, from which a new picture emerges, and through engaging in the consultation both patient and doctor are themselves changed. Feedback loops in the consultation change the practice of the doctor and the behaviour of the patient during the consultation and in future consultations.
DISTRIBUTED CONTROL
Control within a complex, adaptive system is distributed with outcomes emerging from self-organisation within the system, rather than as a result of design or external control. As an example of this self-organisation, consider a shoal of fish swimming in the sea: there is no leader so when a predator approaches, the shoal responds not by a request for orders from a hierarchical leadership, but by the local interactions of individual fish in response to the threat spreading through the shoal. Thus self-organisation happens as a result of interaction between the many agents in a complex system.
Considering a consultation as a complex system implies potential for the system to self organise. There is, of course, a difference between a consultation and the example of the shoal of fish, as fish do not have the equivalent of human consciousness and many of the agents within the consultation act through the human actors. However, it is perhaps the potential of self-organisation that offers the most radical and controversial view of the consultation: it rejects the traditional idea of the locus of control being the doctor and replaces it with an understanding of control based on the relationships between agents and influences acting within the consultation.
This proposition does not deny the powerful position the doctor holds as an ‘expert’ and gatekeeper to many aspects of health care. However, it challenges doctors to explicitly consider whether outcomes, such as resolution of emotions, establishing shared understanding, or making decisions, may be allowed to emerge through interaction and how much they themselves guide the consultation in a particular direction. Either, or both, may be appropriate. Doctors also need to be aware that agents, as well as interactions between agents that we may not easily recognise, can influence consultations in unexpected ways.
NON-LINEARITY AND UNCERTAINTY
The non-linear nature of the complex consultation means that not only may a very small action or observation entirely transform the assessment and management of a patient's problem, but also that a major intervention may not achieve the outcome that is hoped for. Non-linearity and distributed control mean that outcome is essentially unpredictable. For the consultation, this challenges deeply held ideas of what medical consultations should generate, and challenges many consultation models.
Both doctor and patient like to feel that the process that they embark upon during the consultation is safe and predictable. Yet, the complexity model, with its inherent uncertainty and unpredictability, seems to fit better with the experience of general practice. Chance remarks, minor observations, and ‘minor’ clinical data can send consultations off in very different directions. For example, a patient may present with a history of chest pain that might suggest cardiac pain, and yet subtle non-verbal clues suggestive of depression as the cause of the patient's physical symptoms may be detected. Although a physical cause may need to be excluded, these clues alter the approach to the whole assessment.
RULES AND BOUNDARIES
The concept that simple rules may give rise to complex patterns comes from examples such as a flock of birds. A few simple rules that each bird follows can be identified; these give rise to flocking patterns. It seems that complex, adaptive systems may emerge from simple rules, particularly when there are relatively few agents in the system. This is known as ‘simple complexity’.
This concept of simple rules giving rise to complex patterns is linked with the understanding of distributed control (as discussed above).39–41 The ‘rules’ in complex, adaptive systems are not deterministic and what emerges is not necessarily predictable. So what sort of rules might operate in the consultation? Certainly there are social rules that govern the interaction of doctors and patients, as these are roles with social expectations, for example, expertise, power, and vulnerability. There are the distribution rules (turn-taking rules) of conversational analysis (Schegloff42), and ethical rules, such as the 13 rules governing clinical care identified by the UK General Medical Council.43 Consultation models, such as those by Pendleton et al16 and Neighbour,17 can also be viewed as essentially rule-based.
Although some consultations may have the character of ‘simple complexity’, in many consultations there may be so many influencing agents that the role of simple rules is difficult to discern. In these consultations the types of rules discussed here may act by limiting what is likely to happen during a consultation. However, they can also act as agents within consultations. For example, a change in the socially constructed power relationship between doctor and patient, or a change in a statutory process associated with health care (such as sickness certification), may radically change the dynamics of consultations.
CONSULTATION PATTERNS AND THE ‘EDGE OF CHAOS’
GPs are likley to recognise that consultations are constrained by factors such as time, context, and experience, and so some similarity between consultations would be expected. However, each consultation is different, with different agents and influences interacting in the complex, adaptive system, and so there is likely to be considerable variation of pattern between consultations, even involving the same clinician.
Consider the doctor reviewing a hypertensive patient. Talk focuses on symptoms, medication problems and attention to cardiovascular risk analysis. The process is doctor-led and frequently follows a pattern of talk and activity used with many patients — and also repeatedly with an individual patient over time. The nature of this consultation may inhibit the emergence of new information if patterns of talk and action are predictable and novelty is stifled or ignored. In contrast, a consultation characterised by the facilitation of free-flowing conversation allows the expression of novelty and creativity and, perhaps, a glimpse of surprising insights that may lead the consultation into completely new areas. This experience of general practice resonates with the understanding of complex, adaptive systems as relatively stable systems that may constantly change and have the potential for dramatic change. A stable pattern of consultation may be appropriate, but there are times in general practice when doctors need to think more creatively when trying to work out why they are unable to effect a beneficial change or understand a current pattern of illness or behaviour.
The literature on change management at both organisational and individual levels44 describes how to identify factors that are barriers both in moving towards change and moving away from the current state. Complexity theory enhances this understanding: a complex, adaptive system is most creative and adaptive when in a state of bounded instability; Kaufman suggests that complex systems move to the ‘edge of chaos’ to solve problems.40,41
Applying this to the consultation, it will move from safe, familiar territory to less familiar patterns of talk and action. This might happen, for example, when the doctor's personal life and experiences are brought into the consultation either by the doctor or by the patient (Box 1). Where this happens the result might be to establish a greater, more empathic understanding between doctor and patient, but it also has the capacity to be destructive if either party is upset. With this sort of shift in the consultation, the opportunity arises to gain new insights and create new opportunities for change. This type of consultation might be described as consulting at the ‘edge of chaos’, and risk is implied. This risk might be to the doctor–patient relationship, or perhaps might involve the surfacing of an issue that the doctor or patient had not wanted to discuss.
Box 1. Example of a consultations at the edge of chaos.
Katherine is a 50-year-old patient who is a frequent attender and might be regarded as a ‘heartsink’ patient. She visits her doctor at least every 2 weeks complaining of minor physical symptoms. On one particular occasion her doctor is running late on what has been a particularly difficult day in the practice. Katherine enters the consulting room and starts to explain her usual symptoms once again. Frustrated by his inability to resolve Katherine's problems, her doctor asks her directly why she keeps coming to see him. Rather taken aback, Katherine explains that she thought he might able to find a solution to her problems — to which the doctor replies that if he had such a remedy, didn't she think that he would have given it to her several years previously and avoided their many subsequent fruitless encounters. Clearly confused and upset, Katherine leaves. She returns a few weeks later, not seeking a cure but asking for advice about how to live with her problems. Subsequently, her consultation frequency settles into a more conventional pattern.
CONCLUSION
The consultation can be described as a complex, adaptive system, but what advantages does such a ‘lens’ offer? The most important, is that it increases GPs' understanding of uncertainty and unpredictability within the consultation.
For too long the medical process has been presented as one based on predictability and certainty, a presentation supported by the myth of physician supremacy and the power of modern medicine.45 Both patients and doctors have, at times, taken too much comfort from the predictability and certainty with which they want to endow medicine. The ‘necessary fallibility’46 that arises from the complexity of individuals and health has been largely ignored. This places an unrealistic and unfair pressure on the doctor to find successful solutions to all problems and denies patients the opportunity to share and understand the uncertain reality of illness and health care. This presentation of medicine has influenced the way doctors have approached and analysed consultations, and designed protocols and decision aids.
Understanding the consultation as a complex, adaptive system provides a theoretical base for the experience of uncertainty and unpredictability in general practice. With this understanding, doctors may be enabled to take risks within consultations and so allow greater creativity. Doctors need to be able to display what Stacey described as the ‘good-enough holding of anxiety’28 that is provoked by uncertainty. This skill will be developed through being aware of, and learning about, the many agents operating in consultations, the uncertainties this creates, and the unpredictable nature of consultation outcomes. Doctors need to work with uncertainty and unpredictability in ways that is both creative and relatively safe.
The framework provided by complexity theory helps us understand the role of the doctor, not as an objective external observer, as suggested by traditional medical models of the doctor–patient interaction, but as an enquiring participant, who seeks to influence change in a patient's condition.
Acknowledgments
The authors thank the Complexity and Primary Care Group (www.complexityprimarycare.org) for the creative dialogue that has led to writing this paper.
REFERENCES
- 1.Alderson P. The importance of theories in health care. BMJ. 1998;317(7164):1007–1010. doi: 10.1136/bmj.317.7164.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Balint M. The doctor, his patient and the illness. 2nd ed. London: Pitman; 1964. [Google Scholar]
- 3.Fry J. Profiles of disease. A study in the natural history of common diseases. Edinburgh and London: E&S Livingstone; 1966. [Google Scholar]
- 4.McWhinney IR. A textbook of family medicine. New York: Oxford University Press; 1989. [Google Scholar]
- 5.Mechanic D. The concept of illness behaviour. J Chronic Dis. 1962;15:189–194. doi: 10.1016/0021-9681(62)90068-1. [DOI] [PubMed] [Google Scholar]
- 6.Tuckett D. An introduction to medical sociology. London: Tavistock; 1976. [Google Scholar]
- 7.Boreham P, Gibson D. The informative process in private medical consultations: a preliminary investigation. Soc Sci Med. 1978;12(5A):409–416. [PubMed] [Google Scholar]
- 8.Kleinman A. Patients and healers in the context of culture: an exploration of the borderland between anthropology, medicine and psychiatry. Berkeley: University of California Press; 1980. [Google Scholar]
- 9.Helman CG. Disease versus illness in general practice. J R Coll Gen Pract. 1981;31(230):548–552. [PMC free article] [PubMed] [Google Scholar]
- 10.Rosenstock IM. Why people use health services. Milbank Mem Fund Q. 1966;44(3):94–127. [PubMed] [Google Scholar]
- 11.Berne E. Games people play: the psychology of human relationships. Harmondsworth: Penguin; 1964. [Google Scholar]
- 12.Rotter JB. Generalised expectancies for internal versus external control of reinforcement. Psychol Monogr. 1966;80(1):1–28. [PubMed] [Google Scholar]
- 13.Byrne PS, Heath CC. Practitioners' use of non-verbal behaviour in real consultations. J R Coll Gen Pract. 1980;30(215):327–331. [PMC free article] [PubMed] [Google Scholar]
- 14.Byrne P, Long B. Doctors talking to patients: a study of the verbal behaviours of doctors in the consultation. London: HMSO; 1976. [Google Scholar]
- 15.Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196(4286):129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- 16.Pendleton D, Schofield T, Tate P, Havelock P. The consultation: an approach to learning and teaching. Oxford: Oxford University Press; 1984. [Google Scholar]
- 17.Neighbour R. The inner consultation: how to develop an effective and intuitive consulting style. Newbury: Petroc Press; 1999. [Google Scholar]
- 18.Griffiths F, Byrne D. General practice and the new science emerging from the theories of ‘chaos’ and complexity. Br J Gen Pract. 1998;48(435):1697–1699. [PMC free article] [PubMed] [Google Scholar]
- 19.Plsek PE, Greenhalgh T. Complexity science: the challenge of complexity in health care. BMJ. 2001;323(7313):625–628. doi: 10.1136/bmj.323.7313.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wilson T, Holt T. Complexity science: coomplexity and clinical care. BMJ. 2001;323(7314):685–688. doi: 10.1136/bmj.323.7314.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Plsek PE, Wilson T. Complexity, leadership, and management in healthcare organisations. BMJ. 2001;323(7315):746–749. doi: 10.1136/bmj.323.7315.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fraser SW, Greenhalgh T. Coping with complexity: educating for capability. BMJ. 2001;323(7316):799–803. doi: 10.1136/bmj.323.7316.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dean A. Complexity and substance misuse. Addiction Research and Theory. 2001;9(1):19–41. [Google Scholar]
- 24.Gleick J. Chaos: making a new science. London: William Heinemann; 1988. [Google Scholar]
- 25.Prigogine I, Stengers I. Order out of chaos: mans new dialogue with nature. New York: Bantam; 1984. [Google Scholar]
- 26.Waldrop MM. Complexity: the emerging science at the edge of order and chaos. London: Viking; 1992. [Google Scholar]
- 27.Stacey RD. Complex responsive processes in organisations. London: Routledge; 2001. [Google Scholar]
- 28.Stacey RD. Strategic management and organisational dynamics: the challenge of complexity. 3rd ed. Harlow: Prentice Hall; 2002. [Google Scholar]
- 29.Hassey A. Complexity and the clinical encounter. In: Sweeney K, Griffiths F, editors. Complexity and healthcare: an introduction. Abingdon: Radcliffe Medical Press; 2002. [Google Scholar]
- 30.Zimmerman B, Lindberg C, Plsek P. Edgeware insights from complexity science for health care leaders. 2nd ed. Irving: VHA; 2001. [Google Scholar]
- 31.Helman C. The culture of general practice. Br J Gen Pract. 2002;52(481):619–620. [PMC free article] [PubMed] [Google Scholar]
- 32.NHS Executive. Computerisation in general practice survey. London: Department of Health; 1998. [Google Scholar]
- 33.Waring N. To what extent are general practices ‘paperless’ and what are the constraints to them becoming more so? Br J Gen Pract. 2000;50(450):46–47. [PMC free article] [PubMed] [Google Scholar]
- 34.Gray JA. Postmodern medicine. Lancet. 1999;354(9189):1550–1553. doi: 10.1016/s0140-6736(98)08482-7. [DOI] [PubMed] [Google Scholar]
- 35.Greatbatch D, Campion P, Heath C, Luff P. How do desktop computers affect the doctor–patient interaction? Fam Pract. 1995;12(1):32–36. doi: 10.1093/fampra/12.1.32. [DOI] [PubMed] [Google Scholar]
- 36.Turkle S. The second self: Computers and the human spirit. London: Granada; 1984. [Google Scholar]
- 37.ten Have P. Doing conversational analysis: a practical guide. London: Sage; 1999. [Google Scholar]
- 38.Jefferson G. On exposed and embedded correction in conversation. In: Button G, Lee J, editors. Talk and social organisation. Clevedon, Phildelphia: Multilingual Matters; 1987. [Google Scholar]
- 39.Holland J. Emergence from chaos to order. Oxford: Oxford University Press; 1998. [Google Scholar]
- 40.Kauffman S. The origins of order: self-organisation and selection in evolution. Oxford: Oxford University Press; 1993. [Google Scholar]
- 41.Kauffman S. At home in the universe: the search for the laws of self-organisation and complexity. New York: Oxford University Press; 1995. [Google Scholar]
- 42.Schegloff EA, Sack H. Opening up closings. Semotica. 1973;8:289–327. [Google Scholar]
- 43.General Medical Council. Good medical practice. 3rd edn. London: General Medical Council; 2001. www.gmc-uk.org/standards/good.htm (accessed 19 Nov 2004) [Google Scholar]
- 44.Armstrong M. Management processes and functions. London: Institute of Personnel and Development; 1992. [Google Scholar]
- 45.Illich I. Limits to medicine: medical nemesis: the expropriation of health. New York: Penguin; 1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gorovitz S, MacIntyre A. Toward a theory of medical fallibility. J Med Philos. 1976;1(1):51–71. [Google Scholar]