Abstract
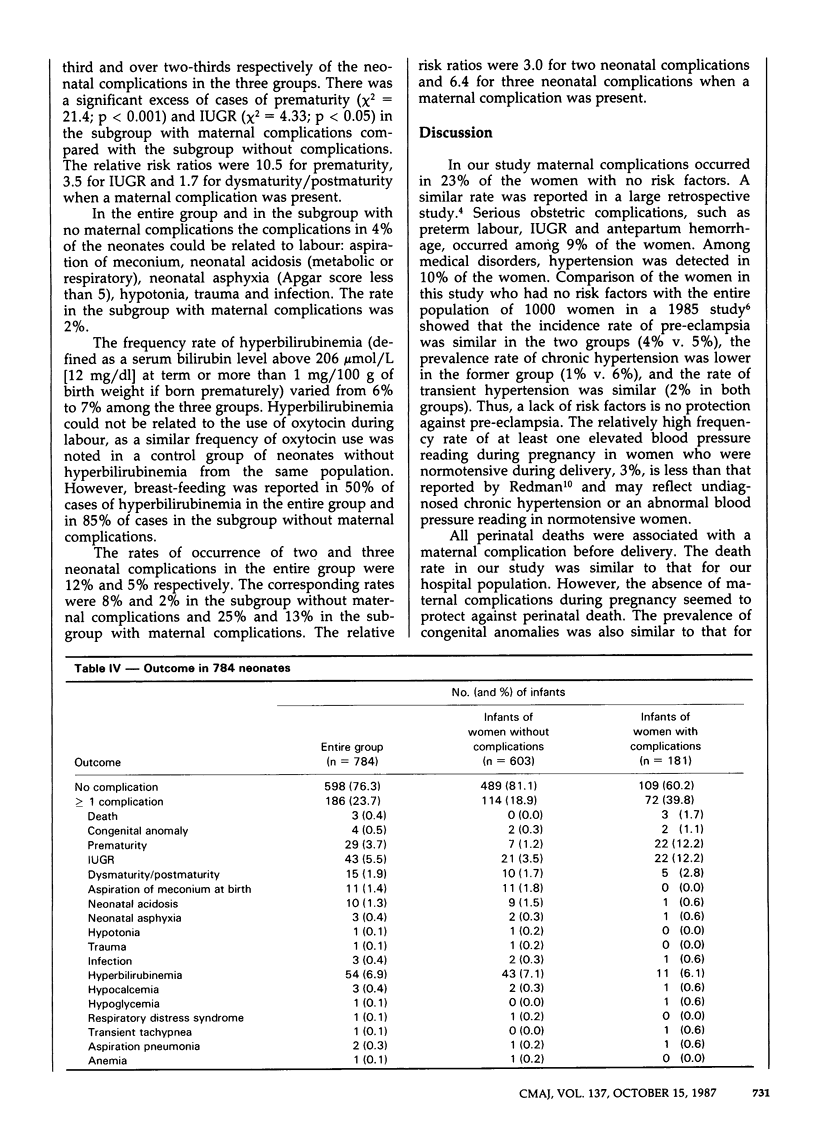
Between November 1979 and April 1984, 790 consecutive pregnant women who considered themselves as having a "normal" pregnancy were followed in private practice from 9 weeks' gestation until 6 weeks post partum. The women had no pre-existing disease or problem classified as a risk to the pregnancy at the time of their first visit, had a singleton pregnancy and gave birth at Notre-Dame Hospital, Montreal. Maternal complications occurred during the course of pregnancy in 181 women (23%). Complications were mostly related to obstetric conditions (10%), such as preterm labour, intrauterine growth retardation (IUGR) and antepartum hemorrhage, or to medical conditions (12%), the most prevalent of which was hypertension (77% of medical conditions). Neonatal complications occurred in 183 infants (23%). The corrected perinatal death rate was 2.5 per 1000. Prematurity, IUGR and dysmaturity/postmaturity accounted for nearly half of the complications. Hyperbilirubinemia occurred in 7% of the cases. Among women without any maternal complications during pregnancy, the frequency rate of neonatal complications was 19%, compared with 23% among the entire group of 790 women. Our results suggest that the absence of maternal complications does not protect the infant from a neonatal complication. Further refinement is needed to identify markers of obstetric, medical and neonatal complications in pregnancies with no risk factors.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Hobel C. J., Hyvarinen M. A., Okada D. M., Oh W. Prenatal and intrapartum high-risk screening. I. Prediction of the high-rish neonate. Am J Obstet Gynecol. 1973 Sep 1;117(1):1–9. doi: 10.1016/0002-9378(73)90720-5. [DOI] [PubMed] [Google Scholar]
- Klein M., Papageorgiou A., Westreich R., Spector-Dunsky L., Elkins V., Kramer M. S., Gelfand M. M. Care in a birth room versus a conventional setting: a controlled trial. Can Med Assoc J. 1984 Dec 15;131(12):1461–1466. [PMC free article] [PubMed] [Google Scholar]
- Moutquin J. M., Rainville C., Giroux L., Raynauld P., Amyot G., Bilodeau R., Pelland N. A prospective study of blood pressure in pregnancy: prediction of preeclampsia. Am J Obstet Gynecol. 1985 Jan 15;151(2):191–196. doi: 10.1016/0002-9378(85)90010-9. [DOI] [PubMed] [Google Scholar]
- Nesbitt R. E., Jr, Aubry R. H. High-risk obstetrics. II. Value of semiobjective grading system in identifying the vulnerable group. Am J Obstet Gynecol. 1969 Apr 1;103(7):972–985. doi: 10.1016/s0002-9378(16)34448-9. [DOI] [PubMed] [Google Scholar]
- Rosenberg S. N., Albertsen P. C., Jones E. E., Roberts R. S. Complications of labor and delivery following uncomplicated pregnancy. Med Care. 1981 Jan;19(1):68–79. doi: 10.1097/00005650-198101000-00008. [DOI] [PubMed] [Google Scholar]
- Saldana L. R., Rivera-Alsina M. E., Arias J. W., Ross P. J., Pokorny S. F. Home birth: negative implications derived from a hospital-based birthing suite. South Med J. 1983 Feb;76(2):170–173. [PubMed] [Google Scholar]
- Sokol R. J., Rosen M. G., Stojkov J., Chik L. Clinical application of high-risk scoring on an obstetric service. Am J Obstet Gynecol. 1977 Jul 15;128(6):652–661. doi: 10.1016/0002-9378(77)90212-5. [DOI] [PubMed] [Google Scholar]


