The predominant mechanism for resistance to β-lactam antibiotics in gram-negative bacteria is the synthesis of β-lactamase. To meet this challenge, β-lactams with greater β-lactamase stability, including cephalosporins, carbapenems, and monobactams, were introduced in the 1980s. Resistance appeared initially in organisms such as Enterobacter cloacae, Citrobacter freundii, Serratia marcescens, and Pseudomonas aeruginosa that could, by mutation, overproduce their chromosomal AmpC (also termed class C or group 1) β-lactamase, thus providing resistance to both oxyimino- and 7-α-methoxy-cephalosporins and monobactams (74).
Later, resistance appeared in bacterial species that lack an inducible AmpC enzyme, such as Klebsiella pneumoniae, Escherichia coli, Salmonella spp., and Proteus mirabilis, and this resistance was found to be mediated by plasmids encoding extended-spectrum β-lactamases (ESBLs), which are enzymes that arose by mutations in TEM or SHV β-lactamases of more limited hydrolytic capacity (39, 40, 68). Such resistance included oxyimino-cephalosporins and monobactams but not 7-α-methoxy-cephalosporins and was blocked by clavulanate, sulbactam, or tazobactam, which are inhibitors that are generally ineffective against class C enzymes (49, 75).
With continuing use of 7-α-methoxy-cephalosporins (cefoxitin and cefotetan) and the clinical introduction of β-lactamase inhibitor combinations (clavulanate with amoxicillin or ticarcillin, sulbactam with ampicillin, and tazobactam with piperacillin), plasmids encoding class C β-lactamases appeared (56). Like their counterpart on the chromosome, such enzymes provided a broader spectrum of resistance than ESBLs and were not blocked by commercially available inhibitors.
Furthermore, in a strain with decreased outer membrane permeability such enzymes can provide resistance to carbapenems as well, as has been observed with clinical isolates of K. pneumoniae during an outbreak in New York (13) and in individual isolates of E. coli in the United Kingdom (78) and of K. pneumoniae in Sweden (17).
HISTORY
AmpC β-lactamases, demonstrated or presumed to be chromosomally mediated, have been described in Acinetobacter spp., Aeromonas spp., Chromobacterium violaceum, C. freundii, Enterobacter spp., E. coli, Hafnia alvei, Lysobacter lactamgenus, Morganella morganii, Ochrobactrum anthropi, Proteus rettgeri, Providencia stuartii, P. aeruginosa, Psychrobacter immobilis, Rhodobacter sphaeroides, S. marcescens, and Yersinia enterocolitica. In many genera, AmpC is inducible via a system involving ampD, ampG, ampR, and intermediates in peptidoglycan recycling (38, 86). The ampC gene of E. coli is normally expressed at a low level, regulated by a growth rate-dependent attenuation mechanism (42) but not by induction, since ampR is missing (35). In Shigella flexneri and Shigella dysenteriae, ampC is included in a large deletion (55). An ampC locus appears on the genetic map of Salmonella (76), but the evidence for its existence was indirect and its presence has not been confirmed in the sequenced genomes of Salmonella enterica serotypes Typhimurium or Paratyphi (57), so that Salmonella is considered to be AmpC− (56). A chromosomal ampC gene is also lacking in Klebsiella spp. (57) and P. mirabilis.
In 1976, Bobrowski et al. described a plasmid-mediated β-lactamase indistinguishable from the AmpC enzyme of E. coli in a strain of P. mirabilis (11). Unfortunately, the original plasmid was lost, there was some doubt about the transfer experiments, and molecular studies were not done. In 1982, Levesque et al. reported a plasmid-mediated cephalosporinase in Achromobacter spp. (48). Regrettably, the original strain was lost, the β-lactamase gene was not sequenced, and in retrospect the biochemical properties of the enzyme resembled those of a group 2b broad-spectrum enzyme rather than of a group 1 cephalosporinase. In 1983, Knothe et al. reported the transfer of cefoxitin resistance from S. marcescens to Proteus or Salmonella spp., but resistance segregated on transfer to E. coli and no biochemical or molecular studies were done (44).
In 1989, Bauernfeind et al. described a K. pneumoniae isolate from South Korea that could transfer resistance to cefoxitin and cefotetan as well as to penicillins, oxyimino-cephalosporins, and monobactams to E. coli (6). The enzyme, termed CMY-1 for its cephamycinase activity, had an isoelectric point (pI) of 8.0 and was more sensitive to inhibition by sulbactam than by clavulanate or tazobactam, suggesting that it might be a class C enzyme. However, the first proof that a class C β-lactamase had been captured on a plasmid was provided by Papanicolaou et al., who described transmissible resistance to α-methoxy- and oxyimino-β-lactams mediated by an enzyme (MIR-1) with the biochemical properties of a class 1 β-lactamase and showed that part of the MIR-1 gene was 90% identical to the ampC gene of E. cloacae (65).
Subsequently, plasmid-mediated class C β-lactamases have been discovered worldwide (Table 1). They have been named with inconsistency typical of β-lactamase nomenclature according to the resistance produced to cephamycins (CMY), cefoxitin (FOX), and moxalactam (MOX) or latamoxef (LAT), to the type of β-lactamase, such as AmpC type (ACT) or Ambler class C (ACC), and to the site of discovery, such as the Miriam Hospital in Providence, R.I. (MIR-1) or Dhahran hospital in Saudi Arabia (DHA). BIL-1 was even named after the patient (Bilal) who provided the original sample (D. J. Payne, personal communication).
TABLE 1.
Chronology of discovery of AmpC plasmid-encoded β-lactamasesa
| Name | Countryb | Yearc | Species | pI | Reference(s) |
|---|---|---|---|---|---|
| MIR-1 | United States | 1988 | K. pneumoniae | 8.4 | 41, 65 |
| CMY-1 | South Korea | 1988 | K. pneumoniae | 8.0 | 6, 9 |
| BIL-1 | United Kingdom (Pakistan) | 1989 | E. coli | 8.8 | 66, 88 |
| FOX-1 | Argentina | 1989 | K. pneumoniae | 6.8–7.2 | 31 |
| CMY-2 | Greece | 1990 | K. pneumoniae | 9.0 | 8 |
| France (Algeria) | 1994 | Salmonella senftenberg | 9.0 | 46 | |
| MOX-1 | Japan | 1991 | K. pneumoniae | 8.9 | 36 |
| DHA-1 | Saudi Arabia | 1992 | S. enteritidis | 7.8 | 26 |
| France | 1998 | K. pneumoniae | 7.8 | Verdet et al.d | |
| DHA-2 | France | 1992 | K. pneumoniae | 7.8 | 24 |
| FOX-2 | Germany (Guatemala) | 1993 | K. pneumoniae | 6.7 | 10 |
| LAT-1 | Greece | 1993 | K. pneumoniae | 9.4 | 82, 83 |
| FOX-3 | Italy | 1994 | K. oxytoca, K. pneumoniae | 7.25 | 51 |
| LAT-2 | Greece | 1994 | K. pneumoniae, E. coli, E. aerogenes | 9.1 | 28 |
| ACT-1 | United States | 1994 | K. pneumoniae, E. coli | 9.0 | 13 |
| MOX-2 | France (Greece) | 1995 | K. pneumoniae | 9.2 | Boyer-Mariotte et al.e |
| CMY-4 | Tunisia | 1996 | P. mirabilis | 9.2 | 85 |
| United Kingdom | 1999 (P) | E. coli | >8.5 | 78 | |
| Sweden (India) | 1998 | K. pneumoniae | 9.0 | 17 | |
| ACC-1 | Germany | 1997 | K. pneumoniae | 7.7 | 7 |
| France (Tunisia) | 1998 | K. pneumoniae | 7.8 | 60 | |
| Tunisia | 1997–2000 | K. pneumoniae, P. mirabilis, Salmonella spp. | 7.8 | 71 | |
| France (Tunisia) | 2000 | P. mirabilis, E. coli | 7.7 | 30 | |
| CMY-3f | France | 1998 (P) | P. mirabilis | 9.0 | 14 |
| LAT-3 | Greece | 1998 (P) | E. coli | 8.9 | 29 |
| LAT-4 | Greece | 1998 (P) | E. coli | 9.4 | 29 |
| CMY-8 | Taiwan | 1998 | K. pneumoniae | 8.25 | 91 |
| CMY-5 | Sweden | 1999 (P) | K. oxytoca | 8.4 | 89, 90 |
| FOX-4 | Spain | 2000 (P) | E. coli | 6.4 | 12 |
Other plasmid-mediated AmpC-type β-lactamases have been described in GenBank but are not yet published, including CMY-6, CMY-7, CMY-9, CMY-10, CMY-11, and FOX-5.
Country of isolation (if different, probable country of origin is indicated in parentheses).
Year of isolation or date of publication (P).
C. Verdet, N. Boutros, B. Salauze, A. Rossier, T. Lambert, A. Philippon, and G. Arlet. Abstr. 20th Réunion Interdisciplinaire Chimiothérapie Anti-Infectieuse, abstr. 24/C4, 2000.
S. Boyer-Mariotte, L. Raskine, B. Hanau, A. Philippon, M.M. Sanson-LePors, and G. Arlet, Abstr. 38th Intersci. Conf. Antimicrob. Agents Chemother., abstr. C-7, 1998.
Chromosomal location.
Increasingly, a demonstration of enzyme uniqueness relies on nucleotide sequencing, a sometimes imperfect technique. Barlow and Hall (M. Barlow and B. G. Hall, submitted for publication) recently reanalyzed several plasmid-mediated AmpC genes and concluded that the amino acid sequences of CMY-2, BIL-1, and LAT-2 were identical, as were LAT-1 and LAT-4 and also LAT-3 and CMY-6. In the text and tables below, the originally published names have been retained, with apparent identities in parentheses, such as BIL-1 (CMY-2).
EPIDEMIOLOGICAL FEATURES
As shown in Table 1, plasmid-mediated class C β-lactamases have been discovered most frequently in isolates of K. pneumoniae and also in other naturally AmpC− species such as K. oxytoca, Salmonella, and P. mirabilis. Some enzymes have been found in E. coli, although this species can also increase production of its normally weakly expressed chromosomal AmpC enzyme by gene duplication or mutation in the ampC promoter or attenuator with consequent enhanced gene expression (18, 62). In Greece, plasmid-mediated LAT-2 (CMY-2) has been found in clinical isolates of Enterobacter aerogenes simultaneously with its appearance in clinical strains of K. pneumoniae and E. coli (28), and in France plasmid-mediated ACC-1 has been found in both E. coli and P. mirabilis isolates obtained from the same urine sample (30). In the United States, ceftriaxone-resistant Salmonella have begun to appear that owe their resistance to plasmid-mediated CMY-2 β-lactamase. Between 1996 and 1998, 13 ceftriaxone-resistant Salmonella strains were isolated from symptomatic patients in eight different states (22). Several Salmonella serotypes were involved. Such strains have been isolated from cattle and pigs (87). One 12-year old boy living in Nebraska was infected with a ceftriaxone-resistant strain identical to S. enterica serotype Typhimurium strains isolated from his father’s infected calves (23).
A striking feature is the global distribution of strains producing plasmid-determined cephalosporinases. They have been found in Africa (Algeria, Tunisia), Asia (India, Japan, Pakistan, South Korea), Europe (France, Germany, Greece, Italy, Sweden, United Kingdom), the Middle East (Saudi Arabia), North America (United States), and South and Central America (Argentina, Guatemala) (Table 1). Just as with strains producing ESBLs such as SHV-2 or SHV-5 (77), travel and transfer of patients has allowed the importation of BIL-1 (CMY-2) from Pakistan to the United Kingdom (66), strains with BIL-1-like enzymes from the Indian subcontinent to London (59), several CMY types (CMY-2, CMY-6, CMY-7) from Punjab (India) to London (unpublished results), CMY-2 from Algeria to France (46), CMY-4 from India to Sweden (17), FOX-2 from Guatemala to Germany (10), ACC-1 from Tunisia to France (30, 60), and MOX-2 from Greece to France (S. Boyer-Mariotte, L. Raskine, B. Hanau, A. Philippon, M. M. Sanson-LePors, and G. Arlet, Abstr. 38th Intersci. Conf. Antimicrob. Agents Chemother., abstr. C-7, 1998). CMY-2 is the most prevalent of the plasmid-mediated AmpC enzymes and the most widely distributed geographically, having been reported in Algeria, France, Germany, Greece, India, Pakistan, Taiwan, Turkey, the United Kingdom, and the United States (5).
Except for Salmonella strains and occasional K. pneumoniae isolates (43), most strains producing plasmid-determined AmpC enzymes have been isolated from patients after several days in the hospital. Affected patients have often had prolonged stays in intensive care units. Some patients had one or more surgical procedures (65), an underlying disease such as leukemia (78) or cancer (27, 36, 59), or were immunocompromised after liver or kidney transplantation (59). Sources of organisms included cultures of urine (about 50% of isolates), blood, wounds, sputum, or stool. Some isolates were recovered in mixed cultures with other potential pathogens. A majority of the patients had been treated with β-lactam antibiotics including cefoxitin, moxalactam, cefmetazole, cefotetan, or imipenem (13, 31, 36, 65). Many strains with plasmid-determined AmpC enzymes also produce TEM-1, TEM-2, or even an ESBL, such as SHV-5 (28, 29, 59).
As already observed for ESBL-producing K. pneumoniae organisms (15, 61, 72), AmpC-producing nosocomial isolates can be responsible for outbreaks, for example, MIR-1 (11 patients) (65), a BIL-1(CMY-2)-like enzyme (5 patients) (59), ACC-1 (13 patients) (60), and ACT-1 (17 patients) (13).
SUSCEPTIBILITY PATTERNS
Table 2 illustrates in vitro susceptibilities for E. coli transconjugants or transformants producing plasmid-mediated AmpC β-lactamases. Some of the MICs for what ought to be similar enzymes differ by more than can be attributed to experimental variation (e.g., LAT-1 and LAT-4 with cefotaxime, ceftazidime, or aztreonam) and may have resulted from differences in host E. coli strains. Strains with plasmid-mediated AmpC enzymes were consistently resistant to aminopenicillins (ampicillin or amoxicillin), carboxypenicillins (carbenicillin or ticarcillin), and ureidopenicillins (piperacillin) and, among the penicillins, these strains were susceptible only to amdinocillin or temocillin. The enzymes provided resistance to cephalosporins in the oxyimino group (ceftazidime, cefotaxime, ceftriaxone, ceftizoxime, cefuroxime) and the 7-α-methoxy group (cefoxitin, cefotetan, cefmetazole, moxalactam). MICs were usually higher for ceftazidime than for cefotaxime and for cefoxitin than for cefotetan. The enzymes were also active against the monobactam aztreonam, although for some strains aztreonam MICs were in the susceptible range. Susceptibility to cefepime or cefpirome was little affected and was unchanged for carbapenems (imipenem, meropenem).
TABLE 2.
In vitro susceptibilities (MIC) of E. coli derivatives producing plasmid-encoded AmpC β-lactamase
| Anti-microbial agent | MIC (μg/ml) (reference no.) for derivatives producing:
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ACC-1 (7) | ACT-1 (13) | BIL-1 (CMY-2)a (66, 88) | CMY-1 (9) | CMY-2 (8) | CMY-3 (14) | CMY-4 (85) | CMY-5 (90) | CMY-8 (91) | DHA-1 (26) | DHA-2 (24) | FOX-1 (31) | FOX-2 (10) | FOX-3 (51) | FOX-4 (12) | LAT-1 (83) | LAT-2 (CMY-2)a(28) | LAT-3 (29) | LAT-4 (LAT-1)a (29) | MIR-1 (65) | MOX-1 (36) | |
| Ampicillinb | 64 | 2,048 | 1,024 | >128 | >256 | >512 | >512 | 1,024 | 256 | >128 | 1,000 | >512 | |||||||||
| Carbenicillinc | 128 | 1,024 | >128 | 128 | 128 | >2,048 | ≥1,024 | 512 | >128 | 128 | |||||||||||
| Piperacillin | 32 | 32 | 64 | 128 | 64 | 64 | 128 | 64 | |||||||||||||
| Temocillin | 4 | 8 | 8 | 8 | 16 | 64 | |||||||||||||||
| Mecillinam | 4 | 4 | |||||||||||||||||||
| Cephalothind | >1,028 | >1,024 | >128 | 512 | 128 | >512 | |||||||||||||||
| Cefotaxime | 8 | ≤2 | 8 | 64 | 16 | 16 | 16 | 64 | >256 | 64 | 4 | 2 | 16 | 1 | 64 | 128 | 64 | 96 | 4 | 64 | >512 |
| Ceftazidime | 32 | 4 | >16 | 4 | 128 | 64 | 8 | 256 | 32–64 | 64 | 8 | 8 | 32 | 16 | >128 | >128 | >256 | 128 | 8 | 128 | 16 |
| Cefoxitin | 4 | >256 | 256 | 256 | 128 | 8 | >256 | 128 | 16 | 128 | 256 | 64 | >512 | 64 | 256 | 256 | 64 | ≥256 | |||
| Cefotetan | 2 | 16 | 256 | 64 | 32 | 32 | 64 | 128 | 128 | ≥64 | >512 | ||||||||||
| Cefmetazole | 128 | 64 | 4 | ≥64 | 512 | ||||||||||||||||
| Moxalactam | 1 | 8 | 2 | 0.06 | 0.5 | 1 | 1 | 32 | 64 | >512 | |||||||||||
| Aztreonam | 1 | 4 | 4 | 16 | 64 | 32 | 64 | 16 | 2 | 1 | 2 | 1 | 64 | 64 | 64 | 64 | 8 | 128 | 16 | ||
| Cefepime | 0.25 | ≤0.06 | 0.25 | 0.5 | 0.06 | 0.125 | 0.03 | 0.13 | ≤0.06 | 2 | 0.5 | 0.125 | 1 | ||||||||
| Cefpirome | 1 | 2 | 0.5 | 0.25 | 1 | 1 | |||||||||||||||
| Imipenem | 0.13 | 1 | 0.25 | 0.5 | 0.25 | 0.25 | 0.5–1 | 0.25–0.5 | ≤0.125 | 0.25 | 0.5 | 0.12 | 0.5 | 2 | 1 | 0.5 | |||||
| Meropenem | 0.03 | 0.06 | 0.06 | 0.03 | 0.12 | 0.125 | |||||||||||||||
Revised identity is shown in parentheses.
Or amoxicillin.
Or ticarcillin.
Or cefazolin.
Alterations in antibiotic access to the enzyme can markedly change the susceptibility profile. With loss of outer membrane porin channels, K. pneumoniae strains carrying plasmids determining AmpC enzymes can have imipenem MICs as high as 64 μg/ml and meropenem MICs of 16 μg/ml (53). In such strains, MICs of cefepime and cefpirome become inoculum dependent, and at inocula of 107/ml MICs can exceed 256 μg/ml (53). Clinical isolates of K. pneumoniae and E. coli with imipenem MICs from 16 to 64 μg/ml through porin loss and carriage of ACT-1 (13) or CMY-4 (17, 78) have already been reported and are a cause for concern.
The effects of β-lactamase inhibitors on susceptibility is summarized in Table 3. Although commercially available inhibitors, especially sulbactam, caused a modest reduction in MICs of cefoxitin, E. coli derivatives with plasmid-mediated AmpC enzymes were not susceptible to inhibitor combinations, with the possible exception of piperacillin-tazobactam. Resistance was, however, blocked by BRL 42715 (7, 19, 53), Ro 47-8284 (7), Ro 48-1256 (50), or Ro 48-1220 (81).
TABLE 3.
Effect of β-lactamase inhibitors (MIC) on E. coli derivatives producing plasmid-mediated AmpC β-lactamases
| Agent(s) | MIC (μg/ml) (reference no.) for derivatives producing:
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ACC-1a (60) | BIL-1b (CMY-2)h (88) | CMY-1c (9) | CMY-2c (8) | CMY-3b (14) | DHA-1d (26) | DHA-2a (24) | FOX-1e (31) | FOX-2b (10) | FOX-3d (51) | FOX-4d (12) | LAT-1 (81, 83) | MIR-1d (65, 81) | |
| Ampicillin oramoxicillin | >128 | 64 | 2,048 | 1,024 | >512 | >512 | 1,024 | 256 | >128 | 1,000 | |||
| + Clavulanate | >128 | >32 | 128 | 1,024 | >512 | >512 | 32 | 256 | >64g | ≥256 | |||
| Cefoxitin | 256 | 256 | 128 | 256 | 64 | >512 | |||||||
| + Clavulanate | 64 | 128 | 64 | 128 | 64 | >512 | |||||||
| + Sulbactam | 32 | 32 | 32 | ||||||||||
| + Tazobactam | 64 | 64 | 128 | ||||||||||
| Cefotaxime | 8 | 64 | 1 | 64 | |||||||||
| + Clavulanate | >4 | 16 | 1 | 64 | |||||||||
| + Sulbactam | 16 | ||||||||||||
| + Tazobactam | 32 | ||||||||||||
| Ceftazidime | >16 | 4 | 8 | 16 | >128 | 32 | 128 | ||||||
| + Clavulanate | >4 | 4 | 8 | 16 | >128 | 32d | 128 | ||||||
| + Tazobactam | 4d | 16 | |||||||||||
| + Ro 48-1220 | 0.5d | 2 | |||||||||||
| Piperacillin | 32 | 128 | 64 | 64 | |||||||||
| + Tazobactam | 8 | 32 | 16 | 4 | |||||||||
| Ticarcillin | 256 | 1,024 | ≥1,024 | >256 | |||||||||
| + Clavulanate | 128 | 512 | 32 | >128g | |||||||||
Clavulanate at 2 μg/ml and tazobactam at 4 μg/ml.
Inhibitor concentration, 2 μg/ml.
In the proportions of 1:4 (clavulanate), 1:1 (sulbactam), and 1:7 (tazobactam).
Inhibitor concentration, 4 μg/ml.
Inhibitor concentration, 5 μg/ml.
In the proportion of 1:4 (clavulanate), 1:2 (sulbactam), and 1:8 (tazobactam).
Clavulanate at 2 μg/ml with ticarcillin and in the proportion of 1:2 with ampicillin.
Revised identity is shown in parentheses.
DETECTION
In bacterial species without an inducible AmpC-type β-lactamase, appearance of a susceptibility pattern typical of an Enterobacter or C. freundii isolate that overproduces its chromosomal β-lactamase is highly suggestive of a plasmid-encoded AmpC-type enzyme (56, 67). Unfortunately, other mechanisms can produce a similar resistance phenotype. In E. coli hyperproduction of chromosomal AmpC together with OmpF porin loss (52), or in K. pneumoniae porin deficiency alone (33), can give cephamycin and oxyimino-β-lactam resistance. Furthermore, not all strains with plasmid-mediated AmpC enzymes meet the NCCLS criteria for resistance to cephamycins and oxyimino-cephalosporins. For example, E. coli with ACC-1 can be resistant to ceftazidime but not cefoxitin or cefotetan, while a strain with DHA-2 was intermediate in resistance to cefoxitin but susceptible to cefotaxime or ceftazidime (Table 2). Suspected isolates can be studied further for cephamycin hydrolysis with the three-dimensional test (20, 80) or the Masuda bioassay (65) and for β-lactamase inhibitor effects. Unfortunately, inhibitors (BRL 42715, Ro 47-8284, Ro 48-1220, Ro 48-1256) that are active against AmpC enzymes are not readily available, but cloxacillin (69) or cefoxitin (65) have been used to block AmpC activity selectively after isoelectric focusing. Lack of inhibition of activity against oxyimino-β-lactams or cephamycins by clavulanate is indirect evidence for the presence of an AmpC enzyme, but some AmpC enzymes are unusually susceptible to inhibition by tazobactam (1). A reference laboratory is needed for β-lactamase isoelectric focusing or gene localization. Detecting a plasmid-mediated AmpC enzyme in a strain with a native inducible β-lactamase or a coexisting ESBL is even more challenging.
Given the difficulty in detecting plasmid-mediated AmpC β-lactamases, their prevalence is currently likely to be underestimated. Coudron et al. studied 1,286 consecutive, nonrepeat isolates from a single VA Medical Center collected between 1995 and 1997 and estimated that 1.6% of E. coli isolates, 1.1% of K. pneumoniae isolates, and 0.4% of P. mirabilis isolates were cefoxitin-resistant AmpC β-lactamase producers, mostly via transmissible plasmids (20).
ENZYMATIC PROPERTIES
Plasmid-mediated AmpC-type β-lactamases have pIs between 6.4 and 9.4 (Table 1). Several of the FOX-type enzymes show multiple satellite bands (31). In clinical isolates containing several β-lactamases, AmpC enzymes can be identified after isoelectric focusing by differential inhibition of nitrocefin reactivity with 5 mg of cefoxitin/ml (65) or detection of cefoxitin hydrolysis by bioassay (10). A few plasmids carry ampR as well as ampC genes and are inducible (DHA-1 and DHA-2) (3, 24), but most plasmid-mediated ampC genes are expressed constitutively, for example, MIR-1, even in the presence of a complete system for induction (41).
The apparent molecular size of the mature plasmid-mediated AmpC β-lactamases vary from 38 to 42 kDa with 378 (3), 381 (8, 29, 41), 382 (10, 37), or 386 (7) amino acid residues. Kinetic properties were characteristic of chromosomal AmpC enzymes with relative Vmax values generally 10-fold or more greater for cephalothin and cephaloridine than for ampicillin and penicillin, greater activity with penicillin than with ampicillin, and low hydrolysis rates for oxyimino- or α-methoxy-compounds (Table 4). On the other hand, Km values for cefoxitin, cefotetan, cefotaxime, moxalactam, or aztreonam were generally less than those for penicillin or ampicillin and much lower than the Km values for cephaloridine, cephalothin, or cefepime (Table 5).
TABLE 4.
Substrate profile (Vmax relative to cephaloridine) of plasmid-determined AmpC β-lactamases
| Agent |
Vmax (reference no.)
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ACC-1 (7) | ACT-1 (13) | CMY-3 (14) | DHA-1 (26) | FOX-1c (31) | FOX-3 (51) | FOX-4 (12) | LAT-1 (83) | LAT-2 (CMY-2)d (28) | LAT-3 (29) | LAT-4 (LAT-1)d (29) | MIR-1 (65) | MOX-1 (36) | |
| Benzylpenicillin | 7.1 | 5 | 67 | 1.3 | 1.2 | 5 | 3 | 4 | 5 | 4 | |||
| Ampicillina | 1 | 3 | 0.2 | 1 | 1 | 2 | 2 | 1 | 40 | ||||
| Carbenicillinb | <0.1 | <1 | <1 | ||||||||||
| Cephalothin | 110 | 262 | 371 | 320 | 130 | 169 | 138 | 140 | 122 | ||||
| Cefoxitin | <0.01 | 0.11 | <0.1 | 0.74 | <1 | 3.3 | <1 | <1 | |||||
| Cefotetan | <0.01 | 0.014 | 8.3 | ||||||||||
| Ceftazidime | ≤0.1 | <0.1 | 2 | <1 | 0.25 | 1 | 2.2 | 2 | 2 | 3 | 1.5 | ||
| Cefotaxime | <0.02 | 0.006 | <0.1 | <1 | <1 | 0.09 | <1 | 1 | <1 | <1 | 10 | 201 | |
| Moxalactam | <0.1 | <1 | 2.4 | ||||||||||
| Aztreonam | <0.1 | <0.1 | <1 | <1 | 80 | ||||||||
Or amoxicillin.
Or ticarcillin.
Values shown are for pI 6.8 variant. pI 7.2 variant gave similar results.
Revised identity is shown in parentheses.
TABLE 5.
Affinity constants (Km) of plasmid-encoded AmpC β-lactamases
| Agent |
Km (μM) (reference no.)
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| ACC-1 (7) | ACT-1 (13) | BIL-1a (CMY-2)c (66) | CMY-3 (14) | FOX-1b (31) | FOX-3 (51) | FOX-4 (12) | LAT-2 (CMY-2)c (28) | MOX-1 (36) | |
| Benzylpenicillin | 10 | 3 | 43 | 36 | 12 | ||||
| Ampicillin | 8.7 | 23 | 17 | 2.4 | |||||
| Cephalothin | 40 | 224 | 187 | 55 | |||||
| Cephaloridine | 122 | 380 | 90 | 375 | 363 | 1,400 | 10 | 134 | |
| Cefoxitin | 3.7 | 0.2 | 1.3 | 37 | |||||
| Cefotetan | 2.5 | 805 | |||||||
| Cefotaxime | 7 | 0.01 | 0.5 | 1.2 | 1,064 | ||||
| Ceftazidime | 17 | 20 | 115 | 14 | 2.7 | ||||
| Moxalactam | 0.005 | 1.7 | |||||||
| Aztreonam | 0.01 | 40 | |||||||
| Cefepime | 1,040 | ||||||||
| Imipenem | 7.5 | ||||||||
Ki values with nitrocefin as substrate.
Values shown are for pI 6.8 variant; pI 7.2 variant gave similar results.
Revised identity is shown in parentheses.
As is typical of group 1 cephalosporinases (16), plasmid-mediated AmpC enzymes were inhibited by low concentrations of aztreonam, cefoxitin, or cloxacillin and only by high concentrations of clavulanate (Table 6). Sulbactam and particularly tazobactam were more effective inhibitors but were an order of magnitude less potent than Ro 48-1220.
TABLE 6.
Inhibition profiles of plasmid-determined AmpC β-lactamases
| Agent | 50% inhibitory concn (μM) (reference no.)
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ACT-1 (13) | BIL-1 (CMY-2)b (66) | CMY-3a (14) | DHA-1 (26) | FOX-1 (31) | FOX-3 (51) | LAT-1 (28, 81, 83) | LAT-2 (CMY-2)b (28) | LAT-3 (29) | LAT-4 (LAT-1)b (29) | MIR-1 (65) | MOX-1a (36) | |
| Aztreonam | 0.06 | 0.020 | 0.0015 | 0.03 | 0.02 | |||||||
| Cefoxitin | 4.1 | 0.8 | 0.65 | 0.006 | ||||||||
| Clavulanate | 52 | 362 | 140 | >100 | >1 | 3 | >250 | 250 | >100 | >100 | 0.21 | 5.6 |
| Cloxacillin | 0.1 | 0.023 | 0.02 | 0.001 | 0.35 | |||||||
| Ro 48–1220 | 0.8 | 0.7 | 0.8 | |||||||||
| Sulbactam | 2.6 | 18 | 10 | 48 | 50 | |||||||
| Tazobactam | 1.3 | 3.2 | 10 | 0.6 | 13 | 12 | 12 | 0.008 | ||||
| Ticarcillin | 0.01 | |||||||||||
Value shown is Ki instead of 50% inhibitory concentration.
Revised identity is shown in parentheses.
The amino acid sequence of the enzymes revealed an active-site serine in the motif Ser-X-X-Lys (where X is any amino acid) at residues 64 to 67 of the mature protein. A Lys-Ser/Thr-Gly motif has been found at residues 315 to 317 and plays an essential role in forming the tertiary structure of the active site. A tyrosine residue at position 150 forms part of the class C-typical motif Tyr-X-Asn and is also important (but not essential) for catalysis of β-lactam hydrolysis (21, 64)
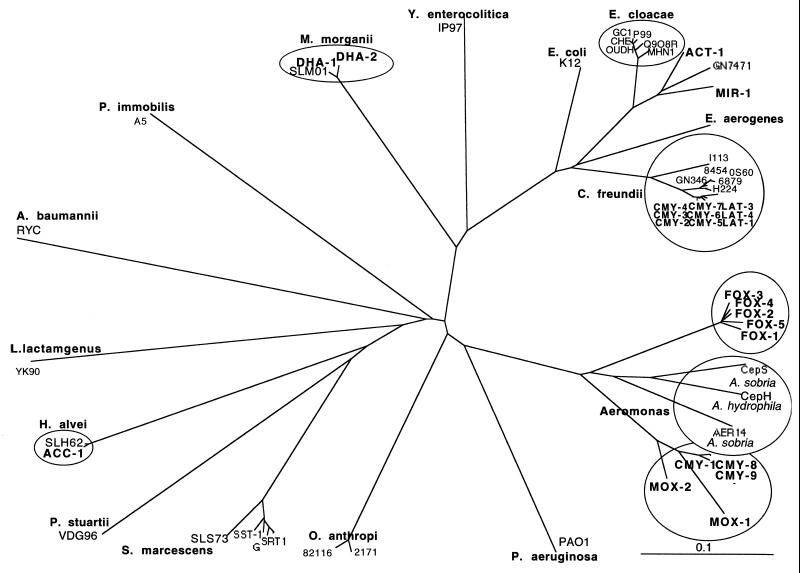
A dendrogram of chromosomal and plasmid-encoded AmpC enzymes (Fig. 1) demonstrates the diversity of chromosomal AmpC genes and the close relationship of some plasmid-mediated enzymes to chromosomal enzymes of particular organisms. The plasmid-mediated enzymes can be divided into five or six clusters: the C. freundii group with LAT types and certain CMY types, the Enterobacter group with MIR-1 and ACT-1, the M. morganii group with DHA-1 and DHA-2, the H. alvei group represented by ACC-1, and the Aeromonas group with MOX-, FOX-, and other CMY-type enzymes. The relationship between plasmid-encoded enzymes and certain chromosomal β-lactamases is very close: there is 100% amino acid homology within the M. morganii and H. alvei groups and more than 94% homology within the C. freundii group. ACT-1 and MIR-1 share 91.4% amino acid identity with each other but only 85 to 87% identity with most E. cloacae AmpC enzymes. However, the enzyme from E. cloacae strain GN7471 (47) has 91.1% identity to ACT-1 and MIR-1, and an environmental strain of Enterobacter was 98% identical (M. Rottman and G. Arlet, personal communication), so that origin from some Enterobacter species is likely. FOX enzymes have 95% or more sequence identity within the group, and CMY-1, CMY-8, and CMY-9 are more than 97% identical, but either group has only about 74% identity with the available Aeromonas sobria AmpC sequences, which in turn differ from each other by fully 25%. The AmpC sequence of P. aeruginosa is even more distant, so the origin of these enzymes remains uncertain.
FIG. 1.
Dendrogram for chromosomal and plasmid-encoded AmpC β-lactamases, calculated by Clustal X (34) and the neighbor-joining method (73). Branch lengths are proportional to the number of amino acid exchanges. GenBank accession numbers for blaAmpC can be found at http://www.rochester.edu/College/BIO/labs/HallLab/AmpC_Phylo.html
Unlike ESBLs, which differ from their parent enzymes by amino acid substitutions that alter the properties of the active site (45), remodeling seems not to be necessary for the success of a plasmid-mediated AmpC enzyme. M. Barlow and B. G. Hall (submitted) found that chromosomal ampC genes from C. freundii strains isolated in the 1920s were just as effective in providing β-lactam resistance as plasmid-mediated ampC alleles such as CMY-2 or LAT-3 when all were cloned into a common vector in a common E. coli host. Nonetheless, once a blaAmpC gene is plasmid-borne further evolution may occur. For example, a naturally occurring Asn→Ile substitution at position 346 in CMY-1 has been reported to increase the ceftazidime MIC for a strain with the variant enzyme by four- to eightfold (A. Bauernfeind, I. Schneider, D. Meyer, R. Jungwirth, Y. Chong, and K. Lee, Abstr. 37th Intersci. Conf. Antimicrob. Agents Chemother., abstr. C-203, 1997). It is likely that in time other such changes will be observed, since a variety of genetic changes can improve the activity of the chromosomal AmpC enzyme of E. cloacae to particular substrates, such as activity toward cefuroxime and ceftazidime with a tandem duplication of three amino acids at positions 208 to 210 (63) or toward cefepime and cefpirome with an amino acid substitution at position 318 (58) or a deletion of six amino acids at residues 289 to 294 (4).
GENETIC FEATURES
Genes for the AmpC enzymes have been located on plasmids of sizes varying from 7 to 180 kb (37, 78). A few of the plasmids have not been self-transmissible but are transferable by transformation (65, 78, 89) or mobilization (28, 29, 82, 83). Plasmids encoding AmpC enzymes often carry multiple other resistances, including resistance to aminoglycosides, chloramphenicol, sulfonamide, tetracycline, trimethoprim, or mercuric ion (9, 10, 13, 65, 78). A plasmid encoding a FOX-type enzyme even carried a gene for fluoroquinolone resistance (54). Clinical isolates often produce other β-lactamases in addition to an AmpC enzyme. The bla genes may be on different plasmids, but often they coexist on the same plasmid. For example, the gene for ACT-1 was found in clinical isolates along with a pI 5.6 β-lactamase consistent with TEM-10 or TEM-26 and a pI 7.6 enzyme consistent with SHV-1, and on cloning the ACT-1 gene was found in a 15-kb cluster with genes for a β-lactamase of pI 5.4, presumably TEM-1, and pI 7.0, possibly another SHV-type enzyme (13). Furthermore, an ACT-1 probe hybridized to chromosomal DNA of these clinical strains, implying mobility of the gene by carriage on a transposon. Indirect evidence suggests that CMY-3 and CMY-4 could be transposon-mediated as well: CMY-3 because its gene is located on the chromosome of a species (P. mirabilis) lacking a native AmpC gene (14), and CMY-4 because in E. coli clinical isolates from London a CMY-4 probe hybridized to both 7-kb and 45-kb plasmids, a dual location that could be explained by transposability (78). The MIR-1 gene is located near a sequence closely related to an insertion sequence transposase, but direct attempts to demonstrate transposability of MIR-1 or BIL-1 (CMY-2) have not been successful (25, 41).
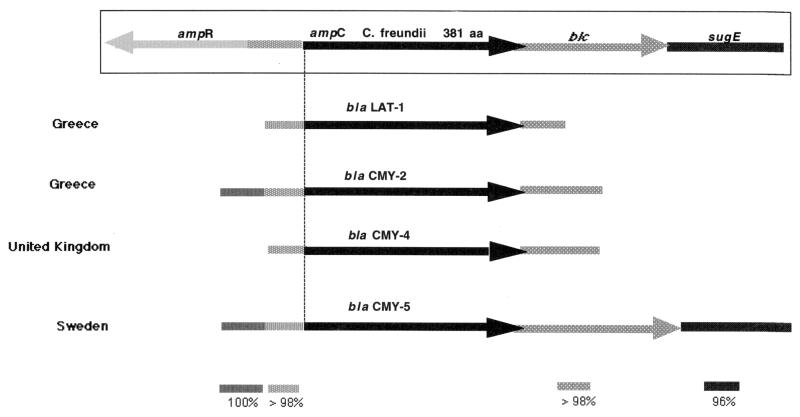
The C. freundii-type blaCMY-5 gene has been mapped in plasmid pTKH11 to be adjacent to the blc and sugE genes found downstream from ampC on the C. freundii chromosome (89). The ampR gene upstream from ampC on the chromosome is missing and its place has been taken by a putative insertion element which could have been involved in gene capture. So far as they have been sequenced, other plasmids encoding C. freundii-type AmpC enzymes have a similar organization (Fig. 2), suggesting a direct derivation from the C. freundii chromosome with subsequent accumulation of mutations in the ampC gene to produce the present array of CMY- and LAT-type enzymes, a conclusion also supported by phylogenetic analysis (M. Barlow and B. G. Hall, submitted).
FIG. 2.
Comparative genetic organization of plasmid-encoded ampC genes related to the chromosomal β-lactamase gene of C. freundii. Adjacent nucleotide homology is that available for each gene and may be more extensive if carried further.
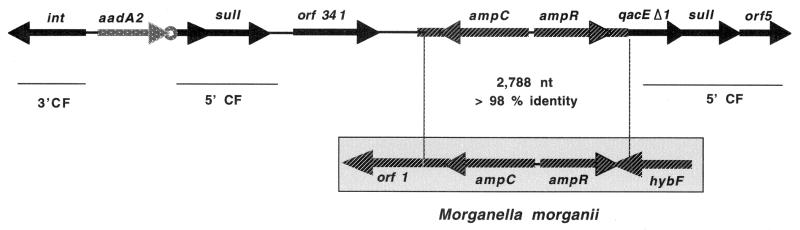
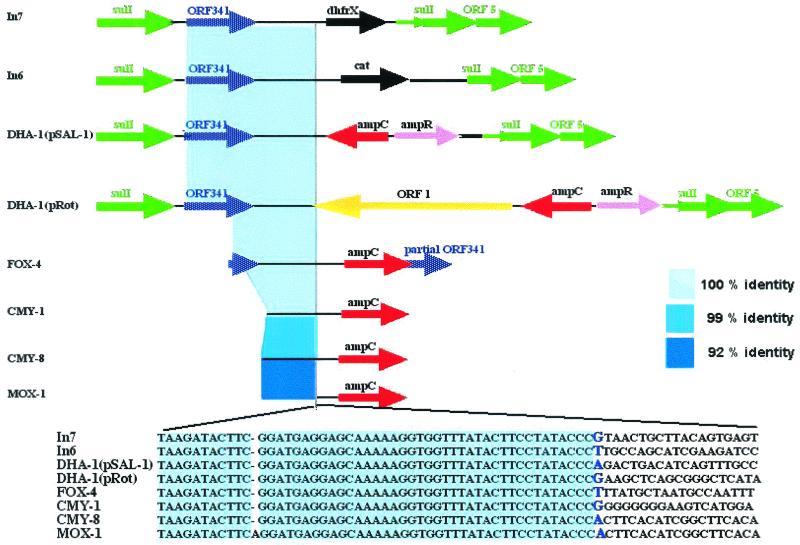
Many resistance genes, including those for Ambler class A, B, and D β-lactamases, are located in gene cassettes with a downstream 59-base element that acts as a specific recombination site for incorporation into integrons (32). Analysis of published sequences indicates that AmpC genes found on plasmids are not linked to 59-base elements. The DHA-1 structural and regulatory genes on plasmid pSAL-1, however, are present in an integron (Fig. 3) which includes a site-specific integrase, two copies of qacEΔ1sulI, an aadA2 gene for aminoglycoside resistance with its downstream 59-base element, and ORF341, a postulated recombinase (84). The genetic organization of this integron is similar to In6 and In7 found in plasmids pSa and pDGO100, which lack bla genes (79). ampC and ampR genes from the chromosome of M. morganii (2, 70) thus appear to have inserted into a complex sulI-type integron. Since no downstream 59-base element remains, either it was deleted or integration involved another mechanism. Verdet et al. identified a 50-bp sequence near blaDHA-1 that is present also in In6 and In7. A virtually identical sequence occurs near genes for FOX-4, CMY-1, CMY-8, and MOX-1 (Fig. 4). Such a sequence could represent a recombination site different from the 59-base element. Further study of the structure of plasmids carrying ampC genes is likely to reveal additional tricks used by bacteria to mobilize genes for dissemination.
FIG. 3.
Structure of the integron coding for DHA-1 β-lactamase in pSAL-1 and its relationship to genes on the chromosome of M. morganii.
FIG. 4.
Comparison of the sequence between common regions of In7, In6, pSAL-1 (DHA-1), pROT (DHA-1), pGC-2 (FOX-4), pMVP-1 (CMY-1), pKPW142 (CMY-8), and pRMOX-1 (MOX-1).
CONCLUSIONS
Among gram-negative bacteria, the emergence of resistance to expanded-spectrum cephalosporins has been a major concern, initially in a limited number of bacterial species (E. cloacae, C. freundii, S. marcescens, and P. aeruginosa) that could mutate to hyperproduce their chromosomal class C β-lactamase. A few years later, resistance appeared in bacterial species not naturally producing AmpC enzymes (K. pneumoniae, Salmonella spp., P. mirabilis) due to the production of TEM- or SHV-type ESBLs. Characteristically, such resistance has included oxyimino- but not 7-α-methoxy-cephalosporins, has been blocked by inhibitors such as clavulanate, sulbactam, or tazobactam, and did not involve carbapenems. Plasmid-mediated AmpC β-lactamases represent a new threat since they confer resistance to 7-α-methoxy-cephalosporins such as cefoxitin or cefotetan, are not affected by commercially available β-lactamase inhibitors, and can, in strains with loss of outer membrane porins, provide resistance to carbapenems. This resistance mechanism has been found around the world, can cause nosocomial outbreaks, appears to be increasing in prevalence, and merits further study to define the best options for detection and treatment.
ADDENDUM
The sequence of ORF341 has recently been revised, extending the open reading frame to 1,541 nucleotides that encode a protein of 513 amino acids; this sequence has been renamed ORF 513 (GenBank accession no. L06418).
REFERENCES
- 1.Babini, G. S., F. Danel, S. D. Munro, P. A. Micklesen, and D. M. Livermore. 1998. Unusual tazobactam-sensitive AmpC β-lactamase from two Escherichia coli isolates. J. Antimicrob. Chemother. 41:115–118. [DOI] [PubMed] [Google Scholar]
- 2.Barnaud, G., G. Arlet, C. Danglot, and A. Philippon. 1997. Cloning and sequencing of the gene encoding the AmpC β-lactamase of Morganella morganii. FEMS Microbiol. Lett. 148:15–20. [DOI] [PubMed] [Google Scholar]
- 3.Barnaud, G., G. Arlet, C. Verdet, O. Gaillot, P. H. Lagrange, and A. Philippon. 1998. Salmonella enteritidis: AmpC plasmid-mediated inducible β-lactamase (DHA-1) with an ampR gene from Morganella morganii. Antimicrob. Agents Chemother. 42:2352–2358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barnaud, G., R. Labia, L. Raskine, M. J. Sanson-Le Pors, A. Philippon, and G. Arlet. 2001. Extension of resistance to cefepime and cefpirome associated to a six amino acid deletion in the H-10 helix of the cephalosporinase of an Enterobacter cloacae clinical isolate. FEMS Microbiol. Lett. 195:185–190. [DOI] [PubMed] [Google Scholar]
- 5.Bauernfeind, A., Y. Chong, and K. Lee. 1998. Plasmid-encoded AmpC β-lactamases: how far have we gone 10 years after the discovery. Yonsei Med. J. 39:520–525. [DOI] [PubMed] [Google Scholar]
- 6.Bauernfeind, A., Y. Chong, and S. Schweighart. 1989. Extended broad spectrum β-lactamase in Klebsiella pneumoniae including resistance to cephamycins. Infection 17:316–321. [DOI] [PubMed] [Google Scholar]
- 7.Bauernfeind, A., I. Schneider, R. Jungwirth, H. Sahly, and U. Ullmann. 1999. A novel type of AmpC β-lactamase, ACC-1, produced by a Klebsiella pneumoniae strain causing nosocomial pneumonia. Antimicrob. Agents Chemother. 43:1924–1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bauernfeind, A., I. Stemplinger, R. Jungwirth, and H. Giamarellou. 1996. Characterization of the plasmidic β-lactamase CMY-2, which is responsible for cephamycin resistance. Antimicrob. Agents Chemother. 40:221–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bauernfeind, A., I. Stemplinger, R. Jungwirth, R. Wilhelm, and Y. Chong. 1996. Comparative characterization of the cephamycinase blaCMY-1 gene and its relationship with other β-lactamase genes. Antimicrob. Agents Chemother. 40:1926–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bauernfeind, A., S. Wagner, R. Jungwirth, I. Schneider, and D. Meyer. 1997. A novel class C β-lactamase (FOX-2) in Escherichia coli conferring resistance to cephamycins. Antimicrob. Agents Chemother. 41:2041–2046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bobrowski, M. M., M. Matthew, P. T. Barth, N. Datta, N. J. Grinter, A. E. Jacob, P. Kontomichalou, J. W. Dale, and J. T. Smith. 1976. Plasmid-determined β-lactamase indistinguishable from the chromosomal β-lactamase of Escherichia coli. J. Bacteriol. 125:149–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bou, G., A. Oliver, M. Ojeda, C. Monzón, and J. Martínez-Beltran. 2000. Molecular characterization of FOX-4, a new AmpC-type plasmid-mediated β-lactamase from an Escherichia coli strain isolated in Spain. Antimicrob. Agents Chemother. 44:2549–2553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bradford, P. A., C. Urban, N. Mariano, S. J. Projan, J. J. Rahal, and K. Bush. 1997. Imipenem resistance in Klebsiella pneumoniae is associated with the combination of ACT-1, a plasmid-mediated AmpC β-lactamase, and the loss of an outer membrane protein. Antimicrob. Agents Chemother. 41:563–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bret, L., C. Chanal-Claris, D. Sirot, E. B. Chaibi, R. Labia, and J. Sirot. 1998. Chromosomally encoded ampC-type β-lactamase in a clinical isolate of Proteus mirabilis. Antimicrob. Agents Chemother. 42:1110–1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brun-Buisson, C., P. Legrand, A. Philippon, F. Montravers, M. Ansquer, and J. Duval. 1987. Transferable enzymatic resistance to third-generation cephalosporins during nosocomial outbreak of multiresistant Klebsiella pneumoniae. Lancet ii:302–306. [DOI] [PubMed] [Google Scholar]
- 16.Bush, K., G. A. Jacoby, and A. A. Medeiros. 1995. A functional classification scheme for β-lactamases and its correlation with molecular structure. Antimicrob. Agents Chemother. 39:1211–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cao, V. T., G. Arlet, B. M. Ericsson, A. Tammelin, P. Courvalin, and T. Lambert. 2000. Emergence of imipenem resistance in Klebsiella pneumoniae owing to combination of plasmid-mediated CMY-4 and permeability alteration. J. Antimicrob. Chemother. 46:895–900. [DOI] [PubMed] [Google Scholar]
- 18.Caroff, N., E. Espaze, D. Gautreau, H. Richet, and A. Reynaud. 2000. Analysis of the effects of −42 and −32 ampC promoter mutations in clinical isolates of Escherichia coli hyperproducing AmpC. J. Antimicrob. Chemother. 45:783–788. [DOI] [PubMed] [Google Scholar]
- 19.Coleman, K., D. R. Griffin, J. W. Page, and P. A. Upshon. 1989. In vitro evaluation of BRL 42715, a novel β-lactamase inhibitor. Antimicrob. Agents Chemother. 33:1580–1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coudron, P. E., E. S. Moland, and K. S. Thomson. 2000. Occurrence and detection of AmpC β-lactamases among Escherichia coli, Klebsiella pneumoniae, and Proteus mirabilis isolates at a Veterans’ Medical Center. J. Clin. Microbiol. 38:1791–1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dubus, A., S. Normarck, M. Kania, and M. G. P. Page. 1994. The role of tyrosine 150 in catalysis of β-lactam hydrolysis by AmpC β-lactamase from Escherichia coli investigated by site-directed mutagenesis. Biochemistry 33:8577–8586. [DOI] [PubMed] [Google Scholar]
- 22.Dunne, E. F., P. D. Fey, P. Kludt, R. Reporter, F. Mostashari, P. Shillam, J. Wicklund, C. Miller, B. Holland, K. Stamey, T. J. Barrett, J. K. Rasheed, F. C. Tenover, E. M. Ribot, and F. J. Angulo. 2000. Emergence of domestically acquired ceftriaxone-resistant Salmonella infections associated with AmpC β-lactamase. JAMA 284:3151–3156. [DOI] [PubMed] [Google Scholar]
- 23.Fey, P. D., T. J. Safranek, M. E. Rupp, E. F. Dunne, E. I. P. C. Ribot, P. A. Bradford, F. J. Angulo, and S. H. Hinrichs. 2000. Ceftriaxone-resistant salmonella infection acquired by a child from cattle. N. Engl. J. Med. 342:1242–1249. [DOI] [PubMed] [Google Scholar]
- 24.Fortineau, N., L. Poirel, and P. Nordmann. 2001. Plasmid-mediated and inducible cephalosporinase DHA-2 from Klebsiella pneumoniae. J. Antimicrob. Chemother. 47:207–210. [DOI] [PubMed] [Google Scholar]
- 25.Fosberry, A. P., D. J. Payne, E. J. Lawlor, and J. E. Hodgson. 1994. Cloning and sequence analysis of blaBIL-1, a plasmid-mediated class C β-lactamase in Escherichia coli BS. Antimicrob. Agents Chemother. 38:1182–1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gaillot, O., C. Clement, M. Simonet, and A. Philippon. 1997. Novel transferable β-lactam resistance with cephalosporinase characteristics in Salmonella enteritidis. J. Antimicrob. Chemother. 39:85–87. [DOI] [PubMed] [Google Scholar]
- 27.Gazouli, M., M. E. Kaufmann, E. Tzelepi, H. Dimopoulou, O. Paniara, and L. S. Tzouvelekis. 1997. Study of an outbreak of cefoxitin-resistant Klebsiella pneumoniae in a general hospital. J. Clin. Microbiol. 35:508–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gazouli, M., L. S. Tzouvelekis, E. Prinarakis, V. Miriagou, and E. Tzelepi. 1996. Transferable cefoxitin resistance in enterobacteria from Greek hospitals and characterization of a plasmid-mediated group 1 β-lactamase (LAT-2). Antimicrob. Agents Chemother. 40:1736–1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gazouli, M., L. S. Tzouvelekis, A. C. Vatopoulos, and E. Tzelepi. 1998. Transferable class C β-lactamases in Escherichia coli strains isolated in Greek hospitals and characterization of two enzyme variants (LAT-3 and LAT-4) closely related to Citrobacter freundii AmpC β- lactamase. J. Antimicrob. Chemother. 42:419–425. [DOI] [PubMed] [Google Scholar]
- 30.Girlich, D., A. Karim, C. Spicq, and P. Nordmann. 2000. Plasmid-mediated cephalosporinase ACC-1 in clinical isolates of Proteus mirabilis and Escherichia coli. Eur. J. Clin. Microbiol. Infect. Dis. 19:893–895. [DOI] [PubMed] [Google Scholar]
- 31.Gonzalez Leiza, M., J. C. Perez-Diaz, J. Ayala, J. M. Casellas, J. Martinez-Beltran, K. Bush, and F. Baquero. 1994. Gene sequence and biochemical characterization of FOX-1 from Klebsiella pneumoniae, a new AmpC-type plasmid-mediated β-lactamase with two molecular variants. Antimicrob. Agents Chemother. 38:2150–2157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hall, R. M., and C. M. Collis. 1998. Antibiotic resistance in gram-negative bacteria: the role of gene cassettes and integrons. Drug Resist. Updates 1:109–119. [DOI] [PubMed] [Google Scholar]
- 33.Hernández-Allés, S., M. C. Conejo, A. Pascual, J. M. Tomás, V. J. Benedí, and L. Martínez-Martínez. 2000. Relationship between outer membrane alterations and susceptibility to antimicrobial agents in isogenic strains of Klebsiella pneumoniae. J. Antimicrob. Chemother. 46:273–277. [DOI] [PubMed] [Google Scholar]
- 34.Higgins, D. G., A. J. Bleasby, and R. Fuchs. 1992. CLUSTAL V: improved software for multiple sequence alignment. Comput. Appl. Biosci. 8:189–191. [DOI] [PubMed] [Google Scholar]
- 35.Honoré, N., M. H. Nicolas, and S. T. Cole. 1986. Inducible cephalosporinase production in clinical isolates of Enterobacter cloacae is controlled by a regulatory gene that has been deleted from Escherichia coli. EMBO J. 5:3709–3714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Horii, T., Y. Arakawa, M. Ohta, S. Ichiyama, R. Wacharotayankun, and N. Kato. 1993. Plasmid-mediated AmpC-type β-lactamase isolated from Klebsiella pneumoniae confers resistance to broad-spectrum β-lactams, including moxalactam. Antimicrob. Agents Chemother. 37:984–990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Horii, T., Y. Arakawa, M. Ohta, T. Sugiyama, R. Wacharotayankun, H. Ito, and N. Kato. 1994. Characterization of a plasmid-borne and constitutively expressed blaMOX-1 gene encoding AmpC-type β-lactamase. Gene 139:93–98. [DOI] [PubMed] [Google Scholar]
- 38.Jacobs, C., J.-M. Frère, and S. Normark. 1997. Cytosolic intermediates for cell wall biosynthesis and degradation control inducible β-lactam resistance in gram-negative bacteria. Cell 88:823–832. [DOI] [PubMed] [Google Scholar]
- 39.Jacoby, G. A. 1994. Genetics of extended-spectrum beta-lactamases. Eur. J. Clin. Microbiol. Infect. Dis. 13(Suppl. 1):2–11. [DOI] [PubMed] [Google Scholar]
- 40.Jacoby, G. A., and A. A. Medeiros. 1991. More extended-spectrum β-lactamases. Antimicrob. Agents Chemother. 35:1697–1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jacoby, G. A., and J. Tran. 1999. Sequence of the MIR-1 β-lactamase gene. Antimicrob. Agents Chemother. 43:1759–1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jaurin, B., T. Grundström, T. Edlund, and S. Normark. 1981. The E. coli β-lactamase attenuator mediates growth rate-dependent regulation. Nature 290:221–225. [DOI] [PubMed] [Google Scholar]
- 43.Jenks, P. J., Y. M. Hu, F. Danel, S. Mehtar, and D. M. Livermore. 1995. Plasmid-mediated production of class I (AmpC) β-lactamase by two Klebsiella pneumoniae isolates from the UK. J. Antimicrob. Chemother. 35:235–236. [DOI] [PubMed] [Google Scholar]
- 44.Knothe, H., P. Shah, V. Krcmery, M. Antal, and S. Mitsuhashi. 1983. Transferable resistance to cefotaxime, cefoxitin, cefamandole and cefuroxime in clinical isolates of Klebsiella pneumoniae and Serratia marcescens. Infection 11:315–317. [DOI] [PubMed] [Google Scholar]
- 45.Knox, J. R. 1995. Extended-spectrum and inhibitor-resistant TEM-type β-lactamases: mutations, specificity, and three-dimensional structure. Antimicrob. Agents Chemother. 39:2593–2601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Koeck, J. L., G. Arlet, A. Philippon, S. Basmaciogullari, H. V. Thien, Y. Buisson, and J. D. Cavallo. 1997. A plasmid-mediated CMY-2 β-lactamase from an Algerian clinical isolate of Salmonella senftenberg. FEMS Microbiol. Lett. 152:255–260. [DOI] [PubMed] [Google Scholar]
- 47.Kuga, A., R. Okamoto, and M. Inoue. 2000. ampR gene mutations that greatly increase class C β-lactamase activity in Enterobacter cloacae. Antimicrob. Agents Chemother. 44:561–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Levesque, R., P. H. Roy, R. Letarte, and J. C. Pechère. 1982. A plasmid-mediated cephalosporinase from Achromobacter species. J. Infect. Dis. 145:753–761. [DOI] [PubMed] [Google Scholar]
- 49.Livermore, D. M. 1995. β-lactamases in laboratory and clinical resistance. Clin. Microbiol. Rev. 8:557–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Livermore, D. M., and M. Yuan. 1996. Antibiotic resistance and production of extended-spectrum β-lactamases amongst Klebsiella spp. from intensive care units in Europe. J. Antimicrob. Chemother. 38:409–424. [DOI] [PubMed] [Google Scholar]
- 51.Marchese, A., G. Arlet, G. C. Schito, P. H. Lagrange, and A. Philippon. 1998. Characterization of FOX-3, an AmpC-type plasmid-mediated β-lactamase from an Italian isolate of Klebsiella oxytoca. Antimicrob. Agents Chemother. 42:464–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Martínez-Martínez, L., M. C. Conejo, A. Pascual, S. Hernández-Allés, S. Ballesta, E. Ramírez De Arellano-Ramos, V. J. Benedí, and E. J. Perea. 2000. Activities of imipenem and cephalosporins against clonally related strains of Escherichia coli hyperproducing chromosomal β-lactamase and showing altered porin profiles. Antimicrob. Agents Chemother. 44:2534–2536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Martínez-Martínez, L., A. Pascual, S. Hernández-Allés, D. Alvarez-Díaz, A. I. Suárez, J. Tran, V. J. Benedí, and G. A. Jacoby. 1999. Roles of β-lactamases and porins in activities of carbapenems and cephalosporins against Klebsiella pneumoniae. Antimicrob. Agents Chemother. 43:1669–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Martínez-Martínez, L., A. Pascual, and G. A. Jacoby. 1998. Quinolone resistance from a transferable plasmid. Lancet 351:797–799. [DOI] [PubMed] [Google Scholar]
- 55.Maurelli, A. T., R. E. Fernández, C. A. Bloch, C. K. Rode, and A. Fasano. 1998. “Black holes” and bacterial pathogenicity: a large genomic deletion that enhances the virulence of Shigella spp. and enteroinvasive Escherichia coli. Proc. Natl. Acad. Sci. USA 95:3943–3948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Medeiros, A. 1997. Evolution and dissemination of β-lactamases accelerated by generations of β-lactam antibiotics. Clin. Infect. Dis. 24:S19–S45. [DOI] [PubMed] [Google Scholar]
- 57.Morosini, M. I., J. A. Ayala, F. Baquero, J. L. Martínez, and J. Blázquez. 2000. Biological cost of AmpC production for Salmonella enterica serotype Typhimurium. Antimicrob. Agents Chemother. 44:3137–3143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Morosini, M. I., M. C. Negri, B. Shoichet, M. R. Baquero, F. Baquero, and J. Blázquez. 1998. An extended-spectrum AmpC-type β-lactamase obtained by in vitro antibiotic selection. FEMS Microbiol. Lett. 165:85–90. [DOI] [PubMed] [Google Scholar]
- 59.M’Zali, F. H., J. Heritage, D. M. Gascoyne-Binzi, M. Denton, N. J. Todd, and P. M. Hawkey. 1997. Transcontinental importation into the UK of Escherichia coli expressing a plasmid-mediated AmpC-type β-lactamase exposed during an outbreak of SHV-5 extended-spectrum β-lactamase in a Leeds hospital. J. Antimicrob. Chemother. 40:823–831. [DOI] [PubMed] [Google Scholar]
- 60.Nadjar, D., M. Rouveau, C. Verdet, J. Donay, J. Herrmann, P. H. Lagrange, A. Philippon, and G. Arlet. 2000. Outbreak of Klebsiella pneumoniae producing transferable AmpC-type β-lactamase (ACC-1) originating from Hafnia alvei. FEMS Microbiol. Lett. 187:35–40. [DOI] [PubMed] [Google Scholar]
- 61.Naumovski, L., J. P. Quinn, D. Miyashiro, M. Patel, K. Bush, S. B. Singer, D. Graves, T. Palzkill, and A. M. Arvin. 1992. Outbreak of ceftazidime resistance due to a novel extended-spectrum β-lactamase in isolates from cancer patients. Antimicrob. Agents Chemother. 36:1991–1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nelson, E. C., and B. G. Elisha. 1999. Molecular basis of AmpC hyperproduction in clinical isolates of Escherichia coli. Antimicrob. Agents Chemother. 43:957–959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nukaga, M., S. Haruta, K. Tanimoto, K. Kogure, K. Taniguchi, M. Tamaki, and T. Sawai. 1995. Molecular evolution of a class C β-lactamase extending its substrate specificity. J. Biol. Chem. 270:5729–5735. [DOI] [PubMed] [Google Scholar]
- 64.Oefner, C., A. D’Arcy, J. J. Daly, K. Gubernator, R. L. Charnas, I. Heinze, C. Hubschwerlen, and F. K. Winkler. 1990. Refined crystal structure of β-lactamase from Citrobacter freundii indicates a mechanism for β-lactam hydrolysis. Nature 343:284–288. [DOI] [PubMed] [Google Scholar]
- 65.Papanicolaou, G. A., A. A. Medeiros, and G. A. Jacoby. 1990. Novel plasmid-mediated β-lactamase (MIR-1) conferring resistance to oxyimino- and α-methoxy β-lactams in clinical isolates of Klebsiella pneumoniae. Antimicrob. Agents Chemother. 34:2200–2209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Payne, D. J., N. Woodford, and S. G. B. Amyes. 1992. Characterization of the plasmid mediated β-lactamase BIL-1. J. Antimicrob. Chemother. 30:119–127. [DOI] [PubMed] [Google Scholar]
- 67.Philippon, A., G. Arlet, and P. H. Lagrange. 1994. Origin and impact of plasmid-mediated extended-spectrum beta-lactamases. Eur. J. Clin. Microbiol. Infect. Dis. 13(Suppl. 1):17–29. [DOI] [PubMed] [Google Scholar]
- 68.Philippon, A., R. Labia, and G. Jacoby. 1989. Extended-spectrum β-lactamases. Antimicrob. Agents Chemother. 33:1131–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pitout, J. D., K. S. Thomson, N. D. Hanson, A. F. Ehrhardt, E. S. Moland, and C. C. Sanders. 1998. β-Lactamases responsible for resistance to expanded-spectrum cephalosporins in Klebsiella pneumoniae, Escherichia coli, and Proteus mirabilis isolates recovered in South Africa. Antimicrob. Agents Chemother. 42:1350–1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Poirel, L., M. Guibert, D. Girlich, T. Naas, and P. Nordmann. 1999. Cloning, sequence analyses, expression, and distribution of ampC-ampR from Morganella morganii clinical isolates. Antimicrob. Agents Chemother. 43:769–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rhimi-Mahjoubi, F., M. Bernier, G. Arlet, Z. Ben Jemaa, P. Jouve, A. Hammami, and A. Philippon. Mise en évidence de la céphalosporinase plasmidique ACC-1 dans différentes entérobactéries (Klebsiella pneumoniae, Proteus mirabilis, Salmonella) isolées dans un hopital Tunisien (Sfax, 1997–2000). Path. Biol., in press. [DOI] [PubMed]
- 72.Rice, L. B., S. H. Willey, G. A. Papanicolaou, A. A. Medeiros, G. M. Eliopoulos, R. C. Moellering, Jr., and G. A. Jacoby. 1990. Outbreak of ceftazidime resistance caused by extended-spectrum β-lactamases at aMassachusetts chronic-care facility. Antimicrob. Agents Chemother. 34:2193–2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Saitou, N., and M. Nei. 1987. The neighbor-joining method: a new method for reconstructing phylogenetic trees. Mol. Biol. Evol. 4:406–425. [DOI] [PubMed] [Google Scholar]
- 74.Sanders, C. C. 1987. Chromosomal cephalosporinases responsible for multiple resistance to newer β-lactam antibiotics. Annu. Rev. Microbiol. 41:573–593. [DOI] [PubMed] [Google Scholar]
- 75.Sanders, C. C. 1992. β-lactamases of gram-negative bacteria: new challenges for new drugs. Clin. Infect. Dis. 14:1089–1099. [DOI] [PubMed] [Google Scholar]
- 76.Sanderson, K. E., A. Hessel, and K. E. Rudd. 1995. Genetic map of Salmonella typhimurium, edition VIII. Microbiol. Rev. 59:241–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shannon, K. P., A. King, I. Phillips, M. H. Nicolas, and A. Philippon. 1990. Importation of organisms producing broad-spectrum SHV-group β-lactamases into the United Kingdom. J. Antimicrob. Chemother. 25:343–351. [DOI] [PubMed] [Google Scholar]
- 78.Stapleton, P. D., K. P. Shannon, and G. L. French. 1999. Carbapenem resistance in Escherichia coli associated with plasmid-determined CMY-4 β-lactamase production and loss of an outer membrane protein. Antimicrob. Agents Chemother. 43:1206–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Stokes, H. W., C. Tomaras, Y. Parsons, and R. M. Hall. 1993. The partial 3′-conserved segment duplications in the integrons In6 from pSa and In7 from pDGO100 have a common origin. Plasmid 30:39–50. [DOI] [PubMed] [Google Scholar]
- 80.Thomson, K. S., and C. C. Sanders. 1992. Detection of extended-spectrum β-lactamases in members of the family Enterobacteriaceae: comparison of the double-disk and three-dimensional tests. Antimicrob. Agents Chemother. 36:1877–1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tzouvelekis, L. S., M. Gazouli, E. E. Prinarakis, E. Tzelepi, and N. J. Legakis. 1997. Comparative evaluation of the inhibitory activities of the novel penicillanic acid sulfone Ro 48–1220 against β-lactamases that belong to groups 1, 2b, and 2be. Antimicrob. Agents Chemother. 41:475–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tzouvelekis, L. S., E. Tzelepi, and A. F. Mentis. 1994. Nucleotide sequence of a plasmid-mediated cephalosporinase gene (blaLAT-1) found in Klebsiella pneumoniae. Antimicrob. Agents Chemother. 38:2207–2209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tzouvelekis, L. S., E. Tzelepi, A. F. Mentis, and A. Tsakris. 1993. Identification of a novel plasmid-mediated β-lactamase with chromosomal cephalosporinase characteristics from Klebsiella pneumoniae. J. Antimicrob. Chemother. 31:645–654. [DOI] [PubMed] [Google Scholar]
- 84.Verdet, C., G. Arlet, G. Barnaud, P. H. Lagrange, and A. Philippon. 2000. A novel integron in Salmonella enterica serovar Enteritidis, carrying the bla(DHA-1) gene and its regulator gene ampR, originated from Morganella morganii. Antimicrob. Agents Chemother. 44:222–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Verdet, C., G. Arlet, S. Ben Redjeb, A. Ben Hassen, P. H. Lagrange, and A. Philippon. 1998. Characterisation of CMY-4, an AmpC-type plasmid-mediated β-lactamase in a Tunisian clinical isolate of Proteus mirabilis. FEMS Microbiol. Lett. 169:235–240. [DOI] [PubMed] [Google Scholar]
- 86.Wiedemann, B., H. Dietz, and D. Pfeifle. 1998. Induction of β-lactamase in Enterobacter cloacae. Clin. Infect. Dis. 27(Suppl. 1):S42–S47. [DOI] [PubMed] [Google Scholar]
- 87.Winokur, P. L., A. Brueggemann, D. L. DeSalvo, L. Hoffmann, M. D. Apley, E. K. Uhlenhopp, M. A. Pfaller, and G. V. Doern. 2000. Animal and human multidrug-resistant, cephalosporin-resistant Salmonella isolates expressing a plasmid-mediated CMY-2 AmpC β-lactamase. Antimicrob. Agents Chemother. 44:2777–2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Woodford, N., D. J. Payne, A. P. Johnson, M. J. Weinbren, R. M. Perinpanayagam, R. C. George, B. D. Cookson, and S. G. B. Amyes. 1990. Transferable cephalosporin resistance not inhibited by clavulanate in Escherichia coli. Lancet 336:253. [DOI] [PubMed] [Google Scholar]
- 89.Wu, S. W., K. Dornbusch, G. Kronvall, and M. Norgren. 1999. Characterization and nucleotide sequence of a Klebsiella oxytoca cryptic plasmid encoding a CMY-type β-lactamase: confirmation that the plasmid-mediated cephamycinase originated from the Citrobacter freundii AmpC β-lactamase. Antimicrob. Agents Chemother. 43:1350–1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wu, S. W., K. Dornbusch, M. Norgren, and G. Kronvall. 1992. Extended spectrum β-lactamase from Klebsiella oxytoca, not belonging to the TEM or SHV family. J. Antimicrob. Chemother. 30:3–16. [DOI] [PubMed] [Google Scholar]
- 91.Yan, J.-J., S.-M. Wu, S.-H. Tsai, J.-J. Wu, and I.-J. Su. 2000. Prevalence of SHV-12 among clinical isolates of Klebsiella pneumoniae producing extended-spectrum β-lactamases and identification of a novel AmpC enzyme (CMY-8) in Southern Taiwan. Antimicrob. Agents Chemother. 44:1438–1442. [DOI] [PMC free article] [PubMed] [Google Scholar]