Abstract
Mycoplasma gallisepticum enrofloxacin-resistant mutants were generated by stepwise selection in increasing concentrations of enrofloxacin. Alterations were found in the quinolone resistance-determining regions of the four target genes encoding DNA gyrase and topoisomerase IV from these mutants. This is the first description of such mutations in an animal mycoplasma species.
Mycoplasma gallisepticum is responsible for chronic respiratory diseases of chickens and sinusitis of turkeys (17). Control by antimicrobials is sometimes necessary to minimize its transmission in case of an outbreak. M. gallisepticum is known to be susceptible to several antimicrobials (10, 17) but can develop resistance against some of the quinolones used in veterinary medicine (14). Unlike human mollicutes (3, 5, 16), mechanisms involved in fluoroquinolone resistance are unknown in veterinary mycoplasmas. Most of the reported mutations involved in quinolone resistance are concentrated in the quinolone resistance-determining regions (QRDRs) of the gyrA and parC genes of DNA gyrase and topoisomerase IV, respectively (3, 16, 18, 19, 22, 23). However, some mutations in the gyrB and parE QRDRs were found to be responsible for low-level resistance to fluoroquinolones (4, 5, 13). The QRDRs of the gyrA, gyrB, and parE genes of M. gallisepticum were previously described (8, 20), but reports of their implication in fluoroquinolone resistance have never been published. In this study, we report the complete sequence of the parC QRDR of M. gallisepticum and the different alterations of the four QRDRs associated with quinolone resistance in mutants selected in vitro.
Two strains of M. gallisepticum, ATCC 15302, a reference strain (26), and 41-91, a field strain (15), were used in the selection. Strains were grown in Frey agar or broth medium (15). Flumequine, norfloxacin, ofloxacin, and oxolinic acid used for the MIC determinations were purchased from Sigma-Aldrich (Saint Quentin Fallavier, France), while danofloxacin came from Pfizer (Amboise, France), marbofloxacin came from Vétoquinol (Magny-Vernois, France), difloxacin came from Fort Dodge Animal Health (Princeton, N.J.), and enrofloxacin and ciprofloxacin came from Bayer Pharma (Puteaux, France).
Selection of enrofloxacin-resistant mutants was performed by serial transfers and incubations in Frey broth medium containing subinhibitory concentrations of enrofloxacin at 37°C for 5 days. The drug concentrations were gradually increased. This process was repeated 10 times. The MICs for the cloned resistant strains were determined by an agar dilution method (6) on Frey medium. Antimicrobial concentrations ranged between 0.03 and 64 μg/ml. Plate contents were incubated at 37°C in a 5% CO2 atmosphere for 5 days.
DNAs were prepared according to standard methods. Amplifications of the QRDRs of gyrA and gyrB and of parE were performed with specific primers designed from the M. gallisepticum S6 strain sequences (8) and from the M. gallisepticum A5969 strain sequence (20), respectively. The 3" terminal region encoding the ParC QRDR was unknown for M. gallisepticum. Amplification of the parC QRDR was initially performed with primers chosen from the M. gallisepticum A5969 parC sequence (20) and from the alignment of known nucleotide sequences of different bacteria (1, 2, 7, 12). The nucleotide sequences obtained were then used to determine two new internal primers, ParCD3 (5"-GAAGAATAGATGGATAAGAAA-3") and ParCR6 (5"-GTCTCTTTGTTAATATTCTCA-3").
PCR was performed with a Perkin-Elmer 9600 thermal cycler in a total volume of 50 μl containing a 0.2 μM concentration of each primer (Oligo Express, Montreuil, France), a 200 μM concentration of each deoxynucleoside triphosphate (Pharmacia Biotech, Orsay, France), 5 μl of 10× EXTRA-POL I Taq buffer, and 1 U of EXTRA-POL I Taq polymerase (Eurobio, les Ulis, France). After 5 min at 95°C, amplification was performed over 40 cycles, with 30 min at 95°C, 30 min between 52 and 64°C depending on the primers used, and 15 min at 72°C, with a final extension step of 10 min at 72°C. The purified PCR products were directly sequenced with an ABI PRISM AmpliTaq FS, DyeDeoxy-Terminator kit in an ABI PRISM 373A sequencer (Perkin-Elmer, Courtaboeuf, France).
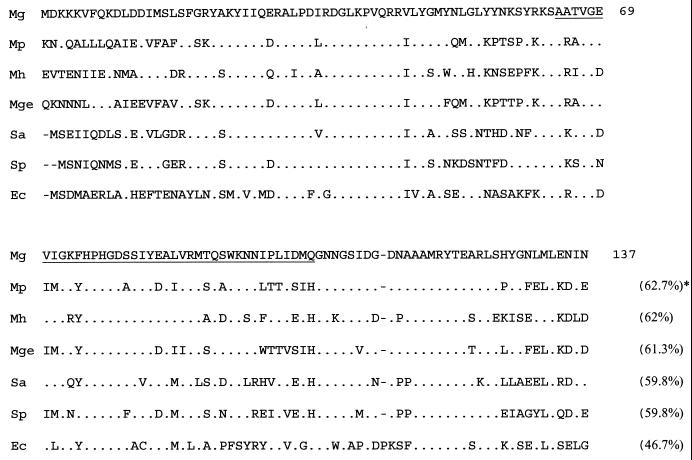
The sequence of the parC QRDR of M. gallisepticum, which had been only partially sequenced beforehand (20), was amplified and characterized. The nucleotide and the peptide sequences of the 413-bp amplified fragments of parC obtained from strains ATCC 15302 and 41-91 presented 96.6 and 100% identity, respectively. As expected, the amino acid sequence exhibited higher homology with the ParC than with the GyrA sequences of other bacteria. The M. gallisepticum ParC QRDR showed a higher identity percentage with the ParC subunits of other mycoplasma species and gram-positive bacteria like Staphylococcus aureus and Streptococcus pneumoniae than with the gram-negative Escherichia coli (Fig. 1).
FIG. 1.
Alignment of the ParC amino acid sequence of M. gallisepticum ATCC 15302 (Mg) with those of Mycoplasma pneumoniae (Mp) (12), M. hominis (Mh) (2), Mycoplasma genitalium (Mge) (1), S. aureus (Sa) (7), S. pneumoniae (Sp) (19), and E. coli (Ec) (11). The numbering used corresponds to that of the E. coli ParC peptide sequence. Symbols: ., identical amino acids; -, gap introduced to maximize similarities; and ∗, identity percentage. The QRDR is underlined.
Twenty-two enrofloxacin-resistant mutants obtained from both strains were characterized for their susceptibility to nine quinolones and for the QRDR status of their gyrA, gyrB, parC, and parE genes (Tables 1 and 2). These mutants exhibited cross-resistance for all quinolones studied. Interestingly, the activity of danofloxacin appeared to be least affected by the presence of numerous mutations. When tested, the mutants were susceptible to nonquinolone antimicrobials, like erythromycin, tetracycline, and chloramphenicol (data not shown). The most resistant mutants presented three mutations, with two of them in GyrA or ParC, or four substitutions in at least three of the four target genes, suggesting that the level of MICs could be correlated with the number of mutations. Thus, the mutant with the highest resistance was mutant ATM5 derived from the reference strain; it harbored four target alterations (Table 1).
TABLE 1.
MICs and mutations observed in ATCC 15302 mutants selected after 10 passages in enrofloxacin
| Strain | MIC (μg/ml)a
|
Mutations in QRDRs ofb:
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GyrA
|
GyrB
|
ParC
|
ParE
|
|||||||||||||||||
| ENR | CIP | OFX | MAR | DAN | DIF | NOR | OA | UB | 81 | 83 | 84 | 87 | 464 | 80 | 84 | 463 | 467 | |||
| Parent | 0.03 | 0.03 | 0.03 | 0.06 | 0.03 | 0.06 | 0.125 | 1 | 1 | Gly | Ser | Ala | Glu | Asn | Ser | Glu | Ser | Cys | ||
| ATM1 | 2 | 0.5-1 | 2 | 1 | 2 | 2 | 4 | 32 | 64 | Gly | Asp | Gly | ||||||||
| ATM2 | 8 | 16 | 16 | 16 | 4 | 16 | 16 | 16 | 32 | Lys | Leu | Phe | ||||||||
| ATM3 | 8 | 16 | 16 | 16 | 4 | 16 | 32 | 16 | 32 | Ala | Arg | Lys | ||||||||
| ATM4 | 8 | 16 | 16 | 16 | 4 | 16 | 32 | 32 | 32 | Arg | Pro | Lys | ||||||||
| ATM5 | 64 | 32 | 64 | 64 | 8 | 32 | 64 | 64 | 64 | Arg | Pro | Leu | Leu | |||||||
ENR, enrofloxacin; CIP, ciprofloxacin; OFX, ofloxacin; MAR, marbofloxacin; DAN, danofloxacin; DIF, difloxacin; NOR, norfloxacin; OA, oxolinic acid; and UB, flumequine.
E. coli numbering.
TABLE 2.
MICs and mutations observed in 41-91 mutants selected after 10 passages in enrofloxacin
| Strain | MIC (μg/ml)a
|
Mutations in QRDRs ofb:
|
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GyrA
|
GyrB
|
ParC
|
ParE
|
||||||||||||||||||
| ENR | CIP | OFX | MAR | DAN | DIF | NOR | OA | UB | 83 | 87 | 426 | 465 | 64 | 80 | 81 | 84 | 420 | 463 | |||
| Parent | 0.06 | 0.03 | 0.06 | 0.06 | 0.06 | 0.125 | 0.25 | 4 | 2 | Ser | Glu | Asp | Glu | Ala | Ser | Ser | Glu | Asp | Ser | ||
| 41M1 | 0.125 | 0.125 | 0.125 | 0.125 | 0.125 | 0.125 | 0.25 | 4 | 8 | Asn | |||||||||||
| 41M2 | 0.25 | 0.5 | 1 | 1 | 0.5 | 0.25 | 4 | 8 | 16 | Asn | Pro | ||||||||||
| 41M3 | 0.5 | 0.25 | 2 | 1 | 0.5 | 0.5 | 2 | 8 | 32 | Asn | Asn | ||||||||||
| 41M4 | 1 | 2 | 1 | 1 | 2 | 2 | 4 | 16 | 32 | Asn | Pro | Leu | |||||||||
| 41M5 | 2 | 0.5 | 2 | 2 | 1 | 1 | 2 | 8 | 16 | Lys | Asn | Asn | |||||||||
| 41M6 | 2 | 1 | 1 | 1 | 2 | 4 | 4 | 16 | 32 | Ile | Asn | Pro | |||||||||
| 41M7 | 2 | 2 | 4 | 2 | 1 | 2 | 4 | 16 | 16 | Ile | Asn | Leu | |||||||||
| 41M8 | 2 | 4 | 8 | 4 | 2 | 4 | 8 | 32 | 32 | Asn | Asn | Gln | Leu | ||||||||
| 41M9 | 8 | 8 | 16 | 16 | 2 | 8 | 4 | 32 | 32 | Arg | Asn | Pro | |||||||||
| 41M10 | 8 | 8 | 8 | 8 | 2 | 4 | 8 | 16 | 16 | Ile | Asn | Ser | Gly | Leu | |||||||
| 41M11 | 16 | 16 | 32 | 32 | 2 | 8 | 32 | 16 | 32 | Ile | Lys | Lys | |||||||||
| 41M12 | 16 | 16 | 16 | 16 | 4 | 4 | 8 | 32 | 16 | Ile | Asn | Gly | Leu | ||||||||
| 41M13 | 16 | 16 | 16 | 16 | 2 | 8 | 16 | 16 | 32 | Lys | Lys | Leu | Asn | ||||||||
| 41M14 | 16 | 16 | 32 | 32 | 4 | 8 | 16 | 16 | 32 | Ile | Asn | Leu | Leu | ||||||||
| 41M15 | 16 | 16 | 32 | 64 | 4 | 8 | 16 | 32 | 32 | Ile | Asn | Trp | Pro | ||||||||
| 41M16 | 32 | 32 | 16 | 32 | 4 | 8 | 32 | 32 | 32 | Arg | Gly | Leu | Asn | ||||||||
| 41M17 | 32 | 32 | 32 | 64 | 4 | 8 | 16 | 32 | 32 | Ile | Asn | Leu | Pro | ||||||||
ENR, enrofloxacin; CIP, ciprofloxacin; OFX, ofloxacin; MAR, marbofloxacin; DAN, danofloxacin; DIF, difloxacin; NOR, norfloxacin; OA, oxolinic acid; and UB, flumequine.
E. coli numbering.
Unlike other mollicutes, such as Mycoplasma hominis (3, 5, 16), Ureaplasma urealyticum (4), and Acholeplasma laidlawii (21), where no GyrB mutation was found, M. gallisepticum mutants exhibited four different alterations in GyrB at positions 426, 464, and 465 (E. coli numbering), previously associated with quinolone resistance in other bacteria (9, 13, 19, 25). Mutations of GyrB at position 426 were likely obtained in the early steps of the process and were then found in all subsequent derivatives, introducing a bias in the frequency of GyrB alterations. However, mutants investigated in this study (Tables 1 and 2) were obtained from three and four independent selection experiments realized with both reference and field strains, respectively, suggesting that the frequency of GyrB mutations is not due only to the selection method. In ParE, the Asp-420→Asn substitution observed was previously described at the corresponding position in M. hominis (5). The two other mutations found in ParE, at positions 463 and 467, have never been described previously.
Eight different mutations were found at four distinct positions, 81, 83, 84, and 87, in the GyrA QRDR of M. gallisepticum (E. coli numbering). These positions have been previously found mutated in quinolone-resistant mutants from other bacteria (3-5, 11, 16, 19, 22-24). In the ParC QRDR, seven amino acid alterations were found at positions 80, 81, and 84 previously altered in other bacteria (3-5, 11, 16, 18, 23). To our knowledge, the Ala-64→Ser substitution found in mutant 41M10 (Table 2) has never been described.
Some mutants exhibited the same mutations but had different MIC profiles of the fluoroquinolones tested (data not shown). Additional mechanisms, like mutations elsewhere in the topoisomerase genes or modifications in drug efflux systems, may contribute to the resistant phenotype of these mutants.
In summary, our results generally showed that the development of mutants with high levels of resistance to quinolones in M. gallisepticum required mutations in both topoisomerases, like for most bacteria (3-5, 11, 13, 16, 22, 23). When available, the study of clinical strains will be helpful in validating these in vitro data. Like M. hominis in humans, M. gallisepticum could be a good model for the study of fluoroquinolone resistance in animal mycoplasmas.
Nucleotide sequence accession number. The nucleotide sequence data reported in this paper will appear in the GenBank nucleotide sequence databases with the accession number AF372652.
Acknowledgments
We thank Thierry Laurent for technical assistance, Claire de Boisséson for useful advice and technical assistance, Hélène Renaudin for useful advice, and Christiane Bébéar for critical reading of the manuscript.
This work was in part supported by the Conseil Général des Côtes d'Armor and by the Conseil Régional de Bretagne.
REFERENCES
- 1.Bailey, C. C., R. Younkins, W. M. Huang, and K. F. Bott. 1996. Characterization of genes encoding topoisomerase IV of Mycoplasma genitalium. Gene 168:77-80. [DOI] [PubMed] [Google Scholar]
- 2.Bébéar, C. M., A. Charron, J. M. Bové, C. Bébéar, and J. Renaudin. 1998. Cloning and nucleotide sequences of the topoisomerase IV parC and parE genes of Mycoplasma hominis. Antimicrob. Agents Chemother. 42:2024-2031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bébéar, C. M., H. Renaudin, A. Charron, J. M. Bové, C. Bébéar, and J. Renaudin. 1998. Alterations in topoisomerase IV and DNA gyrase in quinolone-resistant mutants of Mycoplasma hominis obtained in vitro. Antimicrob. Agents Chemother. 42:2304-2311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bébéar, C. M., H. Renaudin, A. Charron, D. Gruson, M. Lefrançois, and C. Bébéar. 2000. In vitro activity of trovafloxacin compared to those of five antimicrobials against mycoplasmas including Mycoplasma hominis and Ureaplasma urealyticum fluoroquinolone-resistant isolates that have been genetically characterized. Antimicrob. Agents Chemother. 44:2557-2560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bébéar, C. M., J. Renaudin, A. Charron, H. Renaudin, B. de Barbeyrac, T. Schaeverbeke, and C. Bébéar. 1999. Mutations in the gyrA, parC, and parE genes associated with fluoroquinolone resistance in clinical isolates of Mycoplasma hominis. Antimicrob. Agents Chemother. 43:954-956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bébéar, C., and J. A. Robertson. 1996. Determination of minimal inhibitory concentrations, p. 189-197. In J. G. Tully and S. Razin (ed.), Molecular and diagnostic procedures in mycoplasmology, vol. II. Diagnostic procedures. Academic Press, New York, N.Y. [Google Scholar]
- 7.Ferrero, L., B. Cameron, B. Manse, D. Lagneaux, J. Crouzet, A. Famechon, and F. Blanche. 1994. Cloning and primary structure of Staphylococcus aureus DNA topoisomerase IV: a primary target of fluoroquinolones. Mol. Microbiol. 13:641-653. [DOI] [PubMed] [Google Scholar]
- 8.Forsyth, M. H., A. S. Sayed, and S. J. Geary. 1995. Sequence and transcriptional analysis of the genes encoding the class-II topoisomerase of Mycoplasma gallisepticum. Gene 163:161-162. [DOI] [PubMed] [Google Scholar]
- 9.Gensberg, K., Y. F. Jin, and L. V. J. Piddock. 1995. A novel gyrB mutation in a fluoroquinolone-resistant clinical isolate of Salmonella typhimurium. FEMS Microbiol. Lett. 132:57-60. [DOI] [PubMed]
- 10.Hannan, P. C. T., G. D. Windsor, A. de Jong, N. Schmeer, and M. Stegemann. 1997. Comparative susceptibilities of various animal-pathogenic mycoplasmas to fluoroquinolones. Antimicrob. Agents Chemother. 41:2037-2040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heisig, P. 1996. Genetic evidence of a role of parC mutations in development of high-level fluoroquinolone resistance in Escherichia coli. Antimicrob. Agents Chemother. 40:879-885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Himmelreich, R., H. Hilbert, H. Plagens, E. Pirkl, B. C. Li, and R. Herrmann. 1996. Complete sequence analysis of the genome of the bacterium Mycoplasma pneumoniae. Nucleic Acids Res. 24:4420-4449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ito, H., H. Yoshida, M. Bogaki-Shonai, T. Niga, H. Hattori, and S. Nakamura. 1994. Quinolone resistance mutations in the DNA gyrase gyrA and gyrB genes of Staphylococcus aureus. Antimicrob. Agents Chemother. 38:2014-2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jordan, F. T. W., S. Gilbert, D. L. Knight, and C. A. Yavari. 1989. Effects of Baytril, tylosin and tiamulin on avian mycoplasmas. Avian Pathol. 18:659-673. [DOI] [PubMed] [Google Scholar]
- 15.Kempf, I., A. Blanchard, F. Gesbert, M. Guittet, and G. Bennejean. 1993. The polymerase chain reaction for Mycoplasma gallisepticum detection. Avian Pathol. 22:739-750. [DOI] [PubMed] [Google Scholar]
- 16.Kenny, G. E., P. A. Young, F. D. Cartwright, K. E. Sjöstrom, and W. M. Huang. 1999. Sparfloxacin selects gyrase mutations in first-step Mycoplasma hominis mutants, whereas ofloxacin selects topoisomerase IV mutations. Antimicrob. Agents Chemother. 43:2493-2496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ley, D. H., and H. W. Yoder, Jr. 1997. Mycoplasma gallisepticum infection, p. 194-195. In B. W. Calnek (ed.), Diseases of poultry, 10th ed. Iowa State University Press, Ames, Iowa.
- 18.Nakano, M., T. Deguchi, T. Kawamura, M. Yasuda, M. Kimura, Y. Okano, and Y. Kawada. 1997. Mutations in the gyrA and parC genes in fluoroquinolone-resistant clinical isolates of Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 41:2289-2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pan, X. S., and L. M. Fisher. 1998. DNA gyrase and topoisomerase IV are dual targets of clinafloxacin action in Streptococcus pneumoniae. Antimicrob. Agents Chemother. 42:2810-2816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Skamrov, A. V., E. S. Feoktistova, and R. S. Bibilashvili. 1995. Cloning and sequencing of Mycoplasma gallisepticum gene for ATP-binding subunit of DNA topoisomerase type II. Mol. Biol. 29:175-180. [PubMed] [Google Scholar]
- 21.Taganov, K. D., A. E. Gushchin, T. A. Akopian, N. Y. Oparina, N. Y. Abramycheva, and V. M. Govorun. 2000. Analysis of the DNA gyrase genes of Acholeplasma laidlawii PG-8B. Mol. Biol. 34:256-262. [PubMed] [Google Scholar]
- 22.Tankovic, J., F. Mahjoubi, P. Courvalin, J. Duval, and R. Leclercq. 1996. Development of fluoroquinolone resistance in Enterococcus faecalis and role of mutations in the DNA gyrase gyrA gene. Antimicrob. Agents Chemother. 40:2558-2561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang, T., M. Tanaka, and K. Sato. 1998. Detection of grlA and gyrA mutations in 344 Staphylococcus aureus strains. Antimicrob. Agents Chemother. 42:236-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yoshida, H., M. Bogaki, M. Nakamura, and S. Nakamura. 1990. Quinolone resistance-determining region in the DNA gyrase gyrA gene of Escherichia coli. Antimicrob. Agents Chemother. 34:1271-1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yoshida, H., M. Bogaki, M. Nakamura, L. M. Yamanaka, and S. Nakamura. 1991. Quinolone resistance-determining region in the DNA gyrase gyrB gene of Escherichia coli. Antimicrob. Agents Chemother. 35:1647-1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zander, D. V. 1961. Origin of S6 strain Mycoplasma. Avian Dis. 5:154-156. [Google Scholar]