Abstract
Rifampin-resistant mutants were selected from UV-light-treated Bacillus cereus (20 mutants) and attenuated B. anthracis (23 mutants). In addition, spontaneous rifampin-resistant mutants were also isolated in attenuated B. anthracis (22 mutants). The rifampin resistance clusters of the rpoB gene were sequenced for all 65 mutants. Mutations associated with resistance were consistent with those from other bacteria, though two novel changes were observed. The spontaneous rate of resistance was estimated at 1.57 × 10−9 mutations/generation by a Luria-Delbrück fluctuation test.
Rifampin (RIF) is a bactericidal antibiotic effective against a wide variety of bacteria. RIF kills bacteria by binding to RNA polymerase and blocking the elongation of the RNA transcript when it becomes 2 or 3 nucleotides in length. Unfortunately, bacteria develop resistance to RIF at a high frequency (2). RIF-resistant (RIF-R) mutants have been characterized for many pathogenic species, including Escherichia coli (7), Mycobacterium tuberculosis (5), Staphylococcus aureus (1), Helicobacter pylori (4), and members of the Legionellaceae (10). RIF resistance is commonly due to mutations in the beta subunit of RNA polymerase, encoded by the rpoB gene. Mutations conferring RIF resistance have been identified in four clusters known as the N-terminal cluster and clusters I, II, and III, with the majority of mutations occurring in cluster I (2). In the present study, RIF-R mutants of Bacillus cereus (ATCC 14579) and an attenuated Bacillus anthracis strain (Ames: pXO1-, pXO2-) were selected and the RIF-R clusters of the rpoB gene were sequenced.
Independent UV-induced RIF-R mutants of both B. cereus and B. anthracis and spontaneous RIF-R mutants of B. anthracis were isolated on selective media. UV-induced RIF-R mutants were obtained by exposing 10 ml of an exponentially growing culture of either Bacillus species to 28,800 μJ of UV light in a UV Stratalinker (Stratagene). Fifteen 500-μl aliquots were taken from each of several 10-ml cultures and incubated overnight. A 100-μl aliquot from each of these cultures was spread onto plates containing RIF (150 μg/ml) and incubated for 48 h. Only a single RIF-R colony from each aliquot was picked to ensure independent mutational events. A simplified heat-soak DNA extraction was performed as previously described (8). Likewise, spontaneous B. anthracis mutants were generated by plating 500-μl aliquots from 100 independent 5-ml B. anthracis cultures in exponential growth onto plates containing RIF (50 μg/ml) and incubated for 48 h. Following colony purification, RIF-R colonies were streaked onto plates containing a higher RIF concentration (150 μg/ml) and grown overnight. Heat-soak DNA extractions were then performed. All cultures were grown at 37°C in Luria-Bertani broth unless otherwise indicated.
MICs for the RIF-R mutants were obtained using a combination of plating and E-test (AB BIODISK) methods (Table 1). The plating method was used on all of the RIF-R mutants by spotting RIF-R Bacillus Mueller-Hinton (MH) broth cultures in exponential growth onto MH plates containing various concentrations of RIF (200 to 1,600 μg/ml), incubating overnight, and checking for growth. The E-test method was used on all of the B. anthracis RIF-R mutants by inoculating 3 ml of MH broth with a RIF-R colony, incubating the culture at 37°C for ≥5 h, and then adjusting the culture turbidity to 1 McFarland as outlined in the E-test instructions. MH blood agar plates were streaked for lawns and the RIF E-test was performed according to kit instructions.
TABLE 1.
B. anthracis and B. cereus RIF-R mutants and their MICs
| Mutanta | Position and amino acid Substitution | MIC (μg/ml) of RIF |
|---|---|---|
| B. anthracis | ||
| wt | 0.016 | |
| UVM1 | 472 Ser(TCT)→Phe(TTT) | 400–500 |
| UVM2 | 468 Lys(AAA)→Gln(CAA) | 400–500 |
| UVM3 | 459 Thr(ACA)→Ser(TCA) | 400–500 |
| UVM4 | 467 His(CAC)→Tyr(TAC) | 800–1,000 |
| UVM5 | 450 Ser(TCT)→Cys(TGT) | 400–500 |
| UVM6 | 453 Ser(TCT)→Cys(TGT) | 400–500 |
| UVM7 | 450 Ser(TCT)→Phe(TTT) | 400–1,000 |
| UVM8 | 454 Gln(CAG)→Arg(CGG) | 800–1,000 |
| UVM9 | 467 His(CAC)→Arg(CGC) | 400–1,000 |
| SM1 | 454 Gln(CAG)→Lys(AAG) | 264–500 |
| SM2 | 454 Gln(CAG)→Arg(CGG) | 500–1,000 |
| SM3 | 467 His(CAC)→Tyr(TAC) | 500–1,000 |
| SM4 | 467 His(CAC)→Arg(CGC) | 500–1,000 |
| SM5 | 472 Ser(TCT)→Phe(TTT) | 264–500 |
| B. cereus | ||
| wt | 0.5 | |
| UVM1 | 453–455 SerGlnPhe deletion | 800 |
| UVM2 | 467 His(CAT)→Leu(CTT) | 800 |
| UVM3 | 454 Gln(CAG)→Arg(CGG) | 800 |
| UVM4 | 467 His(CAT)→Arg(CGT) | 400 |
| UVM5 | 472 Ser(TCT)→Phe(TTT) | 400 |
| UVM6 | 454 Gln(CAG)→Arg(CGG) & 457 Asp(GAC)→Ala(GCC) | 800 |
| UVM7 | 467 His(CAT)→Pro(CCT) | 800 |
UVM designates UV-induced mutants, and SM designates spontaneous mutants.
Sequences were determined for clusters I, II, and III of wild-type (wt) B. cereus and B. anthracis, 20 UV-generated B. cereus RIF-R mutants, 23 UV-generated B. anthracis RIF-R mutants, and 22 spontaneous RIF-R B. anthracis mutants. The primers used for PCR amplification and sequencing were RIF-F1 (5′ CGTGAGAGAATGTCGATCC) and RIF-R1 (5′ CGCGAACGAAGATAATGA) for amplifying the cluster I region and RIF-F2 (5′ GCATTAGGACCTGGTGGT) and RIF-R2 (5′ GCTGATACGTACTCCATACCT) for amplifying the cluster II and III regions. Alignment of sequences (using MegAlign software; DNASTAR) found all RIF resistance-associated mutations within the cluster I region of the rpoB gene (Table 1). There were no mutations in the other two clusters.
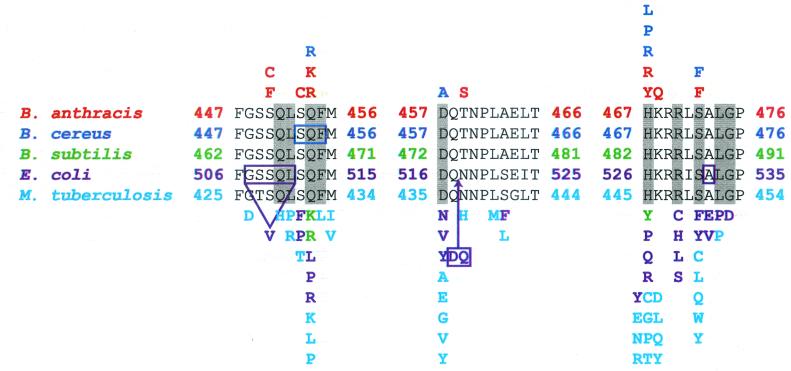
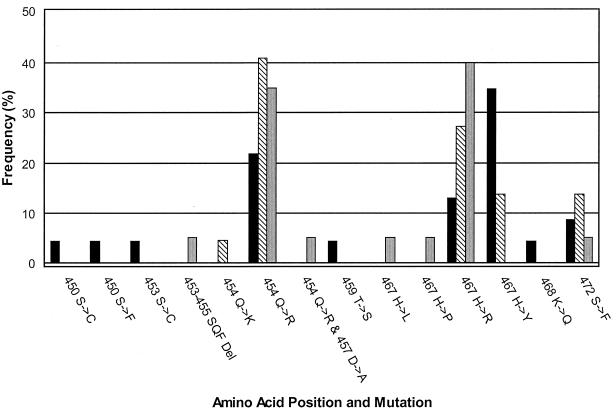
Most of the mutations identified in this study correspond to known RIF resistance mutations in Bacillus subtilis (6), E. coli, and M. tuberculosis (2). Amino acid substitutions that do not directly correspond to these known mutations still occur at the same positions (Fig. 1). Twelve amino acid positions are known to interact directly with RIF (2); mutations were observed at four of these positions in either B. anthracis or B. cereus (Fig. 1). The remaining four amino acid positions at which mutations are observed in B. anthracis and B. cereus surround the RIF binding pocket (2). Two of these changes (positions 450 and 468) are unique to B. anthracis, while deletion at positions 453 to 455 is unique to B. cereus (Fig. 1). All of the substitutions conferring RIF resistance involve replacement by an amino acid with a differently sized side chain, which may alter the RIF binding pocket and prevent RIF from binding (2). The majority of mutations observed in this study occurred at positions 454 and 467 (Fig. 2). Both of these positions interact directly with two of the four critical hydroxyl groups of RIF (2).
FIG. 1.
RIF resistance mutations in the rpoB cluster I. Mutations from B. subtilis (7), E. coli, and M. tuberculosis (2) have been previously reported. Amino acid substitutions occurring in B. anthracis (red), B. cereus (blue), B. subtilis (green), E. coli (purple), and M. tuberculosis (light blue) are indicated. Deletions conferring RIF resistance are boxed and connected by a line to any change in amino acids (e.g., V in E. coli). A large arrow indicates one insertion (DQ) conferring RIF resistance found in E. coli. Ten of the twelve amino acid positions that interact directly with RIF are shaded in gray (2).
FIG. 2.
RIF resistance mutation frequency. The frequency data for UV-generated RIF-R B. anthracis mutants (black bars), spontaneous RIF-R B. anthracis mutants (striped bars), and UV-generated RIF-R B. cereus mutants (gray bars) are shown.
There is greater diversity among UV-generated RIF-R B. anthracis mutants than among spontaneously occurring mutants. In fact, all but one of the spontaneous RIF-R B. anthracis mutants are identical to UV-generated B. anthracis mutants (Table 1; Fig. 2). This is likely due to the mutagenic effects of UV light. In support of this idea, all of the unique mutations conferring RIF resistance in these two species occurred in UV-generated mutants as opposed to spontaneous mutants (Table 1; Fig. 1).
Interestingly, while the most commonly occurring B. cereus RIF-R mutants parallel RIF-R B. anthracis mutants, many of the remaining RIF-R B. cereus mutants (all UV induced) did not occur in B. anthracis. Likewise, there are a number of infrequent mutations conferring RIF resistance in B. anthracis that are not found in B. cereus (Fig. 2). This could simply be a factor of a small sample size or may indicate a fundamental difference between RIF resistance mutations that occur in these two species or in the repair mechanisms used by these two species.
A Luria-Delbrück fluctuation test (9) was performed and used to determine the spontaneous mutation rate of RIF resistance in B. anthracis. Ninety-six independent 1-ml cultures of wt B. anthracis were grown overnight with heavy shaking in 24-well plates (Costar). Six randomly chosen cultures were used to determine an average total number of cells/culture of 1.23 × 109 by reading the optical density at 625 nm and using the equation y = (108)(x) + 3 × 106, where y is equal to the number of cells per milliliter and x is equal to the optical density at 625 nm. This equation was previously determined by comparing optical densities and direct cell counts for a number of B. anthracis growth curves.
The remaining 90 cultures were transferred to sterile 1.5-ml microcentrifuge tubes and centrifuged at 3,000 × g for 5 min; ≥850 μl of the supernatant was removed, and the pellet was resuspended and spread onto MH plates containing RIF (50 μg/ml). Thirteen plates contained growth after 48 h, yielding a mutation rate of 1.57 × 10−9 RIF-R mutants per generation. This mutation rate is somewhat higher than the estimated point mutation rate of 6 × 10−10 per generation for E. coli (3). However, the RIF resistance mutation rate estimated here is a composite rate from three distinct positions (Fig. 2), which would then correspond to individual rates of 7.14 × 10−10 (n = 454), 6.42 × 10−10 (n = 467), and 2.14 × 10−10 (n = 472) per generation.
The mechanisms behind RIF resistance in B. anthracis and B. cereus are similar to mechanisms found in other species, although we have found unique mutations conferring RIF resistance in both of these species. This documentation of mutational changes associated with RIF-R mutants and mutation rates will lead to better detection and diagnostics for clinical situations where RIF is used.
Acknowledgments
This work was supported by grants from the U.S. Department of Energy CBNP program, the National Institutes of Health (R01 GM60795), and the NAU Cowden Endowment for Microbiology.
REFERENCES
- 1.Aubry-Damon, H., C. Soussy, and P. Courvalin. 1998. Characterization of mutations in the rpoB gene that confer rifampin resistance in Staphylococcus aureus. Antimicrob. Agents Chemother. 42:2590–2594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campbell, E. A., N. Korzheva, A. Mustaev, K. Murakami, S. Nair, A. Goldfarb, and S. A. Darst. 2001. Structural mechanism for rifampicin inhibition of bacterial RNA Polymerase. Cell 104:901–912. [DOI] [PubMed] [Google Scholar]
- 3.Drake, J. W. 1991. A constant rate of spontaneous mutation in DNA-based microbes. Proc. Natl. Acad. Sci. USA 88:7160–7164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heep, M., S. Odenbreit, D. Beck, J. Decker, E. Prohaska, U. Rieger, and N. Lehn. 2000. Mutations at four distinct regions of the rpoB gene can reduce the susceptibility of Helicobacter pylori to rifamycins. Antimicrob. Agents Chemother. 44:1713–1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heep, M., B. Brandstätter, U. Rieger, N. Lehn, E. Richter, S. Rüsch-Gerdes, and S. Niemann. 2001. Frequency of rpoB mutations inside and outside the cluster I region in rifampin-resistant clinical Mycobacterium tuberculosis isolates. J. Clin. Microbiol. 39:107–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ingham, C. J., and P. A. Furneaux. 2000. Mutations in the β subunit of the Bacillus subtilis RNA polymerase that confer both rifampicin resistance and hypersensitivity to NusG. Microbiology 146:3041–3049. [DOI] [PubMed] [Google Scholar]
- 7.Jin, D. J., and C. A. Gross. 1988. Mapping and sequencing of mutations in the Escherichia coli rpoB gene that lead to rifampicin resistance. J. Mol. Biol. 202:45–58. [DOI] [PubMed] [Google Scholar]
- 8.Keim, P., L. B. Price, A. M. Klevytska, K. L. Smith, J. M. Schupp, R. Okinaka, P. J. Jackson, and M. E. Hugh-Jones. 2000. Multiple-locus variable-number tandem repeat analysis reveals genetic relationships within Bacillus anthracis. J. Bacteriol. 182:2928–2936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luria, S. E., and M. Delbrück. 1943. Mutations of bacteria from virus sensitivity to virus resistance. Genetics 28:491–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nielsen, K., P. Hindersson, N. Høiby, and J. M. Bangsborg. 2000. Sequencing of the rpoB gene in Legionella pneumophila and characterization of mutations associated with rifampin resistance in the Legionellaceae. Antimicrob. Agents Chemother. 44:2679–2683. [DOI] [PMC free article] [PubMed] [Google Scholar]