Abstract
Nineteen of 27 ceftazidime-resistant Enterobacter cloacae isolates from a neonatal intensive care unit in Thessaloniki, Greece, had genes coding for the novel extended-spectrum β-lactamase IBC-1; 18 of those 19 harbored similar conjugative plasmids and belonged to two distinct genetic lineages. A synergy test with ceftazidime and imipenem enabled us to identify five unrelated blaIBC-1-carrying E. cloacae isolates from other wards of the hospital. It seems that this integron-associated gene is capable of dispersing both by clonal spread and by gene dissemination.
Strains of Enterobacter cloacae resistant to expanded-spectrum cephalosporins have been implicated in outbreaks of serious infections in neonatal intensive care units (NICUs) (2, 4, 11, 14). In this species stable derepression of the chromosomal Ampler class C β-lactamase is the major cause of resistance to the above drugs (12, 13, 18). However, production of class A extended-spectrum β-lactamases (ESBLs) has also been detected in enterobacters, but their prevalence is generally very low (1, 5, 13). Recently, a novel integron-associated class A β-lactamase with extended-spectrum properties, designated IBC-1, has been described for an E. cloacae clinical strain in Greece (3).
Preliminary susceptibility data in our hospital indicated that several infections among preterm neonates in our NICU were due to ceftazidime-resistant E. cloacae that usually exhibited cross-resistance to other unrelated antimicrobials. The similar antimicrobial susceptibility patterns of these isolates prompted an investigation to determine whether a limited spread of a single strain existed and also to study the mechanism(s) of resistance to newer β-lactam antibiotics.
During the study period (August 1998 to June 2000), 27 nonrepetitive E. cloacae isolates were consecutively collected from clinical specimens of separate premature neonates in the NICU of Hippokration General Hospital. Ceftazidime-resistant nonrepetitive E. cloacae isolates that were recovered from separate patients in various other departments of the hospital were also included in the study. Species identification was done by using the Vitek automated identification system (bioMerieux, Marcy l'Etoile, France) and was confirmed with the ATB-GN system (bioMerieux).
Susceptibilities of the isolates to antibiotics were determined by an agar dilution technique (9). The antibiotics used are shown in Table 1. The isolates were screened for the presence of IBC-like ESBLs by placing a disk of ceftazidime (30 μg) at distances of 15 mm (edge to edge) from disks containing imipenem (30 μg), amoxicillin plus clavulanate (20 and 10 μg, respectively), and piperacillin plus tazobactam (75 and 10 μg, respectively). Any enhancement of the zone of inhibition between the ceftazidime disk and that containing any β-lactamase inhibitor was interpreted as presumptive evidence for the presence of an ESBL (1, 7).
TABLE 1.
Antibiotic susceptibilities of the 27 E. cloacae isolates recovered in the NICU
| Antibiotic | MIC (μg/ml)
|
No. of resistant isolatesc | |||
|---|---|---|---|---|---|
| Definition of resistance | Range | MIC50d | MIC90e | ||
| Amoxicillin-clavulanatea | >8 | >32 | >32 | >32 | 27 |
| Piperacillin | >64 | 128->128 | 128 | >128 | 27 |
| Piperacillin-tazobactamb | >64 | 32->128 | 128 | >128 | 20 |
| Cefoxitin | >16 | >32 | >32 | >32 | 27 |
| Ceftazidime | >16 | >32 | >32 | >32 | 27 |
| Cefotaxime | >32 | 4->64 | 16 | >32 | 9 |
| Ceftriaxone | >32 | 4->64 | 16 | >32 | 10 |
| Aztreonam | >16 | 8->32 | 16 | >32 | 11 |
| Imipenem | >8 | ≤0.5-2 | 0.5 | 1 | 0 |
| Gentamicin | >4 | ≤0.5-32 | 1 | 4 | 2 |
| Tobramycin | >4 | ≤0.5-32 | 16 | 32 | 23 |
| Netilmicin | >16 | ≤0.5->64 | 32 | >64 | 23 |
| Amikacin | >16 | ≤0.5->64 | 32 | 64 | 23 |
| Tetracycline | >8 | 1->64 | >64 | >64 | 26 |
| Trimethoprim | >8 | ≤0.5->64 | >64 | >64 | 26 |
| Sulfamethoxazole | >256 | >512 | >512 | >512 | 27 |
Amoxicillin component of an amoxicillin-clavulanate 2:1 ratio test.
Piperacillin component tested with a fixed concentration of 4 μg of tazobactam per ml.
Resistance rates were defined according to the NCCLS interpretative criteria (9).
MIC at which 50% of the isolates tested are inhibited.
MIC at which 90% of the isolates tested are inhibited.
Pulsed-field gel electrophoresis (PFGE) of XbaI-digested genomic DNA was performed (6), and banding patterns of the strains were compared visually by following the criteria of Tenover et al. (15). In order to investigate the presence of blaIBC-1, a 400-bp internal fragment of the gene was amplified with the primers 5′-TGCATCGGAAAAATTAACCT-3′ (forward) and 5′-AATTTTACGAAAATACTGCG-3′ (reverse), corresponding to the segment 51-450 of the published sequence (3). The conditions were an initial denaturation at 94°C for 5 min; 30 cycles of amplification at 94°C for 25 s, 54°C for 40 s, and 72°C for 50 s; and a final extension at 72°C for 6 min. E. cloacae HT9 (3) was used as a positive control in all PCR experiments.
Conjugal experiments were performed as described previously (17). blaIBC-1-bearing strains and transconjugants were analyzed for plasmids by an alkaline lysis procedure (10). For restriction endonuclease analysis, extracted plasmids were digested with 10 U of EcoRI. Isoelectric focusing (IEF) of β-lactamases was performed in polyacrylamide gels containing ampholytes (Pharmacia-LKB) covering a pH range from 3.5 to 9.5 (8).
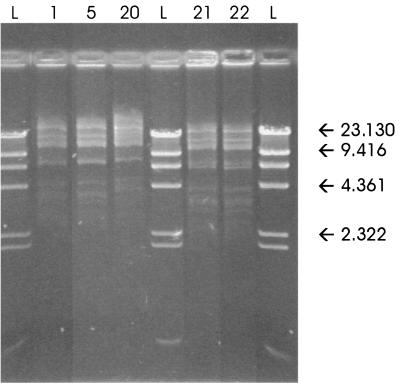
The susceptibilities of the enterobacters that were recovered in the NICU during the study period are presented in Table 1. All 27 E. cloacae isolates were resistant to ceftazidime (MIC > 32 μg/ml) while for most of them (16 out of 27) the MICs of cefotaxime, ceftriaxone, and aztreonam were ≤16 μg/ml, indicative of nonoverproduced chromosomal cephalosporinase. By PFGE analysis two major clonal types were detected, including 12 and 6 isolates (PFGE types I and II, respectively) (Table 2). The remaining isolates belonged to distinct PFGE types that contained one or two isolates. Ceftazidime resistance was transferred at frequencies varying from 3.7 × 10−3 to 6.8 × 10−4 per donor cell by all 18 isolates that belonged to PFGE types I and II; the remaining enterobacters did not transfer ceftazidime resistance. MIC tests confirmed the transfer of resistance to ceftazidime, piperacillin, amikacin, netilmicin, tobramycin, tetracycline, trimethoprim, and sulfamethoxazole in all cases. Plasmids of approximately 85 kb were visualized in all transconjugants that exhibited a high degree of similarity on the basis of their restriction enzyme digestion profiles (Fig. 1).
TABLE 2.
Characteristics of blaIBC-1-carrying isolates
| Isolate (PFGE type) | Ward | Date of isolation (mo/day/yr) | Site of isolation | Resistance pattern of clinical isolatesa, b | Transferable resistance |
|---|---|---|---|---|---|
| (I) | NICU | 9/7/98 | Conjunctiva | PTZ, CAZ, CTX, CRO, ATM, TOB, NET, AMK, TMP | + |
| 2 (II) | NICU | 10/18/98 | Bronchial tube | CAZ, CTX, CRO, ATM, TOB, NET, AMK, TMP | + |
| 3 (IV) | Surgery 5 | 1/21/99 | Intravascular catheter | PTZ, CAZ, CTX, CRO, ATM, TOB, NET, AMK, TMP | − |
| 4 (II) | NICU | 2/19/99 | Conjunctiva | CAZ, TOB, NET, AMK, TMP | + |
| 5 (II) | NICU | 2/20/99 | Pus | CAZ, TOB, NET, AMK, TMP | + |
| 6 (II) | NICU | 3/8/99 | Blood | PTZ, CAZ, TOB, NET, AMK, TMP | + |
| 7 (II) | NICU | 3/19/99 | Blood | PTZ, CAZ, TOB, NET, AMK, TMP | + |
| 8 (I) | NICU | 5/17/99 | Blood | CAZ, CTX, CRO, ATM, TOB, NET, AMK, TMP | + |
| 9 (I) | NICU | 6/18/99 | Bronchial tube | PTZ, CAZ, TOB, NET, AMK, TMP | + |
| 10 (I) | NICU | 6/20/99 | Bronchial tube | CAZ, TOB, NET, AMK, TMP | + |
| 11 (I) | NICU | 6/27/99 | Blood | PTZ, CAZ, TOB, NET, AMK, TMP | + |
| 12 (I) | NICU | 6/28/99 | Blood | PTZ, CAZ, TOB, NET, AMK, TMP | + |
| 13 (II) | NICU | 6/30/99 | Conjunctiva | PTZ, CAZ, TOB, NET, AMK, TMP | + |
| 14 (I) | NICU | 7/17/99 | Conjunctiva | CAZ, TOB, NET, AMK, TMP | + |
| 15 (III) | NICU | 7/25/99 | Blood | PTZ, CAZ, TMP | − |
| 16 (I) | NICU | 7/26/99 | Blood | PTZ, CAZ, TOB, NET, AMK, TMP | + |
| 17 (I) | NICU | 7/29/99 | Blood | PTZ, CAZ, TOB, NET, AMK, TMP | + |
| 18 (I) | NICU | 8/2/99 | Blood | PTZ, CAZ, ATM, TOB, NET, AMK, TMP | + |
| 19 (I) | NICU | 8/18/99 | Blood | PTZ, CAZ, CTX, CRO, ATM, TOB, NET, AMK, TMP | + |
| 20 (V) | Medicine 2 | 11/15/99 | Blood | PTZ, CAZ, CTX, TOB, NET, AMK, TMP | + |
| 21 (VI) | Pediatric ICU | 1/14/00 | Blood | CAZ, TOB, NET, AMK, TMP | + |
| 22 (VII) | Pediatric ICU | 1/27/00 | Blood | CAZ, TOB, NET, AMK, TMP | + |
| 23 (I) | NICU | 3/20/00 | Bronchial tube | PTZ, CAZ, ATM, TOB, NET, AMK, TMP | + |
| 24 (VIII) | Surgery 2 | 4/25/00 | Wound | CAZ, ATM | − |
All isolates were resistant to amoxicillin-clavulanate, piperacillin, cefoxitin, sulfamethoxazole, and tetracycline.
Abbreviations: AMK, amikacin; ATM, aztreonam; CAZ, ceftazidime; CRO, ceftriaxone; CTX, cefotaxime; NET, netilmicin; PTZ, piperacillin-tazobactam; TMP, trimethoprim; TOB, tobramycin.
FIG. 1.
EcoRI restriction digest profiles of five 85-kb plasmids carried by ceftazidime-resistant transconjugants derived from different E. cloacae isolates. The origins of the corresponding clinical isolates are shown in Table 2. Lanes L, HindIII digest of lambda phage.
IEF testing showed production of a β-lactamase with an apparent isoelectric point of 6.9 that corresponded to IBC-1 β-lactamase in all transconjugants. This β-lactamase was also visualized in their donors as well as in a ceftazidime-resistant nontransferable E. cloacae isolate that belonged to a separate clonal type (PFGE type III). The gene blaIBC-1 was amplified in PFGE type I and II enterobacters and their respective transconjugants as well as in the PFGE type III isolate. No blaIBC-1-specific fragment was detected in the remaining enterobacters.
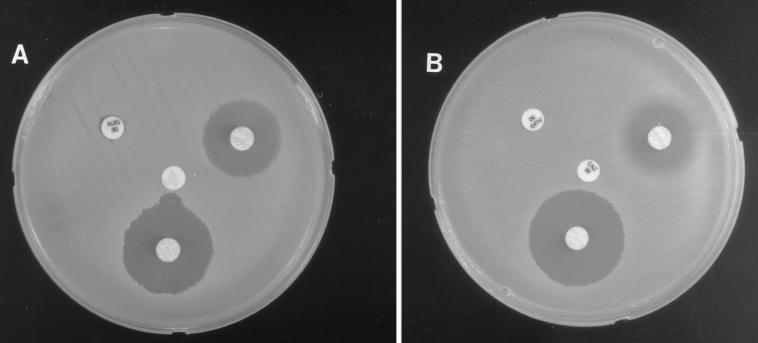
Synergy tests were used in order to evaluate their efficacy in the detection of blaIBC-1-containing isolates. The test with ceftazidime and imipenem was repeatedly positive for 16 of the blaIBC-1-positive isolates, while in the remaining three cases the test gave enhanced inhibition zones that were not always easy to read; it was negative for the remaining ceftazidime-resistant enterobacters. Synergy tests with ceftazidime and amoxicillin-clavulanate or piperacillin-tazobactam were negative for all E. cloacae isolates (Fig. 2).
FIG. 2.
Synergy tests for representative E. cloacae isolates producing IBC-1 enzyme (A) and not producing the enzyme (B). Drug abbreviations on disks: AUG (top left), amoxicillin-clavulanate; IPM (bottom), imipenem; CAZ (center), ceftazidime; TZP (top right), piperacillin-tazobactam. The numbers on the disks are the amounts of drug (in micrograms).
The synergy test with ceftazidime and imipenem was also used in order to detect E. cloacae isolates that express the IBC-1 β-lactamase possibly present in other departments of the hospital. During the study period 34 ceftazidime-resistant enterobacters were recovered from separate patients in various other departments. Five E. cloacae isolates derived from four different wards were positive in the synergy test, and PCR and IEF testing confirmed the presence of IBC-1. Their resistance patterns are presented in Table 2. All had macrorestriction patterns distinct from those of one another and from those of isolates recovered in the NICU (PFGE types IV to VIII) (Table 2). Ceftazidime resistance was transferable from three isolates. Their transconjugants exhibited the same resistance profile, and each had one plasmid of the same size (approximately 85 kb) as, and exhibited restriction enzyme profiles similar to, those derived from enterobacters in the NICU.
Genetic analysis of the E. cloacae isolates showed that two clones persisted in the NICU during the study period, harboring similar conjugative plasmids that coded for the novel integron-associated ESBL IBC-1. It is of interest that, although the two major E. cloacae clones persisted in the NICU for at least 20 months, these strains were not detected outside this unit, at least among IBC-1-expressing E. cloacae isolates. Potential reservoirs such as environmental sources were not identified in this study (data not shown). The fact that two E. cloacae clones containing the blaIBC-1 gene cassettes have been spread in the hospital setting of the NICU might imply that the neonate's gastrointestinal tract became colonized and the transmission occurred via the hands of the medical or nursing staff. However, it is possible that other factors such as overcrowding in the unit and contamination of multidose vials with E. cloacae may have contributed to the dissemination of the outbreak strains. After the first episodes of ceftazidime-resistant E. cloacae infections guidelines for control of fomites and cross-contamination were devised. Thus, all equipment used to care for the patients was decontaminated, and the staff engaged in therapy used disposable gloves and gowns. Indeed, in the NICU there was only one episode of IBC-1-bearing E. cloacae from August 1999 through June 2000.
IBC-1 is inhibited more by imipenem and less by β-lactamase inhibitors such as clavulanate and tazobactam (3). The synergy test with ceftazidime and imipenem enabled us to identify ceftazidime-resistant isolates that carried the blaIBC-1 gene from other departments of the hospital. In this study, the disks in the synergy test were placed at distances of 15 mm (edge to edge) in order to more precisely recognize ESBLs in derepressed variants of enterobacters (1, 16). It has yet to be determined whether the application of the synergy test could also contribute to the identification of clinical isolates of other gram-negative bacteria producing IBC-like β-lactamases.
Acknowledgments
We thank L. S. Tzouvelekis for stimulating discussions and revision of the manuscript.
REFERENCES
- 1.Coudron, P. E., E. S. Moland, and C. C. Sanders. 1997. Occurrence and detection of extended-spectrum β-lactamases in members of the family Enterobacteriaceae at a veterans medical center: seek and you may find. J. Clin. Microbiol. 35:2593-2597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Finnstrom, O., B. Isaksson, S. Haeggman, and L. G. Burman. 1998. Control of an outbreak of a highly β-lactam-resistant Enterobacter cloacae strain in a neonatal special care unit. Acta Paediatr. 87:1070-1074. [DOI] [PubMed] [Google Scholar]
- 3.Giakkoupi, P., L. S. Tzouvelekis, A. Tsakris, V. Loukova, D. Sofianou, and E. Tzelepi. 2000. IBC-1, a novel integron-associated class A β-lactamase with extended-spectrum properties produced by an Enterobacter cloacae clinical strain. Antimicrob. Agents Chemother. 44:2247-2253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hervas, J. A., F. Ballesteros, A. Alomar, J. Gil, V. J. Benedi, and S. Alberti. 2001. Increase of Enterobacter in neonatal sepsis: a twenty-two-year study. Pediatr. Infect. Dis. J. 20:134-140. [DOI] [PubMed] [Google Scholar]
- 5.Hibbert-Rogers, L. C. F., J. Heritage, D. M. Gascoyne-Binzi, P. M. Hawkey, N. Todd, I. J. Lewis, and C. Bailey. 1995. Molecular epidemiology of ceftazidime resistant Enterobacteriaceae from patients on a paediatric oncology ward. J. Antimicrob. Chemother. 36:65-82. [DOI] [PubMed] [Google Scholar]
- 6.Jalaluddin, S., J.-M. Devaster, R. Scheen, M. Gerard, and J.-P. Butzler. 1998. Molecular epidemiological study of nosocomial Enterobacter aerogenes isolates in a Belgian hospital. J. Clin. Microbiol. 36:1846-1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jarlier, V., M. H. Nicolas, G. Fournier, and A. Philippon. 1988. Extended-broad spectrum β-lactamases conferring transferable resistance to newer β-lactam agents in Enterobacteriaceae: hospital prevalence and susceptibility patterns. Rev. Infect. Dis. 10:867-878. [DOI] [PubMed] [Google Scholar]
- 8.Matthew, M., A. M. Harris, M. J. Marshall, and G. W. Ross. 1975. The use of analytical isoelectric focusing for detection and identification of β-lactamases. J. Gen. Microbiol. 88:169-178. [DOI] [PubMed] [Google Scholar]
- 9.National Committee for Clinical Laboratory Standards. 1997. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically, 4th ed. Approved standard M7-A4. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 10.Olsen, J. E. 1990. An improved method for rapid isolation of plasmid DNA from wild-type gram-negative bacteria for plasmid restriction profile analysis. Lett. Appl. Microbiol. 10:209-212. [DOI] [PubMed] [Google Scholar]
- 11.Peters, S. M., J. Bryan, and M. F. Cole. 2000. Enterobacterial repetitive intergenic consensus polymerase chain reaction typing of isolates of Enterobacter cloacae from an outbreak of infection in a neonatal intensive care unit. Am. J. Infect. Control 28:123-129. [PubMed] [Google Scholar]
- 12.Pfaller, M. A., R. N. Jones, S. A. Marshall, S. L. Coffman, R. J. Hollis, M. B. Edmond, and R. P. Wenzel. 1997. Inducible ampC β-lactamase producing gram-negative bacilli from blood stream infections: frequency, antimicrobial susceptibility, and molecular epidemiology in a national surveillance program (SCOPE). Diagn. Microbiol. Infect. Dis. 28:211-219. [DOI] [PubMed] [Google Scholar]
- 13.Sanders, W. E., Jr., and C. C. Sanders. 1997. Enterobacter spp.: pathogens poised to flourish at the turn of the century. Clin. Microbiol. Rev. 10:220-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shi, Z. Y., P. Y. Liu, Y. J. Lau, Y. H. Lin, and B. S. Hu. 1996. Epidemiological typing of isolates from an outbreak of infection with multidrug-resistant Enterobacter cloacae by repetitive extragenic palindromic unit b1-primed PCR and pulsed-field gel electrophoresis. J. Clin. Microbiol. 34:2784-2790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tenover, F. C., R. D. Arbeit, R. V. Goering, P. A. Mickelsen, B. E. Murray, D. H. Persing, and B. Swaminathan. 1995. Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J. Clin. Microbiol. 33:2233-2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tenover, F. C., M. J. Mohammed, T. S. Gorton, and Z. F. Dembek. 1999. Detection and reporting of organisms producing extended-spectrum β-lactamases: survey of laboratories in Connecticut. J. Clin. Microbiol. 37:4065-4070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tsakris, A., A. P. Johnson, R. C. George, S. Mehtar, and A. C. Vatopoulos. 1991. Distribution and transferability of plasmids encoding trimethoprim resistance in urinary pathogens from Greece. J. Med. Microbiol. 34:153-157. [DOI] [PubMed] [Google Scholar]
- 18.Tzelepi, E., L. S. Tzouvelekis, A. C. Vatopoulos, A. F. Mentis, A. Tsakris, and N. J. Legakis. 1992. High prevalence of stably derepressed class-I β-lactamase expression in multiresistant clinical isolates of Enterobacter cloacae from Greek hospitals. J. Med. Microbiol. 37:91-95. [DOI] [PubMed] [Google Scholar]