Abstract
Streptococcus pyogenes BM4478 and Staphylococcus aureus BM4479 were isolated from a patient undergoing rifampin therapy. High-level resistance to rifampin was due to the following mutations in the rpoB gene: Ser522Leu in strain BM4478 and His526Asn and Ser574Leu in strain BM4479.
Streptococcus pyogenes is responsible for high rates of morbidity due to an increase in invasive group A streptococcal infections and bacteremia worldwide, with the most commonly reported predisposing factor being skin lesions (R. C. George, A. Efstratiou, M. A. Monnickendam, M. B. Mcevoy, G. Hallas, A. P. Johnson, and A. Tanna, Abstr. 39th Intersci. Conf. Antimicrob. Agents Chemother., abstr. 309, p. 658, 1999). S. pyogenes is also the leading cause of bacterial pharyngotonsillitis. An increase in macrolide resistance in this species (E. L. Kaplan, D. R. Johnson, and C. D. Rothermel, Abstr. 39th Intersci. Conf. Antimicrob. Agents Chemother., abstr. 535, p. 714, 1999) and the reduced efficacy of oral penicillin V in its eradication from upper respiratory tracts in children have led to the proposal of penicillin being used in combination with rifampin (9).
The mechanisms involved in rifampin resistance in S. pyogenes have not been investigated. In gram-positive bacteria, resistance appears to be due to mutational alterations of the intracellular target of the drug, the RNA polymerase β subunit encoded by the rpoB gene (1, 3, 12). The mutations are generally clustered in a 702-bp fragment, from nucleotide positions 486 to 717 (Escherichia coli coordinates), corresponding to the rifampin resistance-determining (Rif) region in the center of the rpoB gene (1).
S. pyogenes BM4478 and Staphylococcus aureus BM4479, both resistant to high levels of rifampin (MIC, >256 μg/ml), were isolated in 1999 from a patient with a recurrent ulcer infection undergoing therapy with rifampin alone at the Hospital Henri Mondor, Créteil, France. The isolates remained susceptible to all antibiotics that are usually active against gram-positive cocci, except tetracycline for BM4478 and penicillin G and tetracycline for BM4479.
(An initial report of this work was presented at the 41st Interscience Conference on Antimicrobial Agents and Chemotherapy, Chicago, Ill., 16 to 19 December 2001 [H. Aubry-Damon, G. Gerbaud, and P. Courvalin, Abstr. 41st Intersci. Conf. Antimicrob. Agents Chemother., abstract C1-159, p. 82, 2001].)
We amplified by PCR the entire rpoB gene (Table 1, primer pair A) from BM4478 and CIP5641T, an antibiotic-susceptible S. pyogenes type strain (rifampin MIC = 0.008 μg/ml), and a portion of the rpoB gene (Table 1, primer pair F) corresponding to the Rif mutated region in previously studied bacterial genera (1, 2, 4, 8) from Staphylococcus aureus BM4479 and plasmid-free Staphylococcus aureus RN4220, which is susceptible to antibiotics (rifampin MIC = 0.008 μg/ml). The amplification products were cloned in the pCRII vector (Invitrogen) and sequenced on both strands with an automated sequencer (CEQ 2000 DNA Analysis system; Beckman Coulter).
TABLE 1.
Oligonucleotides used to detect mutations in the rpoB genes
| Primera | Sequence (5′-3′) | Size of PCR product (bp) | Origin or reference |
|---|---|---|---|
| S. pyogenes | |||
| Pair A | |||
| + | GATAACTTAGTTGCGATTTGC | 3,798 | This study |
| − | TTTGATGACTTTACCAGTTCC | ||
| Pair B | |||
| + | CCTGCTGATATTTTGGC | 520 | This study |
| − | TCAACCTTACGGTAAGG | ||
| Pair C | |||
| + | ATCGTTATGGGTCGTCA | 609 | This study |
| − | GTATCACGCGTTTCAGA | ||
| Pair Db | |||
| + | CGTGAACGTATGTCTGT | 370 | This study |
| − | CGGTCAACCTTACGGTA | ||
| Pair Eb | |||
| + | ATGCAACGTCAGGCTGT | 210 | This study |
| − | CCTGAGTTTGAACGACG | ||
| Staphylococcus aureus, pair F | |||
| + | AGTCTATCACACCTCAACAA | 702 | 1 |
| − | TAATAGCCGCACCAGAATCA |
+ and − indicate sense and antisense primers, respectively.
The same primers were used for S. pyogenes and S. pneumoniae.
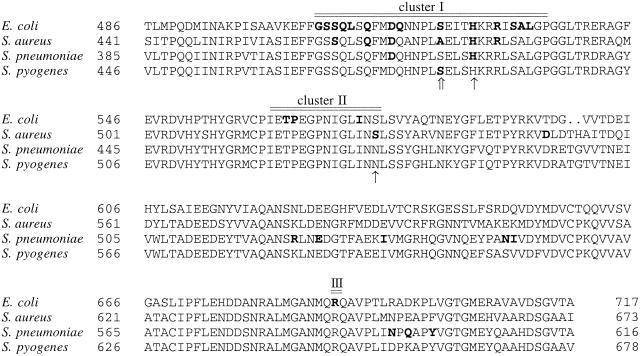
Relative to the susceptible strains CIP5641T and SF370 (accession number AE006480), S. pyogenes BM4478 had two base pair changes in the rpoB gene that resulted in amino acid substitutions (Fig. 1) as follows: in cluster I at position 522 (Ser522Leu) and outside of the Rif region at position 722 (Gln722His) (E. coli coordinates). The two mutational changes, His526Asn in cluster I and Ser574Leu in cluster II (E. coli coordinates), found in Staphylococcus aureus BM4479 have already been shown to confer high-level resistance and cross-resistance to the rifamycins (12). In Streptococcus pneumoniae and in Staphylococcus aureus, the His526Asn mutation, when present alone, confers low-level resistance (3, 12). Few Ser574Leu mutations were found in cluster II of rifampin-resistant E. coli (6). However, the level of resistance conferred was not investigated.
FIG. 1.
Amino acid sequence comparison of the Rif region of the rpoB gene of E. coli, Staphylococcus aureus, S. pneumoniae, and S. pyogenes. Clusters I, II, and III are indicated by a double line above the alignment. Dots indicate gaps introduced to optimize the alignment. Residues where substitutions are known to be involved in rifampin resistance are in bold. Mutations leading to rifampin resistance in S. pyogenes BM4478 and in Staphylococcus aureus BM4479 are indicated by double and single upward-pointing arrows, respectively.
To determine the role of the two alterations in S. pyogenes BM4478, purified PCR products (1 μg), each containing a single mutation, were added to rifampin-susceptible competent cells (5) of S. pneumoniae CP1000 (rifampin MIC = 0.023 μg/ml), and transformants were selected on rifampin at 10 μg/ml. The TCA/TTA (Ser522Leu) mutation was amplified as part of a 520-bp PCR product obtained with primer pair B and mutation CAA/CAC (Gln722His) was amplified as part of a 609-bp PCR product obtained with primer pair C (Table 1). The corresponding PCR products were also amplified from DNA of susceptible strain CIP5641T. The DNA of two transformants from each experiment was amplified and sequenced using primer pairs D and E (Table 1) to screen positions 522 and 722, respectively. Only transformation with the 520-bp PCR product containing the TTA mutation yielded resistant colonies at a frequency (Table 2) compatible with monogenic transformation (10). In the remaining experiments resistant derivatives of the recipient strain with mutations outside of the 370- and 210-bp portions sequenced were obtained at a frequency of ca. 10−6. These data indicate that in S. pyogenes BM4478 rifampin resistance was due to the Ser522Leu substitution located in cluster I. Mutations at this position also lead to high levels of resistance in Staphylococcus aureus (1), E. coli (4), Neisseria meningitidis (2), and Mycobacterium tuberculosis (8).
TABLE 2.
Transformation of S. pneumoniae CP1000 with PCR-amplified DNA from BM4478 and CIP5641T
| Sequence in donor DNA (amino acid)a | Frequency of resistant recipient on rifampin at 10 μg/ml | Sequence in resistant recipient DNA (amino acid) |
|---|---|---|
| 520-bp product | ||
| No DNA | 1.2 × 10−6 | TCA (Ser522) |
| TCA (Ser522) | 1.3 × 10−6 | TCA (Ser522) |
| TTA (Leu522) | 3.1 × 10−3 | TTA (Leu522) |
| 609-bp product | ||
| No DNA | 1.1 × 10−6 | CAA (Gln722) |
| CAA (Gln722) | 1.2 × 10−6 | CAA (Gln722) |
| CAC (His722) | 1.1 × 10−6 | CAA (Gln722) |
Amino acid positions are from E. coli coordinates.
Interestingly, the substitutions in S. pyogenes and Staphylococcus aureus clinical isolates were different. Staphylococcus aureus BM4479 probably acquired high-level rifampin resistance in two steps. Rifampin resistance emerges easily in Staphylococcus aureus, in particular in methicillin-resistant strains (1). The occurrence of multiple mutations may be explained by epidemic dissemination of strains and their frequent exposure to rifampin. The mutations in BM4478 and BM4479 were clustered from nucleotide positions 522 to 526 (E. coli coordinates), suggesting that substitution of the corresponding amino acids in cluster I of S. pyogenes, like in E. coli, prevents the binding of rifampin to RNA polymerase (11). It has been shown in E. coli that residues 516 to 540 are part of the target of rifampin and participate with residues 1065 and 1237 in the formation of the initiation site when the β subunit is assembled in the RNA polymerase complex (7).
This study suggests that, as in Staphylococcus aureus, cluster I in the central Rif region is the primary target for rifampin in S. pyogenes.
Acknowledgments
This work was supported in part by a Bristol-Myers Squibb Unrestricted Biomedical Research Grant in Infectious Diseases.
REFERENCES
- 1.Aubry-Damon, H., C. J. Soussy, and P. Courvalin. 1998. Characterization of mutations in the rpoB gene that confer rifampin resistance in Staphylococcus aureus. Antimicrob. Agents Chemother. 42:2590-2594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carter, P. E., F. J. R. Abadi, D. E. Yakubu, and T. H. Pennington. 1994. Molecular characterization of rifampin-resistant Neisseria meningitidis. Antimicrob. Agents Chemother. 38:1256-1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Enright, M., P. Zawadski, P. Pickerill, and C. G. Dowson. 1998. Molecular evolution of rifampicin resistance in Streptococcus pneumoniae. Microb. Drug Resist. 4:65-70. [DOI] [PubMed] [Google Scholar]
- 4.Jin, D. J., and C. A. Gross. 1988. Mapping and sequencing of mutations in the Escherichia coli rpoB gene that lead to rifampicin resistance. J. Mol. Biol. 202:45-58. [DOI] [PubMed] [Google Scholar]
- 5.Morrison, D. A., M.-C. Trombe, M. K. Hayden, G. A. Waszak, and J.-D. Chen. 1984. Isolation of transformation-deficient Streptococcus pneumoniae mutants defective in control of competence using insertion-duplication mutagenesis with the erythromycin resistance determinant of pAMβ1. J. Bacteriol. 159:870-876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Severinov, K., M. Soushko, A. Goldfarb, and V. Nikiforov. 1993. Rifampicin region revisited. J. Biol. Chem. 268:14820-14825. [PubMed] [Google Scholar]
- 7.Severinov, K., A. Mustaev, E. Severinova, M. Koslov, S. A. Darst, and A. Goldfarb. 1995. The beta subunit Rif-cluster I is only angstroms away from the active center of Escherichia coli RNA polymerase. J. Biol. Chem. 270:29428-29432. [DOI] [PubMed] [Google Scholar]
- 8.Taniguchi, H., H. Aramaki, Y. Nikaido, Y. Mizuguchi, M. Nakamura, T. Koga, and S. Yoshida. 1996. Rifampicin resistance and mutation of the rpoB gene in Mycobacterium tuberculosis. FEMS Microbiol. Lett. 144:103-108. [DOI] [PubMed] [Google Scholar]
- 9.Tanz, R. R., T. Stanford, and T. Schulman. 1985. Penicillin plus rifampin eradicates pharyngeal carriage of group A streptococci. J. Pediatrics 106:876-880. [DOI] [PubMed] [Google Scholar]
- 10.Tiraby, G., and M. S. Fox. 1973. Marker discrimination in transformation and mutation of pneumococcus. Proc. Natl. Acad. Sci. USA 70:3541-3545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wehrli, W. 1983. Rifampin: mechanisms of action and resistance. Rev. Infect. Dis. 5(Suppl. 3):S407-S411. [DOI] [PubMed] [Google Scholar]
- 12.Wichelhaus, T. A., V. Schäfer, V. Brade, and B. Böddinghaus. 1999. Molecular characterization of rpoB mutations conferring cross-resistance to rifamycins on methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 43:2813-2816. [DOI] [PMC free article] [PubMed] [Google Scholar]