Abstract
Cidofovir {[(S)-1-(3-hydroxy-2-phosphonylmethoxypropyl)cytosine] [HPMPC]}-resistant forms of camelpox, cowpox, monkeypox, and vaccinia viruses were developed by prolonged passage in Vero 76 cells in the presence of drug. Eight- to 27-fold-higher concentrations of cidofovir were required to inhibit the resistant viruses than were needed to inhibit the wild-type (WT) viruses. Resistant viruses were characterized by determining their cross-resistance to other antiviral compounds, examining their different replication abilities in two cell lines, studying the biochemical basis of their drug resistance, and assessing the degrees of their virulence in mice. These viruses were cross resistant to cyclic HPMPC and, with the exception of vaccinia virus, to (S)-1-(3-hydroxy-2-phosphonylmethoxypropyl)adenine. Three of the four resistant cowpox and monkeypox viruses exhibited reduced abilities to infect and replicate in 3T3 cells compared to their abilities in Vero 76 cells. Compared to the WT virus polymers the resistant cowpox virus DNA polymerase was 8.5-fold less sensitive to inhibition by cidofovir diphosphate, the active form of the drug. Intracellular phosphorylation of [3H]cidofovir was not stimulated or inhibited by infection with resistant cowpox virus. In intranasally infected BALB/c mice, WT cowpox virus was 80-fold more virulent than the resistant virus. Cidofovir treatment (100 mg/kg of body weight, given one time only as early as 5 min after virus challenge) of a resistant cowpox virus infection could not protect mice from mortality. However, the drug prevented mortality in 80 to 100% of the mice treated with a single 100-mg/kg dose at 1, 2, 3, or 4 days after WT virus challenge. By application of these results to human orthopoxvirus infections, it is anticipated that resistant viruses may be untreatable with cidofovir but their virulence may be attenuated. Studies will need to be conducted with cidofovir-resistant monkeypox virus in monkeys to further support these hypotheses.
Although smallpox virus has been eradicated from human populations, concerns about infections with poxviruses are increasing. The use of smallpox virus as a bioterrorist weapon is a significant possibility (6, 22). Monkeypox virus has recently reemerged in the Democratic Republic of the Congo, with person-to-person transmission and some fatalities occurring (13). Molluscum contagiosum, which is caused by another poxvirus, is a problematic skin infection in AIDS patients (19). Vaccinia virus can cause severe infections in immunocompromised individuals (15). An approved treatment for all of these conditions would be desirable.
In the past, marboran was used to treat smallpox virus infections but was judged to be ineffective (12). Ribavirin, when combined with immunoglobulin, showed efficacy in the treatment of a vaccinia virus infection in an immunocompromisedindividual (15). (S)-1-(3-Hydroxy-2-phosphonylmethoxypro-pyl)adenine (HPMPA) and cidofovir {[(S)-1-(3-hydroxy-2-phosphonylmethoxypropyl)cytosine] [HPMPC]} have beenused successfully in experimental mouse models of vaccinia virus infections (9, 20, 25). AIDS patients treated with cidofovir for their concurrent molluscum contagiosum infections have shown dramatic improvement (17, 33). It has recently been reported that the drug was very effective in treating cowpox virus infections in mice (5, 24).
Cidofovir-resistant (CDV-R) isolates of cytomegalovirus have been isolated from treated patients (14, 31) or derived by cell culture passage of wild-type (WT) viruses under drug pressure (16, 26). Mutations were found in the viral DNA polymerase gene that conferred drug resistance (29, 32). Resistance to cidofovir results in cross-resistance to other antiviral drugs (29, 31). The most serious clinical consequence of infection with drug-resistant viruses is the inability to effectively treat the disease with the specific medication and sometimes with other similarly acting drugs. Drug-resistant virus variants which are weakened in virulence compared to WT viruses (26), causing only mild infections in the host, may also arise.
Cidofovir is the most effective antiorthopoxvirus agent currently under preclinical investigation, and for this reason, it is being considered for licensure. The present study was initiated to determine what kinds of problems, such as cross-resistance to other inhibitors, might be anticipated in the treatment of CDV-R viruses and whether resistant viruses will be as virulent as the parental virus strain in vivo. In order to further compare resistant and WT viruses, experiments were performed to determine the differential replicative properties of the viruses in two cell lines and to ascertain the biochemical basis of their drug resistance.
MATERIALS AND METHODS
Antiviral compounds.
Cidofovir, cyclic HPMPC (4), cidofovir diphosphate (cidofovir-PP), and HPMPA were obtained from Norbert Bischofberger, Gilead Sciences, Foster City, Calif. [3H]cidofovir was purchased from Moravek Biochemicals, Brea, Calif. Ribavirin was obtained from ICN Pharmaceuticals, Costa Mesa, Calif. Carbocyclic 3-deazaadenosine (C-c3Ado) (10) was supplied by John Secrist, Southern Research Institute, Birmingham, Ala. Mycophenolic acid (MPA) (11) and the 5′-triphosphate derivative of cytosine arabinoside (Ara-CTP) (30) were purchased from Sigma Chemical Co., St. Louis, Mo.
Viruses and cells.
Camelpox (Somalia strain), cowpox (Brighton strain), monkeypox (Zaire strain), and vaccinia (Copenhagen strain) viruses were obtained from Joseph Esposito, Centers for Disease Control and Prevention, Atlanta, Ga. The viruses were propagated in African green monkey kidney (Vero 76) cells. The Vero 76 and BALB/3T3 clone A31 cells(3T3 cells) used in the virus experiments were obtained from the American Type Culture Collection, Manassas, Va. The cells were cultured in Dulbecco's high-glucose medium containing 10% fetal bovine serum. The serum concentration was reduced to 2% for the assays and virus propagation. A low number of cell culture passages of poxviruses (passaged three times from originally obtained stocks) was used to initiate these studies.
Development and isolation of CDV-R and WT viruses.
CDV-R forms of the above-mentioned viruses were prepared by replicating the viruses for at least 20 passages in the presence of increasing concentrations of drug. Additional passages of the viruses in the absence of drug were often needed during this process to enhance the virus titers prior to subsequent exposure to drug. The final virus preparations were twice plaque purified by dilution to extinction in 96-well plates. Drug sensitivity assays were run with 5 to 10 virus isolates per plaque purification step to select the resistant virus for later use. Low-passage WT viruses were also twice plaque purified by the process described above. Large virus pools were made in Vero 76 cells (in medium devoid of cidofovir) from the final virus isolates. For the other comparisons, WT cowpox viruses were passaged 30 times in Vero 76 cells in drug-free medium.
During the process described above, two types each of CDV-R cowpox and monkeypox viruses were isolated, one of which produced rounded cells during infection and another that produced syncytia. With the camelpox and vaccinia viruses, we were able to detect and plaque purify only viruses that produced a rounded-cell cytopathology (no syncytium-forming [SF] viruses were present). The twice-plaque-purified CDV-R viruses were designated as follows: resistant camelpox, camelpox-R; resistant cowpox causing rounded-cell cytopathology, cowpox-R; resistant syncytium-forming cowpox, cowpox-R (SF); resistant monkeypox causing rounded-cell cytopathology, monkeypox-R; resistant syncytium-forming monkeypox, monkeypox-R (SF); and resistant vaccinia, vaccinia-R. The WT viruses were also plaque purified from low-passage in vitro stocks by the process explained above and were designated, e.g., as cowpox-WT virus. A syncytium-forming WT cowpox virus was isolated during this process and designated cowpox-WT (SF) virus. As described below, some of the SF viruses differed from their sister viruses (those producing rounded-cell cytopathology) in their replicative properties, in cell culture, and/or in their virulence properties in mice.
Plaque reduction and virus yield assays.
The sensitivities of the plaque-purified WT and CDV-R poxviruses to selected antiviral compounds were determined in six-well plates of Vero 76 cells. The selected compounds represented different classes of antiviral agents, such as those inhibiting viral DNA polymerases (cidofovir, cyclic HPMPC, and HPMPA) (34), IMP dehydrogenase inhibitors (ribavirin and MPA) (11, 23), and C-c3 Ado, an inhibitor of S-adenosylhomocysteine hydrolase (10). Plates of cells were infected with about 100 PFU of virus per well, the virus was adsorbed for 1.5 to 2 h, and then twofold dilutions of antiviral compounds were applied. The incubation times differed for the viruses as follows: vaccinia virus, 3 days; cowpox virus, 4 days; monkeypox virus, 6 days; and camelpox virus, 7 days. At the end of the incubation periods, the vaccinia, cowpox, and monkeypox viruses formed 3-mm-diameter plaques, whereas, camelpox virus produced smaller, 1-mm-diameter, plaques. The cells were fixed and stained in 3% buffered formalin-0.2% crystal violet for 15 min. The plaques were counted with the aid of a handheld magnifying lens. The concentrations of the compounds reducing plaque numbers by 50% (EC50s) were determined by plotting the percentage of reduction versus the inhibitor concentration on semi-log10 graph paper.
To determine the differential abilities of WT and CDV-R viruses to replicate in Vero 76 and 3T3 cells, virus yield assays were conducted. Twelve-well plates of cells were infected with cowpox or monkeypox virus at about 100 PFU/well. Lower dilutions of virus stocks were required to achieve 100 PFU/well in 3T3 cells than in Vero 76 cells because of the different plaquing efficiencies of the two cell types (see Table 2). After virus adsorption (1.5 to 2 h), the cells were fed maintenance medium with or without drug. Each day, a portion of the infected cells was frozen, thawed, and sonicated for 30 s. Subsequently, the medium (including both intracellular and extracellular virus produced during the infection) was titrated by plaque assay on new monolayers of Vero 76 cells. After 4 or 6 days, the cells were fixed and stained and the plaques were counted.
TABLE 2.
Differential plaquing efficiencies of Vero 76 (monkey) and 3T3 (mouse) cells for WT and CDV-R poxviruses
| Virus strain | Virus titera (log10 PFU/ml) in:
|
n-Fold differencec | |
|---|---|---|---|
| Vero 76 cells | 3T3 cells | ||
| Cowpox-WT | 8.4 ± 0.4 | 7.1 ± 0.5 | 20 |
| Cowpox-WT (p30)b | 8.3 ± 0.1 | 7.3 ± 0.1 | 10 |
| Cowpox-R | 7.7 ± 0.3 | 5.5 ± 0.5 | 160 |
| Cowpox-WT (SF) | 8.3 ± 0.4 | 7.0 ± 0.1 | 20 |
| Cowpox-WT (SF) (p30)b | 8.5 ± 0.1 | 7.6 ± 0.1 | 8 |
| Cowpox-R (SF) | 8.1 ± 0.3 | 6.9 ± 0.1 | 16 |
| Monkeypox-WT | 7.3 ± 0.2 | 6.2 ± 0.5 | 13 |
| Monkeypox-R | 8.9 ± 0.1 | 6.3 ± 0.1 | 400 |
| Monkeypox-R (SF) | 7.3 ± 0.3 | 4.0 ± 0.2 | 2,000 |
Values are means of three separate determinations ± standard deviations.
Virus passaged 30 times in Vero 76 cells.
Virus titer in Vero 76 cells divided by virus titer in 3T3 cells.
In order to compare the plaquing efficiencies on Vero 76 and 3T3 cells for the different forms of cowpox and monkeypox viruses, pools of each virus were titrated in parallel in the two cell lines. After 4 or 6 days, the cells were fixed and stained and the plaques were counted.
Intracellular phosphorylation of cidofovir.
Confluent monolayers of Vero 76 cells in T-25 flasks were exposed to cowpox-WT or cowpox-R (SF) virus at 0.1 PFU per cell. This infecting dose caused considerable damage to the monolayers at 24 h. After 1 h of virus adsorption, the medium was removed and replaced with 30 or 100 μM [3H]cidofovir. Uninfected cells were treated in parallel. After 24 h, the medium was removed and the cells were treated with 3.5% perchloric acid to release nucleotides into the medium. The samples were neutralized with 10 N NaOH containing 1 M imidazole. The samples were stored at −70°C until they were analyzed with a strong anion-exchange (SAX) column (Whatman, Clifton, N.J.) by a high-pressure liquid chromatography method described previously (21). The amounts of cidofovir-PP present were expressed as picomoles of compound per 106 cells.
Cowpox DNA polymerase purification and assay.
Cowpox-WT and cowpox-R (SF) viruses were each used to infect approximately 109 Vero 76 cells (80 T-150 flasks of cells per virus) at 1 to 3 PFU/cell. These viruses were selected because they were the ones used in the animal experiments. After 5 h of incubation, the infected cells were scraped from the flasks, pelleted by low-speed centrifugation, and stored at −70°C. The procedures for disrupting the cells and partially purifying the DNA polymerases were the same as those used by Moss and Cooper (18) to study vaccinia virus DNA polymerase. The basic method, as previously described, involved the use of DE-52 (Whatman) and P-11 phosphocellulose (Whatman) column chromatographies with gradient buffers. The DE-52 column clearly separated the virus-induced DNA polymerase activity from cell enzyme activity. The DNA polymerase reaction mixture (100-μl volume) contained 50 mM potassium phosphate (pH 7.5), 5 mM MgCl2, 0.5 mM dithiothreitol, 10 μg of activated calf thymus DNA (Sigma) per ml, 100 μM concentration of dATP, dGTP, and dCTP, 5 μM tritiated (2 μCi/reaction mixture) TTP (Moravek Biochemicals), and 1 mg of bovine serum albumin per ml. After incubation for 4 h at 37°C, aliquots were spotted on DE-81 chromatography paper squares (Whatman) and washed in 5% sodium phosphate (dibasic) by the method described by Altman and Lerman (1).
Once the enzymes were purified and stored at −70°C in 50% glycerol, the substrate concentration required for 50% maximal enzyme velocity (Michaelis constants [Km values]) was determined. dCTP was evaluated, since in later experiments, this would be the competitive substrate for the inhibitors Ara-CTP and cidofovir-PP. Km determinations were made with nonradioactive dATP, dGTP, and TTP (100 μM each) and [3H]dCTP (2μCi/reaction mixture; Moravek Biochemicals) at various concentrations. Plotting the inverse of the substrate concentration versus the inverse of the velocity (Lineweaver-Burk plots) yielded the Km values.
The competitive effects of Ara-CTP and cidofovir-PP on the rates of the DNA polymerase reactions were studied by testing varying concentrations of these inhibitors against fixed concentrations of [3H]dCTP. For Ara-CTP, the competitive concentrations of dCTP used were 1 and 3μM. Because the potency of cidofovir-PP was much less than that of Ara-CTP (requiring much higher concentrations of cidofovir-PP in the reaction mixture) and the amount of cidofovir-PP was very limited, it was necessary to test DNA polymerase activity at a lower competitive concentration (0.25 μM) of dCTP. The concentrations of the compounds that reduced the rate of enzymatic reactions by 50% (IC50s) were determined by plotting the percentage of reduction versus the inhibitor concentration on semi-log10 graph paper. Inhibition constants (Ki values) were calculated from the formula IC50 = Ki (1 + S/Km), where S was the concentration of dCTP in the reaction mixture. The formula relating Ki to IC50 was previously published (7).
Mouse experiments.
Normal BALB/c mice weighing 13 to 15 g each at the start of the infection were purchased from B & K Universal, Fremont, Calif. Severe combined immunodeficient (SCID) mice weighing about 20 g each were obtained from the National Institutes of Health breeding colony at Fort Detrick, Frederick, Md. They were kept 5 or 10 to a cage for the infection studies. For the mouse experiments, we adhered to the Guide for the Care and Use of Laboratory Animals (19a) and used facilities fully accredited by the American Association for Accreditation of Laboratory Animal Care.
In order to run proper comparative experiments, it was first necessary to determine the relative virulences of the WT and drug-resistant viruses in mice. Based upon previous studies performed with CDV-R murine cytomegalovirus (26), it was anticipated that CDV-R poxviruses would be less virulent than WT viruses in mice. To determine the virulence of the cowpox virus, mice were infected intranasally with 0.05 ml of WT or CDV-R viruses (after the mice were anesthetized by intraperitoneal injection with ketamine [100 mg/kg of body weight]). The virus was given in 3.2-fold (0.5-log10)-dilution increments to groups of mice, with the highest dose being 107 or 108 PFU of WT or CDV-R virus, respectively, per animal. The mice were held until death or for 21 days. Because of the high cost of nonhuman primates, we were unable to conduct virulence studies of CDV-R monkeypox viruses with monkeys. There is no small-animal model for camelpox virus, and the WT strain of vaccinia virus was not lethal to mice. Thus, the studies with mice were confined to investigation of cowpox virus.
Antiviral experiments were conducted with healthy BALB/c mice challenged intranasally with 10 50% lethal doses (LD50) of virus (as determined in the manner described above). Infections were initiated with either 1 × 106 PFU of WT virus or 8 × 107 PFU of cowpox-R (SF) virus per animal. Intraperitoneal treatments with cidofovir were given by injection immediately after (within 5 min) or 1 or more days after virus inoculation (see Table 4). The lungs from five mice per group were collected after sacrifice on day 4 for lung virus titer determinations. Deaths were recorded daily through 21 days.
TABLE 4.
Effects of cidofovir on lethal cowpox virus infections in BALB/c mice caused by WT and CDV-R viruses
| Treatmenta | Survivors/total no. of mice | Day of death (mean ± SD)c | Lung virus titer on day 4 (log10 ± SD) |
|---|---|---|---|
| Cowpox-WT | |||
| Cidofovir | |||
| 0b | 10/10e | >21 ± 0.0 | 3.8 ± 0.5e |
| 1 | 8/10e | 11.0 ± 1.4 | 6.8 ± 0.4f |
| 2 | 9/10e | 7.0 ± 0.0 | 7.2 ± 0.5g |
| 3 | 10/10c | >21 ± 0.0 | 7.7 ± 0.3 |
| 4 | 8/10e | 9.0 ± 0.0 | NDd |
| 5 | 0/10 | 10.4 ± 2.7 | NDd |
| Placebo | |||
| 0 | 0/10 | 8.6 ± 1.3 | 7.9 ± 0.1 |
| Cowpox-R (SF) | |||
| Cidofovir | |||
| 0 | 0/10 | 8.3 ± 0.7e | 8.1 ± 0.1g |
| 1 | 0/10 | 7.7 ± 0.5f | 8.0 ± 0.2g |
| 2 | 0/10 | 7.7 ± 1.1 | 8.1 ± 0.2 |
| 3 | 0/10 | 7.5 ± 0.7 | 8.2 ± 0.1 |
| Placebo | |||
| 0 | 0/10 | 7.0 ± 0.0 | 8.4 ± 0.1 |
For cidofovir treatment, a 100-mg/kg dose was administered intraperitoneally one time only on the day of treatment.
Following the day of virus challenge. Mice treated on day 0 were given treatment immediately after infection.
Of mice that died prior to day 21.
ND, not determined. The titers of these groups would be equivalent to those of the placebo group because of the time of first treatment.
Significantly different from results obtained with the placebo-treated group (P < 0.001).
Significantly different from results obtained with the placebo-treated group (P < 0.01).
Significantly different from results obtained with the placebo-treated group (P < 0.05).
In a second study, SCID mice were infected intranasally with either 106 PFU of WT virus or 107 PFU of cowpox-R (SF) virus per animal. The dose of the resistant virus was less than that used to infect the healthy BALB/c mice (see above), because orthopoxvirus infections in immunodeficient mice are more severe (20) and the treatment efficacy in healthy mice proved to be negligible. Cidofovir treatments were given every 3 days from days 0 through 30 after virus challenge. Deaths were recorded daily through 45 days (when all the animals were dead). The lungs and nasal and sinus tissues from some of the mice that died were collected for the determination of virus titers and sensitivity to inhibition by cidofovir.
For virus titer determinations in tissues, the tissues were harvested, weighed, and frozen at−70°C. Later, thawed tissues were homogenized with sterile mortars and pestles in 1 ml of cell culture medium, and then the homogenates were frozen. On the day of titration, the homogenates were sonicated for 30 s each and centrifuged at 600 × g for 5 min. The samples were serially diluted in 10-fold increments and plaque titrated in either 6- or 12-well plates of Vero 76 cells. The numbers of plaques were determined after 3 or 4 days, after the samples were fixed and stained with crystal violet (5, 24). Virus titers were reported as log10 PFU per gram of tissue.
The treatment schedules and doses of cidofovir that were used for the experiments conducted with BALB/c and SCID mice were based upon previous work (5, 25). The single-dose and infrequent-treatment regimens with cidofovir were not toxic to the mice, as judged by weight gain and the lack of alterations of selected blood components (creatinine, blood urea nitrogen, alanine aminotransferase, and aspartate aminotransferase) that are indicative of toxicity in uninfected, treated mice (data not shown).
For these antiviral studies, statistical interpretations of increases in the numbers of survivors were determined by the two-tailed Fisher exact test. Increases in the mean day of death and reductions in lung virus titers were statistically analyzed by the two-tailed Mann-Whitney U test. All comparisons of drug-treated groups were made to the placebo control group by use of the InStat computer program (GraphPad Software, San Diego, Calif.).
RESULTS
In vitro activities of drugs against WT and CDV-R poxviruses.
In plaque reduction assays, 16- to 27-fold-higher concentrations of cidofovir were required to inhibit the cowpox-R and monkeypox-R viruses than were required to inhibit WT viruses (Table 1). The degrees of resistance were less for camelpox and vaccinia viruses (8- and 10-fold-higher concentrations, respectively, than were needed to inhibit WT viruses). Viruses that were resistant to cidofovir were resistant to a similar degree to cyclic HPMPC, which is a prodrug form of cidofovir (4). Resistant cowpox viruses were 80- to 95-fold more resistant than WT viruses to HPMPA; resistant monkeypox and camelpox viruses were 18- to 24-fold more resistant to this adenosine analog than were the WT viruses. Interestingly, vaccinia-R virus was still potently inhibited by HPMPA, with only a twofold decrease in sensitivity to the compound. MPA, C-c3Ado, and, for the most part, ribavirin, inhibited resistant and WT viruses to nearly the same degrees. Vaccinia-R virus was fivefold less sensitive than vaccinia-WT virus to inhibition by ribavirin. However, when a 90% reduction in virus yield was used as a measure of ribavirin activity against vaccinia-WT and -R viruses, the differences in potency were only twofold (data not shown).
TABLE 1.
Activities of compounds against WT and CDV-R poxviruses, as determined by plaque reduction assays in Vero 76 cells
| Virus strain | EC50 (μM)a of:
|
|||||
|---|---|---|---|---|---|---|
| MPA | Ribavirin | C-c3Ado | Cidofovir | Cyclic HPMPC | HPMPA | |
| Camelpox-WT | 2.5 ± 0.5 | 290 ± 36 | 39 ± 1.2 | 2.3 ± 0.5 | 2.2 ± 0.5 | 0.5 ± 0.2 |
| Camelpox-R | 2.4 ± 0.1 | 215 ± 28 | 20 ± 2.6 | 22 ± 5 (10) | 19 ± 3.6 (9) | 12 ± 3.3 (24) |
| Cowpox-WT | 3.2 ± 0.5 | 625 ± 165 | >1,000 | 45 ± 7 | 57 ± 4.2 | 4.2 ± 0.6 |
| Cowpox-WT (SF) | 3.2 ± 0.2 | 605 ± 75 | >1,000 | 58 ± 13 | 47 ± 16 | 4.6 ± 0.8 |
| Cowpox-R | 3.3 ± 1.1 | 430 ± 80 | >1,000 | >1,000 (>22) | >1,000 (>18) | >400 (>95) |
| Cowpox-R (SF) | 3.7 ± 0.2 | 640 ± 95 | >1,000 | 730 ± 160 (16) | >1,000 (>18) | 330 ± 65 (79) |
| Monkeypox-WT | 2.5 ± 1.3 | 96 ± 19 | 4.5 ± 2.5 | 27 ± 11 | 34 ± 25 | 3.7 ± 1.3 |
| Monkeypox-R | 1.9 ± 0.2 | 140 ± 25 | 4.2 ± 1.8 | 505 ± 50 (19) | 760 ± 340 (22) | 68 ± 18 (18) |
| Monkeypox-R (SF) | 1.0 ± 0.1 | 145 ± 28 | 5.5 ± 2.1 | 725 ± 105 (27) | 850 ± 210 (25) | 80 ± 40 (22) |
| Vaccinia-WT | 0.4 ± 0.3 | 21 ± 6 | 20 ± 8 | 19 ± 6 | 21 ± 9 | 3.4 ± 0.7 |
| Vaccinia-R | 1.0 ± 0.5 | 97 ± 31 (5) | 9 ± 1.4 | 150 ± 36 (8) | 185 ± 105 (9) | 8 ± 1.7 |
Values are means of three separate determinations ± standard deviations. The numbers in parentheses refer to the n-fold change in potency (the EC50 against the resistant virus divided by the EC50 against the parental WT virus).
Comparative replication of viruses in Vero 76 and 3T3 cells.
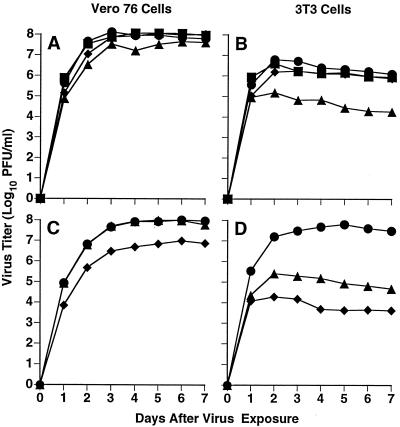
Drug-resistant viruses may exhibit altered or decreased abilities to replicate relative to their WT counterparts. In order to investigate this possibility, the replication of cowpox and monkeypox viruses in Vero 76 and mouse 3T3 cells was studied. 3T3 cells were selected in order to make a correlation between mouse cell culture data and in vivo virulence study results. CDV-R cowpox viruses replicated in Vero 76 cells to approximately the same titers as those of WT viruses (Fig. 1A). The cowpox-R virus produced about 30-fold less virus than did the WT virus in 3T3 cells (Fig. 1B), whereas the cowpox-R (SF) strain replicated as well as the WT cowpox did in these cells. Monkeypox viruses showed a slightly different pattern of replication. The monkeypox-R (SF) strain was less able than WT virus cells to replicate in Vero 76 cells (Fig. 1C), and both the monkeypox-R and monkeypox-R (SF) strains replicated poorly in 3T3 cells compared to the replication of WT virus (Fig. 1D).
FIG. 1.
WT and CDV-R cowpox (A and B) and monkeypox (C and D) virus yields from Vero 76 (monkey) and 3T3 (mouse) cells. Approximately 100 virus PFU/well was used to initiate each infection. Symbols: •, WT virus; ▪, WT (SF) virus; ▴, CDV-R virus; ⧫, CDV-R (SF) virus. The assay variability was no greater than ±3.2-fold (0.5 log10).
As a follow-up to the experiments described above, Vero 76 and 3T3 cells were studied for their abilities to plaque cowpox and monkeypox virus stocks. Pools of each virus were plaque titrated under standard conditions, and the plaques were counted. The 3T3 cells were less efficient than the Vero 76 cells in plaquing the viruses of either WT species (Table 2). 3T3 cells were much less able than Vero 76 cells to plaque cowpox-R, monkeypox-R, and monkeypox-R (SF) viruses. However, 3T3 cells were able to plaque the cowpox-R (SF) strain and the cowpox-WT viruses to the same levels. Cowpox-WT and cowpox-WT (SF) viruses that were passaged 30 times in Vero 76 cells were as infective to 3T3 cells as were low-passage cowpox strains.
Phosphorylation of cidofovir in infected cells.
The antiviral form of cidofovir in cells is cidofovir-PP, an analog of dCTP that inhibits viral DNA polymerases (34). To test whether viral resistance to cidofovir could be the result of reduced intracellular phosphorylation in infected cells, cells were exposed to virus and [3H]cidofovir for 24 h, followed by analysis of cidofovir-PP content. Uninfected, cowpox-WT-infected, and cowpox-R (SF)-infected Vero 76 cells exposed to 30 μM [3H]cidofovir had cidofovir-PP levels of 4.8, 5.6, and 5.1 pmol/106 cells, respectively. Cells treated with a 100 μM drug concentration had levels of 18, 15, and 14 pmol/106 cells, respectively. These results indicate that the levels of phosphorylation of cidofovir did not differ appreciably among uninfected cells, cells infected with WT cowpox virus, and cells infected with CDV-R cowpox virus. Thus, resistance of cowpox virus to cidofovir appears to be unrelated to differences in the levels of intracellular phosphorylation of the drug following infections with WT or resistant viruses, since no differences were detected.
Inhibition of cowpox DNA polymerase.
Ara-CTP and cidofovir-PP were compared for their abilities to inhibit cowpox DNA polymerase that was partially purified from cowpox-WT and cowpox-R (SF) virus strains (Table 3). Km values for dCTP for the cowpox-WT and -R (SF) viruses were 2.3 and 2.7 μM, respectively. Ara-CTP was only twofold less inhibitory to CDV-R virus polymerase than it was to the WT enzyme (comparing Ki/Km ratios), whereas cidofovir-PP was 8.5-fold less inhibitory to cowpox-R (SF) polymerase than it was to the WT enzyme. These data support the hypothesis that decreased sensitivity of the resistant virus DNA polymerase to cidofovir-PP may largely account for the drug resistance phenotype.
TABLE 3.
Inhibition of WT and CDV-R cowpox virus DNA polymerase activities by cidofovir-PP and Ara-CTP
| Virus | Km values (μM) for dCTPa | Cidofovir-PP
|
Ara-CTP
|
||
|---|---|---|---|---|---|
| Ki (μM)a | Ki/Km | Ki (μM) | Ki/Km | ||
| Cowpox-WT | 2.3 ± 0.7 | 26 ± 4 | 11.3 | 1.3 ± 0.1 | 0.6 |
| Cowpox-R (SF) | 2.7 ± 0.2 | 260 ± 85 | 96 (8.5) | 3.3 ± 0.1 | 1.2 (2) |
Values are the means of three independent assays ± standard deviations. Values in parentheses represent the Ki/Km ratio for the resistant virus divided by the Ki/Km ratio for the WT virus.
Lethality of cowpox viruses in mice.
WT and CDV-R forms of cowpox virus were evaluated for their abilities to cause lethal disease in BALB/c mice when administered intranasally. The LD50 of cowpox-WT or cowpox-WT (SF) virus was approximately 105 PFU/mouse. Cowpox-R virus was unable to kill mice at 108 PFU/animal, whereas the LD50 of cowpox-R (SF) virus was 8 × 106 PFU/mouse. Thus, the cowpox-R strain was not useful for chemotherapy studies due to its low virulence, but the cowpox-R (SF) strain was acceptable if given intranasally at a high infectious dose.
The multiple cell culture passages required to create CDV-R viruses may have caused genetic changes unrelated to the cidofovir-induced mutation(s) that resulted in virulence attenuation in vivo. To investigate this possibility, cowpox-WT and cowpox-WT (SF) viruses were passaged 30 times in Vero 76 cells in the absence of drug and then tested for virulence in mice. Both of these WT viruses had approximately the same levels of virulence for animals as did the low-passage WT viruses (data not shown), demonstrating that cell culturing alone did not alter in vivo virulence in a currently measurable or detectable way.
Treatment of cowpox virus infections in BALB/c mice with cidofovir.
Single intraperitoneal cidofovir treatments were given to mice that were infected intranasally with 10 LD50 of either cowpox-WT or cowpox-R (SF) viruses (Table 4). The compound was 80 to 100% protective against WT virus when given on day 0, 1, 2, 3, or 4 after infection. Lung virus titers (determined on day 4 of the infection) were significantly reduced in groups treated on day 0, 1, or 2. In particular, treatment on day 0 caused a marked (3,200-fold) reduction in lung virus titer. Mice infected with cowpox-R (SF) virus received little benefit from cidofovir treatment. Treatment on day 0 or 1 increased the mean day of death by a maximum of 1.3 days, and all mice died. Only moderate (less than three-fold) decreases in lung virus titers were seen on day 4 following these early treatments.
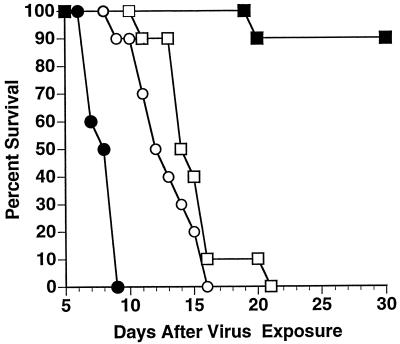
Treatment of cowpox virus infections in SCID mice with cidofovir.
SCID mice were infected intranasally with cowpox virus and treated every 3 days with cidofovir (100 mg/kg) through day 30 of the infection. Cowpox-WT virus-infected animals treated with placebo were dead by day 9, whereas only 10% of the cidofovir-treated mice were dead at day 30 (Fig. 2). After treatments were discontinued, the live mice remaining in the cidofovir-treated group were dead by day 44 (data not shown). The fact that cidofovir could not prevent mortality in SCID mice infected with cowpox-WT virus corresponds to the results reported for cidofovir treatment of vaccinia virus (20) and murine cytomegalovirus (28) infections in this mouse strain.
FIG. 2.
Treatment of intranasal infections with WT and CDV-R cowpox virus in SCID mice. Starting immediately after intranasal virus challenge, subcutaneous treatments (100 mg/kg) were given once daily every 3 days through day 30. Symbols: •, placebo-treated cowpox-WT virus-infected mice; ▪, cidofovir-treated cowpox-WT virus-infected mice; ○, placebo-treated cowpox-R (SF) virus-infected mice; □, cidofovir-treated cowpox-R (SF) virus-infected mice.
Placebo-treated SCID mice infected with cowpox-R (SF) virus were dead by day 15 (Fig. 2). Mice treated with cidofovir had a mean delay in death of 1.5 days, which was not significantly different from the results for the placebo group but does suggest a minor inhibitory effect on disease progression (as was observed in healthy mice) (Table 4). The lungs and nasal and sinus tissues of mice infected with cowpox-R (SF) virus that died on days 14 to 16 were subjected to virus titer assays. Both the placebo- and cidofovir-treated groups had approximately equal virus titers (>107 PFU/g in the lungs and >108 PFU/g in the nasal and sinus tissues).
WT and cowpox-R viruses recovered from treated mice were analyzed by plaque reduction assay in Vero 76 cells to determine their sensitivities to cidofovir. The drug had essentially the same EC50s against the recovered viruses as it did against the original infecting viruses (data not shown).
DISCUSSION
Through extensive cell culture adaptation, orthopoxviruses which exhibited 8- to 27-fold-greater resistance than WT viruses to cidofovir were developed. The extent of viral resistance to the drug is on the same order of magnitude as that reported against CDV-R forms of herpes simplex virus (2) and cytomegaloviruses (26, 31). For all resistant poxviruses tested, cross-resistance was also evident toward cyclic HPMPC, a prodrug form of cidofovir (4). Camelpox, cowpox, and monkeypox viruses were cross resistant to HPMPA. Similar findings have been published for herpes simplex virus and murine cytomegaloviruses (2, 26). The CDV-R vaccinia virus was not cross resistant to HPMPA, suggesting a different type of drug resistance mutation than that exhibited by the other viruses. It was curious that this virus showed a moderately decreased (fivefold less) sensitivity to ribavirin by plaque reduction. However, by virus yield reduction, the difference in the potencies of ribavirin against the WT and resistant viruses was only twofold (data not shown), indicating no appreciable difference in activity. Cross-resistance between ribavirin and cidofovir would not be expected, since ribavirin acts via inhibition of cellular IMP dehydrogenase (23, 27) whereas cidofovir is a viral DNA polymerase inhibitor (34). Application of these data to a possible clinical situation suggests the possibility that treatment of variola or monkeypox virus infections in humans could lead to the emergence of CDV-R viruses that are cross resistant to other antiviral compounds.
Experiments on the mode of drug resistance were conducted to determine the nature of the resistance phenotype. These focused on studying the intracellular phosphorylation of cidofovir to the active form (cidofovir-PP) and determining the effect of cidofovir-PP on the viral DNA polymerase obtained from WT and resistant viruses. In the first set of experiments, cidofovir was shown to be phosphorylated to cidofovir-PP in uninfected, cowpox-WT-infected, and cowpox-R (SF)-infected cells to approximately the same degrees. This result was similar to its metabolism in cells infected with WT and CDV-R forms of murine cytomegalovirus (21). The degrees of phosphorylation of cidofovir in cowpox virus-infected and uninfected cells were similar, which suggests that the virus does not possess a cidofovir-phosphorylating enzyme. Thus, drug resistance would be expected to be unrelated to phosphorylation. In contrast, compounds such as acyclovir and ganciclovir are phosphorylated by herpes simplex virus and/or human cytomegalovirus kinases, and drug resistance can occur via mutated viral enzymes that do not phosphorylate these compounds well (3, 8).
A more promising approach to understanding viral resistance to cidofovir was to study the poxvirus DNA polymerase. Experiments showed that cidofovir-PP was 8.5-fold less inhibitory to the cowpox-R (SF) DNA polymerase than it was to cowpox-WT polymerase. Other investigators have determined that human cytomegalovirus resistance to cidofovir was due to mutations in the viral DNA polymerase (29). Thus, it seems likely that orthopoxvirus resistance to cidofovir is due primarily to mutations in the viral DNA polymerase, resulting in a decreased sensitivity of the enzyme to inhibition by cidofovir-PP. The exact mutations in the cowpox and other orthopoxvirus DNA polymerases responsible for the drug resistance phenotype will need to be determined by gene sequencing. Mutations in the murine cytomegalovirus DNA polymerase gene that putatively conferred resistance to cidofovir have been reported (32).
Compared to WT viruses, the cowpox-R, monkeypox-R, and monkeypox-R (SF) viruses exhibited decreased abilities to replicate to high titers and to efficiently plaque in mouse 3T3 cells. However, cowpox-WT virus passaged 30 times in Vero 76 cells was not altered in its ability to replicate to high titers or to initially plaque in 3T3 cells. Thus, cell culturing alone did not seem to alter the replicative or cell binding properties of the virus. It is understandable how resistance to cidofovir (via a mutated viral DNA polymerase) could lead to viruses that are less fit in their ability to replicate to high titers in a particular cell line. But it seems unlikely that such a mutation would alter the ability of viruses to initially infect cells, since virus adsorption to cells is related to receptor binding rather than to viral DNA polymerase activity. The resistant viruses were all plaque purified, which could have led to the selection of variants that were less able to bind to 3T3 cells. Overall, these viruses contain defects resembling those of host range mutants.
There was a correlation between the reduced ability of the cowpox-R virus to initially infect and replicate to high titers in 3T3 cells and its very low virulence in mice. In contrast, the cowpox-R (SF) strain was very similar to the two cowpox-WT viruses in its replicative properties in 3T3 and Vero 76 cells. This resistant virus was also able to cause lethal infections in mice but required a high-titer challenge dose. Thus, in vivo attenuation of the virus occurred in a way that the present cell culture studies failed to detect or measure. Logically, attenuation should be linked to reduced replicative fitness and/or decreased cell receptor binding properties. Mouse lung cells may be less suitable hosts than 3T3 cells for the cowpox-R (SF) virus, but additional research is required to verify this.
The results of the mouse studies showed that animals infected with the cowpox-R (SF) virus were unsuccessfully treated with cidofovir, living only 1.3 to 1.5 days longer than placebo-treated animals. These effects were seen in healthy and immunodeficient mice. The efficacy of cidofovir in vivo was consistent with the reduced potency of cidofovir in vitro against the resistant virus. Although the impact of the drug in combating resistant virus infections was negligible, the low virulence of the CDV-R viruses makes them less of a threat to healthy hosts infected with lower virus challenge doses. Application of these results to human orthopoxvirus infections suggests the possibility that CDV-R viruses may be attenuated in vivo. However, the data obtained from these studies should be interpreted cautiously, since the virulence of the resistant cowpox viruses was studied only in mice, with no other animal species being investigated.
The development of cidofovir resistance often coincides with the appearance of poorly growing viruses in cell culture (26), yet one of the resistant monkeypox virus isolates actually replicated to higher titers in Vero 76 cells than did its WT counterpart. Thus, it may be important to determine the virulence of the CDV-R forms of monkeypox viruses in monkeys. The low availability of these animals coupled with other research priorities dictating their use prevented us from performing such studies, but they may be done in the future. Because of the close relatedness of monkeypox disease in humans to smallpox, monkeys infected with CDV-R monkeypox virus may be the best model for determining whether CDV-R viruses affecting humans are attenuated in vivo.
Acknowledgments
This research was supported by an appointment of D.F.S. to the Research Participation Program at the U.S. Army Medical Research Institute of Chemical Defense (USAMRICD) administered by the Oak Ridge Institute for Sciences and Education through an interagency agreement between the U.S. Department of Energy and USAMRICD and by contract NO1-AI-65291 from the Virology Branch, National Institute of Allergy and Infectious Diseases, National Institutes of Health.
REFERENCES
- 1.Altman, S., and L. S. Lerman. 1970. Kinetics and intermediates in the intracellular synthesis of bacteriophage T4 deoxyribonucleic acid. J. Mol. Biol. 50:235-261. [DOI] [PubMed] [Google Scholar]
- 2.Andrei, G., R. Snoeck, and E. De Clercq. 1997. Differential susceptibility of several drug-resistant strains of herpes simplex virus type 2 to various antiviral compounds. Antivir. Chem. Chemother. 8:457-461. [Google Scholar]
- 3.Biron, K. K. 1991. Ganciclovir-resistant human cytomegalovirus clinical isolates; resistance mechanisms and in vitro susceptibility to antiviral agents. Transplant. Proc. 23:162-167. [PubMed] [Google Scholar]
- 4.Bischofberger, N., M. J. M. Hitchcock, M. S. Chen, D. B. Barkhimer, K. C. Cundy, K. M. Kent, S. A. Lacy, W. A. Lee, Z.-H. Li, D. B. Mendel, D. F. Smee, and J. L. Smith. 1994. 1-[((S)-2-Hydroxy-2-oxo-1,4,2-dioxaphosphorinan-5-yl)methyl]cytosine, an intracellular prodrug for (S)-1-(3-hydroxy-2-phosphonylmethoxypropyl)cytosine with improved therapeutic index in vivo. Antimicrob. Agents Chemother. 38:2387-2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bray, M., M. Martinez, D. F. Smee, D. Kefauver, E. Thompson, and J. W. Huggins. 2000. Cidofovir (HPMPC) protects mice against lethal aerosol or intranasal cowpox virus challenge. J. Infect. Dis. 181:10-19. [DOI] [PubMed] [Google Scholar]
- 6.Breman, J. G., and D. A. Henderson. 1998. Poxvirus dilemmas—monkeypox, smallpox and biological terrorism. N. Engl. J. Med. 339:556-559. [DOI] [PubMed] [Google Scholar]
- 7.Cheng, Y.-C., and W. H. Prusoff. 1973. Relationship between the inhibition constant (Ki) and the concentration of inhibitor which causes 50 per cent inhibition (I50) of an enzymatic reaction. Biochem. Pharmacol. 22:3099-3108. [DOI] [PubMed] [Google Scholar]
- 8.Coen, D. M., P. A. Schaffer, P. A. Furman, P. M. Keller, and M. H. St. Clair. 1982. Biochemical and genetic analysis of acyclovir-resistant mutants of herpes simplex virus type 1. Am. J. Med. 73:351-360. [DOI] [PubMed] [Google Scholar]
- 9.De Clercq, E., A. Holý, and I. Rosenberg. 1989. Efficacy of phosphonylmethoxyalkyl derivatives of adenine in experimental herpes simplex virus and vaccinia virus infections in vivo. Antimicrob. Agents Chemother. 33:185-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Clercq, E., and J. A. Montgomery. 1983. Broad-spectrum antiviral activity of the carbocyclic analog of 3-deazaadenosine. Antivir. Res. 3:17-24. [DOI] [PubMed] [Google Scholar]
- 11.Franchetti, P., and M. Grifantini. 1999. Nucleoside and non-nucleoside IMP dehydrogenase inhibitors as antitumor and antiviral agents. Curr. Med. Chem. 6:599-614. [PubMed] [Google Scholar]
- 12.Heiner, G. G., N. Fatima, P. K. Russell, A. T. Haase, N. Ahmad, N. Mohammed, D. B. Thomas, T. M. Mack, M. M. Khan, G. L. Knatterud, R. L. Anthony, and F. R. McCrumb, Jr. 1971. Field trials of methisazone as a prophylactic agent against smallpox. Am. J. Epidemiol. 94:435-449. [DOI] [PubMed] [Google Scholar]
- 13.Heymann, D. L., M. Szczeniowski, and K. Esteves. 1998. Re-emergence of monkeypox in Africa: a review of the past six years. Br. Med. Bull. 54:693-702. [DOI] [PubMed] [Google Scholar]
- 14.Jabs, D. A., C. Enger, M. Forman, and J. P. Dunn for The Cytomegalovirus Retinitis and Viral Resistance Study Group. 1998. Incidence of foscarnet resistance and cidofovir resistance in patients treated for cytomegalovirus retinitis. Antimicrob. Agents Chemother. 42:2240-2244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kesson, A. M., J. K. Ferguson, W. D. Rawlinson, and A. L. Cunningham. 1997. Progressive vaccinia treated with ribavirin and vaccinia immune globulin. Clin. Infect. Dis. 25:911-914. [DOI] [PubMed] [Google Scholar]
- 16.Lurain, N. S., K. D. Thompson, E. W. Holmes, and G. S. Read. 1992. Point mutations in the DNA polymerase gene of human cytomegalovirus that result in resistance to antiviral agents. J. Virol. 66:7146-7152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meadows, K. P., S. K. Tyring, A. T. Pavia, and T. M. Rallis. 1997. Resolution of recalcitrant molluscum contagiosum virus lesions in human immunodeficiency virus-infected patients treated with cidofovir. Arch. Dermatol. 133:987-990. [PubMed] [Google Scholar]
- 18.Moss, B., and N. Cooper. Genetic evidence for vaccinia virus-encoded DNA polymerase: isolation of phosphonoacetate-resistant enzyme from the cytoplasm of cells infected with mutant virus. J. Virol. 43:673-678. [DOI] [PMC free article] [PubMed]
- 19.Munoz-Perez, M. A., A. Rodriguez-Pichardo, F. Camacho, and M. A. Colmenero. 1998. Dermatological findings correlated with CD4 lymphocyte counts in a prospective 3 year study of 1161 patients with human immunodeficiency virus disease predominantly acquired through intravenous drug abuse. Br. J. Dermatol. 139:33-39. [DOI] [PubMed] [Google Scholar]
- 19a.National Research Council. 1996. Guide for the care and use of laboratory animals, rev. ed. National Academy Press, Washington, D.C.
- 20.Neyts, J., and E. De Clercq. 1993. Efficacy of (S)-1-(3-hydroxy-2-phosphonylmethoxypropyl)cytosine for the treatment of lethal vaccinia virus infections in severe combined immune deficiency (SCID) mice. J. Med. Virol. 41:242-246. [DOI] [PubMed] [Google Scholar]
- 21.Okleberry, K. M., R. P. Warren, and D. F. Smee. 1997. Metabolism of ganciclovir and cidofovir in cells infected with drug-resistant and wild-type strains of murine cytomegalovirus. Antivir. Res. 35:83-90. [DOI] [PubMed] [Google Scholar]
- 22.Orent, W. 1998. Escape from Moscow. Sciences (New York) 38:26-31. [Google Scholar]
- 23.Robins, R. K., G. R. Revankar, P. A. McKernan, B. K. Murray, J. J. Kirsi, and J. A. North. 1986. The importance of IMP dehydrogenase inhibition in the broad spectrum antiviral activity of ribavirin and selenazofurin. Adv. Enzyme Regul. 24:29-43. [DOI] [PubMed] [Google Scholar]
- 24.Smee, D. F., K. W. Bailey, and R. W. Sidwell. 2000. Intranasal treatment of cowpox virus respiratory infections in mice with cidofovir. Antivir. Res. 47:171-177. [DOI] [PubMed] [Google Scholar]
- 25.Smee, D. F., K. W. Bailey, and R. W. Sidwell. 2001. Treatment of lethal vaccinia virus respiratory infections in mice with cidofovir. Antivir. Chem. Chemother. 12:71-76. [DOI] [PubMed] [Google Scholar]
- 26.Smee, D. F., B. B. Barnett, R. W. Sidwell, E. J. Reist, and A. Holy. 1995. Antiviral activities of nucleosides and nucleotides against wild-type and drug-resistant strains of murine cytomegalovirus. Antivir. Res. 26:1-9. [DOI] [PubMed] [Google Scholar]
- 27.Smee, D. F., and J. W. Huggins. 1999. Mode of action of ribavirin against cowpox and monkeypox viruses. Antivir. Res. 41:A52. [Google Scholar]
- 28.Smee, D. F., J. L. B. Morris, J. A. Leonhardt, J. R. Mead, A. Holy, and R. W. Sidwell. 1992. Treatment of murine cytomegalovirus infections in severe combined immunodeficient mice with ganciclovir, (S)-1-[3-hydroxy-2-(phosphonylmethoxy)propyl]cytosine, interferon, and bropirimine. Antimicrob. Agents Chemother. 36:1837-1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sullivan, V., K. K. Biron, C. Talarico, S. C. Stanat, M. Davis, L. M. Pozzi, and D. M. Coen. 1993. A point mutation in the human cytomegalovirus DNA polymerase gene confers resistance to ganciclovir and phosphonylmethoxyalkyl derivatives. Antimicrob. Agents Chemother. 37:19-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taddie, J. A., and P. Traktman. 1993. Genetic characterization of the vaccinia virus DNA polymerase: cytosine arabinoside resistance requires a variable lesion conferring phosphonoacetate resistance in conjunction with an invariant mutation localized to the 3′-5′ exonuclease domain. J. Virol. 67:4323-4336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tatarowicz, W. A., N. S. Lurain, and K. D. Thompson. 1992. A ganciclovir-resistant clinical isolate of human cytomegalovirus exhibiting cross-resistance to other DNA polymerase inhibitors. J. Infect. Dis. 166:904-907. [DOI] [PubMed] [Google Scholar]
- 32.Tatti, K. M., H. Stang, D. Barnard, D. Smee, and R. F. Schinazi. 1998. Mutations occur in highly conserved domains of murine cytomegalovirus DNA polymerase in cidofovir- and lobucavir-resistant strains. Antivir. Res. 37:A70. [Google Scholar]
- 33.Toro, J. R., L. V. Wood, N. K. Patel, and M. L. Turner. 2000. Topical cidofovir: a novel treatment for recalcitrant molluscum contagiosum in children infected with human immunodeficiency virus 1. Arch. Dermatol. 136:983-985. [DOI] [PubMed] [Google Scholar]
- 34.Xiong, X., J. L. Smith, C. Kim, E. Huang, and M. S. Chen. 1996. Kinetic analysis of the interaction of cidofovir diphosphate with human cytomegalovirus DNA polymerase. Biochem. Pharmacol. 51:1563-1567. [DOI] [PubMed] [Google Scholar]