Abstract
Two 8-methoxy nonfluorinated quinolones (NFQs), PGE 9262932 and PGE 9509924, were tested against contemporary clinical isolates of Staphylococcus aureus (n = 122) and Streptococcus pneumoniae (n = 69) with genetically defined quinolone resistance-determining regions (QRDRs). For S. aureus isolates with wild-type (WT) sequences at the QRDRs, the NFQs demonstrated activities 4- to 32-fold more potent (MICs at which 90% of isolates are inhibited [MIC90s], 0.03 μg/ml) than those of moxifloxacin (MIC90, 0.12 μg/ml), gatifloxacin (MIC90, 0.25 μg/ml), levofloxacin (MIC90, 0.25 μg/ml), and ciprofloxacin (MIC90, 1 μg/ml). Against S. pneumoniae isolates with WT sequences at gyrA and parC, the NFQs PGE 9262932 (MIC90, 0.03 μg/ml) and PGE 9509924 (MIC90, 0.12 μg/ml) were 8- to 64-fold and 2- to 16-fold more potent, respectively, than moxifloxacin (MIC90, 0.25 μg/ml), gatifloxacin (MIC90, 0.5 μg/ml), levofloxacin (MIC90, 2 μg/ml), and ciprofloxacin (MIC90, 2 μg/ml). The MICs of all agents were elevated for S. aureus isolates with alterations in GyrA (Glu88Lys or Ser84Leu) and GrlA (Ser80Phe) and S. pneumoniae isolates with alterations in GyrA (Ser81Phe or Ser81Tyr) and ParC (Ser79Phe or Lys137Asn). Fluoroquinolone MICs for S. aureus strains with double alterations in GyrA combined with double alterations in GrlA were ≥32 μg/ml, whereas the MICs of the NFQs for strains with these double alterations were 4 to 8 μg/ml. The PGE 9262932 and PGE 9509924 MICs for the S. pneumoniae isolates did not exceed 0.5 and 1 μg/ml, respectively, even for isolates with GyrA (Ser81Phe) and ParC (Ser79Phe) alterations, for which levofloxacin MICs were >16 μg/ml. No difference in the frequency of selection of mutations (<10−8 at four times the MIC) in wild-type or first-step mutant isolates of S. aureus or S. pneumoniae was detected for the two NFQs. On the basis of their in vitro activities, these NFQ agents show potential for the treatment of infections caused by isolates resistant to currently available fluoroquinolones.
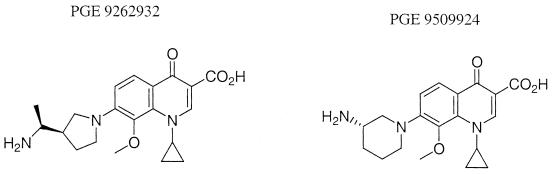
Recently, a series of 8-methoxy nonfluorinated quinolones (NFQs) have been developed by Procter and Gamble Pharmaceuticals (Mason, Ohio). NFQs lack a position-6 fluorine on their quinolone nucleus, differentiating them from fluorinated quinolones such as ciprofloxacin, levofloxacin, gatifloxacin, and moxifloxacin. Two NFQs, PGE 9262932 and PGE 9509924 (Fig. 1), have been shown to possess high in vitro activities against Staphylococcus aureus and Streptococcus pneumoniae, including multidrug-resistant isolates (1, 19, 20; D. F. Sahm, A. Staples, I. Critchley, C. Thornsberry, K. Murfitt, and D. Mayfield, Abstr. 40th Intersci. Conf. Antimicrob. Agents. Chemother., abstr. F-1509, 2000).
FIG. 1.
Chemical structures of the NFQs PGE 9263932 and PGE 9509924.
Resistance to fluoroquinolones has been demonstrated to be due primarily to amino acid substitutions in the quinolone resistance-determining regions (QRDRs) of topoisomerase IV (S. aureus, GrlA and GrlB; S. pneumoniae, ParC and ParE) and DNA gyrase (S. aureus, GyrA and GyrB; S. pneumoniae, GyrA and GyrB) (4, 7, 8, 10, 14, 16, 21, 22, 23, 24). The activities of hydrophilic fluoroquinolones such as ciprofloxacin can also be decreased by their efflux from cells (6, 13). To further our understanding of the activities and potential clinical utilities of NFQs, we determined the activities of PGE 9262932, PGE 9509924, and the comparator fluoroquinolones ciprofloxacin, levofloxacin (which targets GrlA and ParC), moxifloxacin, and gatifloxacin (which targets GyrA) against a recent collection of clinical isolates of S. aureus and S. pneumoniae that had been genetically defined with respect to substitutions in their QRDRs. Four isolates of Staphylococcus epidermidis for which NFQ MICs were elevated were also evaluated to provide a preliminary evaluation of resistance in this species. We also determined the frequencies of selection of mutations in isolates of S. aureus and S. pneumoniae that did not possess GyrA or GrlA-ParC alterations and isolates of both species harboring first-step mutations in either GyrA or GrlA-ParC.
MATERIALS AND METHODS
Isolates studied.
Clinical isolates of S. aureus (n = 116) and S. pneumoniae (n = 69) collected in Europe between 1997 and 2000 (8, 21) and six clinical isolates of S. aureus and four clinical isolates of Staphylococcus epidermidis collected in the United States during 1999 were studied. U.S. staphylococcal isolates were included specifically since the MICs (≥1 μg/ml) of both PGE 9262932 and PGE 9509924 for these isolates were elevated (Focus Technologies, data on file; Sahm et al. 40th ICAAC).
QRDR DNA sequencing.
Sequencing of the QRDR DNAs of the 116 isolates of S. aureus (with gyrA, gyrB, grlA, and grlB mutations) and 69 isolates of S. pneumoniae (with gyrA, gyrB, parC, and parE mutations) collected in Europe was performed by standard methodologies and with standard primer sets, which have been reported previously (8, 21). This group of isolates comprised isolates with a variety of QRDR genotypes, including isolates with wild-type sequences at all four QRDRs and isolates with various putative amino acid alterations known to confer resistance to fluoroquinolones. For this study, wild-type isolates were defined as clinical isolates with no detectable amino acid alterations in their QRDRs. The U.S. staphylococcal isolates studied were selected because the NFQ MICs for the isolates were elevated. All four QRDRs of these isolates were sequenced as described previously (21) to locate mutational changes that may reduce susceptibility to NFQs. For S. epidermidis isolates, only gyrA was sequenced with S. aureus-specific primers (21), as homologs of gyrB, grlA, and grlB have not previously been characterized in this species.
Antimicrobial susceptibility testing.
The susceptibilities of all study isolates to extended-range dilutions of PGE 9262932, PGE 9509924, moxifloxacin, gatifloxacin, levofloxacin, and ciprofloxacin were tested by the broth microdilution method defined by NCCLS (11).
Mutation selection frequencies.
The mutation selection frequencies for both NFQs were determined by using five isolates of S. aureus with wild-type sequences at GyrA and GrlA and five isolates of S. pneumoniae with wild-type sequences at GyrA and ParC. Mutation selection frequencies were also determined for five isolates of S. aureus with a single amino acid alteration in either GyrA or GrlA and five isolates of S. pneumoniae with a single amino acid alteration in either GyrA or ParC.
Each of the 20 isolates was cultured overnight at 35°C on 5% sheep blood agar and resuspended in sterile saline to an optical density at 650 nm of 0.9 to 1.0. This produced suspensions of approximately 1010 CFU/ml (controlled by undertaking viable counts); 100-μl aliquots of each suspension were immediately spread onto a series of Mueller-Hinton agar plates containing PGE 9262932, PGE 9509924, ciprofloxacin, or moxifloxacin. For each agent tested, the plates contained concentrations of two, four, or eight times the MIC for each isolate, as determined by broth microdilution (11). Mueller-Hinton agar plates were supplemented with 5% lysed horse blood for S. pneumoniae. The plates were incubated for 48 h at 35°C and were subsequently examined for growth. Up to 10 mutant colonies per plate were reinoculated onto plates containing the identical antimicrobial concentration to confirm their phenotype of resistance. Nonreproducible mutants were not included in the mutation frequency calculations. When colony counts exceeded 10 and not all 10 colonies selected for reculture grew, colony counts were adjusted proportionately. Mutation selection frequencies were calculated as the number of confirmed resistant colonies divided by the original inoculum. For plates that generated no mutants, the frequency was calculated as <1 divided by the original inoculum.
RESULTS
In vitro activities of PGE 9262932 and PGE 9509924.
The distributions of the MICs of PGE 9262932, PGE 9509924, and all fluoroquinolones tested for S. aureus and S. pneumoniae are shown in Table 1. PGE 9262932 and PGE 9509924 had the lowest MICs at which 90% of isolates were inhibited (MIC90s) for both S. aureus and S. pneumoniae (0.5 and 1 μg/ml, respectively, for PGE 9262932 and 0.25 and 0.5 μg/ml, respectively, for PGE 9509924). These MIC90s were severalfold lower than those of the other fluoroquinolones tested. This was especially so for the MIC90s of PGE 9262932 for the pneumococcal isolates.
TABLE 1.
Distribution of MICs of PGE 9262932, PGE 9509924, and comparative fluoroquinolones for 122 isolates of S. aureus and 69 isolates of S. pneumoniae
| Organism and quinolone | No. of isolates for which the MIC (μg/ml) wasa:
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤0.008 | 0.015 | 0.03 | 0.06 | 0.12 | 0.25 | 0.5 | 1 | 2 | 4 | 8 | 16 | ≥32 | |
| S. aureus | |||||||||||||
| PGE 9262932 | 6 | 19 | 15 | 9 | 18 | 33 | 10 | 4 | 4 | 3 | 1 | ||
| PGE 9509924 | 19 | 18 | 10 | 13 | 30 | 19 | 5 | 4 | 2 | 2 | |||
| Moxifloxacin | 26 | 18 | 2 | 17 | 46 | 6 | 1 | 2 | 1 | 3 | |||
| Gatifloxacin | 15 | 21 | 9 | 13 | 40 | 14 | 3 | 2 | 1 | 4 | |||
| Levofloxacin | 7 | 23 | 9 | 6 | 2 | 9 | 29 | 21 | 10 | 6 | |||
| Ciprofloxacin | 11 | 18 | 7 | 5 | 5 | 5 | 34 | 37 | |||||
| S. pneumoniae | |||||||||||||
| PGE 9262932 | 18 | 9 | 11 | 9 | 12 | 9 | 1 | ||||||
| PGE 9509924 | 2 | 18 | 9 | 10 | 13 | 11 | 6 | ||||||
| Moxifloxacin | 2 | 26 | 12 | 3 | 10 | 14 | 2 | ||||||
| Gatifloxacin | 1 | 3 | 25 | 10 | 2 | 10 | 10 | 6 | 2 | ||||
| Levofloxacin | 1 | 11 | 21 | 6 | 8 | 12 | 6 | 4 | |||||
| Ciprofloxacin | 1 | 8 | 17 | 12 | 7 | 8 | 10 | 6 | |||||
MIC90s (bold) and MIC50s (italic) are indicated. The available NCCLS susceptibility breakpoints are as follows: for S. aureus, ≤1 μg/ml for ciprofloxacin and ≤2 μg/ml for levofloxacin and gatifloxacin; for S. pneumoniae, ≤2 μg/ml for levofloxacin and ≤1 μg/ml for gatifloxacin and moxifloxacin (12).
The activities of PGE 9262932, PGE 9509924, and the fluoroquinolones tested against S. aureus isolates with respect to their GyrA, GyrB, GrlA, and GrlB QRDR alterations are provided in Table 2. Combinations of mutations that did not significantly affect susceptibility compared to the susceptibilities of the wild-type strains but that were detected in only one strain are not included in Table 2 (e.g., the Ser80Phe alteration alone in GrlA, the Glu88Lys alteration alone in alone in GyrA, and the Ser112Arg alteration alone in GyrA). The MIC90s of PGE 9262932 and PGE 9509924 for isolates with wild-type sequences at all four QRDRs were 0.03 μg/ml for both compounds, 4- to 32-fold lower than the MIC90s of the other fluoroquinolones tested. Despite the very high in vitro activities of the NFQs, elevations in the MIC distributions were observed for all agents, as isolates with increased numbers of amino acid alterations in GyrA and GrlA were tested. The ranges of MICs of the NFQs for S. aureus isolates with concurrent single alterations in GyrA (Ser84Leu) combined with single or multiple alterations in GrlA, including Ser80Phe, were 0.12 to 2 μg/ml (modal MIC, 0.5 μg/ml). This compares with an MIC range of ≤0.008 to 0.12 μg/ml (modal MIC, 0.15 μg/ml) for wild-type isolates. The highest MICs of the NFQs (2 to 8 μg/ml) were recorded for isolates with double alterations in GrlA (Ser80Phe or Ser80Tyr with Glu84Gly or Glu84Lys) in combination with single or double alterations in GyrA (Ser84Leu alone or with Ser85Pro or Glu88Lys). The effect of alterations in GyrB and GrlB on NFQ activity appeared to be insignificant.
TABLE 2.
Distribution of MICs of PGE 9262932, PGE 9509924, and comparator fluoroquinolones for 122 isolates of S. aureus with no mutations (wild type) in the four QRDRs or with single mutations or combinations of mutations within the QRDRs of gyrA and grlA
| Amino acid alterations | No. of isolates | Quinolone | No. of isolates for which the MIC (μg/ml) was:
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GyrA | GrlA | ≤0.008 | 0.015 | 0.03 | 0.06 | 0.12 | 0.25 | 0.5 | 1 | 2 | 4 | 8 | 16 | ≥32 | ||
| None | None | 36a | PGE 9262932 | 6 | 17 | 11 | 2 | |||||||||
| PGE 9509924 | 18 | 15 | 2 | 1 | ||||||||||||
| Moxifloxacin | 26 | 9 | 1 | |||||||||||||
| Gatifloxacin | 15 | 16 | 4 | 1 | ||||||||||||
| Levofloxacin | 7 | 21 | 6 | 2 | ||||||||||||
| Ciprofloxacin | 11 | 15 | 6 | 3 | 1 | |||||||||||
| Ser84Leu | Ser80Phe | 49b | PGE 9262932 | 17 | 25 | 6 | 1 | |||||||||
| PGE 9509924 | 10 | 25 | 13 | 1 | ||||||||||||
| Moxifloxacin | 14 | 33 | 1 | 1 | ||||||||||||
| Gatifloxacin | 9 | 32 | 6 | 1 | 1 | |||||||||||
| Levofloxacin | 1 | 5 | 22 | 16 | 4 | 1 | ||||||||||
| Ciprofloxacin | 4 | 23 | 22 | |||||||||||||
| Glu88Lys | Ser80Phe | 12a | PGE 9262932 | 1 | 2 | 1 | 6 | 2 | ||||||||
| PGE 9509924 | 1 | 2 | 1 | 3 | 5 | |||||||||||
| Moxifloxacin | 3 | 9 | ||||||||||||||
| Gatifloxacin | 3 | 7 | 2 | |||||||||||||
| Levofloxacin | 4 | 7 | 1 | |||||||||||||
| Ciprofloxacin | 1 | 9 | 2 | |||||||||||||
| Glu88Lys | Ser80Phe, Glu84Val | 4a | PGE 9262932 | 1 | 2 | 1 | ||||||||||
| PGE 9509924 | 1 | 2 | 1 | |||||||||||||
| Moxifloxacin | 1 | 2 | 1 | |||||||||||||
| Gatifloxacin | 2 | 1 | 1 | |||||||||||||
| Levofloxacin | 1 | 3 | ||||||||||||||
| Ciprofloxacin | 4 | |||||||||||||||
| Ser84Leu | Ser80Phe, Ala48Thr | 4c | PGE 9262932 | 1 | 2 | 1 | ||||||||||
| PGE 9509924 | 1 | 2 | 1 | |||||||||||||
| Moxifloxacin | 3 | 1 | ||||||||||||||
| Gatifloxacin | 1 | 2 | 1 | |||||||||||||
| Levofloxacin | 1 | 3 | ||||||||||||||
| Ciprofloxacin | 1 | 3 | ||||||||||||||
| Ser84Lys | Ser80Phe, Val41Gly, Ile45Met | 1d | PGE 9262932 | 1 | ||||||||||||
| PGE 9509924 | 1 | |||||||||||||||
| Moxifloxacin | 1 | |||||||||||||||
| Gatifloxacin | 1 | |||||||||||||||
| Levofloxacin | 1 | |||||||||||||||
| Ciprofloxacin | 1 | |||||||||||||||
| Ser84Leu, Gly106Asp | Ser80Phe | 1a | PGE 9262932 | 1 | ||||||||||||
| PGE 9509924 | 1 | |||||||||||||||
| Moxifloxacin | 1 | |||||||||||||||
| Gatifloxacin | 1 | |||||||||||||||
| Levofloxacin | 1 | |||||||||||||||
| Ciprofloxacin | 1 | |||||||||||||||
| Ser84Leu | Ser80Phe, Glu84Lys | 1d | PGE 9262932 | 1 | ||||||||||||
| PGE 9509924 | 1 | |||||||||||||||
| Moxifloxacin | 1 | |||||||||||||||
| Gatifloxacin | 1 | |||||||||||||||
| Levofloxacin | 1 | |||||||||||||||
| Ciprofloxacin | 1 | |||||||||||||||
| Ser84Leu, Ser85Pro | Ser80Phe, Glu84Gly | 1a | PGE 9262932 | 1 | ||||||||||||
| PGE 9509924 | 1 | |||||||||||||||
| Moxifloxacin | 1 | |||||||||||||||
| Gatifloxacin | 1 | |||||||||||||||
| Levofloxacin | 1 | |||||||||||||||
| Ciprofloxacin | 1 | |||||||||||||||
| Ser84Leu, Ser85Pro | Ser80Phe, Glu84Lys | 1a | PGE 9262932 | 1 | ||||||||||||
| PGE 9509924 | 1 | |||||||||||||||
| Moxifloxacin | 1 | |||||||||||||||
| Gatifloxacin | 1 | |||||||||||||||
| Levofloxacin | 1 | |||||||||||||||
| Ciprofloxacin | 1 | |||||||||||||||
| Ser84Leu, Glu88Lys | Ser80Tyr, Glu84Gly | 2a | PGE 9262932 | 2 | ||||||||||||
| PGE 9509924 | 1 | 1 | ||||||||||||||
| Moxifloxacin | 1 | 1 | ||||||||||||||
| Gatifloxacin | 2 | |||||||||||||||
| Levofloxacin | 2 | |||||||||||||||
| Ciprofloxacin | 2 | |||||||||||||||
All isolates had wild-type sequences at GyrB and GrlB.
Forty-seven isolates had wild-type sequences at GyrB and GrlB, one isolate had the wild-type sequence at GyrB and the Asp432Gly alteration in GrlB, and one isolate had the wild-type sequence at GyrB and the Asp432Val alteration in GrlB.
Three isolates had wild-type sequences at GyrB and GrlB, and one isolate had the wild-type sequence at GyrB and the Pro451Ser alteration in GrlB.
All isolates had the wild-type sequence at GyrB and the Glu422Asp alteration in GrlB.
The distributions of the MICs of PGE 9262932, PGE 9509924, and the other fluoroquinolones tested for S. pneumoniae isolates with respect to their GyrA, GyrB, ParC, and ParE QRDR alterations are provided in Table 3. As described above for Table 2, combinations of mutations that did not significantly affect susceptibility compared to the susceptibilities of the wild-type strains are not included in Table 3 (e.g., Arg95Cys alone in ParC). Multiple mutations (e.g., alterations in GyrA [Ser81Phe] in combination with alterations in ParC [Asp78Asn or Lys137Asn]) detected in only one isolate are also not included in Table 3. The ranges of MICs of PGE 9262932 and PGE 9509924 for isolates with wild-type sequences at all four QRDRs were ≤0.008 to 0.03 and 0.03 to 0.12 μg/ml, respectively. These were similar to the MIC ranges for isolates with wild-type sequences at GyrA and ParC but with alterations at ParE and GyrB. The MIC90s of PGE 9262932 and PGE 9509924 for all isolates with wild-type sequences at both GyrA and ParC (n = 29) were 8- to 64-fold and 2- to 16-fold lower, respectively, than those of the other fluoroquinolones tested. When the key mutations known to reduce the activities of fluoroquinolones were considered, the MICs for isolates with the Ser81Tyr or Ser81Phe alteration in GyrA alone (n = 5) were higher than those for wild-type strains, although the MICs of PGE 9262932 were still low (0.06 to 0.12 μg/ml) compared to those of levofloxacin (4 to 8 μg/ml). Isolates for which the NFQ and fluoroquinolone MICs were the highest tended to carry a Ser81Phe or Ser81Tyr alteration in GyrA in combination with a Ser79Phe alteration in ParC (n = 20). As such, the NFQs demonstrated more potent activities against isolates with key mutations that confer fluoroquinolone resistance than the other fluoroquinolones studied. Other mutations in parC and parE may appear to be significant in affecting the MICs of NFQ compounds for mutant strains compared to those for the wild-type strains, but this is difficult to verify without studying isogenic strains.
TABLE 3.
Distribution of MICs of PGE 9262932, PGE 9509924, and comparator fluoroquinolones for 69 isolates of S. pneumoniae with no mutations (wild type) in the four QRDRs or with a single mutation or combinations of mutations within the QRDRs of gyrA and parC
| Amino acid alterations | No. of isolates | Quinolone | No. of isolates for which the MIC (μg/ml) was:
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GyrA | ParC | ≤0.008 | 0.015 | 0.03 | 0.06 | 0.12 | 0.25 | 0.5 | 1 | 2 | 4 | 8 | 16 | ≥32 | ||
| None | None | 8a | PGE 9262932 | 3 | 3 | 2 | ||||||||||
| PGE 9509924 | 4 | 2 | 2 | |||||||||||||
| Moxifloxacin | 1 | 3 | 2 | 2 | ||||||||||||
| Gatifloxacin | 1 | 5 | 2 | |||||||||||||
| Levofloxacin | 1 | 5 | 2 | |||||||||||||
| Ciprofloxacin | 1 | 4 | 2 | 1 | ||||||||||||
| None | None | 21b | PGE 9262932 | 11 | 5 | 5 | ||||||||||
| PGE 9509924 | 1 | 11 | 5 | 3 | 1 | |||||||||||
| Moxifloxacin | 1 | 14 | 6 | |||||||||||||
| Gatifloxacin | 1 | 2 | 14 | 4 | ||||||||||||
| Levofloxacin | 1 | 5 | 12 | 3 | ||||||||||||
| Ciprofloxacin | 1 | 5 | 10 | 5 | ||||||||||||
| None | Lys137Asn | 6c | PGE 9262932 | 3 | 1 | 2 | ||||||||||
| PGE 9509924 | 1 | 2 | 2 | 1 | ||||||||||||
| Moxifloxacin | 6 | |||||||||||||||
| Gatifloxacin | 6 | |||||||||||||||
| Levofloxacin | 4 | 2 | ||||||||||||||
| Ciprofloxacin | 1 | 3 | 2 | |||||||||||||
| None | Ser79Phe | 2d | PGE 9262932 | 1 | 1 | |||||||||||
| PGE 9509924 | 1 | 1 | ||||||||||||||
| Moxifloxacin | 2 | |||||||||||||||
| Gatifloxacin | 1 | 1 | ||||||||||||||
| Levofloxacin | 1 | 1 | ||||||||||||||
| Ciprofloxacin | 1 | 1 | ||||||||||||||
| Ser81Tyr | None | 3e | PGE 9262932 | 3 | ||||||||||||
| PGE 9509924 | 2 | 1 | ||||||||||||||
| Moxifloxacin | 1 | 2 | ||||||||||||||
| Gatifloxacin | 1 | 1 | 1 | |||||||||||||
| Levofloxacin | 3 | |||||||||||||||
| Ciprofloxacin | 1 | 1 | 1 | |||||||||||||
| Ser81Phe | None | 2d | PGE 9262932 | 1 | 1 | |||||||||||
| PGE 9509924 | 1 | 1 | ||||||||||||||
| Moxifloxacin | 1 | 1 | ||||||||||||||
| Gatifloxacin | 1 | 1 | ||||||||||||||
| Levofloxacin | 1 | 1 | ||||||||||||||
| Ciprofloxacin | 1 | 1 | ||||||||||||||
| Ser81Phe | Ser79Phe | 16f | PGE 9262932 | 2 | 7 | 6 | 1 | |||||||||
| PGE 9509924 | 1 | 4 | 6 | 5 | ||||||||||||
| Moxifloxacin | 6 | 9 | 1 | |||||||||||||
| Gatifloxacin | 4 | 8 | 4 | |||||||||||||
| Levofloxacin | 8 | 4 | 4 | |||||||||||||
| Ciprofloxacin | 4 | 6 | 6 | |||||||||||||
| Ser81Phe | Ser79Phe, Lys137Asn | 4a | PGE 9262932 | 2 | 2 | |||||||||||
| PGE 9509924 | 2 | 2 | ||||||||||||||
| Moxifloxacin | 3 | 1 | ||||||||||||||
| Gatifloxacin | 2 | 2 | ||||||||||||||
| Levofloxacin | 2 | 2 | ||||||||||||||
| Ciprofloxacin | 2 | 2 | ||||||||||||||
| Ser81Phe | Asp83Asn, Lys137Asn | 2a | PGE 9262932 | 1 | 1 | |||||||||||
| PGE 9509924 | 1 | 1 | ||||||||||||||
| Moxifloxacin | 1 | 1 | ||||||||||||||
| Gatifloxacin | 2 | |||||||||||||||
| Levofloxacin | 2 | |||||||||||||||
| Ciprofloxacin | 2 | |||||||||||||||
All isolates had the wild-type sequences GyrB and ParE.
Twelve isolates had the wild-type sequence at GyrB and the Ile460Val alteration in ParE, one isolate had the Arg541Lys alteration in GyrB and the Ile460Val alteration in ParE, one isolate had the Ala639Gln alteration in GyrB and the Ile460Val alteration in ParE, five isolates had the wild-type sequence at GyrB and the Lys466Met alteration in ParE, one isolate had the Ala639Gln alteration in GyrB and the wild-type sequence at ParE, and one isolate had the Ala538Ser alteration in GyrB and the wild-type sequence at ParE.
Three isolates had wild-type sequences at GyrB and ParE, two isolates had the wild-type sequence at GyrB and the Ile460Val alteration in ParE, and the isolate had the Ala639Gln alteration in GyrB and the wild-type sequence at ParE.
One isolate had wild-type sequences at GyrB and ParE, and one isolate had the wild-type sequence at GyrB and the Ile460Val alteration in ParE.
Two isolates had wild-type sequences at GyrB and ParE, and one isolate had the wild-type sequence at GyrB and the Ile460Val alteration in ParE.
Seven isolates had wild-type sequences at GyrB and ParE, five isolates had the wild-type sequences at GyrB and the Ile460Val alteration in ParE, one isolate had the wild-type sequence at GyrB and the Pro454Ser alteration in at ParE, one isolate had the Ala639Gln alteration in GyrB and the wild-type sequence at ParE, one isolate had the Arg541Lys alteration in GyrB and the Ile460Val alteration in ParE, and one isolate had the Ala639Gln alteration in GyrB and the Ile460Val alteration in ParE.
The MIC ranges for the four isolates of S. epidermidis were 1 to 4 μg/ml for PGE 9262932, 2 to 8 μg/ml for PGE 9509924, and ≥32 μg/ml for moxifloxacin, gatifloxacin, levofloxacin, and ciprofloxacin (data not shown). Each of the four S. epidermidis isolates sequenced demonstrated identical triple alterations in GyrA (Ser63Pro, Ser84Phe, Gly88Lys). The gyrB, grlA, and grlB QRDRs were not sequenced for S. epidermidis isolates.
Mutation selection frequency.
No S. aureus mutants from wild-type isolates or first-step mutant isolates (i.e., isolates with one preexisting mutation) were recovered after exposure to either of the NFQs at four times their MICs. Mutations in wild-type S. aureus strains were selected at rates of <5.1 × 10−9 to 4.3 × 10−7 when they were exposed to PGE 9262932 at a concentration of two times the MIC. PGE 9262932 at two times the MIC selected mutations in first-step mutants of S. aureus at rates of <5.6 × 10−9 to 1.6 × 10−7, while no mutations were detected when this compound was used at four times its MIC. For PGE 9509924 at two times its MIC, mutation selection frequencies were <8.3 × 10−9 to 1.9 × 10−7 for wild-type S. aureus and <7.5 × 10−9 to 8.8 × 10−7 for first-step mutants. No mutations were detected with PGE 9509924 at four times its MIC. Mutation selection frequencies for wild-type strains used as controls were ≥4 × 10−6 and ≥6 × 10−6 for ciprofloxacin and moxifloxacin at two times their MICs, respectively, and 2.2 × 10−6 to 2.3 × 10−8 and <1.3 × 10−8 for ciprofloxacin and moxifloxacin at four times their MICs, respectively. Preliminary studies in which the QRDRs in mutants from wild-type or first-step mutants selected with PGE 9262932 or PGE 9509924 were sequenced detected only one alteration in GyrA (Glu88Lys), and this occurred in an isolate that was already harboring a GrlA (Ser80Phe) alteration and that was selected with PGE 9509924. The MICs for the mutants were confirmed by retesting.
For S. pneumoniae, no mutants were detected with either of the NFQs at four and eight times their MICs. The mutation rates for PGE 9262932 at two times the MIC were <6.6 × 10−9 to 3.1 × 10−8 for wild-type S. pneumoniae strains and were undetectable for first-step mutants. The mutation rates for PGE 9509924 at two times the MIC were <2.5 × 10−9 to 3.4 × 10−8 for wild-type S. pneumoniae strains and were undetectable for first-step mutants. The mutation selection frequencies for wild-type strains obtained with ciprofloxacin and moxifloxacin were not different from those obtained with the NFQs. Importantly for either species, no increase in the mutation selection frequency was detected for isolates with first-step mutations. Preliminary studies in which the QRDRs in mutants from wild-type strains selected on PGE 9262932 were sequenced detected two isolates with alterations GyrA (Glu85Lys), GyrB (Leu466Ile), and ParE (Asp435Asn). Similarly, two isolates selected from a wild-type strain on PGE 9509924 with alterations in GyrA (Glu85Lys or Ser81Tyr) and ParE (Ile460Val) were detected. For both species, the mutations raised the MICs of all agents tested. The MICs for the mutants were confirmed by retesting. These preliminary data suggest that NFQs target gyrA, in addition to parE.
DISCUSSION
Against S. aureus and S. pneumoniae, the NFQs demonstrated in vitro activities superior to those of the most active fluoroquinolones marketed to date, including moxifloxacin, gatifloxacin, and levofloxacin. This was true for both the fluoroquinolone-resistant and the fluoroquinolone-susceptible strains tested. Although wild-type isolates of S. aureus and S. pneumoniae were not isogenic parent strains of strains harboring mutations in QRDRs, they enabled the study of the possible effects of mutations on drug activity. Alone, no alteration in GrlB or ParE significantly raised the MICs of any agent tested for S. aureus or S. pneumoniae, as the MIC ranges for isolates with alterations in one of these two proteins were similar to those for wild-type isolates (data not shown). MIC ranges for first-step mutants of S. aureus and S. pneumoniae (i.e., isolates with single alterations in either GyrA or GrlA-ParC) generally overlapped those for the wild-type isolates, although the NFQ and fluoroquinolone MICs for some isolates of S. pneumoniae with single alterations, in particular, alterations in ParC (Ser79Phe) or GyrA (Ser81Phe or Ser81Tyr), were higher than those for wild-type isolates. It is unlikely that susceptibility testing alone would be able to detect first-step mutations in S. pneumoniae or S. aureus (9). Substitutions in GyrA (Ser84Leu or Ser84Lys) and GrlA (Ser80Phe) in S. aureus and GyrA (Ser81Phe or Ser81Tyr) and ParC (Ser79Phe) in S. pneumoniae elevated the NFQ MICs outside the ranges recorded for wild-type isolates. Other mutations encoding alterations in GrlA in S. aureus or ParC in S. pneumoniae had similar effects, but the effects of these mutations were not as pronounced as the effects of the Ser80Phe alteration in GrlA or the Ser79Phe alteration in ParC.
For both species, the highest NFQ MICs and the highest MICs of the other fluoroquinolones tested were recorded for isolates harboring amino acid substitutions in both GyrA and GrlA or ParC; however, the NFQ MICs remained lower. Exceptions to this generalization can be noted for isolates of S. aureus carrying single alterations in GyrA (Gly88Lys or Ser84Leu) or this alteration in combination with an alteration in GrlA, such as Ser80Phe. The NFQs, moxifloxacin, and gatifloxacin were equally active against these isolates. Preliminary data derived from the characterization of mutants selected by using NFQs showed that alterations occur more frequently in GyrA than in GrlA or ParC, suggesting that NFQs may preferentially target GyrA, which is similar to the case for moxifloxacin and gatifloxacin. This requires further study. Independent of a preferential target, all quinolones were negatively affected by mutations in the QRDRs of DNA gyrase and topisomerase IV (8, 21) Any quinolone compound which has a greater tendency to select for single- and/or double-step mutations may negatively affect the utilities of all quinolones. Thus, it is important to define the mutation selection frequency for any new quinolone. This study demonstrated that, for both S. aureus and S. pneumoniae, the NFQs selected first-step mutants at rates equal to or less than those at which moxifloxacin and ciprofloxacin selected such mutants (3). Importantly, the NFQs also had an equally low tendency to select for second-step mutants. This is in contrast to the findings presented in a previous report, which noted higher mutation rates for other fluorinated quinolones (15). Previous reports have shown that changes at position 6, such as in the NFQs studied here, may lead to an enhancement of in vitro activity but not an enhancement of in vivo activity (2, 17). While the NFQs demonstrated good in vitro activities, future pharmacokinetic and pharmacodynamic studies are necessary to show whether a sufficient area under the concentration-time curve/MIC ratio (assuming that this is the parameter most predictive of clinical outcome, as demonstrated for levofloxacin and another NFQ, BMS-284756 [5, 18]) can be obtained to predict whether NFQs will have sufficient potencies against isolates of S. aureus and S. pneumoniae, especially those harboring significant mutations in QRDRs. It is noteworthy that contemporary clinical isolates of S. aureus and coagulase-negative staphylococci for which NFQ MICs were comparatively high were detected, even though they had not been clinically exposed to NFQs. These isolates are likely to be extremely rare. All of these isolates had multiple mutations in QRDRs; this was especially the case for S. epidermidis, which carried three alterations in GyrA alone and perhaps more alterations in other gene loci. As such, resistance to an NFQ requires multiple mutations in QRDRs and may be difficult to achieve through natural selection.
Acknowledgments
This research project was funded by Procter and Gamble Pharmaceuticals.
We express our appreciation to Robert Leunk, Carl Catrenich, and Sid Roychoudhury from Procter and Gamble Pharmaceuticals for critical reading of the manuscript.
REFERENCES
- 1.Barry, A. L., P. C. Fuchs, and S. D. Brown. 2001. In vitro activities of three nonfluorinated quinolones against representative bacterial species. Antimicrob. Agents Chemother. 45:1923-1927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cecchetti, V., C. Parolin, S. Moro, T. Pecere, E. Filipponi, A. Calistri, O. Tabarrini, B. Gatto, M. Palumbo, A. Fravolini, and G. Palu. 2000. 6-Aminoquinolones as new potential anti-HIV agents. J. Med. Chem. 43:3799-3802. [DOI] [PubMed] [Google Scholar]
- 3.Dalhoff, A., U. Petersen, and E. Endermann. 1996. In vitro activity of BAY 12-8039, a new 8-methoxyquinolone. Chemotherapy (Basel) 42:410-425. [DOI] [PubMed] [Google Scholar]
- 4.Fukuda, H., and K. Hiramatsu. 1999. Primary targets of fluoroquinolones in Streptococcus pneumoniae. Antimicrob. Agents Chemother. 43:410-412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fung-Tonc, J. C., B. Minassian, B. Kolek, E. Huczko, L. Aleksunes, T. Stickle, T. Washo, E. Gradelski, L. Valera, and D. P. Bonner. 2000. Antibacterial spectrum of a novel des-fluoro(6) quinolone, BMS-284756. Antimicrob. Agents Chemother. 44:3351-3356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gill, M. J., N. P. Brenwald, and R. Wise. 1999. Identification of an efflux pump gene, pmrA, associated with fluoroquinolone resistance in Streptococcus pneumoniae. Antimicrob. Agents Chemother. 43:187-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Janoir, C., V. Zeller, M. D. Kitzis, N. J. Moreau, and L. Gutmann. 1996. High-level fluoroquinolone resistance in Streptococcus pneumoniae requires mutations in parC and gyrA. Antimicrob. Agents Chemother. 43:2760-2764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jones, M. E., D. F. Sahm, N. Martin, S. Scheuring, P. Heisig, C. Thornsberry, K. Köhrer, and F.-J. Schmitz. 2000. A prevalence study of gyrA, gyrB, parC, and parE mutations in clinical isolates of Streptococcus pneumoniae with decreased susceptibilities to different fluoroquinolones and originating from worldwide surveillance studies during the 1997-1998 respiratory season. Antimicrob. Agents Chemother. 44:462-466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Millichap, J. J., E. Pestova, F. Siddiqui, G. A. Noskin, and L. R. Peterson. 2001. Fluoroquinolone resistance is a poor surrogate marker for type II topoisomerase mutations in clinical isolates of Streptococcus pneumoniae. J. Clin. Microbiol. 39:2719-2721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Munoz, R., and A. G. De La Campa. 1996. ParC subunit of DNA topoisomerase IV of Streptococcus pneumoniae is a primary target of fluoroquinolones and cooperates with DNA gyrase A subunit in forming resistance phenotype. Antimicrob. Agents Chemother. 40:2252-2257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Committee for Clinical Laboratory Standards. 2000. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically, 5th ed. M7-A5. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 12.National Committee for Clinical Laboratory Standards. 2002. Performance standards for antimicrobial susceptibility testing. Twelfth informational supplement. M100-S12. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 13.Ng, E. Y., M. Trucksis, and D. C. Hooper. 1996. Quinolone resistance mediated by norA: physiological characterization and relationship to flqB, a quinolone resistance locus on the Staphylococcus aureus chromosome. Antimicrob. Agents Chemother. 38:1345-1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pan, X.-S., J. Ambler, S. Mehtar, and L. M. Fisher. 1996. Involvement of topoisomerase IV and DNA gyrase as ciprofloxacin targets in Streptococcus pneumoniae. Antimicrob. Agents Chemother. 40:2321-2326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pestova, E., J. J. Millichap, G. A. Noskin, and L. R. Peterson. 2000. Intracellular targets of moxifloxacin: a comparison with other fluoroquinolones. J. Antimicrob. Chemother. 45:583-590. [DOI] [PubMed] [Google Scholar]
- 16.Pestova, E., R. Beyer, N. P. Cianciotto, G. A. Noskin, and L. R. Peterson. 1999. Contribution of topoisomerase IV and DNA gyrase mutations in Streptococcus pneumoniae to resistance to novel fluoroquinolones. Antimicrob. Agents Chemother. 43:2000-2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peterson, L. R. 2001. Quinolone molecular structure-activity relationships: what we have learned about improving antimicrobial activity. Clin. Infect. Dis. 5(Suppl. 3):S180-S186. [DOI] [PubMed] [Google Scholar]
- 18.Preston, S. L., G. L. Drusano, A. L. Berman, C. L. Fowler, A. T. Chow, B. Dornseif, V. Reichel, J. Natarajan, and M. Corrado. 1998. Pharmacodynamics of levofloxacin: a new paradigm for early clinical trials. JAMA 279:125-129. [DOI] [PubMed] [Google Scholar]
- 19.Roychoudhury, S., T. L. Twimen, K. M. Makin, E. J. McIntosh, B. Ledoussal, and C. E. Catrenich. 2001. Activity of non-fluorinated quinolones (NFQs) against quinolone-resistant Escherichia coli and Streptococcus pneumoniae. J. Antimicrob. Chemother. 48:29-36. [DOI] [PubMed] [Google Scholar]
- 20.Roychoudury, S., C. E. Catrenich, H. D. McKeever, K. M. Makin, P. M. Koenigs, and B. Ledoussal. 2001. Quinolone resistance in staphylococci: activities of the new nonfluorinated quinolones against molecular targets in whole cells and clinical isolates. Antimicrob. Agents Chemother. 45:1115-1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schmitz, F.-J., M. E. Jones, B. Hofmann, B. Hansen, S. Scheuring, M. Lückefahr, A. Fluit, J. Verhoef, U. Hadding, H.-P. Heinz, and K. Köhrer. 1998. Characterization of grlA, grlB, gyrA, and gyrB mutations in 116 unrelated isolates of Staphylococcus aureus and effects of mutations on ciprofloxacin MICs. Antimicrob. Agents Chemother. 42:1249-1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taba, H., and N. Kusano. 1998. Sparfloxacin resistance in clinical isolates of Streptococcus pneumoniae: involvement of multiple mutations in gyrA and parC genes. Antimicrob. Agents Chemother. 42:2193-2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Takahata, M., M. Yonezawa, S. Kurose, N. Futakucki, N. Matsubara, Y. Watanabe, and H. Narita. 1996. Mutations in gyrA and grlA genes of quinolone-resistant clinical isolates of methicillin-resistant Staphylococcus aureus. J. Antimicrob. Chemother. 38:543-546. [DOI] [PubMed] [Google Scholar]
- 24.Tankovic, J., B. Perichon, J. Duval, and P. Courvalin. 1996. Contribution of mutations in gyrA and parC genes to fluoroquinolone resistance of mutants of Streptococcus pneumoniae obtained in vivo and in vitro. Antimicrob. Agents Chemother. 40:2505-2510. [DOI] [PMC free article] [PubMed] [Google Scholar]