Abstract
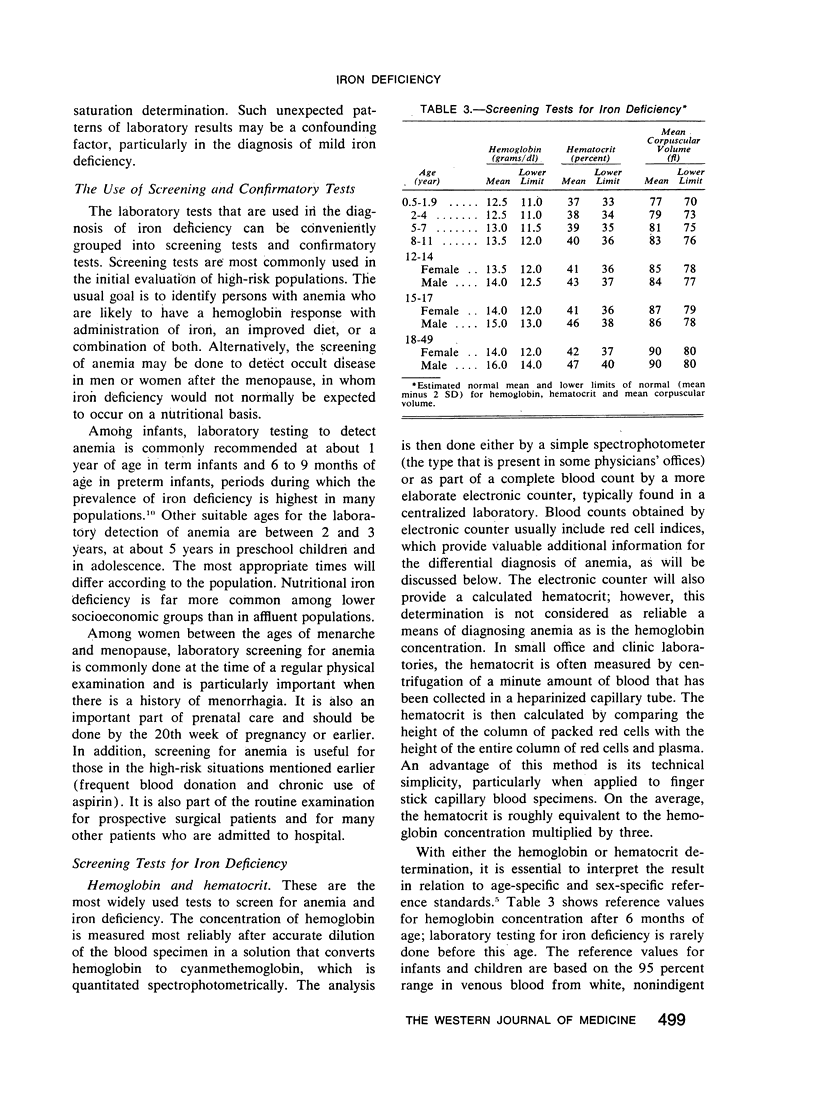
Mild iron deficiency is common among infants, adolescents and women during the childbearing years. Practical and economical approaches toward its identification, treatment and prevention are needed. Laboratory screening is based on hemoglobin or hematocrit determinations compared with age-specific and sex-specific reference standards. If blood specimens have been analyzed by electronic counter, the presence of a normal or low-normal value for red cell volume increases the likelihood that anemia is due to iron deficiency. Other laboratory tests that may be helpful in selected cases include determining serum ferritin, transferrin saturation or erythrocyte protoporphyrin values. However, in most cases, a simple therapeutic trial with ferrous sulfate may be instituted on the basis of history and a screening test alone. If repeat laboratory studies after a month show no improvement, iron treatment should be stopped and other causes of anemia should be considered.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- CONRAD M. E., CROSBY W. H. The natural history of iron deficiency induced by phlebotomy. Blood. 1962 Aug;20:173–185. [PubMed] [Google Scholar]
- Cook J. D., Lipschitz D. A., Miles L. E., Finch C. A. Serum ferritin as a measure of iron stores in normal subjects. Am J Clin Nutr. 1974 Jul;27(7):681–687. doi: 10.1093/ajcn/27.7.681. [DOI] [PubMed] [Google Scholar]
- Cook J. D., Monsen E. R. Food iron absorption in human subjects. III. Comparison of the effect of animal proteins on nonheme iron absorption. Am J Clin Nutr. 1976 Aug;29(8):859–867. doi: 10.1093/ajcn/29.8.859. [DOI] [PubMed] [Google Scholar]
- Dallman P. R., Beutler E., Finch C. A. Effects of iron deficiency exclusive of anaemia. Br J Haematol. 1978 Oct;40(2):179–184. doi: 10.1111/j.1365-2141.1978.tb03655.x. [DOI] [PubMed] [Google Scholar]
- Dallman P. R., Siimes M. A. Percentile curves for hemoglobin and red cell volume in infancy and childhood. J Pediatr. 1979 Jan;94(1):26–31. doi: 10.1016/s0022-3476(79)80344-3. [DOI] [PubMed] [Google Scholar]
- Eschbach J. W., Cook J. D. Quantitating iron balance in hemodialysis patients. Trans Am Soc Artif Intern Organs. 1977;23:54–58. doi: 10.1097/00002480-197700230-00016. [DOI] [PubMed] [Google Scholar]
- Finch C. A., Cook J. D., Labbe R. F., Culala M. Effect of blood donation on iron stores as evaluated by serum ferritin. Blood. 1977 Sep;50(3):441–447. [PubMed] [Google Scholar]
- Garby L., Irnell L., Werner I. Iron deficiency in women of fertile age in a Swedish community. 3. Estimation of prevalence based on response to iron supplementation. Acta Med Scand. 1969 Jan-Feb;185(1-2):113–117. doi: 10.1111/j.0954-6820.1969.tb07305.x. [DOI] [PubMed] [Google Scholar]
- HAMILTON L. D., GUBLER C. J., CARTWRIGHT G. E., WINTROBE M. M. Diurnal variation in the plasma iron level of man. Proc Soc Exp Biol Med. 1950 Oct;75(1):65–68. doi: 10.3181/00379727-75-18102. [DOI] [PubMed] [Google Scholar]
- Hallberg L., Högdahl A. M., Nilsson L., Rybo G. Menstrual blood loss--a population study. Variation at different ages and attempts to define normality. Acta Obstet Gynecol Scand. 1966;45(3):320–351. doi: 10.3109/00016346609158455. [DOI] [PubMed] [Google Scholar]
- Hefnawi F., Askalani H., Zaki K. Menstrual blood loss with copper intrauterine devices. Contraception. 1974 Feb;9(2):133–139. doi: 10.1016/0010-7824(74)90026-2. [DOI] [PubMed] [Google Scholar]
- Koerper M. A., Stempel D. A., Dallman P. R. Anemia in patients with juvenile rheumatoid arthritis. J Pediatr. 1978 Jun;92(6):930–933. doi: 10.1016/s0022-3476(78)80363-1. [DOI] [PubMed] [Google Scholar]
- Lipschitz D. A., Cook J. D., Finch C. A. A clinical evaluation of serum ferritin as an index of iron stores. N Engl J Med. 1974 May 30;290(22):1213–1216. doi: 10.1056/NEJM197405302902201. [DOI] [PubMed] [Google Scholar]
- Massa E., MacLean W. C., Jr, López de Romaña G., de Martinez Y., Graham G. G. Oral iron absorption in infantile protein-energy malnutrition. J Pediatr. 1978 Dec;93(6):1045–1049. doi: 10.1016/s0022-3476(78)81257-8. [DOI] [PubMed] [Google Scholar]
- Monsen E. R., Hallberg L., Layrisse M., Hegsted D. M., Cook J. D., Mertz W., Finch C. A. Estimation of available dietary iron. Am J Clin Nutr. 1978 Jan;31(1):134–141. doi: 10.1093/ajcn/31.1.134. [DOI] [PubMed] [Google Scholar]
- Norrby A. Iron absorption studies in iron deficiency. Scand J Haematol Suppl. 1974;20:1–125. [PubMed] [Google Scholar]
- Okuno T. Red cell size and age. Br Med J. 1972 Feb 26;1(5799):569–570. doi: 10.1136/bmj.1.5799.569-c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PIERSON R. N., Jr, HOLT P. R., WATSON R. M., KEATING R. P. Aspirin and gastrointestinal bleeding. Chromate blood loss studies. Am J Med. 1961 Aug;31:259–265. doi: 10.1016/0002-9343(61)90114-0. [DOI] [PubMed] [Google Scholar]
- Pearson H. A., Robinson J. E. The role of iron in host resistance. Adv Pediatr. 1976;23:1–33. [PubMed] [Google Scholar]
- Piomelli S., Brickman A., Carlos E. Rapid diagnosis of iron deficiency by measurement of free erythrocyte porphyrins and hemoglobin: the FEP/hemoglobin ratio. Pediatrics. 1976 Jan;57(1):136–141. [PubMed] [Google Scholar]
- Stockman J. A., 3rd, Weiner L. S., Simon G. E., Stuart M. J., Oski F. A. The measurement of free erythrocyte porphyrin (FEP) as a simple means of distinguishing iron deficiency from beta-thalassemia trait in subjects with microcytosis. J Lab Clin Med. 1975 Jan;85(1):113–119. [PubMed] [Google Scholar]


