Abstract
Mutations associated with fluoroquinolone resistance in clinical isolates of Proteus mirabilis were determined by genetic analysis of the quinolone resistance-determining region (QRDR) of gyrA, gyrB, parC, and parE. This study included the P. mirabilis type strain ATCC 29906 and 29 clinical isolates with reduced susceptibility (MIC, 0.5 to 2 μg/ml) or resistance (MIC, ≥4 μg/ml) to ciprofloxacin. Susceptibility profiles for ciprofloxacin, clinafloxacin, gatifloxacin, gemifloxacin, levofloxacin, moxifloxacin, and trovafloxacin were correlated with amino acid changes in the QRDRs. Decreased susceptibility and resistance were associated with double mutations involving both gyrA (S83R or -I) and parC (S80R or -I). Among these double mutants, MICs of ciprofloxacin varied from 1 to 16 μg/ml, indicating that additional factors, such as drug efflux or porin changes, also contribute to the level of resistance. For ParE, a single conservative change of V364I was detected in seven strains. An unexpected result was the association of gyrB mutations with high-level resistance to fluoroquinolones in 12 of 20 ciprofloxacin-resistant isolates. Changes in GyrB included S464Y (six isolates), S464F (three isolates), and E466D (two isolates). A three-nucleotide insertion, resulting in an additional lysine residue between K455 and A456, was detected in gyrB of one strain. Unlike any other bacterial species analyzed to date, mutation of gyrB appears to be a frequent event in the acquisition of fluoroquinolone resistance among clinical isolates of P. mirabilis.
Proteus mirabilis is a frequent cause of urinary tract infections that are often persistent and difficult to treat (17). As an opportunistic pathogen, P. mirabilis infects wounds, burns, the respiratory tract, and other sites. In addition, recent studies suggest that P. mirabilis may play a role in rheumatoid arthritis (5, 18). The development of broad-spectrum fluoroquinolones provides new treatment options for P. mirabilis infections, including those caused by strains resistant to other classes of antimicrobial agents. Although fluoroquinolone resistance has been relatively slow to emerge in this species, recent reports indicate an increase in the incidence of clinical isolates of P. mirabilis with decreased susceptibility or resistance to older fluoroquinolones, such as ciprofloxacin (4, 7).
The primary mechanisms of resistance to fluoroquinolones are mutations that result in alteration of the target proteins, DNA gyrase (encoded by gyrA and gyrB) and topoisomerase IV (encoded by parC and parE), and decreased intracellular drug accumulation due to drug efflux or changes in outer membrane proteins. In several species of Enterobacteriaceae, including Escherichia coli, Citrobacter freundii, Klebsiella spp., and Enterobacter spp., decreased susceptibility or resistance to fluoroquinolones is associated with specific point mutations in gyrA. Additional mutations in the gyrase or topoisomerase IV genes contribute to higher levels of resistance (20, 21, 23). These mutations generally occur in highly conserved areas of the genes designated the quinolone resistance-determining regions (QRDRs) (25). The DNA sequences of these genes have not been reported for P. mirabilis, and therefore, mutations associated with fluoroquinolone resistance in P. mirabilis have not been identified. The purpose of this study was to determine the DNA sequence of the QRDR of gyrA, gyrB, parC, and parE in the fluoroquinolone-susceptible type strain of P. mirabilis, to characterize mutations in clinical isolates with decreased susceptibility or resistance to fluoroquinolones, and to analyze the associated MICs for patterns of cross-resistance among this class of antimicrobial agents.
MATERIALS AND METHODS
Bacterial strains and determination of fluoroquinolone susceptibility profiles.
Clinical isolates were obtained during the Intensive Care Antimicrobial Resistance Epidemiology study, in which isolates were collected from hospitals across the United States between 1994 and 1999 (2). Strains selected for DNA sequence analysis were chosen to represent diverse geographical locations and a range of MICs of fluoroquinolones. Susceptibility profiles were determined by the broth microdilution method with cation-adjusted Mueller-Hinton broth (Difco Laboratories, Detroit, Mich.) according to the methods of the NCCLS (13). E. coli ATCC 25922 and Pseudomonas aeruginosa ATCC 27853 were used as control strains. Reagent powders of each of the following antimicrobial agents were obtained from the indicated manufacturers: ciprofloxacin and moxifloxacin, Bayer Corporation, West Haven, Conn.; clinafloxacin, Parke-Davis Pharmaceutical, Ann Arbor, Mich.; gatifloxacin, Bristol-Myers Squibb, Wallingford, Conn.; gemifloxacin, SmithKline Beecham, Philadelphia, Penn.; levofloxacin, Ortho-McNeil Pharmaceutical, Raritan, N.J.; and trovafloxacin, Pfizer, New York, N.Y.
PCR amplification.
Gene fragments encompassing the QRDR and flanking nucleotide sequences were amplified from chromosomal DNA in cell lysates prepared by the method of Conrad et al. (3). Degenerate oligonucleotide primers (Table 1) from conserved regions of each gene were designed from alignments of known DNA sequences in the GenBank database. PCR mixtures (final volume, 50 μl) were prepared with 5 μl of cell lysate containing chromosomal DNA for template, 50 pmol of each primer, 100 μmol of (each) deoxynucleoside triphosphates, 10 mM Tris-HCl (pH 8.3), 1.5 mM MgCl2, and 1 U of AmpliTaq DNA polymerase LD (Applied Biosystems, Foster City, Calif.). Amplification parameters (see Table 1 for annealing temperatures [Ta]) included an initial denaturation for 5 min at 95°C followed by 35 cycles of 95°C for 45 s, 20 s at the Ta, 72°C for 30 s, and a final extension of 72°C for 7 min in a GeneAmp 9700 thermal cycler (Applied Biosystems). PCR products were purified with QIAquick spin columns (QIAGEN, Chatsworth, Calif.).
TABLE 1.
Oligonucleotide primers and annealing temperatures (Ta) used in this study
| Gene | Primera | Ta (°C) | Gene fragmentb |
|---|---|---|---|
| gyrA | 5′ CCAGATGT(A/C/T)CG(A/C/T)GATGG (F) | ||
| 5′ ACGAAATCAAC(G/C)GT(C/T)TCTTTTTC (R) | 52 | 103-438 | |
| gyrB | 5′ TGA(C/T)GATGC(G/C/A)CG(T/C)GAAGG (F) | ||
| 5′ CGTACG(A/G)ATGTG(C/A)GA(G/A)CC (R) | 54 | 936-1506 | |
| 5′ CCACATCCGTCATGATAA (S) | 55 | 1497c | |
| parC | 5′ TTGCC(A/T)TTTAT(C/T)GG(G/T)GATGG (F) | ||
| 5′ CGCGC(A/T)GGCAGCATTTT(A/T)GG (R) | 52 | 91-583 | |
| parE | 5′ GCA(G/A)GA(T/G)(C/G)CGCA(G/A)TT(T/C)G (F) | ||
| 5′ ATC(A/C/G)GAGTC(C/T/G)GCATCCG (R) | 56 | 972-1466 |
Degenerate primers designed from alignment of known sequences. Abbreviations: F, forward; R, reverse; S, sequencing primer.
Nucleotide positions are based on E. coli gene sequences.
DNA sequence analysis.
With the exception of the gyrB reverse sequence, degenerate PCR primers were also used as sequencing primers in dRhodamine Terminator cycle sequencing reactions following the manufacturer's protocol (Applied Biosystems), except the annealing temperature was increased to 52°C (55°C for the gyrB reverse sequence primer). Due to high background in the DNA sequences obtained with the reverse PCR primer, an additional primer was designed using the sequence data from the gyrB forward primer (Table 1). To eliminate possible errors due to amplification artifacts, the forward and reverse sequences were determined using products of independent PCRs. DNA and derived amino acid sequences were analyzed with DNAsis for Windows (version 2.5; Hitachi Software Engineering Co., Ltd., South San Francisco, Calif.).
Nucleotide sequence accession numbers.
The partial DNA sequences of gyrA, gyrB, parC, and parE from P. mirabilis ATCC 29906 were submitted to GenBank and assigned accession numbers AF397169 (gyrA), AF503506 (gyrB), AF363611 (parC), and AF503505 (parE).
RESULTS AND DISCUSSION
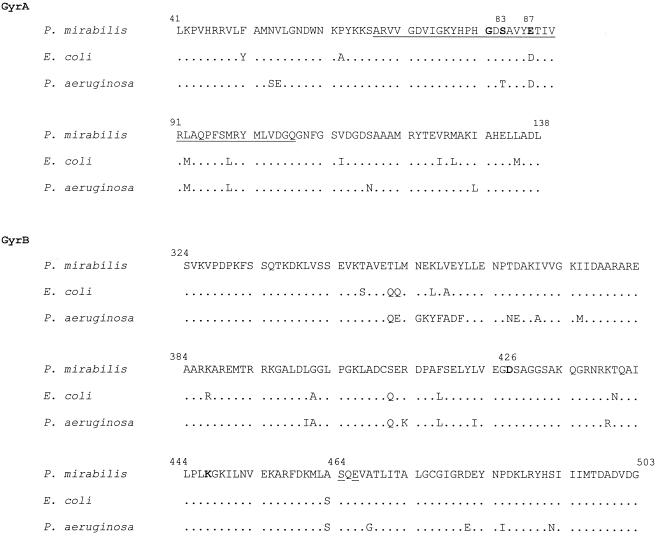
The degenerate oligonucleotide primers designed for this study were based on regions of DNA encoding conserved amino acid sequences in GyrA and ParC from several species of Enterobacteriaceae (23; L. M. Weigel, G. J. Anderson, and F. C. Tenover, Abstr. 101st Gen. Meet. Am. Soc. Microbiol., abstr. A-57, 2001) and gyrB and parE sequences in the GenBank database. Primers for gyrA amplified the expected 335-bp gene fragment from the P. mirabilis type strain, ATCC 29906, corresponding to nucleotide positions 103 to 437 of the E. coli gyrA sequence (data not shown). This gene fragment (excluding primer sequences) encoded amino acids 41 to 138 (Fig. 1). Alignment of the 120-bp gyrA QRDR of P. mirabilis with analogous sequences from E. coli (19) and P. aeruginosa (11) revealed nucleotide identities of 80.0 and 78.4%, respectively (data not shown). The derived amino acid sequence of the QRDR from GyrA of P. mirabilis (Fig. 1, underlined) was highly conserved compared with corresponding sequences from other gram-negative organisms and differed from that of E. coli at only three positions: a conservative change of D87E and the exchange of methionine and leucine at two positions, M92L and L98M. These three amino acid variations are also found in GyrA of Providencia stuartii (23) and Aeromonas salmonicida (14).
FIG. 1.
Amino acid sequence comparison of GyrA and GyrB QRDRs. Amino acid positions are based on E. coli GyrA and GyrB sequences (19, 24). The conventional QRDR of GyrA is underlined. Amino acid positions frequently associated with fluoroquinolone resistance are indicated by boldface type. GyrB amino acid positions altered in P. mirabilis strains (this study) are underlined.
Amplification of the gyrB gene fragment produced the expected 571-bp product corresponding to nucleotides 936 to 1506 of the E. coli gyrB gene sequence (data not shown). The derived amino acid sequence encompassed residues 319 to 493 (Fig. 1). Compared with analogous sequences of gyrB from E. coli (24) and P. aeruginosa (GenBank AB005881) nucleotide sequence identities were 78.9 and 68.2%, respectively (data not shown). Comparison of the aligned GyrB amino acid sequences from the three species revealed both conserved and variable regions.
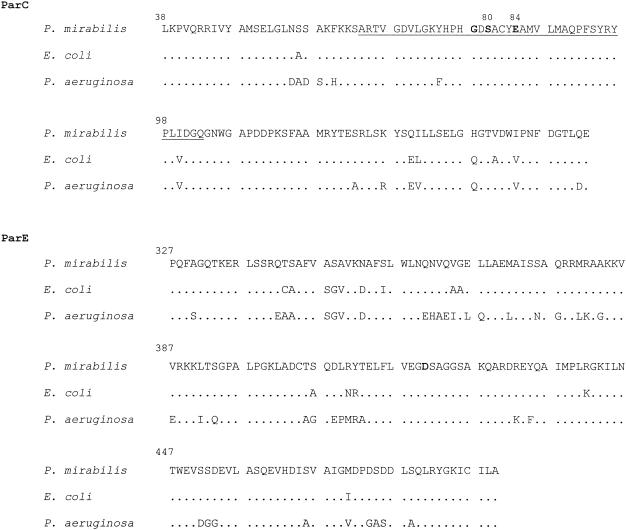
The parC primers amplified a 389-bp gene fragment corresponding to nucleotide positions 91 to 479 of the E. coli parC sequence (10) (data not shown), which encode amino acids residues 38 to 153 (excluding primer sequences [Fig. 2 ]). The nucleotide sequence of the parC QRDR from P. mirabilis shared 80.0% identity with the analogous region of parC from E. coli and 69.0% identity with that of P. aeruginosa (1) (data not shown). Alignment of the ParC amino acid sequences revealed a single conservative amino acid change of V100I in the QRDR (underlined in Fig. 2) when compared with E. coli. An additional change of F74Y was noted in the comparison of the P. mirabilis QRDR with that of P. aeruginosa. DNA and amino acid sequences outside the QRDR were less conserved.
FIG. 2.
Amino acid sequence comparisons of ParC and ParE. Amino acid positions are based on E. coli ParC and ParE sequences (10). The conventional QRDR in ParC is underlined, and the amino acid positions most frequently associated with fluoroquinolone resistance are indicated by boldface type.
Amplification of the parE gene fragment from P. mirabilis produced a 495-bp product corresponding to nucleotides 972 to 1466 of the E. coli parE (10) gene sequence (data not shown), which encodes amino acid residues 327 to 489 (excluding primer sequences [Fig. 2]). Alignment of the parE gene fragment with analogous sequences from E. coli and P. aeruginosa (1) revealed nucleotide identities of 74.4 and 60.4%, respectively (data not shown). Compared with E. coli and P. aeruginosa, the P. mirabilis ParE amino acid sequence was more variable than the ParC sequence (Fig. 2).
Twenty-nine clinical isolates with various levels of decreased susceptibility or resistance to ciprofloxacin (MICs, 0.5 to >128 μg/ml) were selected for genetic analysis. In addition to ciprofloxacin, fluoroquinolone susceptibility profiles of each strain were determined for clinafloxacin, gatifloxacin, gemifloxacin, levofloxacin, moxifloxacin, and trovafloxacin (Table 2). Clinafloxacin showed the highest level of activity on a per-gram basis for all isolates tested, followed by levofloxacin and ciprofloxacin. In general, the MICs of the newer fluoroquinolones, gatifloxacin, gemifloxacin, moxifloxacin, and trovafloxacin, were higher than the MICs of ciprofloxacin and levofloxacin; however, for each of these agents, the MIC varied significantly among strains with identical levels of resistance to ciprofloxacin, indicating that multiple factors contribute to the level of resistance to each agent.
TABLE 2.
QRDR amino acid substitutions and associated MICs of seven fluoroquinolones for clinical isolates of P. mirabilis
| Strain | Amino acid at indicated positionb
|
MIC (μg/ml) ofa:
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GyrA
|
GyrB
|
ParC
|
CIP | LVX | CLX | GAT | MXF | TVA | GMX | ||||
| 83 | 87 | 464 | 466 | 78 | 80 | ||||||||
| ATCC 29906 | S | E | S | E | G | S | ≤0.12 | ≤0.12 | ≤0.03 | ≤0.12 | ≤0.25 | ≤0.12 | ≤0.06 |
| 3201 | —c | — | — | — | — | — | ≤0.12 | ≤0.12 | ≤0.03 | ≤0.25 | ≤0.25 | ≤0.12 | 0.12 |
| 3154 | — | — | F | — | — | — | ≤0.12 | ≤0.12 | ≤0.03 | 0.5 | 0.5 | 0.25 | 0.12 |
| 1075 | R | — | — | — | — | R | 0.5 | 1 | 0.25 | 2 | 2 | 2 | 1 |
| 1549 | I | — | — | — | — | I | 1 | 1 | 0.25 | 2 | 8 | 16 | 4 |
| 3073 | I | — | — | — | — | I | 1 | 1 | 0.25 | 4 | 8 | 16 | 4 |
| 3523 | I | — | — | — | — | R | 1 | 1 | 0.25 | 4 | 8 | 16 | 4 |
| 1391 | R | — | — | — | — | R | 1 | 1 | 0.5 | 4 | 8 | 8 | 4 |
| 1411 | R | — | — | — | — | R | 1 | 2 | 0.5 | 4 | 8 | 8 | 4 |
| 1977 | I | — | — | — | — | I | 2 | 2 | 0.5 | 4 | 16 | 32 | 16 |
| 3917 | I | — | — | — | — | R | 4 | 4 | 0.5 | 8 | 8 | 8 | 8 |
| 1964 | I | — | — | D | — | I | 4 | 4 | 1 | 16 | 16 | 32 | 8 |
| 3110 | R | — | F | — | — | I | 4 | 4 | 1 | 16 | 16 | 32 | 8 |
| 1970 | I | — | — | D | — | I | 4 | 4 | 1 | 16 | 32 | 128 | 8 |
| 3087 | I | — | — | — | — | I | 8 | 2 | 0.5 | 4 | 8 | 16 | 16 |
| 5520 | I | — | —d | — | — | I | 8 | 2 | 1 | 8 | 8 | 16 | 16 |
| 1283 | R | — | — | — | — | R | 8 | 4 | 1 | 16 | 16 | 16 | 32 |
| 4045 | — | K | — | — | — | R | 8 | 4 | 2 | 8 | 8 | 4 | 8 |
| 3623 | R | — | — | — | — | R | 8 | 8 | 2 | 8 | 16 | 16 | 8 |
| 1223 | R | — | Y | — | — | I | 8 | 8 | 2 | 16 | 32 | 32 | 8 |
| 3116 | R | — | — | — | — | R | 8 | 8 | 2 | 16 | 64 | 64 | 32 |
| 1487 | R | — | — | — | — | R | 8 | 16 | 2 | 16 | 64 | 64 | 16 |
| 5662 | R | — | — | — | — | R | 16 | 4 | 1 | 8 | 8 | 4 | 8 |
| 3799 | R | — | Y | — | — | I | 16 | 4 | 2 | 16 | 16 | 16 | 8 |
| 5596 | R | — | F | — | D | — | 16 | 8 | 1 | 16 | 16 | 32 | 8 |
| 3790 | R | — | Y | — | — | I | 16 | 8 | 2 | 16 | 16 | 16 | 32 |
| 4069 | R | — | Y | — | — | I | 32 | 16 | 4 | 64 | 64 | >128 | 32 |
| 3951 | I | — | Y | — | — | R | 128 | 32 | 4 | 64 | 32 | 32 | >32 |
| 3750 | R | — | F | — | — | I | 128 | 64 | 8 | 128 | 128 | 64 | 32 |
| 3991 | R | — | Y | — | — | I | >128 | 32 | 8 | 128 | 64 | >128 | >32 |
Abbreviations: CIP, ciprofloxacin; CLX, clinafloxacin; GAT, gatifloxacin; GMX, gemifloxacin; LVX, levofloxacin; MXF, moxifloxacin; TVA, trovafloxacin. NCCLS breakpoints (susceptible, intermediate, resistant) are as follows: CIP, 1, 2, and 4 μg/ml, respectively; LVX, 2, 4, and 8 μg/ml, respectively. No breakpoints are available for CLX, GAT, MXF, TVA, or GMX.
—, no change from type strain sequence.
Strain 5520 has a 3-nucleotide insert (AAG, encoding an additional lysine) in gyrB, between the codons for K455 and A456.
The DNA and derived amino acid sequences of the QRDRs of gyrA, gyrB, parC, and parE for each clinical isolate were compared with those of the type strain, ATCC 29906. Variation of the gyrA sequences was confined to those mutations associated with resistance (data not shown) with the exception of one silent nucleotide substitution, a C-to-T transition for nucleotide position 269, in 24 of the isolates. With only one exception, gyrA mutations resulted in amino acid changes of S83R or S83I in each isolate (Table 2). These amino acid changes are the same as those reported for fluoroquinolone-resistant P. stuartii (23). The E87K change found in GyrA of one isolate (strain 4045) was also located in an amino acid position known to be associated with resistance in both gram-positive and gram-negative organisms (8). Unlike E. coli, in which high-level fluoroquinolone resistance is associated with double mutations in gyrA and an additional mutation in parC (20, 21), no double mutations were detected in the gyrA gene fragment from isolates of P. mirabilis.
Sequence analysis of parC gene fragments from the clinical isolates revealed nucleotide substitutions in the following codons with no change in amino acid (compared with the type strain sequence): G78 (T to A, 15 strains), V87 (A to G, 18 strains), and F115 (C to T, 8 strains) (data not shown). The only other nucleotide substitutions detected in parC were mutations associated with fluoroquinolone resistance. All but one of the parC mutations occurred in the codon for S80, and like gyrA, these mutations resulted in a change of S80R or S80I. The exception, G78D (strain 5596), was an amino acid position also known to be associated with resistance in both gram-positive and gram-negative organisms, although changes in this amino acid position have been reported less frequently than changes in S80 or E84 of ParC.
An unprecedented frequency of amino acid changes in the GyrB subunit was an unexpected result in this study. The gyrB mutations were generally seen in strains with high-level resistance to fluoroquinolones. Amino acid alterations of GyrB included S464Y, S464F, and E466D and a novel mutation in strain 5520 which introduced three nucleotides (AAG) between the codons for K455 and A456, resulting in the insertion of an additional lysine residue. All but one of the changes of GyrB/S464 occurred in association with a GyrA/Ser83R change. In addition, the GyrB/E466D mutation was seen only with a GyrA/S83I change, suggesting the possibility of a correlation between specific alterations in the structures of the two gyrase subunits. However, in one strain the gyrB mutation occurred without alteration of GyrA or ParC, indicating that this amino acid change in GyrB may be one of the initial mutations acquired in the evolution of resistance in this species. Although trovafloxacin and the two 8-methoxy quinolones, moxifloxacin and gatifloxacin, were the only agents for which decreased susceptibilities were detectable in this strain, the MICs of these fluoroquinolones were increased consistently in several repeats of the susceptibility tests, compared with the susceptible type strain and with the clinical isolate with no mutation in the gyrase or topoisomerase IV genes. Among other species, mutations of gyrB that are known to contribute to resistance are found in the codons for D435 and E474 in Streptococcus pneumoniae (15, 16, 22), D437 and R458 in S. aureus (9), and D426 in E. coli (12). Gensberg et al. (6) have described a mutation associated with fluoroquinolone resistance in a clinical isolate of Salmonella enterica serovar Typhimurium that results in an S463-to-Y alteration of gyrB. This amino acid residue is not conserved in P. mirabilis but is adjacent to the S464Y (or S464I) change detected in this study, suggesting that alteration of serine in either position will affect susceptibility to fluoroquinolones.
Within the gene fragment amplified from parE, the only nucleotide substitution that resulted in an amino acid alteration was a conservative change of V364I in seven isolates. Although ParE alterations do not appear to play an important role in fluoroquinolone resistance among the isolates in this study, mutation of this subunit may occur following exposure of clinical isolates to the novel structures of new quinolone agents as they are introduced into clinical therapy.
A comparison of amino acid changes and fluoroquinolone MICs revealed no correlation between a double mutation (gyrA and parC) and the level of resistance (Table 2). These double mutations were found in isolates with reduced susceptibility to fluoroquinolones and in isolates that were resistant. MICs of ciprofloxacin and levofloxacin were generally lowest for strains with mutations that resulted in changes of GyrA/S83I and ParC/S83I. However, when both the GyrA and ParC changes resulted in serine-to-arginine substitutions or when the amino acid changes were mixed, arginine and isoleucine, there was no correlation of mutations with levels of resistance. Among the strains with three mutations, involving GyrA, GyrB, and ParC, MICs of ciprofloxacin ranged from 4 to >128 μg/ml. These results indicate significant contributions to fluoroquinolone resistance by either additional mutations outside the conventional QRDRs or decreased intracellular drug accumulation due to active drug efflux or altered outer membrane proteins. Because many studies of fluoroquinolone resistance have not included analysis of gyrB or parE, the region designated the QRDR is not well defined and may be expanded as additional data are reported.
In summary, we report the DNA and derived amino acid sequences for the QRDRs of gyrA, gyrB, parC, and parE from the P. mirabilis type strain and clinical isolates. In addition to the classical alterations of GyrA/S83 and ParC/S80, this initial study of fluoroquinolone-resistant strains revealed gyrB mutations in 12 of 21 nonsusceptible isolates. These results suggest that, unlike E. coli or other species that have been analyzed thus far, alteration of the gyrase B subunit is a relatively frequent event in the acquisition of fluoroquinolone resistance by P. mirabilis, reducing the inhibiting effects of these agents on the target protein, DNA gyrase.
REFERENCES
- 1.Akasaka, T., Y. Onodera, M. Tanaka, and K. Sato. 1999. Cloning, expression, and enzymatic characterization of Pseudomonas aeruginosa topoisomerase IV. Antimicrob. Agents Chemother. 43:530-536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Archibald, L., L. Phillips, D. Monnet, J. E. McGowan, Jr., F. C. Tenover, and R. Gaynes. 1997. Antimicrobial resistance in isolates from inpatients and outpatients in the United States: increasing importance of the intensive care unit. Clin. Infect. Dis. 24:211-215. [DOI] [PubMed] [Google Scholar]
- 3.Conrad, S., M. Oethinger, K. Kaifel, G. Klotz, R. Marre, and W. V. Kern. 1996. gyrA mutations in high-level fluoroquinolone-resistant clinical isolates of Escherichia coli. J. Antimicrob. Chemother. 38:443-455. [DOI] [PubMed] [Google Scholar]
- 4.de Champs, C., R. Bonnet, D. Sirot, C. Chanal, and J. Sirot. 2000. Clinical relevance of Proteus mirabilis in hospital patients: a two year survey. J. Antimicrob. Chemother. 45:537-539. [DOI] [PubMed] [Google Scholar]
- 5.Deighton, C. H., J. W. Gray, A. M. Bint, and D. J. Walker. 1992. Anti-Proteus antibodies in rheumatoid arthritis same-sexed sibships. Br. J. Rheumatol. 31:241-245. [DOI] [PubMed] [Google Scholar]
- 6.Gensberg, K., Y. F. Jin, and L. J. V. Piddock. 1995. A novel gyrB mutation in a fluoroquinolone-resistant clinical isolate of Salmonella typhimurium. FEMS Microbiol. Lett. 132:57-60. [DOI] [PubMed] [Google Scholar]
- 7.Hernández, J. R., L. Martínez-Martínez, A. Pascual, A. I. Suárez, and E. J. Perea. 2000. Trends in the susceptibilities of Proteus mirabilis isolates to quinolones. J. Antimicrob. Chemother. 45:407-408. [DOI] [PubMed] [Google Scholar]
- 8.Hooper, D. C. 1999. Mechanisms of fluoroquinolone resistance. Drug Resist. Updates 2:38-55. [DOI] [PubMed] [Google Scholar]
- 9.Ito, H., H. Yoshida, M. Bogaki-shonai, T. Niga, H. Hattori, and S. Nakamura. 1994. Quinolone resistance mutations in the DNA gyrase gyrA and gyrB genes of Staphylococcus aureus. Antimicrob. Agents Chemother. 38:2014-2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kato, J., Y. Nishimura, R. Imamura, H. Niki, S. Hiraga, and H. Suzuki. 1990. New topoisomerase essential for chromosome segregation in E. coli. Cell 63:393-404. [DOI] [PubMed] [Google Scholar]
- 11.Kureishi, A., J. M. Diver, B. Beckthold, T. Schollaardt, and L. E. Bryan. 1994. Cloning and nucleotide sequence of Pseudomonas aeruginosa DNA gyrase gyrA gene from strain PAO1 and quinolone-resistant clinical isolates. Antimicrob. Agents Chemother. 38:1944-1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nagai, K., T. A. Davies, G. A. Pankuch, B. E. Dewasse, M. R. Jacobs, and P. C. Appelbaum. 2000. In vitro selection of resistance to clinafloxacin, ciprofloxacin, and trovafloxacin in Streptococcus pneumoniae. Antimicrob. Agents Chemother. 44:2740-2746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.NCCLS. 2000. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. M7-A5. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 14.Oppegaard, H., and H. Sorum. 1996. Cloning and nucleotide sequence of the DNA gyrase gyrA gene from the fish pathogen Aeromonas salmonicida. Antimicrob. Agents Chemother. 40:1126-1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pan, X.-S., and L. M. Fisher. 1998. DNA gyrase and topoisomerase IV are dual targets of clinafloxacin action in Streptococcus pneumoniae. Antimicrob. Agents Chemother. 42:2810-2816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perichon, B., J. Tankovic, and P. Courvalin. 1997. Characterization of a mutation in the parE gene that confers fluoroquinolone resistance in Streptococcus pneumoniae. Antimicrob. Agents Chemother. 41:1166-1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rózalski, A., Z. Sidorczyk, and K. Kotelko. 1997. Potential virulence factors of Proteus bacilli. Microbiol. Mol. Biol. Rev. 61:65-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Senior, B. W., P. D. P. McBride, K. D. Morley, and M. A. Kerr. 1995. The detection of raised levels of IgM to Proteus mirabilis in sera from patients with rheumatoid arthritis. J. Med. Microbiol. 43:176-184. [DOI] [PubMed] [Google Scholar]
- 19.Swanberg, S. L., and J. C. Wang. 1987. Cloning and sequencing of the Escherichia coli gyrA gene coding for the A subunit of DNA gyrase. J. Mol. Biol. 197:729-736. [DOI] [PubMed] [Google Scholar]
- 20.Vila, J., J. Ruiz, P. Goñi, and M. T. Jimenez de Anta. 1996. Detection of mutations in parC in quinolone-resistant clinical isolates of Escherichia coli. Antimicrob. Agents Chemother. 40:491-493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vila, J., J. Ruiz, F. B. A. Marco, P. Goñi, E. Giralt, and T. Jimenez de Anta. 1994. Association between double mutation in gyrA gene of ciprofloxacin-resistant clinical isolates of Escherichia coli and MICs. Antimicrob. Agents Chemother. 38:2477-2479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weigel, L. M., G. J. Anderson, R. R. Facklam, and F. C. Tenover. 2001. Genetic analyses of mutations contributing to fluoroquinolone resistance in clinical isolates of Streptococcus pneumoniae. Antimicrob. Agents Chemother. 45:3517-3523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weigel, L. M., C. D. Steward, and F. C. Tenover. 1998. gyrA mutations associated with fluoroquinolone resistance in eight species of Enterobacteriaceae. Antimicrob. Agents Chemother. 42:2661-2667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yamagishi, J.-I., H. Yoshida, M. Yamayoshi, and S. Nakamura. 1986. Nalidixic acid-resistant mutations of the gyrB gene of Escherichia coli. Mol. Gen. Genet. 204:367-373. [DOI] [PubMed] [Google Scholar]
- 25.Yoshida, H., M. Bogaki, M. Nakamura, and S. Nakamura. 1990. Quinolone resistance-determining region in the DNA gyrase gyrA gene of Escherichia coli. Antimicrob. Agents Chemother. 34:1271-1272. [DOI] [PMC free article] [PubMed] [Google Scholar]