Abstract
Burkholderia pseudomallei, the causative agent of melioidosis, is a facultative intracellular gram-negative bacterium that is able to survive and multiply in macrophages. Previously, we reported that B. pseudomallei was able to escape macrophage killing by interfering with the expression of inducible nitric oxide synthase (iNOS). In the present study, we extended this finding and demonstrated that B. pseudomallei was able to activate the expression of suppressor of cytokine signaling 3 (SOCS3) and cytokine-inducible Src homology 2-containing protein (CIS) but not SOCS1 in a mouse macrophage cell line (RAW 264.7). The expression of SOCS3 and CIS in B. pseudomallei-infected macrophages directly correlated with a decreased gamma interferon (IFN-γ) signaling response, as indicated by a reduction in Y701-STAT-1 phosphorylation (pY701-STAT-1). Moreover, a reduction in the expression of IFN-γ-induced proteins, such as interferon regulatory factor 1 (IRF-1), was observed in B. pseudomallei-infected macrophages that were treated with IFN-γ. Since pY701-STAT-1 and IRF-1 are essential transcription factors for regulating iNOS expression, the failure to activate these factors could also result in depression of iNOS expression and a loss of macrophage killing capacity. Taken together, the data indicate that the activation of SOCS3 and CIS expression in B. pseudomallei-infected macrophages interfered with IFN-γ signaling, thus allowing the bacteria to escape killing by these phagocytic cells.
Burkholderia pseudomallei is a gram-negative bacterium that is responsible for a large proportion of community-acquired septicemia in several tropical areas, including Southeast Asia and northern Australia (41, 13). This organism is able to survive and multiply inside both phagocytic and nonphagocytic cells (19). After internalization, the bacterium can escape from a membrane-bound phagosome to the cytoplasm, thus facilitating actin-associated membrane protrusion, which may facilitate its spread from one cell to another (18, 19, 21).
Although macrophages are known to play a major role in innate immunity to a number of bacterial infections, B. pseudomallei can survive and multiply inside macrophages (38). Unlike macrophages infected with other gram-negative bacteria (e.g., Salmonella enterica serovar Typhi), B. pseudomallei-infected macrophages are not able to activate inducible nitric oxide synthase (iNOS) expression (38). We previously reported evidence suggesting that the failure to induce iNOS expression may result from an inability to activate beta interferon (IFN-β) production, leading to reduced interferon regulatory factor 1 (IRF-1) and iNOS expression (39). Addition of exogenous IFN-β or IFN-γ at the time of bacterial challenge restored the macrophages' ability to activate both IRF-1 and iNOS expression, which resulted in enhanced killing of intracellular B. pseudomallei (29, 39, 40). These results demonstrated that under the appropriate conditions, IFNs play an essential role in stimulating the antimicrobial activity of macrophages in response to B. pseudomallei infection.
One common property of IFNs is to induce a transcriptional response through a JAK-STAT signal transduction pathway (12). Once STAT-1 is phosphorylated, it is translocated into the nucleus to regulate transcription of promoters containing an IFN-γ-activated site (GAS) element (11, 15). Several IFN-γ-responsive genes, including IRF-1 and iNOS genes, are known to function in macrophage antimicrobial activity (12, 17). However, the macrophage response to IFNs can be influenced by the expression of suppressor of cytokine signaling (SOCS) proteins. Eight members of the SOCS protein family have been identified that serve as negative effectors of cytokine signaling via the JAK/STAT pathway, thus attenuating the macrophage response (1, 6). SOCS1, SOCS3, and cytokine-inducible Src homology 2-containing protein (CIS) have been shown to inhibit tyrosine 701-STAT-1 (Y701-STAT-1) phosphorylation (pY701-STAT-1) in response to IFN stimulation (3, 33). In addition to cytokines, pathogens and their products can induce SOCS expression. For example, lipopolysaccharide (LPS) could induce SOCS1, SOCS3, and CIS expression in macrophages (10, 22, 30, 34). Some pathogens could interfere with the host immune response by activating SOCS expression, leading to suppression of macrophage activation. For example, persistent Listeria monocytogenes infection of macrophages diminished IFN-γ-stimulated transcription and phosphorylation of STAT-1 (35). The decreased IFN-γ signaling also correlated with the induction of SOCS3 expression in the L. monocytogenes-infected macrophages. In the present study, we demonstrated that B. pseudomallei is able to stimulate SOCS3 and CIS expression in macrophages. The expression of these negative regulators in B. pseudomallei-infected macrophages correlated with a decrease in Y701-STAT-1 phosphorylation, which is normally stimulated by exogenous IFN-γ and is essential for IRF-1 and iNOS production, thereby allowing B. pseudomallei to escape killing by the macrophages.
MATERIALS AND METHODS
Cell line and culture conditions.
Mouse macrophage cell line RAW 264.7 was obtained from the American Type Culture Collection (Rockville, MD). Unless indicated otherwise, the cells were cultured in Dulbecco's modified Eagle's medium (Gibco Labs, Grand Island, NY) supplemented with 10% heat-inactivated fetal bovine serum (HyClone, Logan, UT) at 37°C under a 5% CO2 atmosphere.
Bacterial strains.
B. pseudomallei strain 844 used in this study was originally isolated from a patient admitted to Srinagarind Hospital in the Khon Kaen province of Thailand, where melioidosis is endemic. This bacterium was originally identified as B. pseudomallei based on its biochemical characteristics, colonial morphology on selective media, antibiotic sensitivity profiles, and reactivity with polyclonal and monoclonal antibodies (2, 20, 43). S. enterica serovar Typhi, which was used for comparison throughout the experiments, was originally isolated from a patient at Ramathibodi Hospital (Mahidol University, Bangkok, Thailand).
Nonviable B. pseudomallei was prepared by heating the bacteria (108 CFU/ml) in a boiling water bath for 15 min. The heat-treated bacteria were washed three times with phosphate-buffered saline (pH 7.2) (PBS), and complete killing was confirmed by inoculating the suspension onto tryptic soy agar and observing growth after 48 h.
Infection of mouse macrophage cell line RAW 264.7.
An overnight culture of mouse macrophages (1 × 106 cells) in a six-well plate was cocultured with bacteria at a multiplicity of infection (MOI) of 2:1 for 1 h. To remove extracellular bacteria, the cells were washed three times with 2 ml of PBS, and residual bacteria were killed by incubating the preparations in Dulbecco's modified Eagle's medium containing 250 μg/ml kanamycin (Gibco Labs) for 2 h. After this, the infection was allowed to continue in medium containing 20 μg/ml of kanamycin until the experiment was terminated. The viability of the infected macrophages was determined by trypan blue staining and was found to be more than 90% during the time course employed in this study.
To determine intracellular survival and multiplication of the bacteria, a standard antibiotic protection assay was performed as previously described (21). The intracellular bacteria were liberated by lysing the macrophages with 0.1% Triton X-100, and the released bacteria were plated on tryptic soy agar. The number of intracellular bacteria, expressed as CFU, was determined by bacterial colony counting.
Immunoblotting.
Mouse macrophage preparations were lysed in buffer containing 20 mM Tris, 100 mM NaCl, and 1% NP-40. Lysate samples containing 30 μg of protein were electrophoresed on a 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis gel and then electrotransferred to a nitrocellulose membrane (Schleicher & Schuell, Dassel, Germany). The membrane was blocked with 5% milk for 1 h before incubation overnight with appropriate specific polyclonal rabbit antibodies to mouse SOCS1, SOCS3, CIS, pY701-STAT-1, STAT-1, iNOS, IRF-1, or actin (Santa Cruz Biotechnology, Santa Cruz, CA). The blots were then allowed to react with horseradish peroxidase-conjugated swine anti-rabbit immunoglobulin G (Pierce, Rockford, IL). Protein bands were detected by enhanced chemiluminescence as recommended by the manufacturer (Roche Diagnostics, Mannheim, Germany).
Reverse transcriptase PCR.
Total RNA was extracted from infected cells according to the manufacturer's instructions (Eppendorf, Hamburg, Germany) before it was used for cDNA synthesis with cMaster reverse transcriptase (RT) (Eppendorf). The PCR was performed using cDNA as the template and primer pairs specific for SOCS1, SOCS2, SOCS3, CIS, and actin in amplification reactions with Taq DNA polymerase (Invitrogen, Carlsbad, CA). The following primers were used to amplify the genes: for SOCS1, sense primer 5′-CACCTTCTTGGTGCGCG-3′ and antisense primer 5′-AAGCCATCTTCACGCTGAGC-3′ (9); for SOCS2, sense primer 5′-AGGCCCAGAAGCCCCAC-3′ and antisense primer 5′-TTGGTAAAGGCAGTCCCCA-3′ (10); for SOCS3, sense primer 5′-ATGGTCACCCACAGCAAGTT-3′ and antisense primer 5′-AATCCGCTCTCCTGCAGCTT-3′; for CIS, sense primer 5′-GAACCGAAGGTGCTAGACCCT-3′ and antisense primer 5′-TGTACCCTCCGGCATCTTCT-3′ (10); and for actin, sense primer 5′-CCAGAGCAAGAGAGGTATCC-3′ and antisense primer 5′-CTGTGGTGGTGAAGCTGTAG-3′. The amplified products were electrophoresed on a 2% agarose gel and stained with ethidium bromide before they were visualized under a UV lamp.
RESULTS
B. pseudomallei induces SOCS3 and CIS expression in mouse macrophage cell line RAW 264.7.
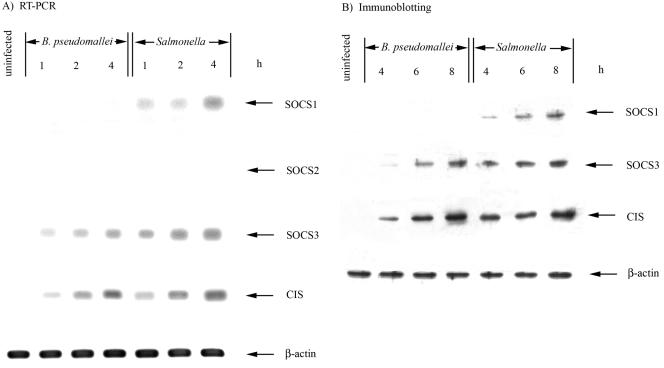
Mouse macrophages were cocultured with bacteria at an MOI of 2:1 and incubated for 1, 2, and 4 h after infection. The levels of SOCS1, SOCS2, SOCS3, and CIS mRNA expression in the infected cells were determined by RT-PCR. Figure 1A shows that B. pseudomallei was able to activate the transcription of SOCS3 and CIS but not the transcription of SOCS1 and SOCS2. Expression of both SOCS3 and CIS was observed within 1 h of infection, and the levels gradually increased with time of incubation. By contrast, macrophages similarly infected with S. enterica serovar Typhi, which was used as a reference for comparison, could activate not only SOCS3 and CIS expression but also SOCS1 mRNA expression within 1 h after infection. SOCS protein expression as determined by immunoblotting (Fig. 1B) of the infected cells was consistent with the mRNA results shown in Fig. 1A.
FIG. 1.
B. pseudomallei-induced SOCS3 and CIS expression in macrophages. Mouse macrophages were infected with either B. pseudomallei or S. enterica serovar Typhi (used as reference) at an MOI of 2:1. At different times, the infected cells were lysed and the levels of SOCS mRNAs (A) and proteins (B) in the cell lysates were determined by RT-PCR and immunoblotting, respectively.
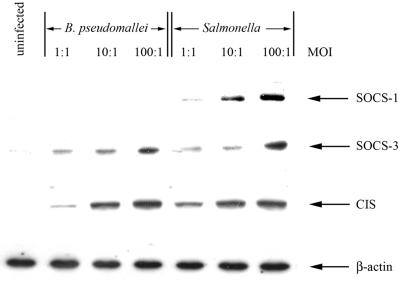
In order to determine if the expression of SOCSs by macrophages required viable bacteria, the cells were cocultured with heat-killed B. pseudomallei or S. enterica serovar Typhi at MOIs of 1:1, 10:1, and 100:1. After 8 h, the cells were harvested, and SOCS protein expression was assessed as described above. Figure 2 shows that exposure of macrophages to nonviable bacteria yielded SOCS and CIS expression patterns that were similar to those obtained with viable bacteria (Fig. 1B), suggesting that SOCS expression does not require active invasion. The level of SOCS3 protein expression directly correlated with the degree of stimulation (MOI). It should be noted that, unlike macrophages cocultured with S. enterica serovar Typhi, macrophages cocultured with killed B. pseudomallei showed no SOCS1 expression even at an MOI as high as 100:1.
FIG. 2.
Expression of SOCS protein in macrophages activated with killed bacteria. Mouse macrophages were treated with either killed B. pseudomallei or S. enterica serovar Typhi at MOIs of 1:1, 10:1, and 100:1. Eight hours later the treated cells were lysed, and the levels of SOCS proteins in the lysate were determined by immunoblotting.
Cytokine activation is not a prerequisite for B. pseudomallei-induced SOCS3 and CIS expression in macrophages.
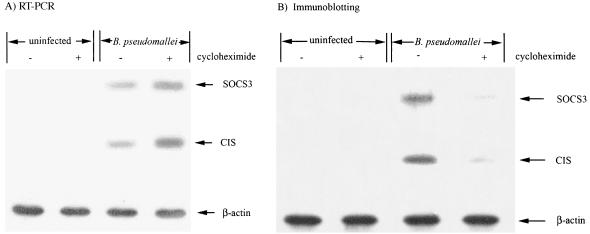
A number of cytokines, including interleukin-10 and tumor necrosis factor alpha (TNF-α), have been reported to have the ability to induce SOCS expression (23). We reported previously that TNF-α could be produced by macrophages infected with B. pseudomallei (38). In order to rule out the possibility that the observed SOCS expression was not related to prior cytokine production, similar experiments were performed in the presence of an inhibitor of protein synthesis, cycloheximide. Macrophages were pretreated with cycloheximide (5 μg/ml) for 1 h before infection, and the levels of SOCS3 and CIS mRNA were determined after 4 h of infection. It was found that the induction of SOCS3 and CIS mRNA expression was not affected by cycloheximide (Fig. 3A). However, the levels of SOCS proteins were markedly reduced in the presence of the inhibitor (Fig. 3B). This was not unexpected in view of the fact that cycloheximide is known to block protein synthesis in cells at the level of translation. It should be mentioned that cycloheximide at the concentration used in this experiment also inhibited TNF-α secretion by the B. pseudomallei-infected macrophages (data not shown). This raises the possibility that the expression of SOCS3 and CIS in B. pseudomallei-infected macrophages is not mediated through the cytokines produced prior to the time of SOCS induction and that B. pseudomallei may be able to directly activate SOCS3 and CIS expression in macrophages.
FIG. 3.
B. pseudomallei-induced SOCS3 and CIS mRNA expression in cycloheximide-treated macrophages. Cycloheximide (5 μg/ml) was added to a macrophage culture 1 h prior to infection. The pretreated macrophage culture was then infected with B. pseudomallei at an MOI of 2:1. The levels of expression of SOCS3 and CIS in the lysates of cycloheximide-treated and untreated infected macrophages were determined and compared by RT-PCR (A) at 4 h after infection and by immunoblotting (B) at 8 h after infection.
B. pseudomallei infection interferes with activation of Y701-STAT-1 phosphorylation.
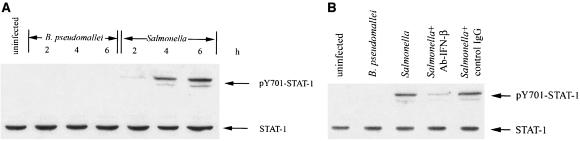
In order to determine whether B. pseudomallei could stimulate Y701-STAT-1 phosphorylation, macrophages were first infected with B. pseudomallei at an MOI of 2:1 and incubated for different times following the initial infection, and pY701-STAT-1 was then detected by immunoblotting. No phosphorylation of Y701-STAT-1 was observed in macrophages infected with B. pseudomallei, while pY701-STAT-1 was detected within 2 h in S. enterica serovar Typhi-infected macrophages (Fig. 4A). However, the presence of neutralizing antibody against IFN-β markedly reduced the level of pY701-STAT-1 in S. enterica serovar Typhi-infected macrophages (Fig. 4B). These results suggest that in S. enterica serovar Typhi-infected macrophages, the phosphorylation of Y701-STAT-1 was mediated through the production of IFN-β. Because B. pseudomallei is unable to induce IFN-β production (39), it is possible that the absence of an IFN-β signal is responsible for the inability to activate phosphorylation of Y701-STAT-1 in B. pseudomallei-infected cells. In fact, we have limited data for exogenous IFN-β that support the possibility described above (data not shown).
FIG. 4.
Failure of B. pseudomallei to induce Y701-STAT-1 phosphorylation. (A) Mouse macrophages were infected with either B. pseudomallei or S. enterica serovar Typhi at an MOI of 2:1. After various times, the levels of phosphorylation of Y701-STAT-1 in the infected cell lysates were determined by immunoblotting. pY701-STAT-1 could be detected only in the S. enterica serovar Typhi-infected macrophages. (B) Phosphorylation of Y701-STAT-1 in S. enterica serovar Typhi-infected macrophages depends on IFN-β production. Mouse macrophages were infected with S. enterica serovar Typhi at an MOI of 2:1 in the presence of neutralizing antibody against IFN-β (10 μg/ml). After 4 h of incubation, the infected cells were lysed, and the level of pY701-STAT-1 was analyzed by immunoblotting. IgG, immunoglobulin G.
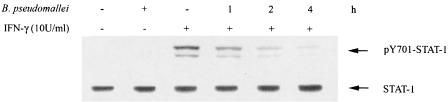
Exogenous IFN-γ added after B. pseudomallei infection fails to induce phosphorylation of Y701-STAT-1.
IFN-γ is known to play an essential role in macrophage activation by signaling through STAT-1 (32), and both SOCS3 and CIS have been reported to interfere with IFN-γ signaling by inhibiting Y701-STAT-1 phosphorylation (3). In order to determine whether induction of SOCS3 and CIS in B. pseudomallei-infected macrophages adversely affected their ability to respond to subsequent IFN-γ activation, the level of pY701-STAT-1 was monitored in B. pseudomallei-infected macrophages that were exposed to IFN-γ at 1, 2, and 4 h postinfection (Fig. 5). IFN-γ exposure at 1 h postinfection reduced the level of Y701-STAT-1 phosphorylation only slightly relative to the level in uninfected cells, while exposure at 2 and 4 h postinfection resulted in drastic reductions in the levels of pY701-STAT-1. It should be noted that the observed decrease in IFN-γ-induced Y701-STAT-1 phosphorylation in infected cells directly correlated with increased levels of SOCS3 and CIS, as shown in Fig. 1.
FIG. 5.
Failure of B. pseudomallei-infected macrophages to phosphorylate Y701-STAT-1 in response to IFN-γ stimulation. Mouse macrophages were infected with B. pseudomallei at an MOI of 2:1 and incubated for 1, 2, and 4 h before IFN-γ (10 U/ml) was added. The cells were then incubated for 1 h before the level of pY701-STAT-1 was determined by immunoblotting. Compared with the uninfected control culture, B. pseudomallei infection interfered with the macrophage response, particularly when the time between bacterial infections was prolonged (4 h).
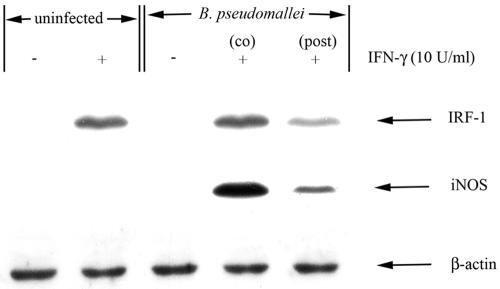
B. pseudomallei infection interferes with IRF-1 and iNOS expression in macrophages stimulated with IFN-γ.
We previously demonstrated that IRF-1 and iNOS played an important role in regulating the bactericidal activity of macrophages against B. pseudomallei (38, 39). Induction of both IRF-1 and iNOS expression in uninfected cells is known to require prior phosphorylation of Y701-STAT-1 (15, 34). Therefore, it was of interest to determine if the depressed pY701-STAT-1 level in B. pseudomallei-infected macrophages (Fig. 4) influenced the expression of IRF-1 and iNOS. In order to address this question, IFN-γ was added to macrophage cultures either at the time of infection (costimulation) or 4 h after infection (poststimulation). IRF-1 and iNOS expression was then determined 4 h after the addition of IFN-γ. Consistent with our previous report (40), IFN-γ exposure alone was able to activate IRF-1 expression but not iNOS expression in uninfected cells (Fig. 6). While B. pseudomallei infection alone in the absence of IFN-γ failed to activate expression of IRF-1 and iNOS, the expression was observed when IFN-γ was added to the cells at the time of infection (Fig. 6). However, the levels of both IRF-1 and iNOS were noticeably reduced when IFN-γ was added 4 h after the cells were infected. These results suggested that the host cell response to IFN-γ was suppressed in B. pseudomallei-infected macrophages and that the suppression required time to become established. The suppression of both IRF-1 and iNOS correlated with both the decrease in the pY701-STAT-1 level shown in Fig. 5 and the increased expression of SOCS3 and CIS shown in Fig. 1.
FIG. 6.
Failure of B. pseudomallei-infected macrophages to activate IRF-1 and iNOS expression in response to postinfection IFN-γ stimulation. Mouse macrophages were infected with B. pseudomallei at an MOI of 2:1 as described in Materials and Methods. In the postinfection stimulation (post) experiment, IFN-γ (10 U/ml) was added 4 h after the cells were infected with B. pseudomallei. The infected cell cultures were incubated for one more hour before excess IFN-γ was removed. The cell cultures were then incubated for a further 3 h, the macrophages were lysed, and the levels IRF-1 and iNOS in the lysates were determined by immunoblotting. For the costimulation (co) experiment, the macrophages were infected with B. pseudomallei in the presence of IFN-γ (10 U/ml). After 1 h of incubation, the macrophages were washed three times with PBS and cultured for three more hours before the levels of IRF-1 and iNOS in the cell lysate were determined by immunoblotting.
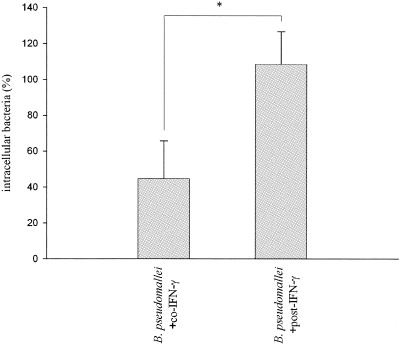
Inability of IFN-γ to enhance killing of intracellular B. pseudomallei in infected macrophages.
Previously, we demonstrated that exogenous IFN-γ, when added to macrophages either prior to or at the time of B. pseudomallei infection, could significantly enhance killing of intracellular B. pseudomallei, suggesting that this effect was likely attributable to the enhanced production of iNOS (40). It was of interest to determine if postinfection incubation had any effect on the observed IFN-γ-induced enhanced killing. Costimulation and poststimulation of infected macrophages with IFN-γ were performed as described previously (Fig. 6), except that the number of viable intracellular bacteria was determined 4 h after IFN-γ addition. Addition of IFN-γ 4 h after infection failed to enhance the intracellular killing of B. pseudomallei. Viable intracellular B. pseudomallei levels were significantly higher in cells that were subjected to poststimulation with IFN-γ than in cells that were costimulated at the time of infection (Fig. 7). The failure of IFN-γ to stimulate killing of intracellular B. pseudomallei when it was added to macrophages at 4 h postinfection correlated well with the reduced IRF-1 and iNOS expression shown in Fig. 6.
FIG. 7.
Inability of IFN-γ to enhance antimicrobial activity of B. pseudomallei-infected macrophages. The experimental protocol for this experiment was similar to that described in the legend to Fig. 6, except that the viability of intracellular bacteria was determined and the results of poststimulation and costimulation conditions were compared. The data indicate the means and standard deviations of three separate experiments, each carried out in duplicate. The asterisk indicates that the P value is <0.01, as determined by Student's t test.
DISCUSSION
The induction of SOCS expression and its significance have been extensively studied in recent years. For example, Leishmania donovani-infected macrophages were reported to induce SOCS3 expression that resulted in suppression of macrophage activation (4). Activation of SOCS3 expression has also been reported in macrophages infected with gram-positive bacteria (e.g., L. monocytogenes and Staphylococcus aureus) (4, 35). Induction of SOCS proteins by isolated bacterial components like LPS has also been demonstrated; however, very limited information on the regulation of these proteins in response to infection with gram-negative bacteria is currently available (7). This study clearly demonstrated that there is a novel association between the intracellular gram-negative bacterium B. pseudomallei and the induction of SOCS3 and CIS expression in an in vitro mouse macrophage model (Fig. 1). Expression of both SOCS3 and CIS mRNA was not affected in the presence of cycloheximide, suggesting that B. pseudomallei itself, and not the cytokines that it induced, was able to directly induce mRNA expression of these negative regulators (Fig. 3). This finding is reinforced by the fact that cycloheximide at the concentration used was found to interfere with neither invasion nor intracellular replication of B. pseudomallei (data not shown). However, it was found that unlike other gram-negative bacteria, such as S. enterica serovar Typhi, B. pseudomallei failed to induce SOCS1 expression (Fig. 1), suggesting that the mechanisms employed by these different gram-negative bacteria to modulate the macrophage response are different. Moreover, it appears that the induction of these negative regulators, at least in the B. pseudomallei system, did not require active invasion since the macrophage responses to viable and nonviable bacteria were similar (Fig. 2). This finding is in accord with the results from other studies showing that purified LPS from other bacteria could also activate SOCS expression (3, 7, 34). It is possible that the type of SOCS response to different gram-negative bacteria, as demonstrated for S. enterica serovar Typhi and B. pseudomallei in the present study, is related to differences in LPS structure. For example, LPS isolated from B. pseudomallei is known to have an unusual chemical structure in the acid-stable inner core region attached to the lipid A moiety (20). This unusual LPS structure has also been shown to be a weak macrophage activator compared with the LPS isolated from other gram-negative bacteria, such as S. enterica serovar Typhi and Escherichia coli (20, 37). It is tempting, therefore, to speculate that the cellular response associated with the expression of different SOCS proteins depends partly on signals generated from different pattern recognition receptors. The participation of a Toll-like receptor (TLR) in SOCS expression has received considerable attention recently. For example, it was reported that SOCS1-deficient mice exhibited increased LPS sensitivity and decreased endotoxin tolerance (22), suggesting that SOCS protein might be involved in TLR signaling. It was subsequently demonstrated that the induction of SOCS3 and CIS, but not the induction of SOCS1, was MyD88 dependent (3). The ability of B. pseudomallei to induce SOCS3 and CIS but not SOCS1, together with its failure to stimulate IFN-β production (39), is consistent with the possibility that B. pseudomallei may also activate macrophages via a MyD88-dependent pathway. The type(s) of TLR and/or non-TLR involved in the activation of macrophages has not been defined yet and is currently being investigated in our laboratory.
The pivotal role of the transcription factor STAT-1 in the innate immune response against microbial infection is well documented (12). STAT-1-deficient mice are highly sensitive to stimulation by intact organisms or isolated individual components (28). Increased susceptibility to intracellular bacteria, such as Mycobacterium, has also been observed in STAT-1-deficient human macrophages (14). Purified LPS has also been shown to activate phosphorylation of Y701-STAT-1 through TLR, and this correlated with IFN-β synthesis, suggesting that the activation of pY701-STAT-1 is mediated through type I IFN synthesized by LPS-activated cells (10, 24). The data presented in this study which demonstrated that the gram-negative bacterium S. enterica serovar Typhi was able to activate Y701-STAT-1 phosphorylation after only 2 h of infection and that the process could be inhibited by neutralizing antibody against IFN-β (Fig. 4) lend support to this idea. In contrast to S. enterica serovar Typhi, B. pseudomallei failed to stimulate pY701-STAT-1 (Fig. 4), a result that was consistent with the organism's inability to activate IFN-β production (39). In addition to IFN-β, IFN-γ could also activate phosphorylation of STAT-1. Activation of this transcription factor is known to regulate SOCS1 expression (16). By contrast, STAT-1-deficient mice could still activate SOCS3 expression in response to IFN-γ stimulation, suggesting that SOCS3 gene regulation does not involve activation of STAT-1 (16). It is possible that the inability of B. pseudomallei to activate SOCS1 expression in our study was also related to its inability to activate phosphorylation of STAT-1 (Fig. 1 and 4).
Of the different SOCS members that have been studied, SOCS1 is probably the most potent inhibitor of IFN signaling, and it acts by suppressing the phosphorylation of STAT-1 (5, 22). SOCS3, on the other hand, is known to play an essential role as a negative inhibitor of interleukin-6, possibly by interfering with the activation of another transcription factor, STAT-3 (8, 25, 44). Based on the data from the STAT-1 phosphorylation studies presented here, it appeared that SOCS3 and CIS could also inhibit IFN-γ signaling, albeit to a lesser extent than they could with STAT-3 (3, 10). Macrophages infected with L. monocytogenes also exhibited diminishing IFN-γ-induced Y701-STAT-1 phosphorylation (35). A decreased response to IFN-γ signaling in L. monocytogenes- and L. donovani-infected macrophages correlated with the induction of SOCS3 expression (4, 35). In the present study, we demonstrated that the gram-negative bacterium B. pseudomallei interfered with IFN-γ-induced Y701-STAT-1 phosphorylation in a mouse macrophage system (Fig. 5). The suppression of STAT-1 phosphorylation also directly correlated with the expression of SOCS3 and CIS (Fig. 1). On the basis of all of the results, it is tempting to conclude that activation of SOCS3 and CIS expression in response to B. pseudomallei infection can interfere with IFN-γ signaling, thus resulting in suppression of IFN-γ-inducing proteins (e.g., IRF-1 and iNOS expression) (Fig. 6). Both IRF-1 and iNOS are known to play a crucial role in controlling the fate of intracellular pathogens (27, 36). In the present study, B. pseudomallei-infected macrophages not only failed to express both IRF-1 and iNOS but also failed to eliminate intracellular B. pseudomallei (Fig. 7).
During the last few years, our group has been working on elucidating the mechanism by which B. pseudomallei modulates the innate host defense, thus allowing it to survive inside macrophages (38, 39). This intracellular bacterium can invade macrophages without stimulating IFN-β production, which is an essential factor for IRF-1 and iNOS expression (39). Failure to activate IRF-1 and iNOS provides the bacteria with the means to survive the antimicrobial activity of macrophages (38, 39). However, exogenous IFN-γ or IFN-β added prior to or at the time of infection could enhance both IRF-1 and iNOS expression and restore antimicrobial activity of these macrophages (40). The protective role of IFN-γ in the host defense against B. pseudomallei has been observed previously in animal models (31). Administration of neutralizing antibody against IFN-γ could significantly lower the 50% lethal dose and also increase bacterial burdens in the liver and spleen of these animals (31). More recently, we demonstrated that the IFN-γ level in the serum of infected BALB/c mice was significantly higher than that in the serum of uninfected mice, yet the high level of IFN-γ failed to eliminate the bacteria from the blood, spleen, liver, and lungs and these animals subsequently died over the next 7 to 10 days (42). The data for this animal model are in accord with the elevated level of IFN-γ noted in patients with severe melioidosis (26). Together, these results suggest that the presence of high IFN-γ levels during ongoing B. pseudomallei infection is not sufficient to control the infection or to eliminate the bacteria from the infected host. The failure of IFN-γ to protect the animals from fatal sepsis (42) could be explained by the ability of B. pseudomallei to activate negative regulator proteins, such as SOCS3 and CIS, as demonstrated in the present study. The expression of these proteins can interfere with IFN-γ signaling via a STAT-1 pathway, making the infected macrophages unable to respond to IFN-γ. This, in turn, results in an inability to activate IFN-γ-responsive protein expression (i.e., IRF-1 and iNOS). Therefore, in addition to interference with proinflammatory cytokine production and antimicrobial activity, the results obtained in the present study provided evidence for another possible mechanism by which B. pseudomallei could modulate the macrophage bactericidal response, thus facilitating its intracellular survival, and may also explain the persistence of the organism in the human host and the high rate of relapse in melioidosis.
Acknowledgments
This work was supported by research grants from the Thailand Research Fund (TRF).
We appreciate the kind suggestions from James Dubbs (Chulabhorn Research Institute, Bangkok, Thailand) during preparation of the manuscript.
Editor: J. B. Bliska
REFERENCES
- 1.Alexander, W., and D. Hilton. 2004. The role of suppressor of cytokine signaling (SOCS) proteins in regulation of the immune response. Annu. Rev. Immunol. 22:503-529. [DOI] [PubMed] [Google Scholar]
- 2.Anuntagool, N., P. Intachote, V. Wuthiekanun, N. J. White, and S. Sirisinha. 1998. Lipopolysaccharide from nonvirulent Ara+ Burkholderia pseudomallei isolates is immunologically indistinguishable from lipopolysaccharide from virulent Ara− clinical isolate. Clin. Diagn. Lab. Immunol. 5:225-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baetz, A., M. Frey, K. Heeg, and A. Dalpke. 2004. Suppressor of cytokine signaling (SOCS) proteins indirectly regulate Toll-like receptor signaling in innate immune cells. J. Biol. Chem. 279:54708-54715. [DOI] [PubMed] [Google Scholar]
- 4.Bertholet, S., H. L. Dickensheets, F. Sheikh, A. A. Gam, R. P. Donnelly, and R. T. Kenny. 2003. Leishmania donovani-induced expression of suppressor of cytokine signaling 3 in human macrophages: a novel mechanism for intracellular parasite suppression of activation. Infect. Immun. 71:2095-2101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brysha, M., J. G. Zhang, P. Bertolino, J. E. Corbin, W. S. Alexander, N. A. Nicola, D. J. Hilton, and R. Starr. 2001. Suppressor of cytokine signaling-1 attenuates the duration of interferon γ signal transduction in vitro and in vivo. J. Biol. Chem. 276:22086-22089. [DOI] [PubMed] [Google Scholar]
- 6.Cooney, R. N. 2002. Suppressors of cytokine signaling (SOCS): inhibitors of the JAK/STAT pathway. Shock 17:83-90. [DOI] [PubMed] [Google Scholar]
- 7.Crespo, A., M. B., Filla, and W. J. Murphy. 2002. Low responsiveness to IFN-γ, after pretreatment of mouse macrophages with lipopolysaccharides, develops via diverse regulatory pathways. Eur. J. Immunol. 32:710-719. [DOI] [PubMed] [Google Scholar]
- 8.Croker, B. A., D. L. Krebs, J. G. Zhang, S. Wormald, T. A. Willson, E. G. Stanley, L. Robb, C. J. Greenhalgh, R. Forster, B. E. Clausen, N. A. Nicola, D. Metcalf, D. J. Hilton, A. W. Roberts, and W. S. Alexander. 2003. SOCS3 negatively regulates IL-6 signaling in vivo. Nat. Immunol. 4:540-545. [DOI] [PubMed] [Google Scholar]
- 9.Dalpke, A. H., S. Opper, S. Zimmermann, and K. Heeg. 2001. Suppressors of cytokine signaling (SOCS)-1 and SOCS-3 are induced by CpG-DNA and modulate cytokine responses in APCs. J. Immunol. 166:7082-7089. [DOI] [PubMed] [Google Scholar]
- 10.Dalpke, A., S. Eckerle, M. Frey, and K. Heeg. 2003. Triggers of Toll-like receptor modulate IFN-γ signaling: involvement of serine 727 STAT1 phosphorylation and suppressors of cytokine signal. Eur. J. Immunol. 33:1776-1787. [DOI] [PubMed] [Google Scholar]
- 11.Decker, T., P. Kovarik, and A. Meinke. 1997. Gas elements: a few nucleotides with a major impact on cytokine-induced gene expression. J. Interferon Cytokine Res. 17:121-134. [DOI] [PubMed] [Google Scholar]
- 12.Decker, T., S. Stockinger, M. Karaghiosoff, M. Muller, and P. Kovarik. 2002. IFNs and STATs in innate immunity to microorganism. J. Clin. Investig. 109:1271-1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dhrarakul, T., and S. Songsivilai. 1999. The many facets of melioidosis. Trends Microbiol. 7:138-146. [DOI] [PubMed] [Google Scholar]
- 14.Dupuis, S., C. Dargemont, C. Fieschi, N. Thomassin, S. Rosenzweig, J. Harris, S. M. Holland, R. D. Schrieber, and J. L. Casanova. 2001. Impairment of mycobacterial but not viral immunity by a germline human STAT-1 mutation. Science 293:300-303. [DOI] [PubMed] [Google Scholar]
- 15.Gao, J., D. C. Morrison, T. J. Parmely, S. W. Russell, and W. J. Murphy. 1997. An interferon-gamma-activated site (GAS) is necessary for full expression of the mouse iNOS gene in response to interferon-gamma and lipopolysaccharide. J. Biol. Chem. 272:1226-1230. [DOI] [PubMed] [Google Scholar]
- 16.Gil, M. P., E. Bohn, A. K. O'Guin, C. V. Ramana, B. Levine, G. R. Stark, H. W. Virgin, and R. D. Schreiber. 2001. Biologic consequences of Stat1-independent IFN signaling. Proc. Natl. Acad. Sci. USA 98:6680-6685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harada, H., E. Takahashi, S. Itoh, K. Harada, T. Hori, and T. Taniguchi. 1994. Structure and regulation of the human interferon regulatory factor 1 (IRF-1) and IRF-2 genes: implication for a gene network in the interferon system. Mol. Cell. Biol. 14:1500-1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harley, V. S., D. A. B. Dance, B. J. Drasar, and G. Tovey. 1998. Effects of Burkholderia pseudomallei and other Burkholderia species on eukaryotic cells in tissue culture. Microbios 96:71-93. [PubMed] [Google Scholar]
- 19.Jones, A. L., T. J. Beveridge, and D. E. Woods. 1996. Intracellular survival of Burkholderia pseudomallei. Infect. Immun. 64:782-790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kawahara, K., S. Dejsirilert, H. Danbara, and T. Ezaki. 1992. Extraction and characterization of lipopolysaccharide from Pseudomonas pseudomallei. FEMS Microbiol. Lett. 96:129-134. [DOI] [PubMed] [Google Scholar]
- 21.Kespichayawattana, W., S. Rattanachetkul, T. Wanun, P. Utaisincharoen, and S. Sirisinha. 2000. Burkholderia pseudomallei induces cell fusion and actin-associated membrane protrusion: a possible mechanism for cell-to-cell spreading. Infect. Immun. 68:5377-5384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kinjyo, I., T. Hanada, K. Inagabi-Ohara, H. Mori, D. Aki, et al. 2002. SOCS1/JAB is a negative regulator of LPS-induced macrophage activation. Immunity 17:583-591. [DOI] [PubMed] [Google Scholar]
- 23.Kovanen, P. E., and W. J. Leonard. 1999. Inhibitors keep cytokines in check. Curr. Biol. 9:R899-R902. [DOI] [PubMed] [Google Scholar]
- 24.Kovarik, P., D. Stoiber, M. Novy, and T. Decker. 1998. Stat1 combines signals derived from IFN-γ and LPS receptors during macrophage activation. EMBO J. 17:3660-3668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lang, R. A. L. Pauleau, E. Parganas, Y. Takahashi, J. Mages, J. N. Ihle, R. Rutschman, and P. J. Murray. 2003. SOCS3 regulates the plasticity of gp130 signaling. Nat. Immunol. 4:546-550. [DOI] [PubMed] [Google Scholar]
- 26.Lauw, F. N., A. J. Simpson, J. M. Prins, M. D. Smith, M. Kurimoto, S. J. van Deventer, P. Speelman, W. Chaowagul, N. J. White, and T. van der Poll. 1999. Elevated plasma concentrations of interferon (IFN)-gamma and the IFN-gamma-inducing cytokines interleukin (IL)-18, IL-12, and IL-15 in severe melioidosis. J. Infect. Dis. 180:1878-1885. [DOI] [PubMed] [Google Scholar]
- 27.Martin, E., C. Nathan, and Q. W. Xie. 1994. Role of interferon regulatory factor 1 in induction of nitric oxide synthase. J. Exp. Med. 180:977-984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meraz, M. A., J. M. White, K. C. Sheehan, E. A. Bach, S. J. Rodig, A. S. Dighe, D. H. Kaplan, J. K. Riley, A. C. Greenlund, D. Campbell, K. Carver-Moore, R. N. DuBois, R. Clark, M. Aguet, and R. D. Schreiber. 1996. Targeted disruption of the Stat 1 gene in mice reveals unexpected physiologic specificity in the JAK-STAT signaling pathway. Cell 84:431-442. [DOI] [PubMed] [Google Scholar]
- 29.Miyaki, K., K. Kawakami, and A. Saito. 1997. Role of reactive nitrogen and oxygen intermediates in gamma interferon-stimulated murine macrophage bactericidal activity against Burkholderia pseudomallei. Infect. Immun. 67:4108-4113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nakagawa, R., T. Naka, H. Tsutshui, M. Fujimoto, A. Kimura, et al. 2002. Socs-1 participate in negative regulation of LPS responses. Immunity 17:677-687. [DOI] [PubMed] [Google Scholar]
- 31.Santanirand, P., V. S. Harley, D. A. B. Dance, B. S. Drasar, and G. J. Bancroft. 1999. Obligatory role of gamma interferon for host survival in murine model of infection with Burkholderia pseudomallei. Infect. Immun. 67:3593-3600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schindler, C., and J. E. Darnell, Jr. 1995. Transcriptional responses to polypeptide ligands: the JAK-STAT pathway. Annu. Rev. Biochem. 64:621-651. [DOI] [PubMed] [Google Scholar]
- 33.Song, M., and K. Shuai. 1998. The suppressor of cytokine signaling (SOCS)1 and SOCS3 but not SOCS2 proteins inhibit interferon-mediated antiviral and antiproliferation activity. J. Biol. Chem. 273:35056-35062. [DOI] [PubMed] [Google Scholar]
- 34.Stoiber, D., P. Kovarik, S. Cohney, J. Johnston, P. Steinlein, and T. Decker. 1999. Lipopolysaccharide induces in macrophages the synthesis of the suppressor of cytokine signaling 3 and suppresses signal transduction in response to the activating factor IFN-gamma. J. Immunol. 163:2640-2647. [PubMed] [Google Scholar]
- 35.Stoiber, D., S. Stockinger, P. Steinlein, J. Kovarik, and T. Decker. 2001. Listeria monocytogenes modulates macrophage cytokine responses through STAT serine phosphorylation and the induction of suppressor of cytokine signaling 3. J. Immunol. 166:466-472. [DOI] [PubMed] [Google Scholar]
- 36.Taniguchi, T., K. Ogasawara, A. Takaoka, and N. Tanaka. 2001. IRF family of transcription factors as regulators of host defense. Annu. Rev. Immunol. 19:623-655. [DOI] [PubMed] [Google Scholar]
- 37.Utaisincharoen, P., N. Tangthawornchaikul, W. Kespichayawattana, N. Anuntagool, P. Chaisuriya, and S. Sirisinha. 2000. Kinetic studies of the production of nitric oxide (NO) and tumor necrosis factor alpha (TNF-α) in macrophages stimulated with Burkholderia pseudomallei endotoxin. Clin. Exp. Immunol. 122:324-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Utaisincharoen, P., N. Tangthawornchaikul, W. Kespichayawattana, P. Chaisuriya, and S. Sirisinha. 2001. Burkholderia pseudomallei interferes with inducible nitric oxide synthase (iNOS) production: a possible mechanism of evading macrophage killing. Microbiol. Immunol. 45:307-313. [DOI] [PubMed] [Google Scholar]
- 39.Utaisincharoen, P., N. Anuntagool, K. Limposuwan, P. Chaisuriya, and S. Sirisinha. 2003. Involvement of beta interferon in enhancing inducible nitric oxide synthase production and antimicrobial activity of Burkholderia pseudomallei-infected macrophages. Infect. Immun. 71:3053-3057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Utaisincharoen, P., N. Anuntagool, S. Arjcharoen, K. Limposuwan, P. Chaisuriya, and S. Sirisinha. 2004. Induction of iNOS expression and antimicrobial activity by interferon (IFN)-β is distinct from IFN-γ in Burkholderia pseudomallei-infected mouse macrophages. Clin. Exp. Immunol. 136:277-283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.White, N. 2003. Melioidosis. Lancet 361:1715-1722. [DOI] [PubMed] [Google Scholar]
- 42.Wongratanacheewin, S., W. Kespichayawattana, P. Intachote, S. Pichyangkul, R. W. Sermswan, A. M. Krieg, and S. Sirisinha. 2004. Immunostimulatory CpG oligodeoxynucleotide confers protection in a murine model of infection with Burkholderia pseudomallei. Infect. Immun. 72:4494-4502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wuthiekanun, V., M. D. Smith, D. A. B. Dance, A. L. Walsh, T. L. Pitt, and N. J. White. 1996. Biochemical characteristics of clinical and environmental isolates of Burkholderia pseudomallei. J. Med. Microbiol. 45:408-412. [DOI] [PubMed] [Google Scholar]
- 44.Yasukawa, H., M. Ohishi, H. Mori, M. Murakami, T. Chinen, D. Aki, T. Hanada, K. Takeda, S. Akira, M. Hoshijima, T. Hirano, K. R. Chien, and A. Yoshimura. 2003. IL-6 induces an anti-inflammatory response in the absence of SOCS3 in macrophages. Nat. Immunol. 4:551-556. [DOI] [PubMed] [Google Scholar]