Abstract
Pulmonary infection with the bacterium Yersinia pestis causes pneumonic plague, an often-fatal disease for which no vaccine is presently available. Antibody-mediated humoral immunity can protect mice against pulmonary Y. pestis infection, an experimental model of pneumonic plague. Little is known about the protective efficacy of cellular immunity. We investigated the cellular immune response to Y. pestis in B-cell-deficient μMT mice, which lack the capacity to generate antibody responses. To effectively prime pulmonary cellular immunity, we intranasally vaccinated μMT mice with live replicating Y. pestis. Vaccination dramatically increased survival of μMT mice challenged intranasally with a lethal Y. pestis dose and significantly reduced bacterial growth in pulmonary, splenic, and hepatic tissues. Vaccination also increased numbers of pulmonary T cells, and administration of T-cell-depleting monoclonal antibodies at the time of challenge abrogated vaccine-induced survival. Moreover, the transfer of Y. pestis-primed T cells to naive μMT mice protected against lethal intranasal challenge. These findings establish that vaccine-primed cellular immunity can protect against pulmonary Y. pestis infection and suggest that vaccines promoting both humoral and cellular immunity will most effectively combat pneumonic plague.
Infectious plague has afflicted mankind throughout recorded history (30). Fleas transmit the bubonic form of plague, which is characterized by painfully swollen lymph nodes (buboes) and can progress to the more deadly septicemic and pneumonic forms. At the pneumonic stage, plague can be directly transmitted from person to person via aerosolized respiratory droplets, thereby causing primary pneumonic plague, a rapidly progressing and often-fatal disease.
The etiologic agent of plague is the gram-negative bacterium Yersinia pestis (30). If diagnosed early, plague can often be treated successfully with antibiotics. However, multiple-antibiotic-resistant isolates of Y. pestis exist (12), and it is well documented that military scientists have devised means to aerosolize Y. pestis (39). Thus, there is concern that antibiotic-resistant Y. pestis may be exploited as a bioweapon.
Over a century of research effort has thus far failed to produce a safe and effective pneumonic plague vaccine (25, 39). Early plague vaccine researchers focused on the more common bubonic form of plague. Haffkine described a vaccine composed of heat-killed cultures of virulent Y. pestis organisms in 1897 (14). Although it was efficacious against bubonic plague (37), an unacceptably high frequency of adverse reactions limited acceptance of Haffkine's vaccine (25). In 1904, Kolle and Otto found that inoculating rodents with live attenuated Y. pestis strains protected them against challenge infections with fully virulent strains (20). Shortly thereafter, Strong established the safety and efficacy of these live attenuated strains in humans (35, 36). However, the attenuated vaccine strains occasionally increased in virulence upon passage through animals and often evoked adverse reactions in humans (25). Therefore, they were not considered suitable for use in the United States, where, rather, formalin-killed whole-cell Y. pestis vaccines were developed. One version of the formalin-killed vaccine, designated the “plague vaccine, USP,” was widely used by U.S. military personnel during the Vietnam War, where evidence suggests that it was significantly less reactogenic than Haffkine's heat-killed vaccine yet still protected against bubonic plague (24). However, animal studies indicate that formalin-killed vaccines do not protect well against pulmonary Y. pestis infection (2, 10, 15), and humans vaccinated with formalin-killed vaccines have contracted pneumonic plague (9, 25, 39).
Modern-day pneumonic plague vaccine efforts are largely focused upon the development of subunit vaccines comprised of recombinant Y. pestis proteins (39). The fraction 1 (F1) and V proteins have received the most attention, as vaccination with their recombinant forms protects mice against pneumonic plague (1, 2, 40). The U.S. Army Medical Research Institute for Infectious Diseases (USAMRIID) has developed a recombinant F1-V fusion protein vaccine that protects mice well (15) but does not fully protect nonhuman primates against pneumonic plague (M. L. Pitt, Animal Models and Correlates of Protection for Plague Vaccines Workshop, Gaithersburg, MD, 13 to 14 October 2004, http://www.fda.gov/cber/minutes/workshop-min.htm). The suboptimal performance of the F1-V vaccine in primates warrants further attempts to improve pneumonic plague vaccine efficacy.
Both humoral and cellular immune responses can potentially contribute to vaccine efficacy (41). Humoral immunity relies upon B-cell production of antibodies and effectively neutralizes extracellular pathogens and toxins, while cellular immunity relies upon the cytolytic and cytokine-producing capacities of T cells and is particularly effective at eradicating intracellular pathogens. Vaccines composed of either killed organisms, such as the USP vaccine, or purified proteins admixed with suitable adjuvants, such as USAMRIID's F1-V fusion protein vaccine, readily prime humoral immunity (15, 25). In contrast, vaccines comprised of replicating agents, such as live attenuated versions of virulent pathogens, most effectively prime cellular immunity (22).
Given that the current formulations of the USP and F1-V vaccines elicit strong humoral immunity yet fail to fully protect against pneumonic plague, we investigated whether cellular immunity can also contribute to plague vaccine efficacy. To specifically focus on cellular immunity, we took advantage of B-cell-deficient μMT mice, which lack the capacity to mount antibody responses (19). We report that μMT mice can be vaccinated with live Y. pestis in a manner that enables them to resist a lethal pulmonary challenge and that the observed protection is abrogated by treatment with T-cell-depleting monoclonal antibodies (MAb). Moreover, the transfer of Y. pestis-primed T cells to naive μMT mice protects against lethal intranasal Y. pestis challenge. These findings demonstrate that vaccine-primed cellular immunity can protect against pulmonary Y. pestis infection and suggest that pneumonic plague vaccine efforts will benefit from incorporating the protective capacities of cellular immunity.
MATERIALS AND METHODS
Mice.
Wild-type C57BL/6 mice and C57BL/6-backcrossed B-cell-deficient μMT mice, 6 to 8 weeks of age, were purchased from Jackson Laboratory (Bar Harbor, ME) or were bred at the Trudeau Institute. Animals were housed at the Trudeau Institute experimental animal facility and cared for according to the Trudeau Institute Animal Care and Use Committee guidelines.
Infections.
For all experiments, mice were infected with Y. pestis strain KIM D27 (21), a pigmentation-negative strain that was generously provided by Robert Brubaker (Michigan State University). The pigmentation-negative phenotype results from a 102-kb chromosomal deletion that somewhat attenuates Y. pestis, particularly when administered via the subcutaneous route (30). KIM D27 was grown in brain heart infusion broth at 26°C, and infectious stocks were stored as single use aliquots at −70°C after resuspension in the same medium supplemented with 20% glycerol. In our hands, the median lethal dose of this stock was approximately 1 × 103 CFU when administered via the intraperitoneal route and 1 × 104 CFU when administered via the intranasal route, as calculated by the method of Reed and Muench (31). To generate sera for adoptive immunotherapy, C57BL/6 mice were intraperitoneally inoculated with 3 × 102 CFU KIM D27 and sera were collected from surviving mice at 30 days postinfection. These convalescent-phase sera were pooled, aliquoted, and stored at −20°C. For vaccinations, μMT mice were intranasally inoculated with 2 × 105 CFU KIM D27, and 10 μl convalescent-phase serum was intraperitoneally administered 18 h later. Vaccinated animals received chow supplemented with 67 mg/g sulfadiazine and 333 mg/g trimethoprim (Uniprim diet; Harlan TEKLAD, Madison, WI) at 2 weeks postvaccination and were so maintained until day 55 postvaccination, at which time they were returned to antibiotic-free chow. This antibiotic treatment ensured that the immunocompromised μMT mice did not inadvertently become infected with environmental pathogens prior to challenge infection. To challenge the mice, animals were intranasally infected with 2 × 105 CFU KIM D27 at day 60 postvaccination. Where indicated, animals were treated with 1 mg monoclonal antibodies specific for mouse CD4 (clone GK1.5) and/or CD8 (clone 2.43), administered as two intraperitoneal doses of 500 μg each on the day before and the day of challenge. These antibodies were purchased from BioExpress (West Lebanon, NH). Control animals received an isotype-matched (rat immunoglobulin G2b, clone LTF.2) antibody. In all survival experiments, unresponsive recumbent animals were considered moribund and were euthanatized.
Measurement of CFU and lymphocyte numbers in tissue.
At the indicated days after initiating infections, mice were euthanized by carbon dioxide narcosis. Spleens and livers were mechanically disrupted and plated for CFU determination. Lungs were perfused with ice-cold saline containing heparin, minced in ice-cold Dulbecco's modified Eagle's medium (DMEM) (Mediatech-Cellgro, Herndon, VA), and then incubated in DMEM containing collagenase IX (0.7 mg/ml) (Sigma Aldrich, St. Louis, MO) and DNase (30 μg/ml) (Sigma Aldrich) at 37°C for 30 min. A single-cell suspension was then obtained by passing the digested lung tissue through a 70-μm nylon tissue strainer (BD Falcon, Bedford, MA). An aliquot was plated for CFU determination, and the remaining cells were counted and prepared for flow cytometry by blocking Fcγ receptors by treatment with MAb 2.4G2 and then staining of cells with fluorochrome-conjugated MAb (all from BD PharMingen) specific for CD4 (clone RM4-5), CD8 (clone 53.6-7), and/or CD44 (clone IM7). Just prior to flow cytometric analysis, the cells were stained with propidium iodide, and only viable propidium iodide-negative cells were quantified.
T-cell transfers.
Cells for adoptive transfer were harvested from μMT mice that had survived vaccination and challenge infections. Three months after the challenge infection, cells were isolated from collagenase-digested lung (as above) and splenic tissues, pooled, and cultured at 5 × 106 cells/ml in DMEM supplemented with 10% fetal bovine serum, 25 mM HEPES, 2 mM glutamine, 100 units/ml penicillin, 100 μg/ml streptomycin, 1 mM sodium pyruvate, 55 μM beta-mercaptoethanol, and approximately 1 × 108 CFU heat-killed (56°C for 60 min) KIM D27 Y. pestis, which had been grown overnight at 37°C in defined medium containing calcium (11). Two days after the initiation of culture, an equal volume of medium containing 20 units/ml recombinant human interleukin-2 (IL-2) was added. Subsequently, the cultures were expanded with IL-2-containing medium as necessary to maintain viable cell densities of fewer than 1 × 106 cells/ml. Seven days after the initiation of culture, the cells were transferred to medium lacking IL-2 and left for 3 days. They were then washed with phosphate-buffered saline, counted, and intravenously injected (5 × 106 viable cells/mouse) into recipient animals, which were challenged with Y. pestis the following day. Flow cytometric analysis established that these cells were approximately 60% CD4 positive and 25% CD8 positive at the time of transfer.
Statistics.
Statistical analyses were performed using the program Prism 4.0 (GraphPad Software, Inc.), employing Student's t tests for parametric data, Mann-Whitney tests for nonparametric data, and log rank tests for survival data.
RESULTS
B-cell-deficient μMT mice can be safely exposed to live Y. pestis in conjunction with passive serotherapy.
In the early 1900s, Kolle and Otto found that guinea pigs, which are highly susceptible to plague, could be most effectively vaccinated against Y. pestis infection if they were inoculated with a lethal dose of live Y. pestis and then protected from vaccination-induced lethality by the administration of convalescent-phase sera (i.e., sera that had been obtained from animals that had survived a prior Y. pestis infection) (20). As replicating agents well prime cellular immunity, we hypothesized that this vaccination protocol of live Y. pestis with serotherapy primed robust cellular immunity. To adapt the protocol for use in mice, we first evaluated the susceptibility of C57BL/6 mice to Y. pestis strain KIM D27. As shown in Fig. 1, 100% of C57BL/6 mice succumbed to 1 × 104 or 1 × 105 CFU KIM D27 following intraperitoneal or intranasal administration, respectively. We then generated convalescent-phase sera for passive serotherapy studies by intraperitoneally infecting cohorts of C57BL/6 mice with 3 × 102 CFU KIM D27 and collecting sera at day 30 postinfection. As shown in Fig. 2A, as little as 10 μl of convalescent-phase serum rescued all wild-type C57BL/6 mice from intranasal infection with 20 times the median lethal dose of KIM D27 (2 × 105 CFU), even when administration of serotherapy was delayed until 18 h postinfection.
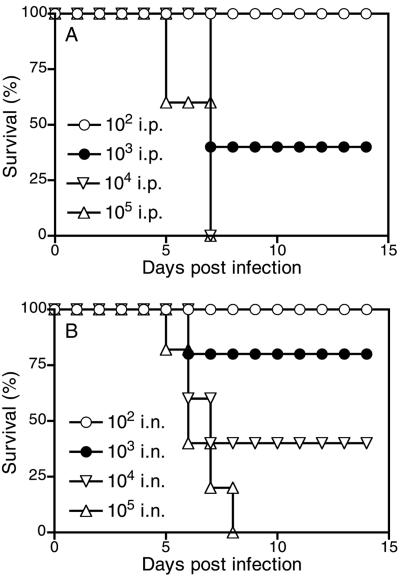
FIG. 1.
Susceptibility of C57BL/6 mice to Y. pestis strain KIM D27. C57BL/6 mice were intraperitoneally (i.p.) (A) or intranasally (i.n.) (B) infected with the indicated number of Y. pestis KIM D27 CFU and monitored daily for survival. An intraperitoneal dose of 3 × 102 CFU was chosen as a sublethal inoculum for generating convalescent-phase sera. An intranasal dose of 2 × 105 CFU was chosen for lethal challenge experiments.
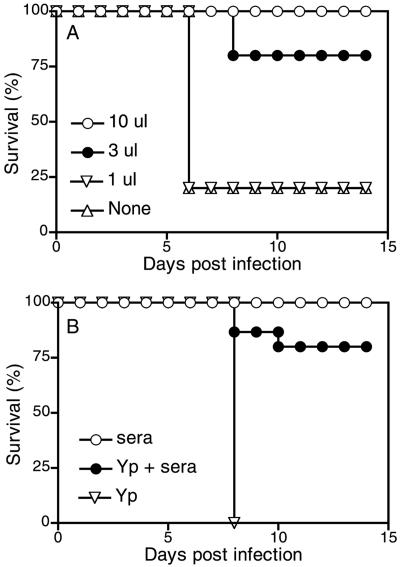
FIG. 2.
Postexposure passive serotherapy protects wild-type and μMT mice from lethal intranasal Y. pestis infection. (A) C57BL/6 mice were intranasally infected with 2 × 105 CFU Y. pestis KIM D27. At 18 h postinfection, the indicated dose of convalescent-phase sera was administered. Compared with mice that received no serotherapy, a 10-μl dose of postexposure serotherapy significantly protected C57BL/6 mice against mortality (n = 5 per group; P < 0.02). (B) B-cell-deficient μMT mice were intranasally infected with 2 × 105 CFU Y. pestis KIM D27 (Yp) or were left uninfected. At 18 h later, some animals received 10 μl of convalescent-phase sera, as indicated. Compared with mice that received no serotherapy, the postexposure serotherapy significantly protected μMT mice (n = 8 per group; P < 0.001).
Vaccines can prime both humoral and cellular immunity. To evaluate the capacity of cellular immunity to combat Y. pestis, we next assessed the safety of this vaccination-with-serotherapy protocol in B-cell-deficient μMT mice, which lack the capacity to generate humoral immunity (19). As shown in Fig. 2B, 10 μl of passive serotherapy administered at 18 h postinfection also protected most μMT mice against a lethal intranasal dose of Y. pestis (P < 0.001 in comparison with infected mice that did not receive serotherapy). Thus, we had established a protocol wherein B-cell-deficient μMT mice could survive exposure to live Y. pestis.
Vaccinated B-cell-deficient μMT mice can survive a lethal pulmonary Y. pestis challenge.
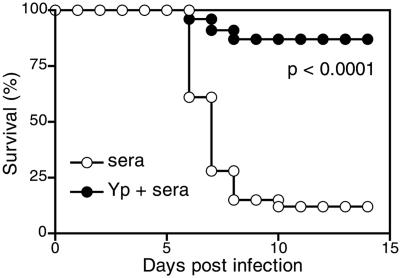
Having demonstrated that passive serotherapy enables μMT mice to survive exposure to live Y. pestis, we next assessed whether those animals were effectively vaccinated against a secondary Y. pestis challenge. To reduce the possibility that residual antibody might affect the outcome of secondary challenge, we employed a minimally protective dose of serotherapy (i.e., 10 μl) in the vaccination protocol, and we administered the secondary challenge at 60 days postvaccination, a time at which the titer of yersinia-specific antibody had declined to below the protective dose (see below). Moreover, the challenge experiments always included groups of control mice that were not infected with Y. pestis at the time of vaccination but did receive serotherapy. Figure 3 shows that 83% of the vaccinated μMT mice, which had been exposed previously to KIM D27, survived the challenge infection, whereas only 16% of the control mice survived the challenge infection. The degree of protection mediated by prior exposure to KIM D27 was highly significant (P < 0.0001). Thus, B-cell-deficient μMT mice, despite their inability to mount humoral immune responses, can be successfully vaccinated against pulmonary Y. pestis infection.
FIG. 3.
Vaccination with live Y. pestis in conjunction with serotherapy protects B-cell-deficient μMT mice against intranasal Y. pestis infection. As indicated, μMT mice were vaccinated via intranasal infection with 2 × 105 CFU Y. pestis KIM D27 followed 18 h later by 10 μl of convalescent-phase sera (Yp + sera) or were treated only with sera. Eighty-six percent of μMT mice survived this vaccination with live Y. pestis. Sixty days later, both groups were intranasally challenged with 2 × 105 CFU Y. pestis KIM D27. Day 0 represents the day of challenge infection (i.e., 60 days postvaccination). μMT mice that had been previously exposed to Y. pestis were protected from the secondary challenge (n = 23 to 29 per group; P < 0.0001). Data are pooled from three independent experiments.
Vaccination of B-cell-deficient μMT mice limits the growth and dissemination of Y. pestis and increases the number of CD4 and CD8 T cells in the infected pulmonary tissues.
To assess whether the vaccination-induced survival of B-cell-deficient μMT mice reflected effective antiyersinia immunity, we measured bacterial burdens and T-cell expansion at 72 h after challenge infection. In comparison with control animals, vaccinated μMT mice harbored 10-fold fewer bacteria in their lungs (Fig. 4A) (P < 0.001) and exhibited dramatically reduced dissemination of bacteria to spleen and liver (Fig. 4A) (P < 0.001 for both). Thus, vaccination of μMT mice with live Y. pestis limits bacterial growth and dissemination upon secondary challenge.
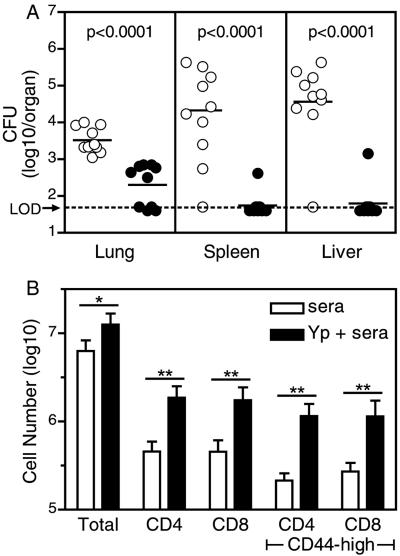
FIG. 4.
Vaccination-mediated protection of μMT mice against intranasal Y. pestis challenge correlates with reduced bacterial growth and dissemination and increased numbers of pulmonary T cells. B-cell-deficient μMT mice were vaccinated with live Y. pestis (2 × 105 CFU Y. pestis KIM D27 [Yp], intranasally) in combination with serotherapy. Control mice received serotherapy alone. Sixty days later, both vaccinated and control mice were intranasally challenged with 2 × 105 CFU Y. pestis KIM D27 as described for Fig. 3. At 72 h postchallenge, mice were euthanized and tissues harvested. (A) Numbers of bacteria were significantly reduced in pulmonary, splenic, and hepatic tissues of vaccinated (closed symbols) compared with control (open symbols) mice (n = 10 per group; P < 0.0001 for all tissues). Data are pooled from two independent experiments. Horizontal bars depict median values; LOD, limit of detection. (B) Numbers of total leukocytes, CD4-positive cells, CD8-positive cells, activated (CD44-high) CD4 cells, and activated CD8 cells in lung tissues of vaccinated (solid bars) compared with control (open bars) mice (n = 5 per group; *, P < 0.005; **, P < 0.0005). Data are representative of results obtained in two independent experiments. Error bars indicate standard deviations.
Vaccination also dramatically altered the number of T lymphocytes within the lung tissue of Y. pestis-challenged animals (Fig. 4B). In control mice, CD4-positive and CD8-positive T cells each comprised approximately 7% of total extractable lung cells at 72 h postchallenge, whereas these percentages both increased to approximately 14% in vaccinated mice. Since the total pulmonary cell number also increased twofold in vaccinated mice, the actual numbers of CD4 and CD8 T cells were more than fourfold higher in the lungs of vaccinated mice than in those of controls (Fig. 4B). Notably, most of the T cells in the vaccinated mice expressed high levels of the activation marker CD44 (Fig. 4B).
Depletion of T cells at the time of challenge abrogates the vaccine-mediated protection of B-cell-deficient μMT mice against lethal Y. pestis challenge.
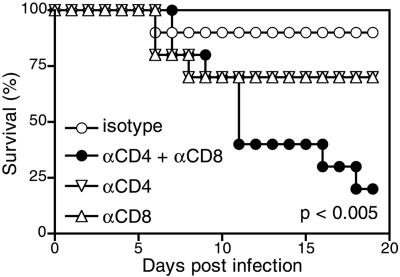
Given that μMT mice lack B cells and that T-cell responses were enhanced in the vaccinated mice, we hypothesized that the protection observed in our vaccine protocol resulted from the priming of Y. pestis-specific T cells. To test this hypothesis, we vaccinated μMT mice and then administered CD4 and/or CD8 T-cell-depleting monoclonal antibodies during the secondary challenge. Administration of both CD4- and CD8-specific monoclonal antibodies significantly reduced the level of protection in comparison with mice treated with isotype-matched control antibodies (Fig. 5) (P < 0.005). Administration of only CD4- or only CD8-specific antibody reduced protection, but not sufficiently to achieve statistical significance. These data suggest that both CD4 and CD8 T cells mediate protection against Y. pestis challenge in this vaccine model.
FIG. 5.
Treatment with MAb specific for CD4 and CD8 at the time of challenge abrogates the vaccination-mediated protection of μMT mice. B-cell-deficient μMT mice were vaccinated with live Y. pestis (2 × 105 CFU Y. pestis KIM D27, intranasally) in combination with serotherapy and were then intranasally challenged 60 days later with 2 × 105 CFU Y. pestis KIM D27 as described for Fig. 3. At the time of challenge, the mice also received treatment with MAb specific for CD4 and/or CD8 or an isotype matched control MAb, as indicated. Treatment with both CD4- and CD8-specific MAb significantly reduced survival compared with treatment with isotype control MAb (n = 10 per group; P < 0.005). Data are pooled from two independent experiments.
The adoptive transfer of Y. pestis-primed T cells protects naive μMT mice against lethal Y. pestis challenge.
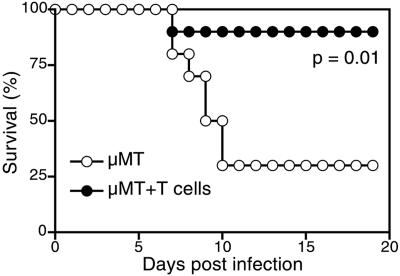
To assess the role of T cells in protection against Y. pestis in a fully antibody-independent model, we adoptively transferred Y. pestis-primed T cells to naive μMT mice and assessed survival after challenge infection. To generate T cells, we isolated lung and splenic tissues from convalescent μMT animals that had survived vaccination and challenge (i.e., the Y. pestis-plus-serum group in Fig. 3), isolated and pooled leukocytes, and expanded the Y. pestis-specific cells by stimulating them in vitro with heat-killed Y. pestis. After 1 week of expansion in vitro, we transferred the cells to naive μMT mice, which were then challenged intranasally with 2 × 105 CFU KIM D27. As shown in Fig. 6, a significantly greater proportion of mice survived the challenge infection if they received Y. pestis-stimulated T cells (P = 0.01). Thus, even in the complete absence of serotherapy, cellular immunity can protect μMT mice against lethal Y. pestis infection.
FIG. 6.
Adoptive transfer of Y. pestis-primed T cells protects naive μMT mice against lethal intranasal Y. pestis infection. Cells isolated from B-cell-deficient μMT mice that had been vaccinated and challenged as described for Fig. 3 were stimulated in vitro with heat-killed Y. pestis, expanded with IL-2, and transferred to naive μMT mice as described in Materials and Methods. The next day, the mice were intranasally challenged with 2 × 105 CFU Y. pestis KIM D27. A significantly greater number of mice that received T cells survived the infection (n = 10 per group; P = 0.01). Data are pooled from two independent experiments.
DISCUSSION
Here, we have demonstrated that vaccine-primed T cells have the capacity to combat pulmonary Y. pestis infections. Prior studies have revealed important protective roles for T cells and T-cell-derived cytokines during infection of mice by the related bacterium Yersinia enterocolitica (3-6, 28, 29, 38). However, until now, protective roles for T cells during Y. pestis infections had yet to be documented.
Recent pneumonic plague vaccine studies have largely focused upon antibody-based humoral immunity, in part due to prior studies documenting that adoptive serotherapy protects mice against lethal Y. pestis infection (13, 16). However, vaccine trials with nonhuman primates suggest that humoral immunity may not suffice to protect humans against pulmonary Y. pestis infection. Specifically, studies by the USAMRIID found that a significant number of nonhuman primates immunized with the F1-V fusion protein vaccine succumbed to aerosol Y. pestis infection, despite their possession of high-titer antibody at the time of challenge (Pitt, Animals Models and Correlates of Protection for Plague Vaccines Workshop, http://www.fda.gov/cber/minutes/workshop-min.htm). Thus, antibodies may not suffice in protecting against pneumonic plague.
Here, we took advantage of a passive serotherapy protocol to develop a method for vaccinating antibody-deficient μMT mice with an otherwise lethal dose of live Y. pestis. Using that protocol, we demonstrated that vaccination can protect antibody-deficient mice against pulmonary Y. pestis infection. Given that our primary model entails the use of serotherapy during the vaccination protocol, it was conceivable that a small amount of antibody persisted until the challenge and contributed to the observed protection. However, all of our experiments included control mice that received serotherapy alone during the vaccination period, and these animals were not protected from challenge infection. Thus, any residual antibody derived from the vaccination protocol, if present at all, did not suffice in protecting the mice against the secondary challenge infection. Moreover, the transfer of Y. pestis-primed T cells to naive μMT mice protected against lethal Y. pestis challenge, thereby confirming that cellular immunity, in the absence of antibody, can protect against pulmonary Y. pestis infection.
Current efforts are aimed at precisely defining the mechanisms underlying cell-mediated protection against pneumonic plague. As shown here, numbers of activated T cells in the lung tissues were significantly increased in vaccinated mice compared with controls, and depleting T cells at the time of challenge abrogated protection. Moreover adoptively transferring Y. pestis-stimulated T cells provided protection, suggesting that vaccine-stimulated T cells are directly responsible for the observed protection. Depleting both CD4 and CD8 T cells reduced protection to a significantly greater extent than could be achieved by depleting only CD4 or only CD8 T cells (Fig. 5). Together, these findings suggest that both CD4 and CD8 T cells contribute to protection against pulmonary Y. pestis infection, and we have initiated studies aimed at defining the precise contributions of each cell type.
T cells recognize processed antigenic epitopes in the context of major histocompatibility complex molecules expressed on the surfaces of cells. Upon reexposure to antigen, vaccine-primed CD4 and CD8 T cells can secrete phagocyte-activating cytokines, such as gamma interferon (IFN-γ) and tumor necrosis factor alpha (TNF-α) (18). Parenteral administration of IFN-γ and TNF-α reportedly protects mice against lethal Y. pestis infection (26), and it appears that Y. pestis virulence factors actively suppress production of IFN-γ and TNF-α (7, 26). These observations strongly suggest that cytokine-mediated cellular immunity is detrimental to Y. pestis. Therefore, current efforts are aimed at evaluating whether our vaccine protocol primes memory T cells that rapidly produce IFN-γ and/or TNF-α in response to challenge infection, thereby promoting the bactericidal capacities of phagocytes and/or protecting phagocytes from the debilitating effects of Y. pestis virulence factors.
Vaccine-primed cytokine production almost certainly contributes to protection, but T cells could also function protectively via their capacity to directly lyse infected cells (18). Y. pestis bacteria can replicate within cells in vitro and are also believed to do so during the initial stages of infection in vivo (8, 17, 34). However, it remains unclear whether intracellular bacteria contribute significantly to the later stages of infection, during which the bacteria occupy primarily extracellular niches (27, 32, 33). Given that cellular immunity is well recognized to combat intracellular pathogens, our finding that cellular immunity combats Y. pestis infection suggests that intracellular Y. pestis bacteria may be relevant to pathogenesis. However, recent studies suggest that cellular immunity also combats bacteria that primarily replicate extracellularly, such as Streptococcus pneumoniae (23). Thus, our demonstration that cellular immunity combats Y. pestis infection does not, in and of itself, indicate that physiologically significant intracellular reservoirs of Y. pestis exist in vivo. We anticipate that further studies of the mechanisms by which CD4 and CD8 T cells contribute to protection will help to clarify the importance of intracellular Y. pestis in the pathogenesis of plague.
Our demonstration that cellular immunity can combat pulmonary Y. pestis infection suggests that development of pneumonic plague vaccines should strive to harness the protective capacities of cell-mediated immunity. We suspect that cellular and humoral immunity will synergize in combating plague infection and that, ideally, plague vaccines should prime both cellular and humoral immunity. USAMRIID's current formulation of the F1-V fusion protein subunit vaccine elicits robust humoral immunity, but its capacity to prime effective cellular immunity has yet to be demonstrated. Our findings indicate that Y. pestis bacteria must possess antigenic targets for cellular immunity. However, there is no a priori reason to assume that F1 and/or V constitutes such a target. Thus, to effectively incorporate cellular immunity into subunit plague vaccines, it is now imperative to define the specific Y. pestis proteins that elicit protective cellular immune responses.
Acknowledgments
This work was supported by Public Health Service grants AI054595 (to S.T.S.), AI057158 (to S.T.S.), and AI061577 (to S.T.S.) and by funds from the Trudeau Institute.
We thank Robert Brubaker for providing Y. pestis KIM D27; Lawrence Johnson, David Woodland, and Robert North for critical reading of the manuscript; Debbie Duso for technical assistance; and the employees of the Trudeau animal facilities for dedicated care of the mice used in these studies.
Editor: D. L. Burns
REFERENCES
- 1.Anderson, G. W., Jr., S. E. Leary, E. D. Williamson, R. W. Titball, S. L. Welkos, P. L. Worsham, and A. M. Friedlander. 1996. Recombinant V antigen protects mice against pneumonic and bubonic plague caused by F1-capsule-positive and -negative strains of Yersinia pestis. Infect. Immun. 64:4580-4585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andrews, G. P., D. G. Heath, G. W. Anderson, Jr., S. L. Welkos, and A. M. Friedlander. 1996. Fraction 1 capsular antigen (F1) purification from Yersinia pestis CO92 and from an Escherichia coli recombinant strain and efficacy against lethal plague challenge. Infect. Immun. 64:2180-2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Autenrieth, I. B., M. Beer, E. Bohn, S. H. Kaufmann, and J. Heesemann. 1994. Immune responses to Yersinia enterocolitica in susceptible BALB/c and resistant C57BL/6 mice: an essential role for gamma interferon. Infect. Immun. 62:2590-2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Autenrieth, I. B., A. Tingle, A. Reske-Kunz, and J. Heesemann. 1992. T lymphocytes mediate protection against Yersinia enterocolitica in mice: characterization of murine T-cell clones specific for Y. enterocolitica. Infect. Immun. 60:1140-1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Autenrieth, I. B., U. Vogel, S. Preger, B. Heymer, and J. Heesemann. 1993. Experimental Yersinia enterocolitica infection in euthymic and T-cell-deficient athymic nude C57BL/6 mice: comparison of time course, histomorphology, and immune response. Infect. Immun. 61:2585-2595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bohn, E., and I. B. Autenrieth. 1996. IL-12 is essential for resistance against Yersinia enterocolitica by triggering IFN-gamma production in NK cells and CD4+ T cells. J. Immunol. 156:1458-1468. [PubMed] [Google Scholar]
- 7.Brubaker, R. R. 2003. Interleukin-10 and inhibition of innate immunity to yersiniae: roles of Yops and LcrV (V antigen). Infect. Immun. 71:3673-3681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cavanaugh, D. C., and R. Randall. 1959. The role of multiplication of Pasteurella pestis in mononuclear phagocytes in the pathogenesis of flea-borne plague. J. Immunol. 83:348-363. [PubMed] [Google Scholar]
- 9.Cohen, R. J., and J. L. Stockard. 1967. Pneumonic plague in an untreated plague-vaccinated individual. JAMA 202:365-366. [PubMed] [Google Scholar]
- 10.Ehrenkranz, N. J., and K. F. Meyer. 1955. Studies on immunization against plague. VIII. Study of three immunizing preparations in protecting primates against pneumonic plague. J. Infect. Dis. 96:138-144. [DOI] [PubMed] [Google Scholar]
- 11.Fowler, J. M., and R. R. Brubaker. 1994. Physiological basis of the low-calcium response in Yersinia pestis. Infect. Immun. 62:5234-5241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Galimand, M., A. Guiyoule, G. Gerbaud, B. Rasoamanana, S. Chanteau, E. Carniel, and P. Courvalin. 1997. Multidrug resistance in Yersinia pestis mediated by a transferable plasmid. N. Engl. J. Med. 337:677-680. [DOI] [PubMed] [Google Scholar]
- 13.Green, M., D. Rogers, P. Russell, A. J. Stagg, D. L. Bell, S. M. Eley, R. W. Titball, and E. D. Williamson. 1999. The SCID/beige mouse as a model to investigate protection against Yersinia pestis. FEMS Immunol. Med. Microbiol. 23:107-113. [DOI] [PubMed] [Google Scholar]
- 14.Haffkine, W. M. 1897. Remarks on the plague prophylactic fluid. Br. Med. J. 1:1461. [Google Scholar]
- 15.Heath, D. G., G. W. Anderson, Jr., J. M. Mauro, S. L. Welkos, G. P. Andrews, J. Adamovicz, and A. M. Friedlander. 1998. Protection against experimental bubonic and pneumonic plague by a recombinant capsular F1-V antigen fusion protein vaccine. Vaccine 16:1131-1137. [DOI] [PubMed] [Google Scholar]
- 16.Hill, J., S. E. Leary, K. F. Griffin, E. D. Williamson, and R. W. Titball. 1997. Regions of Yersinia pestis V antigen that contribute to protection against plague identified by passive and active immunization. Infect. Immun. 65:4476-4482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Janssen, W. A., and M. J. Surgalla. 1969. Plague bacillus: survival within host phagocytes. Science 163:950-952. [DOI] [PubMed] [Google Scholar]
- 18.Kaufmann, S. H. 1993. Immunity to intracellular bacteria. Annu. Rev. Immunol. 11:129-163. [DOI] [PubMed] [Google Scholar]
- 19.Kitamura, D., J. Roes, R. Kuhn, and K. Rajewsky. 1991. A B cell-deficient mouse by targeted disruption of the membrane exon of the immunoglobulin mu chain gene. Nature 350:423-426. [DOI] [PubMed] [Google Scholar]
- 20.Kolle, W., and R. Otto. 1904. Weitere Untersuchungen uber die Pestimmunitat. Z. F. Hyg. 48:399-428. [Google Scholar]
- 21.Lahteenmaki, K., R. Virkola, A. Saren, L. Emody, and T. K. Korhonen. 1998. Expression of plasminogen activator Pla of Yersinia pestis enhances bacterial attachment to the mammalian extracellular matrix. Infect. Immun. 66:5755-5762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levine, M. M., and M. B. Sztein. 2004. Vaccine development strategies for improving immunization: the role of modern immunology. Nat. Immunol. 5:460-464. [DOI] [PubMed] [Google Scholar]
- 23.Malley, R., K. Trzcinski, A. Srivastava, C. M. Thompson, P. W. Anderson, and M. Lipsitch. 2005. CD4+ T cells mediate antibody-independent acquired immunity to pneumococcal colonization. Proc. Natl. Acad. Sci. USA 102:4848-4853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meyer, K. F. 1970. Effectiveness of live or killed plague vaccines in man. Bull. W. H. O. 42:653-666. [PMC free article] [PubMed] [Google Scholar]
- 25.Meyer, K. F., D. C. Cavanaugh, P. J. Bartelloni, and J. D. Marshall, Jr. 1974. Plague immunization. I. Past and present trends. J. Infect. Dis. 129:(Suppl.):S13-S18. [DOI] [PubMed] [Google Scholar]
- 26.Nakajima, R., and R. R. Brubaker. 1993. Association between virulence of Yersinia pestis and suppression of gamma interferon and tumor necrosis factor alpha. Infect. Immun. 61:23-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nakajima, R., V. L. Motin, and R. R. Brubaker. 1995. Suppression of cytokines in mice by protein A-V antigen fusion peptide and restoration of synthesis by active immunization. Infect. Immun. 63:3021-3029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Noll, A., A. Roggenkamp, J. Heesemann, and I. B. Autenrieth. 1994. Protective role for heat shock protein-reactive alpha beta T cells in murine yersiniosis. Infect. Immun. 62:2784-2791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parent, M. A., K. N. Berggren, I. K. Mullarky, F. M. Szaba, L. W. Kummer, J. J. Adamovicz, and S. T. Smiley. 2005. Yersinia pestis V protein epitopes recognized by CD4 T cells. Infect. Immun. 73:2197-2204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Perry, R. D., and J. D. Fetherston. 1997. Yersinia pestis—etiologic agent of plague. Clin. Microbiol. Rev. 10:35-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reed, L. J., and H. Muench. 1938. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 32.Sebbane, F., D. Gardner, D. Long, B. B. Gowen, and B. J. Hinnebusch. 2005. Kinetics of disease progression and host response in a rat model of bubonic plague. Am. J. Pathol. 166:1427-1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Simonet, M., S. Richard, and P. Berche. 1990. Electron microscopic evidence for in vivo extracellular localization of Yersinia pseudotuberculosis harboring the pYV plasmid. Infect. Immun. 58:841-845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Straley, S. C., and P. A. Harmon. 1984. Yersinia pestis grows within phagolysosomes in mouse peritoneal macrophages. Infect. Immun. 45:655-659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Strong, R. P. 1908. Protective inoculation against plague. J. Med. Res. 18:325-346. [PMC free article] [PubMed] [Google Scholar]
- 36.Strong, R. P. 1906. Vaccination against plague. Phillipine J. Sci. 1:181-190. [Google Scholar]
- 37.Taylor, J. 1933. Haffkine's plague vaccine. Indian Med. Res. Memoirs 27:1-125. [Google Scholar]
- 38.Thakur, A. 1996. Role of T-cell subsets in protection, delayed type of hypersensitivity and granuloma formation during Yersinia enterocolitica infection in mice. Immunol. Lett. 49:1-6. [DOI] [PubMed] [Google Scholar]
- 39.Titball, R. W., and E. D. Williamson. 2004. Yersinia pestis (plague) vaccines. Expert Opin. Biol. Ther. 4:965-973. [DOI] [PubMed] [Google Scholar]
- 40.Williamson, E. D., S. M. Eley, K. F. Griffin, M. Green, P. Russell, S. E. Leary, P. C. Oyston, T. Easterbrook, K. M. Reddin, A. Robinson, et al. 1995. A new improved sub-unit vaccine for plague: the basis of protection. FEMS Immunol. Med. Microbiol. 12:223-230. [DOI] [PubMed] [Google Scholar]
- 41.Zinkernagel, R. M. 2003. On natural and artificial vaccinations. Annu. Rev. Immunol. 21:515-546. [DOI] [PubMed] [Google Scholar]