Abstract
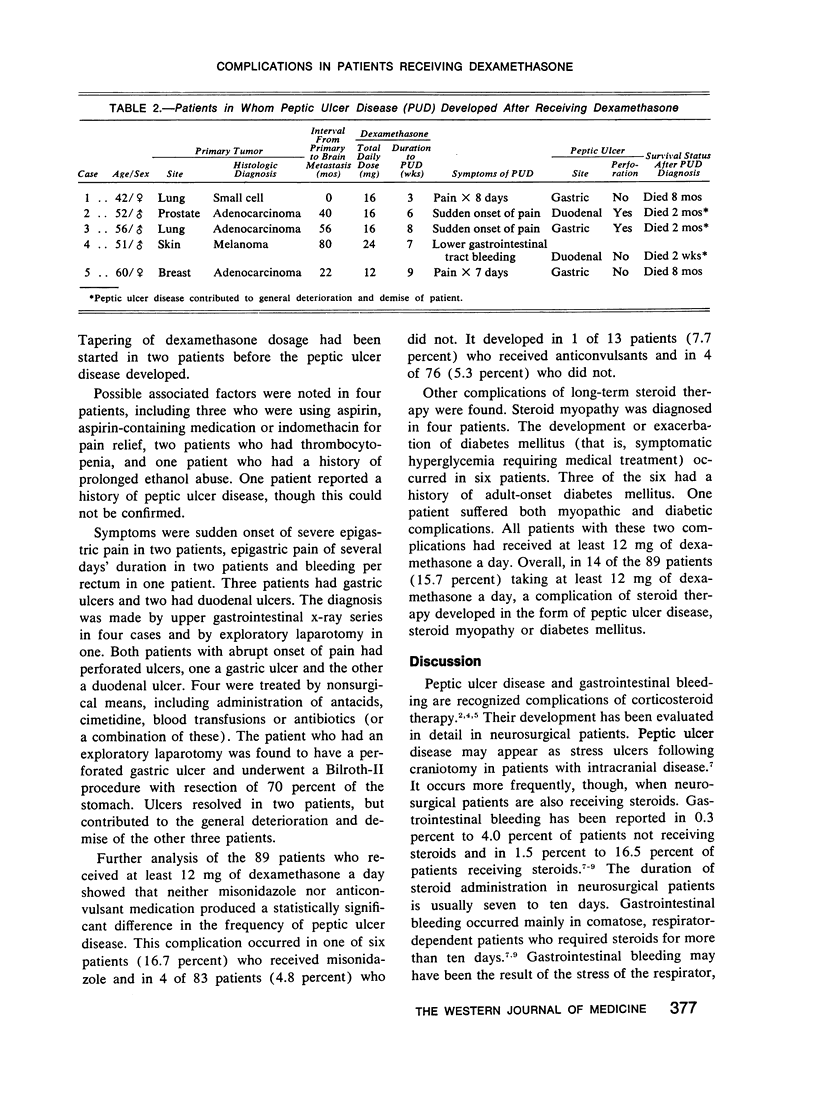
A retrospective analysis was done of 106 patients who received radiation therapy for brain metastasis. Dexamethasone therapy was instituted in 97 patients. Peptic ulcer disease developed in 5 of 89 patients (5.6 percent) who received a dosage of at least 12 mg a day, but did not occur in patients who received a lower dose or in those who did not receive steroids. The interval between institution of dexamethasone therapy and the development of peptic ulcer disease ranged from three to nine weeks. Two patients had perforated ulcers, one of whom required surgical resection. Peptic ulcer disease contributed to the general deterioration and death of three of the five patients. Overall, in 14 of the 89 patients (15.7 percent) a complication of steroid therapy developed in the form of peptic ulcer disease, steroid myopathy or diabetes mellitus (or a combination of these).
Full text
PDF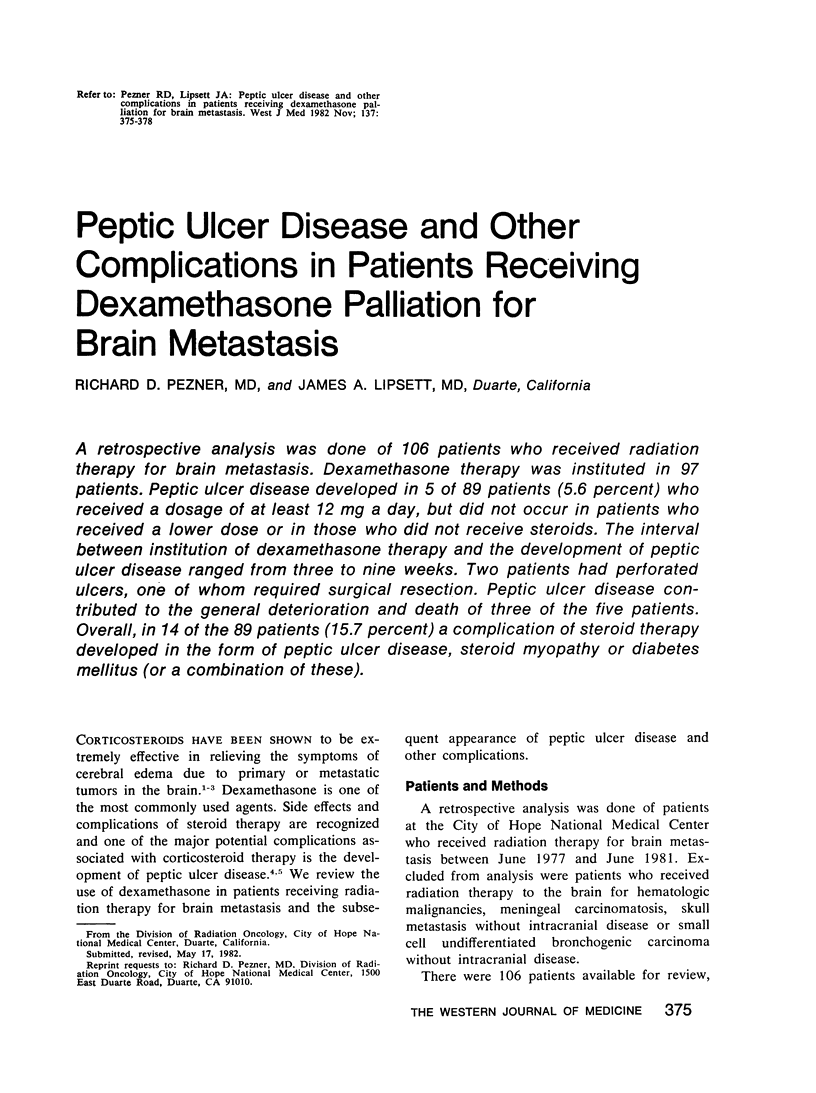
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cairncross J. G., Kim J. H., Posner J. B. Radiation therapy for brain metastases. Ann Neurol. 1980 Jun;7(6):529–541. doi: 10.1002/ana.410070606. [DOI] [PubMed] [Google Scholar]
- Cantu R. C., Amir-Ahmadi H., Prieto A. Evaluation of the increased risk of gastrointestinal bleeding following intracranial surgery in patients receiving high steroid dosages in the immediate postoperative period. Int Surg. 1968 Oct;50(4):325–335. [PubMed] [Google Scholar]
- Dujovne C. A., Azarnoff D. L. Clinical complications of corticosteroid therapy. A selected review. Med Clin North Am. 1973 Sep;57(5):1331–1342. doi: 10.1016/s0025-7125(16)32233-7. [DOI] [PubMed] [Google Scholar]
- Graham K., Caird F. I. High-dose steroid therapy of intracranial tumour in the elderly. Age Ageing. 1978 Aug;7(3):146–150. doi: 10.1093/ageing/7.3.146. [DOI] [PubMed] [Google Scholar]
- Greenberg H. S., Kim J. H., Posner J. B. Epidural spinal cord compression from metastatic tumor: results with a new treatment protocol. Ann Neurol. 1980 Oct;8(4):361–366. doi: 10.1002/ana.410080404. [DOI] [PubMed] [Google Scholar]
- Gutin P. H. Corticosteroid therapy in patients with brain tumors. Natl Cancer Inst Monogr. 1977 Dec;46:151–156. [PubMed] [Google Scholar]
- Jick H., Porter J. Drug-induced gastrointestinal bleeding. Report from the Boston Collaborative Drug Surveillance Program, Boston University Medical Center. Lancet. 1978 Jul 8;2(8080):87–89. doi: 10.1016/s0140-6736(78)91396-x. [DOI] [PubMed] [Google Scholar]
- Ottonello G. A., Primavera A. Gastrointestinal complication of high-dose corticosteroid therapy in acute cerebrovascular patients. Stroke. 1979 Mar-Apr;10(2):208–210. doi: 10.1161/01.str.10.2.208. [DOI] [PubMed] [Google Scholar]


