Recent reports documenting community-acquired infections with methicillin-resistant Staphylococcus aureus (MRSA) are cause for concern (1, 8). However, not all MRSA infections detected within the community were acquired there. In recent years, healthcare practices have shifted MRSA-infected individuals from hospitals into surrounding communities, for treatment and convalescence at home, for example (2). While the epidemiology of nosocomial MRSA has been well studied, less is known about the dissemination of MRSA within communities surrounding hospitals. Generally, apart from unique community strains, it has been thought that MRSA is transferred from hospital environments, known reservoirs of antimicrobial resistance, into surrounding communities. Additionally, patients may become carriers of MRSA during a stay in a healthcare institution and later, perhaps at home, manifest an infection from this MRSA, blurring the definitions of community- and hospital-acquired infections. If these assumptions were true, one would expect the prevalence of MRSA to be higher in outpatients served by hospitals with higher rates of MRSA. To test this hypothesis, we analyzed data from The Surveillance Network (TSN) Database—USA (Focus Technologies, Inc., Herndon, Va.).
TSN Database—USA electronically collects daily routine antimicrobial susceptibility testing and patient demographic data from laboratories, which are the data upon which clinical decisions are made (10). Participant institutions are geographically dispersed throughout the nine U.S. Census Bureau regions. All data are filtered through expert rule algorithms to remove repeat isolates and identify microbiologically atypical results for confirmation or verification before being merged into the final database. The information provided to TSN databases allows us to confidently differentiate inpatients from outpatients but does not allow us to determine whether an infection was community or hospital acquired. Outpatient data contained in TSN databases also include isolates from emergency room visits. For this analysis, we excluded isolates from nursing home and other long-term-care-facility patients, frequently colonized with MRSA. To test our hypothesis that a relationship exists between the prevalence of MRSA in outpatients and inpatients in the same geographic area, we reviewed routine laboratory data comprising 264,687 nonrepeat isolates of S. aureus collected in 2000 from 121 hospitals in TSN Database—USA, each testing at least 100 isolates.
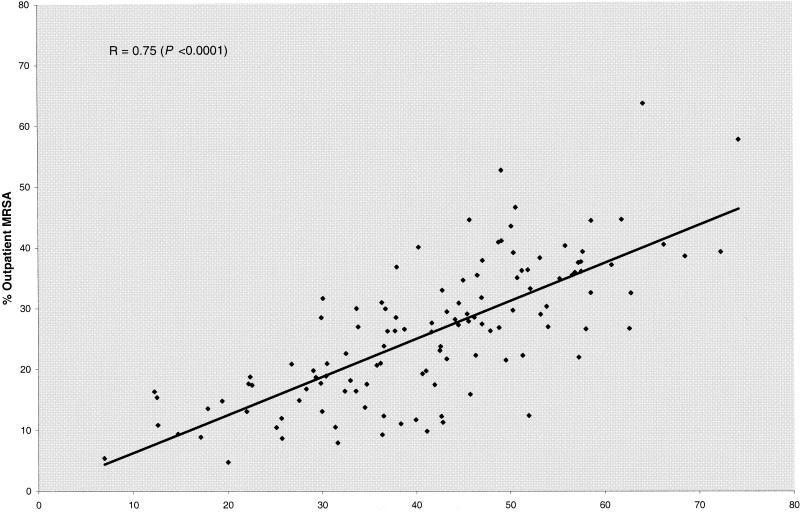
A highly significant relationship (P < 0.0001) was found between the rates of MRSA among outpatient and inpatient isolates of S. aureus in 2000 (Fig. 1). This relationship was confirmed by linear regression analysis (r = 0.75). Almost invariably, hospitals with higher rates of MRSA among their inpatients had higher rates of MRSA among outpatient isolates submitted to their laboratories for culture and antimicrobial susceptibility testing. Similarly, hospitals with lower rates of MRSA among their inpatients had lower rates of MRSA among outpatients from their surrounding communities. Multiple drug resistance, defined as concurrent resistance to three or more antimicrobial drug classes, comprised 76.1% and 66.5% of inpatient and outpatient isolates, respectively. The prevalence of MRSA has continued to increase in the United States. A retrospective analysis of TSN Database—USA showed that the prevalence of MRSA in 33 hospitals participating from 1996 to 2000 increased from 30.1% (4,557/15,143) in 1996 to 45.7% (27,495/60,149) in 2000 (P < 0.0001) in inpatient isolates; among outpatient isolates, the prevalence of MRSA increased from 17.3% (1,781/10,268) to 28.6% (17,858/62,401) (P < 0.0001).
FIG. 1.
The proportion of MRSA in outpatient samples plotted against the proportion of MRSA in inpatient samples for each of the 121 hospitals able to be evaluated which participated in TSN Database—USA during 2000.
Previous reports have noted a growing concern regarding MRSA infections within some community populations, particularly in children (4, 5) and those with dermatological disorders, renal dysfunction, or HIV infection (6, 7, 9). The clear relationship between the rates of MRSA infection among inpatients and outpatients demonstrated here illustrates that MRSA infections are no longer confined to hospitals and are certainly present in the community. It is likely that these include both distinct community clones and those carried by patients formerly either directly or indirectly exposed to the healthcare environment, as demonstrated in a recent U.S. study (3). The present report corroborates the need for heightened awareness of MRSA among community health-care practitioners, including up-to-date knowledge of trends in MRSA at local and regional levels. There is also a need for more rapid, reliable methods to detect and report the presence of methicillin resistance among isolates of S. aureus, especially among outpatients, as standard empirical therapies may not be effective in treating infections by MRSA, especially those derived from hospital environments with a greater tendency for multidrug resistance.
Acknowledgments
We gratefully acknowledge the participation of all the clinical testing institutions participating in the TSN Database—USA network for their valuable contributions of data to this study.
REFERENCES
- 1.Akram, J., and A. E. Glatt. 1998. True community acquired methicillin-resistant Staphylococcus aureus bacteremia. Infect. Control Hosp. Epidemiol. 19:106-107. [DOI] [PubMed] [Google Scholar]
- 2.Boyce, J. M. 1998. Are the epidemiology and microbiology of methicillin-resistant Staphylococcus aureus changing? JAMA 279:623-624. [DOI] [PubMed] [Google Scholar]
- 3.Charlebois, E. D., D. R. Bangsberg, N. J. Moss, M. R. Moore, A. R. Moss, H. F. Chambers, and F. Perdreau-Remington. 2002. Population-based community prevalence of methicillin-resistant Staphylococcus aureus in the urban poor of San Fransisco. Clin. Infect. Dis. 34:425-433. [DOI] [PubMed] [Google Scholar]
- 4.Gorak, E. J., S. M. Yamada, and J. D. Brown. 1999. Community-acquired methicillin-resistant Staphylococcus aureus in hospitalized adults and children without known risk factors. Clin. Infect. Dis. 29:797-800. [DOI] [PubMed] [Google Scholar]
- 5.Herold, B. C., L. C. Immergluck, M. C. Maranan, D. S. Lauderdale, R. E. Gaskin, S. Boyle-Vavra, C. D. Leitch, and R. S. Daum. 1998. Community-acquired methicillin-resistant Staphylococcus aureus in children with no identified predisposing risk. JAMA 279:593-598. [DOI] [PubMed] [Google Scholar]
- 6.Holley, J. L., J. Bernardini, J. R. R. Johnston, and B. Piraino. 1990. Methicillin-resistant staphylococcal infections in an outpatient peritoneal dialysis program. Am. J. Kidney Dis. 16:142-146. [DOI] [PubMed] [Google Scholar]
- 7.Klein, P. A., W. H. Greene, J. Fuhrer, and R. A. Clark. 1997. Prevalence of methicillin-resistant Staphylococcus aureus in outpatients with psoriasis, atopic dermatitis, or HIV infection. Arch. Dermatol. 133:1463-1465. [DOI] [PubMed] [Google Scholar]
- 8.Naimi, T. S., K. H. LeDell, D. J. Boxrud, A. V. Groom, C. D. Steward, S. K. Johnson, J. M. Besser, C. O'Boyle, R. N. Danila, J. E. Cheek, M. T. Osterholm, K. A. Moore, and K. E. Smith. 2001. Epidemiology and clonality of community-acquired methicillin-resistant Staphylococcus aureus in Minnesota, 1996-1998. Clin. Infect. Dis. 33:990-996. [DOI] [PubMed] [Google Scholar]
- 9.Price, M. F., M. E. McBride, and J. E. Wolf, Jr. 1998. Prevalence of methicillin-resistant Staphylococcus aureus in dermatology outpatient population. South. Med. J. 91:369-371. [DOI] [PubMed] [Google Scholar]
- 10.Sahm, D. F., M. K. Marsilio, and G. Piazza. 1999. Antimicrobial resistance in key bloodstream bacterial isolates: electronic surveillance with The Surveillance Network Database—USA. Clin. Infect. Dis. 29:259-263. [DOI] [PubMed] [Google Scholar]