Abstract
Of 15 extended-spectrum β-lactamase (ESBL)-producing isolates of the family Enterobacteriaceae collected from the First Municipal People's Hospital of Guangzhou, in the southern part of the People's Republic of China, 9 were found to produce CTX-M ESBLs, 3 produced SHV-12, and 3 produced both CTX-M and SHV-12. Eleven isolates produced either TEM-1B or SHV-11, in addition to an ESBL. Nucleotide sequence analysis of the 12 isolates carrying blaCTX-M genes revealed that they harbored three different blaCTX-M genes, blaCTX-M-9 (5 isolates), blaCTX-M-13 (1 isolate), and blaCTX-M-14 (6 isolates). These genes have 98% nucleotide homology with blaToho-2. The blaCTX-M genes were carried on plasmids that ranged in size from 35 to 150 kb. Plasmid fingerprints and pulsed-field gel electrophoresis showed the dissemination of the blaCTX-M genes through transfer of different antibiotic resistance plasmids to different bacteria, suggesting that these resistance determinants are highly mobile. Insertion sequence ISEcp1, found on the upstream region of these genes, may be involved in the translocation of the blaCTX-M genes. This is the first report of the occurrence of SHV-12 and CTX-M ESBLs in China. The presence of strains with these ESBLs shows both the evolution of blaCTX-M genes and their dissemination among at least three species of the family Enterobacteriaceae, Escherichia coli, Klebsiella pneumoniae, and Enterobacter cloacae, isolated within a single hospital. The predominance of CTX-M type enzymes seen in this area of China appears to be similar to that seen in South America but is different from those seen in Europe and North America, suggesting different evolutionary routes and selective pressures. A more comprehensive survey of the ESBL types from China is urgently needed.
Until 1994, SHV-2 was the only extended-spectrum β-lactamase (ESBL) described in bacteria originating from the People's Republic of China (10). Recently, ESBL-producing bacteria have been reported from China, but molecular characterization of these ESBLs has not yet been undertaken (38, 45-47). During an antimicrobial resistance-monitoring project in the First Municipal People's Hospital of Guangzhou, which is in the southern part of China, in 1997, ESBL production rates in Escherichia coli, Klebsiella pneumoniae, Enterobacter cloacae, and Citrobacter freundii were 18, 19, 16, and 18%, respectively (45). In 1998, the rates of resistance due to the production of ESBLs rose dramatically, to 33% for E. coli, 37% for K. pneumoniae, 18% for E. cloacae, and 25% for C. freundii (46). A limited number of these ESBL-producing isolates have been selected for investigation in the present study.
(A part of this report was presented at the 21st International Congress of Chemotherapy, Birmingham, United Kingdom, 4 to 7 July 1999, and the 10th European Congress of Clinical Microbiology and Infectious Diseases, Stockholm, Sweden, 28 to 31 May 2000.)
MATERIALS AND METHODS
Bacterial strains.
Fifteen nonduplicate ESBL-producing isolates of the family Enterobacteriaceae were selected from a collection of ESBL-producing strains isolated as part of an antimicrobial resistance monitoring project in the First Municipal People's Hospital of Guangzhou, a 900-bed hospital in the People's Republic of China, between 1997 and 1998. The isolates were chosen to represent the range of species and profiles of resistance to broad-spectrum cephalosporins seen in the hospital during the study period. These included eight E. coli isolates, three K. pneumoniae isolates, three E. cloacae isolates, and one C. freundii isolate. All isolates were positive by a double-disk diffusion test, confirming the production of an ESBL (23). The isolates were identified by conventional methods (25). Species identification of the Enterobacter isolates was achieved by the API 20E strip method (BioMerieux S.A., Marcy l'Etoile, France).
Susceptibility testing.
A disk diffusion susceptibility test was performed on Iso-Sensitest agar (Oxoid, Basingstoke, England) by a comparative method (19). Cefepime, ceftazidime, cefotaxime, cefoxitin, imipenem, and piperacillin plus tazobactam disks were used (Oxoid). The MICs of aztreonam, cefotaxime, ceftazidime, and ceftazidime plus clavulanic acid (at a fixed concentration of 4 μg/ml) were determined by an agar dilution method (19). The antibiotics were supplied as follows: aztreonam, E. R. Squibb & Sons, Hounslow, England; cefotaxime, Roussel Laboratories, Uxbridge, England; ceftazidime, Glaxo Laboratories, Greenford, England; and clavulanic acid, SmithKline Beecham Pharmaceuticals, Brentford, England. E. coli strain NCTC 10418 was used as an antibiotic-sensitive control, and E. coli HB101(pAFF611) encoding SHV-5 was used as a positive control for the ESBL phenotype (22).
Transfer of cefotaxime and ceftazidime resistance markers.
Plasmid transfer of cefotaxime or ceftazidime resistance markers was performed by a broth culture conjugation method (37). Laboratory E. coli strains UB1637 (lys his trp lac recA Strr) and UB5201 (pro met recA Nalr) were used as recipients. The mating time was 4 h. Transconjugants were selected on nutrient agar plates containing either cefotaxime or ceftazidime (2 μg/ml; Sigma, Poole, England) and either streptomycin (25 to 400 μg/ml; Sigma) to select for UB1637 transconjugants or nalidixic acid (25 μg/ml; Sigma) if UB5201 was used as the recipient strain.
Analytical isoelectric focusing.
Crude β-lactamase preparations were extracted by a sonication method (11). Analytical isoelectric focusing was performed as described previously (17), except that agarose gels containing Pharmalyte (pH 3 to 10; Pharmacia Biotech, Uppsala, Sweden) were used. The β-lactamase activity was detected by overlaying the gel with filter paper containing nitrocefin (0.5 mg/ml).
PCR amplification.
All isolates were first screened for the presence of blaSHV and blaTEM by previously described PCR protocols (18, 30, 32). Isolates carrying neither blaSHV nor blaTEM were further screened for the presence of blaToho-1 and blaCTX-M-1 as described previously (15, 48). In addition, primers C-1 and C-2 (Table 1), designed from the nucleotide sequence of blaToho-2 (29), were used to amplify a 906-bp gene fragment. Bacterial DNA was prepared by suspending one or two fresh colonies in 50 μl of sterile distilled water and heating at 95°C for 5 min. PCR amplification was carried out under the following conditions: 95°C for 3 min, followed by 30 cycles of 95°C for 1 min, 55°C for 1 min, and 72°C for 1 min, with a final extension at 72°C for 5 min. Primer C-11, designed from the nucleotide sequence of the tnpA gene of IS Ecp1 (P. D. Stapleton, GenBank accession no. AJ242809), and primer C-5, an internal blaCTX-M primer, were used to amplify the flanking regions upstream of the blaCTX-M genes. All primers designed for this study are shown in Table 1.
TABLE 1.
Oligonucleotide primers used in the study
| Gene or gene region | Primer | Oligonucleotide sequence (5"→3") | GenBank accession no. (reference) | Position of primera |
|---|---|---|---|---|
| blaCTX-M | C-1 | AACACGGATTGACCGTCTTG | D89862 (29) | 82-101 |
| C-2 | TTACAGCCCTTCGGCGAT | D89862 | 981-964 | |
| C-3 | GCTGGTTCTGGTGACCTATTTTACCC | D89862 | 881-907 | |
| C-5 | CCAGCAGCAGCGGAATGCAC | D89862 | 175-156 | |
| Downstream | C-4 | GTTGTCGGGAAGATACGTGA | AF252622 (this study) | 2683-2664 |
| C-6 | CATCACGACTGTGCTGGTCATTAAAC | AF252622 | 2860-2885 | |
| C-7 | GAAATCGCACACCTGGTAATTGATTC | AF252622 | 3035-3050 | |
| Upstream | C-8 | CACTCACCTCACAAGCAACGAA | AJ242809 (unpublished) | 902-923 |
| C-9 | AAATTGACATCCATTACGATTGA | AJ242809 | 553-575 | |
| C-10 | TGAGAATGCAAAAAGCAATGGG | AJ242809 | 252-273 | |
| C-11 | CTTCAAAAAGCATAATCAAAGCCT | AJ242809 | 19-43 | |
| C-12 | ACCATATATCGAGTCATAAAAGCTGA | AJ242809 | 146-121 | |
| C-13 | AAAAATCCCATTGCTTTTTGCATTCT | AJ242809 | 279-254 |
Position counted from the first nucleotide of the entire sequence, as numbered for the GenBank submission.
Differentiation of blaTEM genes.
The blaTEM genes were identified by PCR-restriction fragment length polymorphism (RFLP) analysis (2). The restriction endonucleases used included AluI, BclI, BpmI, BsmaI, HhaI, HpaII, HphI, MseI, NlaIII, and Sau3AI. Restriction endonuclease AluI was supplied by Gibco BRL (Life Technologies, Paisley, United Kingdom), BclI was obtained from Boehringer Mannheim (Mannheim, Germany), and the remaining restriction endonucleases were purchased from New England Biolabs. Four E. coli reference strains, C600(pCFF04) encoding TEM-3, C600(pUD16) encoding TEM-4, C600(pCFF14) encoding TEM-5, and C600(pIF100) encoding TEM-7 (22), were used as controls.
Nucleotide sequence determination.
The nucleotide sequences of the blaSHV and blaTEM genes were determined as described previously (30, 32). The 906-bp fragments of the blaCTX-M genes were also sequenced. To determine the remaining blaCTX-M sequences, plasmid DNAs digested with either BamHI or EcoRI, depending on which enzyme gave the smaller fragment containing blaCTX-M, were used as templates; and the sequence of the entire open reading frame (ORF) was determined. Primers C-1, C-2, and C-3 (Table 1) were used as primers for determination of the blaCTX-M gene sequences. The digested plasmids or amplification products were purified with the QIAquick PCR purification kit (QIAGEN, Crawley, England), and their nucleotide sequences were determined with an ABI PRISM automated sequencing machine (model 373, version 3.3), according to the manufacturer's instructions. The nucleotide sequences of both DNA strands and two independently generated amplimers were determined.
The nucleotide sequences of the flanking regions of the blaCTX-M-14 gene in E. coli strain 8 were determined by using the upstream primers shown in Table 1. The primers used to sequence the upstream region, primers C-8 to C-13, were derived from the nucleotide sequence of the tnpA gene of IS Ecp1 (P. D. Stapleton, GenBank accession no. AJ242809). Walking primers, primers C-4, C-6, and C-7, were designed from data generated in the present study for determination of the sequence of the downstream region. In addition, the nucleotide sequences of the downstream regions of the blaCTX-M-9 and blaCTX-M-13 genes in E. coli strain 2 and K. pneumoniae strain 1, respectively, were determined with primer C-3 (Table 1).
Plasmid DNA analysis, Southern blotting, and hybridization.
Plasmid DNA was extracted by a rapid method (4) and was separated by agarose gel electrophoresis. Plasmids isolated from E. coli strains NCTC 50192 and NCTC 50193 were used as standard size markers. In addition, plasmid DNA from transconjugants was digested with either BamHI or EcoRI. The digested fragments were analyzed by electrophoresis with a 1-kb ladder (Promega) as a DNA size marker. Either plasmid DNAs or restriction fragments were transferred from the agarose gel to a nylon membrane (Boehringer Mannheim) by the method of Southern (39) and were hybridized with digoxigenin-labeled blaSHV, blaTEM, or blaCTX-M gene fragments with the PCR DIG detection system (Boehringer Mannheim).
PFGE.
Pulsed-field gel electrophoresis (PFGE) of chromosomal DNA for strain typing was carried out as described by Gautom (12). Chromosomal DNA was digested with 10 U of XbaI (Gibco BRL) at 37°C for 4 h, according to the supplier's instructions. The DNA fragments were separated by electrophoresis in a 1.2% (wt/vol) agarose gel (Agarose NA; Amersham Pharmacia Biotech AB, Sweden) with an LKB Pharmacia (Uppsala, Sweden) system at 175 V and 12°C for 20 h. The pulse time was increased from 5 to 35 s. A 48.5-kb bacteriophage λ ladder (Bio-Rad, Hemel Hempstead, England) was used as a DNA size marker. The DNA patterns obtained by PFGE were classified visually, and only fragments larger than 48.5 kb, which is the smallest rung of the bacteriophage λ DNA ladder, were considered when the PFGE patterns were compared. The patterns were considered to belong to the same type if there was a difference of no more than three bands (43).
Nucleotide sequence accession numbers.
The nucleotide sequence data for blaCTX-M-9, blaCTX-M-13, and blaCTX-M-14 genes were submitted to the GenBank nucleotide sequence database and assigned accession numbers AF252621, AF252623, and AF252622, respectively.
RESULTS
Bacterial strains.
Each isolate was collected from a different patient, and clinical details are given in Table 2.
TABLE 2.
Sources of the 15 clinical isolates used in the study
| Organism | Date collected (day/mo/yr) | Ward | Specimena | Clinical diagnosis | Antibiotic therapyb |
|---|---|---|---|---|---|
| E. coli 1 | 13/06/97 | Respiratory | Sputum | Bronchopneumonia secondary to chronic bronchitis | Unknown |
| E. coli 2 | 15/08/97 | Cardiology | Sputum | Bronchopneumonia secondary to chronic bronchitis and emphysema | None |
| E. coli 3 | 19/03/97 | Pediatric | NS | Unknown | Unknown |
| E. coli 4 | 24/10/97 | Pediatric | US | Neonatal intracerebral bleeding | Penicillin |
| E. coli 5 | 21/10/98 | Respiratory | Sputum | Low differentiation squamous cell cancer of right lung and chronic pneumonia | None |
| E. coli 6 | 23/10/98 | Respiratory | Sputum | Multiple thrombi, cerebral embolus, and aspiration pneumonia | None |
| E. coli 7 | 30/10/98 | Gastroenterology | Blood | Rectal carcinoma and pneumonia secondary to obstruction | Ceftriaxone |
| E. coli 8 | 06/03/98 | Hematology | Urine | Myelodysplastic syndrome and urinary tract infection | None |
| K. pneumoniae I | 05/10/98 | Neurology | Sputum | Thrombic cerebral embolus and pneumonia | None |
| K. pneumoniae 2 | 21/10/98 | Urology | Sputum | Diabetes mellitus and peripheral neuritis | Unknown |
| K. pneumoniae 3 | 28/10/98 | Respiratory | Sputum | Chronic bronchitis and chronic pulmonary emphysema | Ceftriaxone |
| E. cloacae 1 | 07/03/97 | Neurology | Sputum | Thrombic cerebral embolus and pneumonia | Unknown |
| E. cloacae 2 | 24/04/97 | Hematology | Sputum | Acute myeloblastic leukemia with pneumonia | Unknown |
| E. cloacae 3 | 07/10/98 | Chinese medicine | Sputum | Pneumonia secondary to Parkinson's disease | None |
| C. freundii | 18/03/97 | Surgery | Sputum | Left temporal bone defect | Unknown |
NS, nasopharyngeal swab; US, umbilical swab.
Clinical outcome data were not available.
Susceptibility testing.
All isolates were sensitive to imipenem, and all isolates except E. coli strains 5 and 6 and E. cloacae strains 1 and 3 were intermediately susceptible to cefepime and piperacillin plus tazobactam; E. coli strains 5 and 6 and E. cloacae strains 1 and 3 were resistant to cefepime. E. coli strain 1 and K. pneumoniae strain 2 were resistant to cefoxitin, as were the E. cloacae isolates and the C. freundii strain. On the basis of the MICs of ceftazidime and cefotaxime, three resistance phenotypes were observed among the 15 ESBL producers (Table 3). Nine isolates were more resistant to cefotaxime than to ceftazidime, while three isolates were more resistant to ceftazidime than to cefotaxime. For the remaining three isolates, high cefotaxime and ceftazidime MICs were observed. The presence of clavulanic acid at a fixed concentration of 4 μg/ml greatly reduced the MICs of both cefotaxime and ceftazidime except for those for K. pneumoniae strains 1 and 3.
TABLE 3.
Phenotypic and genotypic characterization of the 15 clinical isolates
| Genus species | MICa (μg/ml)
|
pI | β-Lactamase(s) detected by PCRb | PFGE pattern | Plasmid profile (kb) | ||||
|---|---|---|---|---|---|---|---|---|---|
| ATM | CTX | CTX+ | CAZ | CAZ+ | |||||
| E. coli 1 | 128 | 8 | 0.5 | 64 | 4 | 5.4, 8.2 | SHV-12, TEM-1B∗ | Eco-1 | 130, 10, 8.5 |
| Transconjugantc | 32 | 2 | 0.5 | 16 | 2 | NTd | SHV-12 | 130 | |
| E. coli 2 | 8 | 32 | ≤0.25 | 2 | ≤0.25 | 5.4, 8.1 | CTX-M-9, TEM-1B | Eco-2 | 150, 7.0, 5.0, 4.0 |
| Transconjugant | 4 | 16 | ≤0.25 | 1 | ≤0.25 | NT | CTX-M-9 | 150, 5.0, 4.0 | |
| E. coli 3 | 4 | 16 | ≤0.25 | 1 | ≤0.25 | 5.4, 8.1 | CTX-M-9, TEM-1B | Eco-2 | 150, 7.0, 5.0, 4.0 |
| Transconjugant | 2 | 8 | ≤0.25 | 0.5 | ≤0.25 | NT | CTX-M-9 | 150, 5.0, 4.0 | |
| E. coli 4 | 2 | 32 | NT | 0.5 | ≤0.25 | 8.1 | CTX-M-9 | Eco-3 | 150 |
| E. coli 5 | >128 | 128 | NT | >128 | 0.25 | 8.1 | CTX-M-14, SHV-12, TEM-1B | Eco-4 | 130, 3.5 |
| E. coli 6 | 128 | 64 | NT | 64 | 1 | 8.1 | CTX-M-14, SHV-12, TEM-1B | Eco-4 | 130, 3.5 |
| E. coli 7 | 4 | 32 | ≤0.25 | 1 | ≤0.25 | 5.4, 8.1 | CTX-M-14, TEM-1B | Failede | 130 |
| Transconjugant | 4 | 16 | ≤0.25 | 0.5 | ≤0.25 | NT | CTX-M-14 | 130 | |
| E. coli 8 | 16 | 64 | ≤0.25 | 4 | 0.5 | 5.4, 8.1 | CTX-M-14, TEM-1B∗ | Eco-5 | 130, 5.5, 4.8, 3.5, 2.5, 1.9 |
| Transconjugant | 4 | 8 | ≤0.25 | 1 | ≤0.25 | NT | CTX-M-14 | 130 | |
| K. pneumoniae 1 | 16 | 128 | 16 | 32 | 64 | 5.4, 7.6, 8.2 | CTX-M-13, TEM-1B, SHV-11 | Kp-1 | 55, 35, 7.0 |
| Transconjugant | 8 | 32 | ≤0.25 | 2 | ≤0.25 | NT | CTX-M-13 | 35 | |
| K. pneumoniae 2 | 128 | >128 | ≤0.25 | 32 | 1 | 7.6, 8.1 | CTX-M-14, SHV-11 | Kp-2 | 150, 60, 7.0 |
| Transconjugant | 4 | 32 | ≤0.25 | 1 | ≤0.25 | NT | CTX-M-14 | 60 | |
| K. pneumoniae 3 | 16 | 32 | NT | 8 | 16 | 8.1 | CTX-M-9 | Kp-3 | 150, 7.0, 2.7, 1.9 |
| E. cloacae 1 | 32 | >128 | 0.5 | 8 | 0.5 | 8.1, 9.25 | CTX-M-9 | Ecl-1 | 85, 2.4 |
| Transconjugant | 8 | 32 | ≤0.25 | 2 | ≤0.25 | NT | CTX-M-9 | Plasmid not found | |
| E. cloacae 2 | 64 | 16 | 0.5 | 64 | ≤0.25 | 5.4, 9.25 | SHV-12, TEM-1B | Ecl-2 | Plasmid not found |
| Transconjugant | 8 | 0.5 | ≤0.25 | 8 | ≤0.25 | NT | SHV-12, TEM-1B | Plasmid not found | |
| E. cloacae 3 | >128 | 128 | NT | 128 | 4 | 8.1 | CTX-M-14, SHV-12 | Ecl-3 | 150, 2.4 |
| C. freundii | 128 | 8 | NT | 128 | ≤0.25 | 5.4, 8.2 | SHV-12, TEM-1B | NT | 7.0 |
ATM, aztreonam; CAZ, ceftazidime; CAZ+, ceftazidime plus 4 μg of clavulanic acid per ml; CTX, cefotaxime; CTX+, cefotaxime plus 4 μg of clavulanic acid per ml.
The blaSHV and blaCTX-M genes were characterized by nucleotide sequence analysis, and the blaTEM gene was characterized by PCR-RFLP (2). An asterisk indicates the blaTEM gene that was confirmed by nucleotide sequence analysis.
All transconjugants except those of E. cloacae 2 were E. coli UB1637 transconjugants; the E. cloacae 2 transconjugant was an E. coli UB5201 transconjugant.
NT, not tested.
Despite retesting, no DNA fragments were seen.
Transfer of cefotaxime and ceftazidime resistance markers.
Plasmid transfer of the ESBL phenotype to a laboratory strain of E. coli was successful for 9 of 15 isolates (60%). The susceptibility testing results for the transconjugants are shown in Table 3.
PCR amplification of β-lactamase genes.
Of the 15 ESBL-producing isolates, 4 carried blaTEM, 2 carried blaSHV, and 6 carried both blaSHV and blaTEM (Table 3). The remaining three isolates did not harbor either blaSHV or blaTEM. With Toho-1-specific primers (48), no amplification products were detected from any isolate, but predicted PCR products were obtained with CTX-M-1-specific primers (15). A blaCTX-M amplimer from K. pneumoniae strain 1 was selected for nucleotide sequence analysis. The gene was more closely related to blaToho-2 than to blaCTX-M-1. Primers C-1 and C-2, whose sequences were derived from the nucleotide sequence of the blaToho-2 gene, were used instead of primers specific for CTX-M-1. Twelve isolates were found to carry blaCTX-M genes, of which three harbored both blaCTX-M and blaSHV-12.
Characterization of SHV β-lactamase genes.
Nucleotide sequence analysis of the eight isolates carrying blaSHV genes revealed that six isolates harbored blaSHV-12 and that the remaining isolates carried blaSHV-11. The blaSHV-12 gene has a silent mutation (CTA→CTG [the silent mutation is indicated in boldface]) in the codon encoding the amino acid at position 138, as described previously (33). The blaSHV-11 sequence of K. pneumoniae strain 1 contains five silent mutations (indicated in boldface), at amino acid positions 112 (CAC→CAT), 123 (TGC→TGT), 138 (CTA→CTG), 268 (ACG→ACC), and 287 (GAG→GAA), using the numbering convention of Ambler et al. (1), whereas that of strain 2 carries four silent mutations at amino acid positions 112, 138, 268, and 287, as described above. The silent mutations at amino acid positions 123, 268, and 287 have not previously been described in blaSHV-11, as far as the authors can ascertain.
Characterization of TEM β-lactamase genes.
By using 10 restriction endonucleases, all amplimers of the blaTEM genes from 10 isolates yielded identical RFLP profiles, in which only one silent mutation at nucleotide position 436, using the numbering system of Sutcliffe (41), was detected (data not shown). These profiles were consistent with those of blaTEM-1 variants. Nucleotide sequence analysis of the blaTEM genes from two representative isolates, E. coli strains 1 and 8, showed that both genes were identical to the blaTEM-1B gene described by Goussard and Courvalin (16).
Characterization of CTX-M β-lactamase genes.
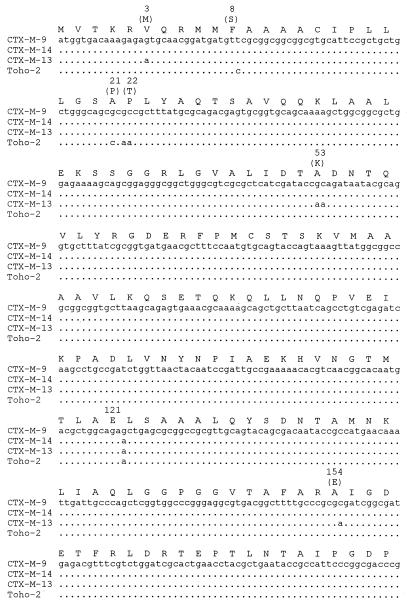
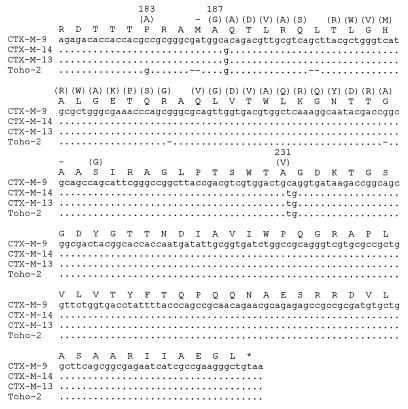
Among the 12 blaCTX-M-carrying isolates, blaCTX-M-9 (5 isolates), blaCTX-M-13 (1 isolate), and blaCTX-M-14 (6 isolates) were identified by nucleotide sequence analysis (Fig. 1). The gene encoding CTX-M-14 differs from that encoding CTX-M-9 by only one amino acid change, at position 231 (Ala→Val), whereas CTX-M-13 differs from CTX-M-9 by four amino acid substitutions, at positions 3 (Val→Met), 53 (Val→Lys), 154 (Ala→Glu), and 231 (Ala→Val). Between CTX-M-13 and CTX-M-14, there are three amino acid substitutions at positions 3, 53, and 154, as described above.
FIG. 1.
Nucleotide sequence alignment of the open reading frames of CTX-M-9 36; this study), CTX-M-13 (this study), CTX-M-14 (this study), and Toho-2 (29). Dots indicate identical nucleotides. Hyphens show nucleotide deletions. Amino acids in parentheses indicate substitutions compared with the sequence of CTX-M-9. The numbering is according to Ambler et al. (1). The asterisk at the end indicates the stop codon.
Nucleotide sequence analysis of the upstream region of blaCTX-M-14 in E. coli strain 8 revealed the presence of at least part of a putative insertion sequence, which showed 100% identity to the tnpA gene of IS Ecp1 (P. D. Stapleton, GenBank accession no. AJ242809) and 99.9% identity to the insertion sequence found upstream of blaCMY-5 (44). PCR amplification with primers C-5 and C-11 (Table 1) was performed to screen for the presence of the insertion sequence in the blaCTX-M-carrying isolates. The predicted amplimers were obtained from the isolates carrying blaCTX-M-13 and blaCTX-M-14, but no PCR products were detected from the isolates carrying blaCTX-M-9. Analysis of the nucleotide sequence of the region downstream of the blaCTX-M-9, blaCTX-M-13, and blaCTX-M-14 genes from E. coli strain 2, K. pneumoniae strain 1, and E. coli strain 8, respectively, revealed that the sequence of the blaCTX-M-14 gene is different from those of the blaCTX-M-9 and blaCTX-M-13 genes. Three hundred forty-five nucleotide bases of the downstream regions of the latter two genes were determined and showed 99% identity. These showed 99 to 100% similarity with the nucleotide sequence downstream of the CTX-M-9 gene (M. Sabate, F. Navarro, J. Barbe, E. Miro, B. Mirelis, and G. Prats, GenBank accession no. AF373104). In addition, analysis of the downstream region of the blaCTX-M-14 gene showed that the first 486 nucleotides had 99% similarity to a part of IS903.B (31). Furthermore, a 5-bp directed repeat sequence was found immediately upstream from the left inverted repeat of ISEcp1 and immediately downstream from the part of the IS903.B gene.
Isoelectric focusing.
Detection of β-lactamases with pIs of 5.4 and 7.6 corresponded with the presence of TEM-1B and SHV-11, respectively. The three CTX-M β-lactamases found in the present study have the same pI, 8.1. The enzyme with a pI of 8.2 was the SHV-12 β-lactamase. The presence of enzymes with pIs of >9.0 was consistent with the production of AmpC enzymes. Only one band with a pI of 8.1 was seen for β-lactamases extracted from the three isolates carrying both the blaSHV-12 and the blaCTX-M-14 genes. The single band detected may indicate the presence of more than one enzyme with identical or, rather, similar pIs. In addition, the absence of bands representing TEM-1 in E. coli strains 5 and 6, SHV-12 in E. cloacae strain 2, and the AmpC β-lactamase in the C. freundii strain and E. cloacae strain 3 may be because enzyme expression was minimal.
Strain typing.
PFGE analysis of the 15 isolates revealed that each of the K. pneumoniae isolates and the E. cloacae isolates gave unique PFGE DNA patterns, whereas five PFGE patterns were seen among the eight E. coli isolates (Table 3). E. coli strains 2 and 3 were indistinguishable, as were strains 5 and 6. Attempts to type E. coli strain 7 failed.
Plasmid DNA analysis.
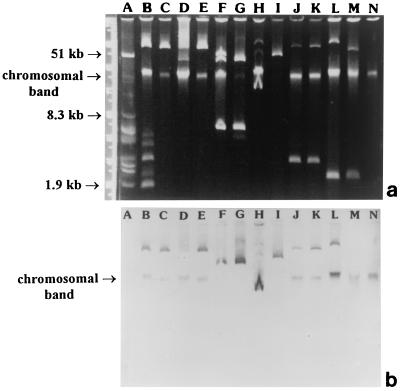
Among the six isolates carrying blaSHV-12, a large plasmid, of approximately 130 kb, from E. coli strain 1 hybridized with the blaSHV probe, but no hybridization with any plasmid from the remaining five isolates was detected (data not shown). Only chromosomal DNAs from these isolates, including the transconjugant of E. cloacae strain 2, hybridized with the blaSHV-specific probe. For the five blaCTX-M-9-carrying isolates, plasmids of approximately 150 kb from E. coli strains 2 and 3 and K. pneumoniae strain 3 hybridized with the blaCTX-M-specific probe, as did chromosomal DNAs from E. coli strain 4 and E. cloacae strain 1. No hybridization with plasmids of either E. coli strain 4 or the E. cloacae strain was observed. Restriction digestion of the plasmids carrying this gene with either BamHI or EcoRI revealed that plasmids from E. coli strains 2 and 3 yielded the same restriction profiles, whereas that from the K. pneumoniae strain showed a unique profile (data not shown). Subsequent Southern blotting and hybridization with the blaCTX-M-specific probe showed that the blaCTX-M-9 genes of the two E. coli isolates were encoded on the same BamHI or EcoRI fragment, whereas that of the K. pneumoniae strain was found on a different fragment. In the present study, only K. pneumoniae strain 1 carried a blaCTX-M-13 gene. This gene was encoded on a single plasmid, of approximately 35 kb (Fig. 2). All CTX-M-14-producing isolates had a plasmid of approximately 60 to 150 kb that hybridized with the blaCTX-M-specific probe (Fig. 2). Restriction digestion of the plasmids with either BamHI or EcoRI showed that each plasmid except those from E. coli strains 5 and 6 carried the blaCTX-M gene on a unique restriction fragment; plasmids from E. coli strains 5 and 6 yielded the same restriction profiles (data not shown). Consistent with this finding was the fact that the blaCTX-M gene was found on fragments of different sizes from all isolates except those from E. coli strains 5 and 6 when the fragments which hybridized with the blaCTX-M-specific probe were indistinguishable.
FIG. 2.
(a) Plasmid DNA profiles of the clinical isolates carrying blaCTX-M genes and their transconjugants; (b) Southern blots hybridized with a blaCTX-M-specific probe. Lanes A, V517 plasmid size marker; lanes B and C, E. coli strain 8 and its transconjugant (blaCTX-M-14), respectively; lanes D and E, E. coli strain 7 and its transconjugant (blaCTX-M-14), respectively; lanes F and G, K. pneumoniae strain 1 and its transconjugant (blaCTX-M-13), respectively; lanes H and I, K. pneumoniae strain 2 and its transconjugant (blaCTX-M-14), respectively; lanes J and K, E. coli strains 5 and 6, respectively (blaCTX-M-14); lanes L, E. cloacae strain 3 (blaCTX-M-14); lanes M and N, E. cloacae strain 1 and its transconjugant (blaCTX-M-9), respectively.
DISCUSSION
Recently, several reports have described ESBLs that do not belong to either the TEM or the SHV family and that are more active against cefotaxime than ceftazidime but that are inhibited by clavulanic acid (3, 5-7, 13-15, 20, 29, 34, 36, 42, 48, 51). They are more closely related to the chromosomal β-lactamase of Klebsiella oxytoca than to the TEM or the SHV β-lactamases (5). These cefotaxime-hydrolyzing β-lactamases include the CTX-M and Toho families, of which four subgroups have been recognized on the basis of amino acid sequence homology (6). The first subgroup, the CTX-M-1 subgroup, includes CTX-M-1 (MEN-1) from E. coli in France (5) and Germany (3), CTX-M-3 from C. freundii and E. coli in Poland (15) and from E. coli in Taiwan (51), and CTX-M-10 from E. coli in Spain (34). The second subgroup is represented by CTX-M-2 and includes CTX-M-2 from Salmonella enterica serovar Typhimurium, E. coli, and Proteus mirabilis in Argentina and from K. pneumoniae in Israel and Paraguay (3); Toho-1 from E. coli in Japan (20); CTX-M-4 from S. enterica serovar Typhimurium in Russia (13); CTX-M-5 from S. enterica serovar Typhimurium in Latvia (7); and CTX-M-6 and CTX-M-7 (previously designated CTX-M-5) from S. enterica serovar Typhimurium in Greece (14). The third subgroup, the Toho-2 subgroup, includes Toho-2 and CTX-M-9 from E. coli in Japan (29) and Spain (36), respectively. The fourth subgroup, the CTX-M-8 subgroup, has only one member, CTX-M-8 from Citrobacter amalonaticus, E. cloacae, and Enterobacter aerogenes, and was first seen in Brazil (6). In addition, kluA-1 and kluA-2, class A chromosomal β-lactamases, have been reported recently from Kluyvera ascorbata in France (C. Humeniuk, G. Arlet, R. Labia, and A. Philippon, GenBank accession nos. AJ272538 and AJ251722, respectively). The kluA-1 β-lactamase has 97 to 99% amino acid identity to members of the CTX-M-2 subgroup, and the nucleotide sequence of kluA-2 is identical to that of CTX-M-5. This finding indicates that the kluA-1 and kluA-2 enzymes from K. ascorbata are likely the progenitors of some plasmid-mediated CTX-M-type enzymes (34).
The clinical isolates used in the present study were screened for the presence of ESBLs by the double-disk diffusion test, and all were positive. Therefore, this report concentrates on the ESBLs that are inhibited by clavulanic acid. All isolates were first screened for the presence of SHV and TEM β-lactamase genes, which are commonly found in members of the family Enterobacteriaceae. As many isolates lacked genes for the TEM and SHV ESBLs but definitely had a phenotype for ESBL production and were found to be more resistant to cefotaxime than to ceftazidime, they were further screened for the presence of blaToho-1 and blaCTX-M-1. Amplification products were detected with CTX-M-1-specific primers only. This may be due to the sequences at the positions that the primers were designed to target, since the amino acid identities among cefotaxime-hydrolyzing enzymes vary from 77 to 99%. It was found that the primers designed to amplify blaCTX-M-1 have nucleotide sequences that are shared by both blaToho-1 and blaToho-2, although some nucleotides are different. Thus, these primers are not specific for the detection of blaCTX-M genes in the CTX-M-1 subgroup only.
This paper describes the occurrence of TEM and SHV β-lactamases in strains from the southern area of mainland China. The TEM β-lactamases that have been reported in the Far East include TEM-52 in Korea (35), TEM-26 in Japan (49), TEM-1 and TEM-10 in southern Taiwan (50, 51), and TEM-1B in Thailand (8). Only TEM-1B was found in the present study. Until 1994, SHV-2 was the only ESBL to have been reported from China (10). Recently, SHV-28, a novel SHV variant, has been reported from China (Y. Yu, W. Zhou, and Y. Chen, GenBank accession no. AF299299). SHV ESBLs that have been described among other Asian countries include SHV-2a and SHV-12 in Korea (26); SHV-2, SHV-12, and SHV-24 in Japan (27, 49); SHV2, SHV-5, and SHV-12 in Taiwan (28, 40, 50); SHV-5 in Singapore (21); and SHV-2a, SHV-5, and SHV-12 in Thailand (8). Recently, two novel SHV variants, SHV-25 and SHV-26, have been reported in Taiwan (9). This paper represents the first report of SHV-12 production by bacteria isolated from mainland China. In addition, species from three different genera of the Enterobacteriaceae, E. coli, E. cloacae, and C. freundii, were found to produce SHV-12, indicating horizontal transfer of this resistance gene.
In the present study, three different CTX-M ESBLs were found, and they were found to be associated with three genera of the family Enterobacteriaceae. One to four amino acid substitutions were found among these enzymes (Fig. 1), but the substitutions did not significantly alter the MICs of cefotaxime (Table 3). Thus, these substitutions do not appear to play an important role in cefotaxime hydrolysis. The kinetics of these enzymes, however, were not studied. It is of interest that CTX-M-13 has a difference of three amino acids from CTX-M-9 and CTX-M-14 at positions 3, 53, and 154. Mutants with intermediate changes must exist, but either these mutations have not yet been discovered or the substitutions alter the efficacy of the β-lactamase, making them difficult to detect.
Both CTX-M-9 and CTX-M-14 enzymes were produced by bacteria of three different genera, suggesting horizontal transfer. PFGE analysis of the clinical isolates indicates the dissemination of these resistance genes in different strains. E. coli strains 2 and 3 were, however, clonal, as were E. coli strains 5 and 6. Seven of the 12 isolates carrying blaCTX-M genes were able to transfer the ESBL phenotype in conjugation experiments, suggesting the spread of blaCTX-M genes by conjugative plasmids. Plasmid fingerprinting of the transconjugants carrying these genes followed by hybridization with the blaCTX-M-specific probe further demonstrated the dissemination of the blaCTX-M genes by different plasmids carrying resistance determinants. This suggests that the genes encoding these β-lactamases are highly mobile. The ISEcp1 insertion sequence observed upstream of the blaCTX-M genes examined in the present study may be involved in the translocation and dissemination of these β-lactamase genes, as was found in the blaCMY-4 gene (P. D. Stapleton, Abstr. 39th Intersci. Conf. Antimicrob. Agents Chemother., abstr. 1457, 1999). In the present study, the blaCTX-M genes were encoded on the chromosome in two isolates, as were the blaSHV-12 genes in five isolates and their transconjugants. This may be explained by the same reasoning that has been applied to the chromosome-encoded Toho-1-like genes, in that mobile elements such as transposons or integrons may be involved in the translocation of these genes (48). This suggestion is strengthened by the occurrence of the bla genes on the chromosomes of transconjugants.
The three enzymes found in the present study have 98% nucleotide homology with Toho-2 (29). However, they share only 86 to 87% amino acid homology since there are nucleotide deletions at four positions in the Toho-2 sequence which are not found in the sequences of the enzymes described here (Fig. 1). In addition, the three enzymes have 78 to 85% amino acid homology with the amino acid sequences of other CTX-M types. Closely related enzymes such as CTX-M-2 in Argentina (3) and Toho-1 in Japan (20), as well as CTX-M-9 in Spain (36) and CTX-M-9, CTX-M-13, and CTX-M-14 in China (this study), have been reported from geographically distant areas. In contrast, Toho-1 (20) and Toho-2 (29), as well as CTX-M-9 (36) and CTX-M-10 (34), which are classified in different subgroups, originated from the same locations. These observations suggest that these genes are the result of divergent evolution from a common ancestor. It also demonstrates the rapid dissemination of these resistance determinants on diverse replicons and through wide-ranging geographical locations.
The strains used for the present study illustrate the widespread dissemination of the blaCTX-M genes on different replicons and among at least three species of the family Enterobacteriaceae. It also highlights the evolution of these genes within a single hospital; other variants will almost certainly exist elsewhere in China. This is supported by a recent submission to GenBank of the sequence of CTX-M-11 from China (C. Minjun, X. Yingchun, and W. Hui, GenBank accession no. AY005110). It was found that CTX-M-11 is closely related to the CTX-M-1 subgroup, whereas the enzymes found in the present study are closely related to the Toho-2 subgroup. Similar divergences of genes within a single locality have been reported elsewhere (20, 29, 34, 36). Recently, CTX-M-3 has been reported from southern Taiwan (51) and two novel cefotaxime-hydrolyzing β-lactamases have been described, CTX-M-12 from K. pneumoniae in Kenya (24) and UOE-1 from E. coli in Japan (T. Muratani, K. Takahashi, and T. Matsumoto, GenBank accession no. AY013478). Both novel enzymes are closely related to the CTX-M-1 subgroup. These findings suggest that variants of cefotaxime-hydrolyzing β-lactamases are becoming more common.
The ESBL-producing isolates evaluated in the present study were classified into three groups on the basis of their resistance phenotypes. The nine isolates that were predominately resistant to cefotaxime produced CTX-M ESBLs, whereas the three isolates that were characterized by high ceftazidime MICs produced SHV-12. In addition, the three isolates resistant to both antibiotics were found to produce both CTX-M and SHV ESBLs. It is worrying that bacteria that harbor multiple β-lactamase genes are being reported with increasing frequency, and we describe the occurrence of SHV and CTX-M ESBLs produced by single strains. The high MICs of both cefotaxime and ceftazidime for strains with more than one ESBL that are reported here, particularly compared with the MICs for bacteria that produce a single ESBL, illustrate the increasing levels of resistance to β-lactams of bacteria of clinical significance. The ease with which such bacteria can be isolated should be a cause for grave concern and indicate the need for more detailed surveillance and epidemiological surveys in this region, which has increasing contact with the rest of the world.
Acknowledgments
We thank the Royal Thai Government for providing support for Aroonwadee Chanawong.
We are grateful to G. A. Jacoby and E. Collatz for providing strains that produce the standard SHV and TEM β-lactamases and to Hui-Ling Chen for providing clinical data on the isolates used in the study.
REFERENCES
- 1.Ambler, R. P., A. F. W. Coulson, J. M. Frere, J. M. Ghuysen, B. Joris, M. Forsman, R. C. Levesque, G. Tiraby, and S. G. Waley. 1991. A standard numbering scheme for the class A β-lactamases. Biochem. J. 276:269-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arlet, G., G. Brami, D. Decre, A. Flippo, O. Gaillot, P. H. Lagrange, and A. Philippon. 1995. Molecular characterisation by PCR-restriction fragment length polymorphism of TEM β-lactamases. FEMS Microbiol. Lett. 134:203-208. [DOI] [PubMed] [Google Scholar]
- 3.Bauernfeind, A., I. Stemplinger, R. Jungwirth, S. Ernst, and J. M. Casellas. 1996. Sequences of β-lactamase genes encoding CTX-M-1 (MEN-1) and CTX-M-2 and relationship of their amino acid sequences with those of other β-lactamases. Antimicrob. Agents Chemother. 40:509-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bennett, P. M., J. Heritage, and P. M. Hawkey. 1986. An ultra-rapid method for the study of antibiotic resistance plasmids. J. Antimicrob. Chemother. 18:421-424. [DOI] [PubMed] [Google Scholar]
- 5.Bernard, H., C. Tancrede, V. Livrelli, A. Morand, M. Barthelemy, and R. Labia. 1992. A novel plasmid-mediated extended-spectrum β-lactamase not derived from TEM- or SHV-type enzymes. J. Antimicrob. Chemother. 29:590-592. [DOI] [PubMed] [Google Scholar]
- 6.Bonnet, R., J. L. M. Sampaio, R. Labia, C. De Champs, D. Sirot, C. Chanal, and J. Sirot. 1999. A novel CTX-M β-lactamase (CTX-M-8) in cefotaxime-resistant Enterobacteriaceae isolated in Brazil. Antimicrob. Agents Chemother. 44:1936-1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bradford, P. A., Y. Yang, D. Sahm, I. Grope, D. Gardovska, and G. Storch. 1998. CTX-M-5, a novel cefotaxime-hydrolyzing β-lactamase from an outbreak of Salmonella typhimurium in Latvia. Antimicrob. Agents Chemother. 42:1980-1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chanawong, A., F. H. M'Zali, J. Heritage, A. Lulitanond, J. Xiong, and P. M. Hawkey. 1999. Widespread distribution of an SHV-5-like extended-spectrum β-lactamases among Enterobacteriaceae isolated from Thailand and the People's Republic of China. J. Antimicrob. Chemother. 44(Suppl. A):92. [Google Scholar]
- 9.Chang, F.-Y., L. K. Siu, C.-P., Fung, M.-H. Huang, and M. Ho. 2001. Diversity of SHV and TEM β-lactamases in Klebsiella pneumoniae: gene evolution in northern Taiwan and two novel β-lactamases, SHV-25 and SHV-26. Antimicrob. Agents Chemother. 45:2407-2413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheng, Y., and M. Chen. 1994. Extended-spectrum β-lactamases in clinical isolates of Enterobacter gergoviae and Escherichia coli in China. Antimicrob. Agents Chemother. 38:2838-2842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Danel, F., L. M. C. Hall, D. Gur, H. E. Akalin, and M. Livermore. 1995. Transferable production of PER-1 β-lactamase in Pseudomonas aeruginosa. J. Antimicrob. Chemother. 35:281-294. [DOI] [PubMed] [Google Scholar]
- 12.Gautom, R. K. 1997. Rapid pulsed-field gel electrophoresis protocol for typing of Escherichia coli O157: H7 and other gram-negative organisms in 1 day. J. Clin. Microbiol. 35:2977-2980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gazouli, M., E. Tzelepi, S. V. Sidorenko, and L. S. Tzouvelekis. 1998. Sequence of the gene encoding a plasmid-mediated cefotaxime-hydrolyzing class A β-lactamase (CTX-M-4): involvement of serine 237 in cephalosporin hydrolysis. Antimicrob. Agents Chemother. 42:1259-1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gazouli, M., E. Tzelepi, A. Markogiannakis, N. J. Legakis, and L. S. Tzouvelekis. 1998. Two novel plasmid-mediated cefotaxime-hydrolyzing β-lactamases (CTX-M-5 and CTX-M-6) from Salmonella typhimurium. FEMS Microbiol. Lett. 165:289-293. [DOI] [PubMed] [Google Scholar]
- 15.Gniadkowski, M., I. Schneider, A. Palucha, R. Jungwirth, B. Mikiewicz, and A. Bauernfeind. 1998. Cefotaxime-resistant Enterobacteriaceae isolates from a hospital in Warsaw, Poland: identification of a new CTX-M-3 cefotaxime-hydrolyzing β-lactamase that is closely related to the CTX-M-1/MEN-1 enzyme. Antimicrob. Agents Chemother. 42:827-832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goussard, S., and P. Courvalin. 1991. Sequence of the genes blaT-1B and blaT-2. Gene 102:71-73. [DOI] [PubMed] [Google Scholar]
- 17.Heritage, J., P. M. Hawkey, N. Todd, and I. J. Lewis. 1992. Transposition of the gene encoding a TEM-12 extended-spectrum β-lactamase. Antimicrob. Agents Chemother. 36:1981-1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hibbert-Rogers, L. C. F., J. Heritage, N. Todd, and P. M. Hawkey. 1994. Convergent evolution of TEM-26, a β-lactamase with extended-spectrum activity. J. Antimicrob. Chemother. 33:707-720. [DOI] [PubMed] [Google Scholar]
- 19.Holt, A., and D. Brown. 1989. Antimicrobial susceptibility testing, p. 176-196. In P. M. Hawkey and D. A. Lewis (ed.), Medical bacteriology. IRL Press, Oxford, United Kingdom.
- 20.Ishii, Y., A. Ohno, H. Taguchi, S. Imajo, M. Ishiguro, and H. Matsuzawa. 1995. Cloning and sequencing of the gene encoding a cefotaxime-hydrolyzing class A β-lactamase isolated from Escherichia coli. Antimicrob. Agents Chemother. 39:2269-2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jacoby, G. A., and A. A. Medeiros. 1991. More extended-spectrum β-lactamases. Antimicrob. Agents Chemother. 35:1697-1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jacoby, G. A., and L. Sutton. 1991. Properties of plasmids responsible for production of extended-spectrum β-lactamases. Antimicrob. Agents Chemother. 35:164-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jarlier, V., M. H. Nicolas, G. Fournier, and A. Philippon. 1988. Extended broad-spectrum β-lactamases conferring transferable resistance to newer β-lactam agents in Enterobacteriaceae: hospital prevalence and susceptibility patterns. Rev. Infect. Dis. 10:867-878. [DOI] [PubMed] [Google Scholar]
- 24.Kariuki, S., J. E. Corkill, G. Revathi, R. Musoke, and C. A. Hart. 2001. Molecular characterisation of a novel plasmid-encoded cefotaximase (CTX-M-12) found in clinical Klebsiella pneumoniae isolates from Kenya. Antimicrob. Agents Chemother. 45:2141-2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kelly, M. T., D. J. Brenner, and J. J. Farmer III. 1985. Enterobacteriaceae, p. 263-277. In E. H. Lennette, A. Balows, W. J. Hausler, Jr., and H. J. Shadomy (ed.), Manual of clinical microbiology, 5th ed. American Society for Microbiology, Washington, D.C.
- 26.Kim, J., Y. Kwon, H. Pai, J.-W. Kim, and D.-T. Cho. 1998. Survey of Klebsiella pneumoniae strains producing extended-spectrum β-lactamases: prevalence of SHV-12 and SHV-2a in Korea. J. Clin. Microbiol. 36:1446-1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kurokawa, H., T. Yagi, N. Shibata, K. Shibayama, K. Kamachi, and Y. Arakawa. 2000. A new SHV-derived extended-spectrum β-lactamase (SHV-24) that hydrolyzes ceftazidime through a single-amino-acid substitution (D179G) in the Ω-loop. Antimicrob. Agents Chemother. 44:1725-1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu, P. Y. F., J. C. Tung, S. C. Ke, and S. L. Chen. 1998. Molecular epidemiology of extended-spectrum β-lactamase-producing Klebsiella pneumoniae isolates in a district hospital in Taiwan. J. Clin. Microbiol. 36:2759-2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ma, L., Y. Ishii, M. Ishiguro, H. Matsuzawa, and K. Yamaguchi. 1998. Cloning and sequencing of the gene encoding Toho-2, a class A β-lactamase preferentially inhibited by tazobactam. Antimicrob. Agent Chemother. 42:1181-1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mabilat, C., S. Goussard, W. Sougakoff, R. C. Spencer, and P. Courvalin. 1990. Direct sequencing of the amplified structural gene and promoter for the extended-spectrum β-lactamase TEM-9 (RHH-1) of Klebsiella pneumoniae. Plasmid 23:27-34. [DOI] [PubMed] [Google Scholar]
- 31.Mollet, B., S. Iida, and W. Arber. 1985. An active variant of the prokaryotic transposable element IS903 carries an amber stop codon in the middle of an open reading frame. Mol. Gen. Genet. 199:534-536. [DOI] [PubMed] [Google Scholar]
- 32.M'Zali, F. M., D. M. Gascoyne-Binzi, J. Heritage, and P. M. Hawkey. 1996. Detection of mutations conferring extended-spectrum activity on SHV β-lactamase using polymerase chain reaction single strand conformational polymorphism (PCR-SSCP). J. Antimicrob. Chemother. 37:797-802. [DOI] [PubMed] [Google Scholar]
- 33.Nuesch-Inderbinen, M. T., F. H. Kayser, and H. Hachler. 1997. Survey and molecular genetics of SHV β-lactamases in Enterobacteriaceae in Switzerland: two novel enzymes, SHV-11 and SHV-12. Antimicrob. Agents Chemother. 41:943-949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oliver, A., J. C. Pérez-D|$$|Aa|fiaz, T. M. Coque, F. Baquero, and R. Cantón. 2001. Nucleotide sequence and characterisation of a novel cefotaxime-hydrolysing β-lactamase (CTX-M-10) isolated in Spain. Antimicrob. Agents Chemother. 45:616-620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pai, H., S. Lyu, J. H. Lee, J. Kim, Y. Kwon, J.-W. Kim, and K. W. Choe. 1999. Survey of extended-spectrum β-lactamases in clinical isolates of Escherichia coli and Klebsiella pneumoniae: prevalence of TEM-52 in Korea. J. Clin. Microbiol. 37:1758-1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sabate, M., R. Tarrago, F. Navarro, E. Miro, C. Verges, J. Barbe, and G. Prats. 2000. Cloning and sequence of the gene encoding a novel cefotaxime-hydrolyzing β-lactamase (CTX-M-9) from Escherichia coli in Spain. Antimicrob. Agents Chemother. 44:1970-1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shannon, K. P., A. King, I. Phillips, M. H. Nicolas, and A. Philippon. 1990. Importation of organisms producing broad-spectrum SHV-group β-lactamases into the United Kingdom. J. Antimicrob. Chemother. 25:343-351. [DOI] [PubMed] [Google Scholar]
- 38.Shen, D., D. J. Biedenbach, P. L. Winokur, M. A. Pfaller, and R. N. Jones. 1999. Phenotypic and genotypic characterisations of Chinese strains of Escherichia coli producing extended-spectrum β-lactamases. Diagn. Microbiol. Infect. Dis. 34:159-164. [DOI] [PubMed] [Google Scholar]
- 39.Southern, E. M. 1975. Detection of specific sequences among DNA fragments separated by agarose gel electrophoresis. J. Mol. Biol. 98:503-517. [DOI] [PubMed] [Google Scholar]
- 40.Sui, L. K., P.-L. Lu, P.-R. Hsueh, F. M. Lin, S.-C. Chang, K.-T. Luh, M. Ho, and C.-Y. Lee. 1999. Bacteremia due to extended-spectrum β-lactamase-producing Escherichia coli and Klebsiella pneumoniae in a pediatric oncology ward: clinical features and identification of different plasmids carrying both SHV-5 and TEM-1 genes. J. Clin. Microbiol. 37:4020-4027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sutcliffe, J. G. 1978. Nucleotide sequence of the ampicillin resistance gene of Escherichia coli plasmid pBR322. Proc. Natl. Acad. Sci. USA 75:3737-3741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tassios, P. T., M. Gazouli, E. Tzelepi, H. Milch, N. Kozlova, S. Sidorenko, N. J. Legakis, and L. S. Tzouvelekis. 1999. Spread of a Salmonella typhimurium clone resistant to expanded-spectrum cephalosporins in three European countries. J. Clin. Microbiol. 37:3774-3777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tenover, F. C., R. D. Arbeit, R. V. Goering, P. A. Mickelsen, B. E. Murray, D. H. Persing, and B. Swaminathan. 1995. Interpreting chromosomal DNA restriction patterns produced by pulsed field gel electrophoresis: criteria for bacterial strain typing. J. Clin. Microbiol. 33:2233-2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wu, S. W., K. Dornbusch, G. Kronvall, and M. Norgren. 1999. Characterization and nucleotide sequence of a Klebsiella oxytoca cryptic plasmid encoding a CMY-type β-lactamase: confirmation that the plasmid-mediated cephamycinase originated from the Citrobacter freundii AmpC β-lactamase. Antimicrob. Agents Chemother. 43:1350-1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xiong, J. 1998. Detection of ESBL producing gram-negative bacilli with Etest ESBL strips. J. Clin. Lab. Sci. 16:138-140. (In Chinese.)
- 46.Xiong, J. 1999. Surveillance of the antimicrobial resistance of the common pathogenic bacteria isolated from thirteen large hospitals in Guangzhou, PRC during late 1998. Guangzhou Med. 30:58-63. (In Chinese.)
- 47.Xu, Y., M. Chen, D. J. Biedenbach, L. M. Deshpande, and R. N. Jones. 1999. Evaluation of the in vitro antimicrobial activity of cefepime compared to other broad-spectrum beta-lactams tested against recent clinical isolates from 10 Chinese hospitals. Chinese Antimicrobial Resistance Study Group. Diagn. Microbiol. Infect. Dis. 35:135-142. [DOI] [PubMed] [Google Scholar]
- 48.Yagi, T., H. Kurokawa, K. Senda, S. Ichiyama, H. Ito, S. Ohsuka, K. Shibayama, K. Shimokata, N. Kato, M. Ohta, and Y. Arakawa. 1997. Nosocomial spread of cephem-resistant Escherichia coli strains carrying multiple Toho-1-like β-lactamase genes. Antimicrob. Agents Chemother. 41:2606-2611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yagi, T., H. Kurokawa, N. Shibata, K. Shibayama, and Y. Arakawa. 2000. A preliminary survey of extended-spectrum β-lactamases (ESBLs) in clinical isolates of Klebsiella pneumoniae and Escherichia coli in Japan. FEMS Microbiol. Lett. 184:53-56. [DOI] [PubMed] [Google Scholar]
- 50.Yan, J. J., S. M. Wu, S. H. Tsai, J. J. Wu, and J. J. Su. 2000. Prevalence of SHV-12 among clinical isolates of Klebsiella pneumoniae producing extended-spectrum β-lactamases and identification of a novel AmpC enzyme (CMY-8) in southern Taiwan. Antimicrob. Agents Chemother. 44:1438-1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yan, J. J., W. C. Ko, S. H. Tsai, H. M. W, Y. T. Jin, and J. J. Wu. 2000. Dissemination of CTX-M-3 and CMY-2 β-lactamases among clinical isolates of Escherichia coli in Southern Taiwan. J. Clin. Microbiol. 38:4320-4325. [DOI] [PMC free article] [PubMed] [Google Scholar]