Abstract
Gram-negative sepsis is related to the activation of interconnected inflammatory cascades in response to bacteria and their products. Recent work showed that flagellin, the monomeric subunit of bacterial flagella, triggers innate immune responses mediated by Toll-like receptor 5. Here, we compared the effects of Salmonella enterica serovar Enteritidis lipopolysaccharide (LPS) and recombinant Salmonella enterica serovar Muenchen flagellin administered intravenously (100 μg) to mice. Flagellin and LPS both elicited a prototypical systemic inflammatory response, with increased levels of tumor necrosis factor alpha, gamma interferon, interleukin 6 and 10, and nitrate in plasma. Flagellin induced a widespread oxidative stress, evidenced by an increase in malondialdehyde and a decrease in reduced glutathione in most organs, as well as liver (increased plasma aminotransferases), but not renal, injury. Alternatively, LPS resulted in a less severe oxidative stress and triggered renal, but not liver, damage. Sequestration of polymorphonuclear neutrophils (increased myeloperoxidase activity) in the lungs was observed with both toxins, while only LPS recruited neutrophils in the gut. In additional experiments, the simultaneous administration of small doses of LPS and flagellin (10 μg) induced a synergistic enhancement of the production of proinflammatory cytokines. Our data support a novel concept implicating flagellin as a mediator of systemic inflammation, oxidant stress, and organ damage induced by gram-negative bacteria.
It is generally acknowledged that the systemic inflammatory response triggered by pathogenic gram-negative bacteria largely depends on the release of lipopolysaccharide (LPS) from the bacterial cell wall (13). Therefore, the systemic administration of LPS has been commonly used to reproduce the typical features of clinical septic shock, including the production of proinflammatory mediators, the development of cardiovascular failure, and multiple organ damage, leading eventually to death (18). However, several important differences distinguish bacterial and LPS-induced shock, notably regarding the kinetics and distribution of proinflammatory gene expression, which limit the inferences that can be drawn from endotoxemic models (11). The many differences between the effects of LPS versus live bacteria support the concept that bacterial components distinct from LPS are additional triggers of systemic inflammation and shock during the course of severe infections with gram-negative bacteria.
A possible candidate for eliciting systemic inflammation and shock is flagellin, the main protein subunit of the flagellar filament from motile microorganisms (3, 22). In addition to its primary role as a structural component of the bacterial flagella, flagellin may act as an exotoxin, being released from motile gram-negative bacteria in vitro (7, 15) and being detectable in significant amounts as a freely circulating protein in the blood of septic rats (7). Recent studies from our laboratory and other investigators indicated that flagellin activates the nuclear translocation of NF-κB and induces the release of a host of proinflammatory mediators in vitro and in vivo (6, 7, 10, 19, 20, 29). Efforts to identify the signaling pathways mediating these effects led to the recent demonstration that flagellin binds and activates the Toll-like receptor 5 (TLR5; 12) and activates interleukin 1 (IL-1) receptor-associated kinase (IRAK) (20). Here, we have investigated further the role of flagellin as a proinflammatory mediator, comparing its effects to those of LPS (both from Salmonella species), focusing on the development of systemic inflammation, the sequestration of polymorphonuclear neutrophils, and the generation of oxidative stress in tissues, as well as the occurrence of organ injury.
MATERIALS AND METHODS
Purified recombinant Salmonella enterica serovar.
Muenchen flagellin was prepared as previously described (7). Briefly, the gene fragment corresponding to amino acids 1 to 156 of the flagellin gene of S. enterica serovar Muenchen was generated by PCR amplification with a sense primer designated 1S (5′-CGCGGATCCCAATGGCACAAGTCATTAATACAAACA) and an antisense primer designated 468A (5′-TCCGCTCGAGTTAAATAGTTTCACCGTCGTTGGCACC). The entire flagellin gene was amplified with primers 1S and 1530A (5′TCCGCTCGAGTTAACGCAGTAAAGAGAGGACGTTTTG). Underlined nucleotides represent adapter sequences added to the ends of primers to maintain the proper reading frame and facilitate cloning (BamHI recognition sites on sense primers and XhoI sites on antisense primers). Template DNA for PCRs was plasmid CL402, a clone of pBR322 containing a 3.8-kb EcoRI fragment of S. enterica serovar Muenchen chromosomal DNA that harbors the 1.5-kb flagellin gene. PCR-generated flagellin DNA was digested with BamHI plus XhoI, gel purified, and subcloned into the BamHI-XhoI sites at the 3′ end of the glutathione S-transferase (GST) gene in expression vector pGEX-5X-2 (Pharmacia Biotech, Piscataway, N.J.) and pET 30C (Novagen). A single colony of E. coli DH5a (Life Technologies, Gaithersburg, Md.) containing the desired plasmid was grown at 37°C in Luria broth containing 100 μg of ampicillin/ml to an A600 of 0.5 and then induced for 3 h with 0.5 mM IPTG (isopropyl-β-d-thiogalactopyranoside). Following induction, bacteria were harvested and washed with STE buffer (10 mM Tris [pH 8], 50 mM NaCl, 1 mM EDTA). Cells were suspended in STE buffer containing 100 μg of lysozyme per ml, incubated for 45 min on ice, and then adjusted to 5 mM dithiothreitol (DTT). After two freeze thaws, the cell suspension was sonicated and clarified by centrifugation at 10,000 × g. The soluble lysate was applied to a glutathione-agarose column, washed with STED buffer (STE plus 5 mM DTT), and then eluted with STED buffer containing 10 mM reduced glutathione. The purity of each eluted fusion protein was analyzed by sodium dodecyl sulfate gel electrophoresis. Purified proteins were dialyzed against phosphate-buffered saline (PBS), quantified by the Bradford method, and stored at −70°C.
To remove any possible contaminant LPS, purified flagellin was passed through a polymyxin B column as previously described (7), resulting in a flagellin preparation containing less than 20 pg of LPS/μg of flagellin, as measured by the chromogenic Limulus amebocyte assay.
Experimental protocols.
In vivo studies were performed in accordance with National Institutes of Health guidelines and with the approval of the local institutional animal care and use committee.
Eighty-five male BALB/c mice (8 to 10 weeks old, 25 to 30 g) were used in a first series of experiments. At baseline, the animals received an intravenous injection, via the tail vein, of either 100 μg (4 mg/kg of body weight) of recombinant S. enterica serovar Muenchen flagellin (n = 40 mice) or 100 μg (4 mg/kg) of S. enteritidis LPS, given in 0.2 ml of vehicle (10 mM PBS [pH 7.4]). A group of five mice not receiving LPS or flagellin was used for control purposes. The dose of LPS administered in this study was selected on the basis of numerous previous works evaluating the effects of LPS in rodents, where doses in the milligram-per-kilogram range were generally administered (9, 17, 31, 33). Accordingly, we used a similar dose of flagellin. At selected time points (from 1 to 8 h after the injection), the animals were anesthetized with pentobarbital (60 mg/kg intraperitoneally). Blood was obtained by cardiac puncture, and a thoraco-laparotomy was performed to harvest the lungs, heart, liver, kidneys, and small intestine, which were immediately frozen in liquid nitrogen and then stored at −70°C.
In a second series of experiments, we investigated a possible synergy between the effects of LPS and flagellin, administered at smaller doses. Mice (n = 5 to 6/group) received an intravenous (i.v.) injection of LPS or flagellin (20 μg/mouse) or a combination of both toxins (10 μg of LPS plus 10 μg of flagellin/mouse). The animals were then sacrificed at selected time-points (1 to 4 h after the injection) for the measurements of plasma cytokines and for biochemical measurements in lung tissue (described below).
Measurements. (i)Circulating levels of TNF-α, IFN-γ, IL-6, and IL-10.
The levels of the different cytokines in plasma were determined by commercially available enzyme-linked immunosorbent assays (R&D Systems, Minneapolis, Minn.), according to the manufacturer’s protocol. Plasma samples were diluted 1:2 to 1:10 in mice challenged with LPS or flagellin, and were assayed undiluted in control mice.
(ii) Plasma AST, ALT, and urea.
The concentrations of aspartate aminotransferase (AST), alanine aminotransferase (ALT), and urea were measured in plasma samples with kits obtained from Sigma Chemicals (St. Louis, Mo.), according to the manufacturer’s protocol.
(iii) Plasma nitrate and nitrite.
Plasma nitrate and nitrite were measured as an index of nitric oxide (NO) production. First, nitrate in the plasma was reduced to nitrite by incubation with nitrate reductase (610 mU/ml) and NADPH (170 mM) at room temperature for 3 h. After 3 h, the nitrite concentration in the samples was measured by the Griess reaction, by adding 100 μl of Griess reagent (0.1% naphthalethylenediamine dihydrochloride in H2O and 1% sulfanilamide in 5% concentrated H3PO4 [1:1 volume]). The optical density at 550 nm (OD550 [corrected for A650]) was measured in a Spectramax microplate reader. Nitrite concentrations were calculated by comparison of the OD550 of standard solutions of sodium nitrite prepared in PBS.
(iv) MPO.
Tissues were homogenized (50 mg/ml) in 0.5% hexadecyltrimethylammonium bromide in 10 mM 3-(N-morpholino) propanesulfonic acid (MOPS) and centrifuged at 15,000 × g for 40 min. The suspension was then sonicated three times for 30 s. An aliquot of supernatant was mixed with a solution of 1.6 mM tetramethylbenzidine and 1 mM hydrogen peroxide. Activity was measured spectrophotometrically as the change in A650 at 37°C with a Spectramax microplate reader (Molecular Devices, Sunnyvale, Calif.). Results are expressed as milliunits of myeloperoxidase (MPO) activity per milligram of protein, as determined by the Bradford assay.
(v) MDA assay.
Malondialdehyde (MDA) formation was utilized to quantify the lipid peroxidation in tissues and measured as thiobarbituric acid-reactive material. Tissues were homogenized (100 mg/ml) in 1.15% KCl buffer. Homogenates (200 μl) were then added to a reaction mixture consisting of 1.5 ml of 0.8% thiobarbituric acid, 200 μl of 8.1% sodium dodecyl sulfate, 1.5 ml of 20% acetic acid (pH 3.5), and 600 μl of distilled H2O and heated at 90°C for 45 min. After cooling to room temperature, the samples were cleared by centrifugation (10,000 × g, 10 min), and their A532 was measured with 1,1,3,3-tetramethoxypropane as an external standard. The level of lipid peroxides was expressed as nanomoles of MDA per milligram of protein.
(vi) Glutathione assay.
The levels of reduced glutathione were determined as an index of antioxidant reserves in tissues. Tissues were homogenized (100 mg/ml) in 5% sulfosalicylic acid. The homogenates were centrifuged at 10,000 × g for 20 min, and an aliquot of the clear supernatant (20 μl) was combined with 0.3 M Na2HPO4 (160 μl) and 0.04% 5,5′-dithiobis-(2-nitrobenzoic acid) in 1% sodium citrate (20 μl). After 10 min of incubation at room temperature, A405 was read in a Spectramax microplate reader. Concentrations of GSH were calculated from a standard curve constructed with known concentrations of reduced glutathione and were expressed in micrograms per 100 milligrams of wet tissue.
Statistical analysis.
All of the results are presented as means ± standard errors. Plasma cytokine levels were compared between groups at selected time points by means of a nonparametric test (Mann-Whitney). All the other parameters were statistically compared by analysis of variance, followed by Bonferroni adjustment. Statistical significance was assigned to a P value of <0.05.
Reagents.
S. enteritidis LPS and all other chemicals were purchased from Sigma Chemicals.
RESULTS
Time course of plasma cytokines and nitrate.
Both LPS and flagellin induced a significant release of tumor necrosis factor alpha (TNF-α), gamma interferon (IFN-γ), IL-6, and IL-10, as shown in Table 1. In the case of LPS, the different cytokines (except IFN-γ) showed an early peak followed by a progressive decrease. The increase in cytokines produced by flagellin was smaller than that of LPS, and its time course was different. The levels of TNF-α and IL-10 had increased already after 1 h and remained stable thereafter, while IL-6 slightly decreased at 4 and 8 h, after an early release at 1 and 2 h. Regarding IFN-γ, the time courses of its increase were similar between LPS and flagellin, marked by a progressive release, starting from the second hour postinjection.
TABLE 1.
Time course of plasma cytokinesa
| Cytokine | Concn of cytokine (pg/ml) atb:
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Control | 1 h | 2 h | 4 h | 8 h | |||||
| L | F | L | F | L | F | L | F | ||
| TNF-α | 0 | 2,800 (447) | 386* (50) | 1,898 (123) | 144* (13) | 588 (67) | 247* (176) | 245 (138) | 358 (144) |
| IFN-γ | 0.2 (0.2) | 1.7 (1.2) | 2.3 (1.9) | 72 (21) | 86 (29) | 989 (165) | 430* (59) | 1,312 (238) | 430* (54) |
| IL-6 | 13 (4) | 4,629 (1,149) | 549* (83) | 20,197 (1,810) | 651* (119) | 9,934 (340) | 290* (22) | 5,558 (860) | 277* (39) |
| IL-10 | 11 (8) | 1,388 (252) | 83* (7) | 1,801 (476) | 98* (17) | 1,061 (194) | 97* (18) | 356 (52) | 75* (17) |
Conscious mice were challenged at baseline with an i.v. injection of S. enterica serovar Enteritidis LPS (L) or S. enterica serovar Muenchen flagellin (F), both at 4 mg/kg (100 μg/mouse). A group of five mice not treated with LPS or flagellin was used for control purposes. Mice were killed after 1, 2, 4 and 8 h, and plasma was obtained for the measurement of circulating cytokines. n = 9 to 10 mice/group at each time point.
Values are means with standard errors given in parentheses. *, P < 0.05 for LPS versus flagellin. All values in the L and F groups were significantly higher than those in control mice.
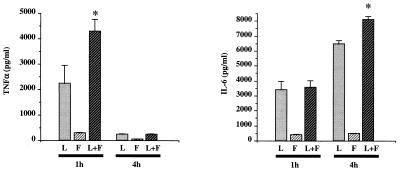
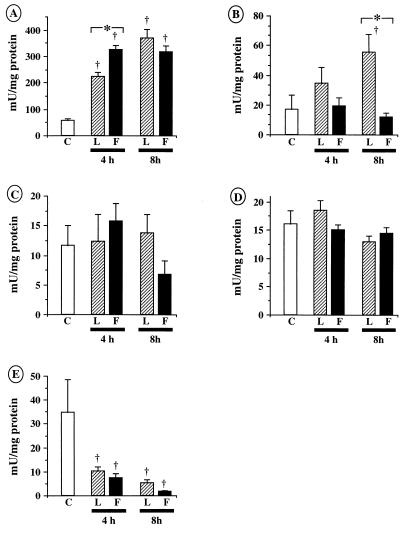
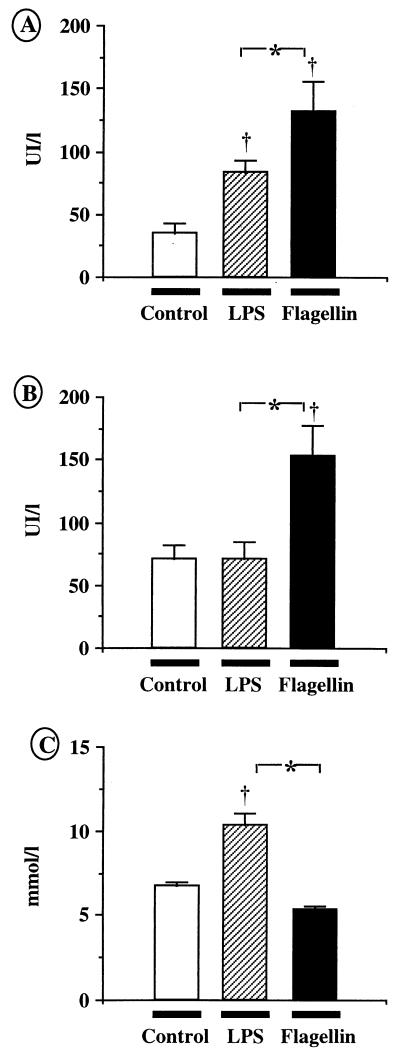
The effects of LPS and flagellin at lower doses and of the coadministration of both LPS and flagellin on the circulating levels of TNF-α and IL-6 are shown in Fig. 1. When compared to the effect of each cytokine separately, the release of both cytokines was significantly enhanced when LPS and flagellin were injected together. At 1 h, the levels of TNF-α were 2,241 ± 704 (LPS), 288 ± 41 (flagellin), and 4,293 ± 476 (LPS plus flagellin; P < 0.05 versus LPS or flagellin alone) pg/ml, whereas the levels of IL-6 at 4 h reached 6,575 ± 166 (LPS), 470 ± 42 (flagellin), and 8,084 ± 225 (LPS plus flagellin; P < 0.05 versus LPS or flagellin alone) pg/ml.
FIG. 1.
Time course of plasma cytokines after the combined administration of LPS (L) and flagellin (F). Conscious mice received an i.v. injection of S. enterica serovar Enteritidis LPS (20 μg) or recombinant S. enterica serovar Muenchen flagellin (20 μg), or a combination of both toxins (each at 10 μg). Plasma was obtained after 1 and 4 h for the determination of the circulating levels of TNF-α (A) and IL-6 (B). A significant synergy between LPS and flagellin was noted for TNF-α (at 1 h) and IL-6 (at 4 h). n = 5 to 6 mice/group. Means ± standard errors: *, P < 0.05 for LPS plus flagellin versus either LPS or flagellin alone.
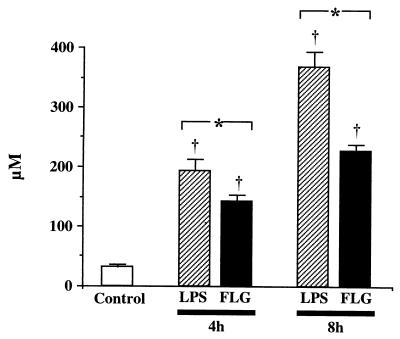
Figure 2 depicts the time course of plasma nitrate, an indicator of NO production, after flagellin or LPS administration. Compared to control values (31.2 ± 4.7 μM), plasma nitrate markedly increased at 4 and 8 h following the injection of both toxins. The levels reached with LPS were significantly greater than with flagellin (at 8 h, values for LPS and flagellin of 368.5 ± 24.6 and 226.4 ± 12.1 μM, respectively).
FIG. 2.
Time course of plasma nitrate. Conscious mice received an i.v. injection of S. enterica serovar enteritidis LPS (100 μg) or recombinant S. enterica serovar muenchen flagellin (FLG; 100 μg) and were killed after 4 or 8 h for the measurement of plasma nitrate. A group of naive mice (n = 5) was used as controls. LPS and flagellin induced a progressive increase in plasma nitrate that was more pronounced after LPS. n = 9 to 10 animals/group at each time point. Means ± standard error: †, P < 0.05 versus control; *, P < 0.05 for LPS versus flagellin.
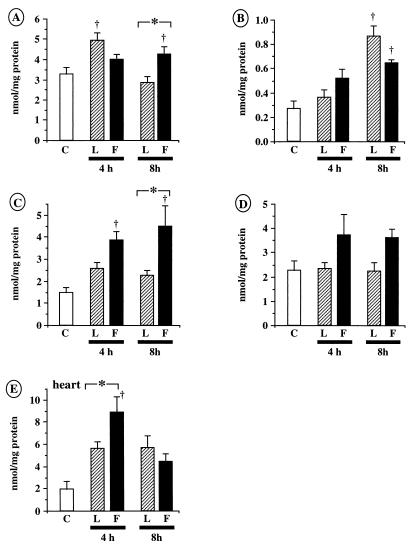
Levels of MDA and reduced glutathione in tissue.
In the lung (Fig. 3A), gut (Fig. 3B), and liver (Fig. 3C), the levels of MDA showed a significant increase following flagellin administration, most notably after 8 h. In the heart (Fig. 3E), flagellin increased the levels of MDA only at 4 h. In the kidney (Fig. 3D), although flagellin increased the formation of MDA, this effect did not reach statistical significance when compared to control animals. In contrast, LPS only increased MDA formation in the lung after 4 h and in the gut after 8 h.
FIG. 3.
Tissue MDA. Conscious mice were challenged with an i.v. injection of 100 μg of S. enterica serovar Enteritidis LPS (L groups) or recombinant S. enterica serovar Muenchen flagellin (F groups). A group of five naïve mice was used as controls (group C). Tissues were harvested after 4 or 8 h to determine the formation of MDA, a marker of lipid peroxidation. (A) Lung. (B) Gut. (C) Liver. (D) Kidney. (E) Heart. LPS transiently increased MDA in the lung and in the gut after 8 h. In contrast, flagellin induced a widespread formation of MDA, significantly more pronounced than after LPS in the lung, liver, and heart. n = 9 to 10 animals/group at each time point. Means ± standard errors: †, P < 0.05 versus control; *, P < 0.05 for LPS versus flagellin
No additive or synergistic effects on lung MDA was observed 4 h after the coadministration of LPS and flagellin, both at 10 μg/mouse (not shown). The levels of MDA were 6.01 ± 0.61 (LPS), 7.25 ± 0.57 (flagellin), and 7.24 ± 0.46 (LPS plus flagellin) nmol/mg of protein.
The levels of reduced glutathione in tissue (Fig. 4) decreased in a comparable way in the lung (Fig. 4A), gut (Fig. 4B), and kidney (Fig. 4D) after flagellin or LPS. In the liver (Fig. 4C), the effect of flagellin was significantly larger after 8 h. Flagellin, but not LPS, also reduced the levels of glutathione in the heart (Fig. 4E).
FIG. 4.
Levels of reduced glutathione (GSH) in tissue. GSH levels were determined as an indicator of antioxidant reserves in organs harvested 4 or 8 h after the i.v. administration of 100 μg of S. enterica serovar Enteritidis LPS (L groups) or recombinant S. enterica serovar Muenchen flagellin (F groups). A group of five naïve mice was used as controls (group C). Both toxins decreased GSH in the lung (A), gut (B), liver (C), and kidney (D). The effect of flagellin was significantly larger in the liver. (E) Flagellin also decreased the levels of GSH in the heart. n = 9 to 10 animals/group at each time point. Means ± standard errors: †, P < 0.05 versus control; *, P < 0.05 for LPS versus flagellin.
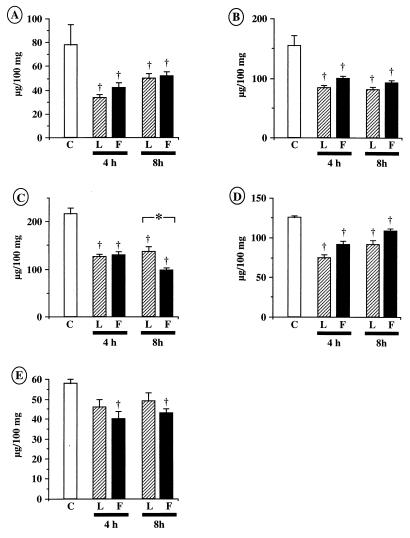
Tissue MPO activity.
Figure 5 illustrates the values of MPO activity in the different organs. In the lung (Fig. 5A), both LPS and flagellin triggered an important recruitment of neutrophils, significantly greater with flagellin at 4 h, while no significant differences were noted at 8 h. In the gut (Fig. 5B), flagellin did not influence MPO activity, whereas LPS induced a significant increase in MPO after 8 h. In the liver (Fig. 5C) and kidney (Fig. 5D), no changes in MPO with respect to the control values were noted, although flagellin tended to be associated with a decrease in liver MPO 8 h after administration. Finally, in the heart (Fig. 5E), a marked decrease in MPO, indicative of a significant reduction in the resident neutrophils in this organ, was noted in mice receiving either LPS or flagellin.
FIG. 5.
Tissue MPO activity. Tissue MPO activity was determined in organs harvested 4 or 8 h after i.v. administration of 100 μg of S. enteritidis LPS (L groups) or recombinant S. muenchen flagellin (F groups). A group of five naïve mice was used as controls (group C). (A) Lung. (B) Gut. (C) Liver. (D) Kidney. (E) Heart. Both LPS and flagellin induced neutrophil accumulation into the lung, an effect that appeared earlier after flagellin. LPS, but not flagellin, also increased MPO in the gut. n = 9 to 10 animals/group at each time point. Means ± standard errors: †, P < 0.05 versus control; *, P < 0.05 for LPS versus flagellin.
MPO was also determined in the lung 4 h after the administration of low doses of LPS or flagellin alone or in combination (not shown). While a significant increase in MPO was measured with both toxins (LPS, 263 ± 38 mU/mg protein), (flagellin, 307 ± 19 mU/mg protein), their coadministration did not increase further MPO (LPS plus flagellin, 268 ± 30 mU/mg of protein; P is not significant versus LPS or flagellin alone).
Levels of aminotransferases and urea in plasma.
The results of the measurements of ALT, AST, and urea, determined 4 h after LPS or flagellin administration, are depicted in Fig. 6. LPS and flagellin induced a significant increase in plasma ALT (Fig. 6A), indicative of liver injury, significantly more pronounced in mice receiving flagellin (controls, 34.8 ± 7.8 IU/liter; LPS, 83.1 ± 10.1; flagellin, 131.2 ± 24.3 IU/liter). Flagellin also induced an increase in AST (Fig. 6B) that was not observed after LPS. Plasma urea showed a significant increase only in mice treated with LPS, whereas flagellin did not affect this parameter (Fig. 6C).
FIG. 6.
Biochemical markers of organ injury. Conscious mice received an i.v. injection of S. enterica serovar Enteritidis LPS (100 μg) or recombinant S. enterica serovar Muenchen flagellin (100 μg). Biochemical markers of liver injury (ALT [A], AST [B]) and renal damage (urea [C]) were determined after 4 h. A group of five naïve mice was used as controls. Flagellin induced significantly more liver injury than LPS, whereas LPS, but not flagellin, induced renal damage.UI, international units. n = 9 to 10 mice/group. Means ± standard errors: †, P < 0.05 versus control; *, P < 0.05 for LPS versus flagellin.
DISCUSSION
Recent studies have indicated that flagellin, a principal component of bacterial flagella, can trigger innate immune responses in mammals by inducing the mobilization of the transcription factor NF-κB and the expression of various proinflammatory genes (6, 7, 10, 19, 20, 29). Two recent reports (12) have demonstrated that these effects are mediated through activation of the Toll-like receptor 5 (12) and IRAK (20) by flagellin. The IL-1 receptor-TLR (IL-1/TLR) family of proteins belong to a group of proteins recently termed “pattern recognition receptors” (14), which mediate innate immune responses following interaction with various pathogen-associated molecular patterns (PAMPs) (34). LPS is another PAMP, which, in contrast to flagellin, binds to the CD14 receptor and then activates TLR4 receptors (5, 23, 25). While the role of LPS as a major proinflammatory component released by gram-negative bacteria is widely established, the flagellin-TLR5 signaling pathway is emerging as a novel concept in the interactions of motile bacteria with eukaryotic organisms. Here, we investigated further the effects of flagellin in vivo, focusing on the systemic release of proinflammatory mediators and the development of inflammatory changes in major organs as well as comparing these effects to those of LPS.
Development of systemic inflammation after flagellin administration.
In agreement with our previous studies (7), we found that flagellin triggered a prototypical systemic inflammatory response, characterized by the production of both proinflammatory (TNF-α, IL-6, and IFN-γ) and anti-inflammatory (IL-10) cytokines (Table 1). While the magnitude of these effects was smaller than that after LPS, an important novel finding was that the release of proinflammatory cytokines was significantly enhanced when both toxins were administered together at low doses (10 μg/mouse) (Fig. 1). Of note, such doses are in the range of the concentrations of free circulating flagellin (0.4 to 2 μg/ml) that can be measured in rats with gram-negative sepsis (7). This synergy, which supports the existence of a cross talk between TLR4 and TLR5 signaling pathways, may represent an important mechanism to amplify proinflammatory signals necessary to fight invading microorganisms. Alternatively, this synergy might favor the development of the overwhelming systemic inflammatory response that characterizes septic shock.
It is now well established that the cardiovascular failure in sepsis is largely related to enhanced NO production following the expression of inducible NO synthase (iNOS) (30). While LPS is a well-recognized inducer of iNOS expression, our data provide evidence that flagellin is able to upregulate NO biosynthesis as well (Fig. 2). This observation, which confirms our earlier findings (7), indicates that flagellin may be, in addition to LPS, an important mediator of circulatory shock in gram-negative sepsis.
Flagellin induces widespread oxidative stress.
Cellular oxidative damage is a well-recognized mechanism of organ injury and dysfunction in gram-negative sepsis (28). In this regard, the diffuse oxidant stress induced by flagellin, evidenced by a sharp increase in MDA formation (Fig. 3), concomitant to a reduction in tissue reduced glutathione (GSH) (Fig. 4), is an important, clinically relevant finding of the present study. It is noteworthy that, in contrast to the larger influence of LPS on the systemic release of cytokines, the pro-oxidant effect of flagellin in tissues was in general significantly greater. This difference suggests that the recognition of LPS and flagellin by distinct TLR receptors elicits alternate immune effector mechanisms. Our data support that activation of the TLR5 receptors by flagellin triggers prototypical host responses, resulting in the generation of a widespread oxidant stress. Interestingly, a recent report showed that interaction of bacterial lipoproteins with TLR2 receptors activates cells to produce a burst of reactive oxygen species (1). Thus, the generation of oxidant species appears to be an important consequence of TLR signaling, which may serve as a primary mechanism of defense against invading pathogens.
Flagellin recruits neutrophils into the lungs.
The acute respiratory distress syndrome (ARDS) is a common complication of sepsis, in part related to the local sequestration and activation of polymorphonuclear neutrophils (4). It is generally acknowledged that LPS is a possible trigger of ARDS in gram-negative sepsis (24, 26, 32). We now identify flagellin as another bacterial toxin leading to the accumulation of neutrophils in the lungs (Fig. 5), an observation consistent with a previous report showing that the intratracheal injection of flagellin provokes a diffuse pneumonitis in mice (8). Of note, we did not find any increase, but rather found a decrease of MPO in response to flagellin in other organs (heart, and, to a lesser extent, liver), whereas LPS also recruited neutrophils in the gut. This suggests specific interactions between flagellin and the pulmonary circulation, resulting in a general mobilization of neutrophils from the periphery towards the lungs. As such, flagellin might represent a previously unrecognized mediator of ARDS in gram-negative sepsis. This hypothesis is currently under investigation in our laboratory.
LPS and flagellin exert contrasting influences on organ damage.
Liver injury and dysfunction are typical features of the multiple organ failure complicating clinical gram-negative septic shock (27). The data presented here support a possible role of flagellin as an initiator of such abnormalities. Indeed, flagellin administration was associated with the occurrence of liver damage, indicated by an increase in plasma aminotransferases (Fig. 6A and B), significantly more pronounced than after LPS. While a possible mechanism underlying this effect was the marked oxidant stress generated by flagellin, additional studies, both morphological and functional, are required to more precisely define the mechanisms of flagellin toxicity on this organ.
Contrasting with their influences on the liver, LPS, but not flagellin, induced renal damage (Fig. 6C). It is worth mentioning here that LPS produces a hypodynamic pattern of shock with redistribution of systemic blood flow (9, 16, 21). The decreased renal perfusion observed under these conditions (2, 31) is responsible for an early increase in plasma urea. Although flagellin also induces arterial hypotension in mice (7), its effects on systemic and regional blood flows are currently unknown. However, the lack of increase of plasma urea in response to flagellin indirectly suggests that it induces a hemodynamic pattern different from that of LPS, an hypothesis that remains to be characterized in detail.
It is noteworthy that the measurements of serum parameters of gross organ damage, while in most cases correlate with the magnitude with the degree of histological damage, do not substitute for the histopathological analysis of tissue injury. Additional studies investigating the specific nature and patterns of the histological tissue damage induced by flagellin versus LPS in the various organs will be required in the future.
Conclusions.
A growing body of evidence indicates that the flagellin subunit of the bacterial flagella represents an important mediator of inflammation released by gram-negative bacteria. The present data further support this emerging concept, by showing that flagellin has powerful pro-oxidant and proinflammatory effects in vivo. Future investigations are required to determine the possible role of flagellin in clinical sepsis. Such information might help to devise novel therapeutic strategies, due to the theoretical possibility of neutralizing the effects of flagellin by specific antibodies.
Acknowledgments
This work was supported, in part, by National Institutes of Health grants RO1GM57407 (A.L.S) and R29GM54773 (C.S). L.L. is supported by a grant from the ADUMED foundation (Switzerland). F.G.S. is supported by a fellowship from FAPESP (Brazil).
Editor: R. N. Moore
REFERENCES
- 1.Aliprantis, A. O., R. B. Yang, M. R. Mark, S. Suggett, B. Devaux, J. D. Radolf, G. R. Klimpel, P. Godowski, and A. Zychlinsky. 1999. Cell activation and apoptosis by bacterial lipoproteins through toll-like receptor-2. Science 285: 736–739. [DOI] [PubMed] [Google Scholar]
- 2.Begany, D. P., J. A. Carcillo, W. A. Herzer, Z. Mi, and E. K. Jackson. 1996. Inhibition of type IV phosphodiesterase by Ro 20-1724 attenuates endotoxin-induced acute renal failure. J. Pharmacol. Exp. Ther. 278: 37–41. [PubMed] [Google Scholar]
- 3.Blair, D. F. 1990. The bacterial flagellar motor. Semin. Cell Biol. 1: 75–85. [PubMed] [Google Scholar]
- 4.Chollet-Martin, S., B. Jourdain, C. Gibert, C. Elbim, J. Chastre, and M. A. Gougerot-Pocidalo. 1996. Interactions between neutrophils and cytokines in blood and alveolar spaces during ARDS. Am. J. Respir. Crit. Care Med. 154: 594–601. [DOI] [PubMed] [Google Scholar]
- 5.Chow, J. C., D. W. Young, D. T. Golenbock, W. J. Christ, and F. Gusovsky. 1999. Toll-like receptor-4 mediates lipopolysaccharide-induced signal transduction. J. Biol. Chem. 274: 10689–10692. [DOI] [PubMed] [Google Scholar]
- 6.Ciacci-Woolwine, F., I. C. Blomfield, S. H. Richardson, and S. B. Mizel. 1998. Salmonella flagellin induces tumor necrosis factor alpha in a human promonocytic cell line. Infect. Immun. 66: 1127–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eaves-Pyles, T., K. Murthy, L. Liaudet, L. Virag, G. Ross, F. G. Soriano, C. Szabo, and A. L. Salzman. 2001. Flagellin, a novel mediator of Salmonella-induced epithelial activation and systemic inflammation: IκBα degradation, induction of nitric oxide synthase, induction of proinflammatory mediators, and cardiovascular dysfunction. J. Immunol. 166: 1248–1260. [DOI] [PubMed] [Google Scholar]
- 8.Feldman, M., R. Bryan, S. Rajan, L. Scheffler, S. Brunnert, H. Tang, and A. Prince. 1998. Role of flagella in pathogenesis of Pseudomonas aeruginosa pulmonary infection. Infect. Immun. 66: 43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fishman, D., L. Liaudet, R. Lazor, C. H. Perret, and F. Feihl. 1997. l-Canavanine, an inhibitor of inducible nitric oxide synthase, improves venous return in endotoxemic rats. Crit. Care Med. 25: 469–475. [DOI] [PubMed] [Google Scholar]
- 10.Gewirtz, A. T., P. O. Simon, C. K. Schmitt, L. J. Taylor, C. H. Hagedorn, A. D. O’Brien, A. S. Neish, and J. L. Madara. 2001. Salmonella typhimurium translocates flagellin across intestinal epithelia, inducing a proinflammatory response. J. Clin. Investig. 107: 99–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Glauser, M. P., D. Heumann, J. D. Baumgartner, and J. Cohen. 1994. Pathogenesis and potential strategies for prevention and treatment of septic shock: an update. Clin. Infect. Dis. 18(Suppl. 2): S205–S216. [DOI] [PubMed] [Google Scholar]
- 12.Hayashi, F., K. D. Smith, A. Ozinsky, T. R. Hawn, E. C. Yi, D. R. Goodlett, J. K. Eng, S. Akira, D. M. Underhill, and A. Aderem. 2001. The innate immune response to bacterial flagellin is mediated by Toll-like receptor 5. Nature 410: 1099–1103. [DOI] [PubMed] [Google Scholar]
- 13.Henderson, B., S. Poole, and M. Wilson. 1996. Bacterial modulins: a novel class of virulence factors which cause host tissue pathology by inducing cytokine synthesis. Microbiol. Rev. 60: 316–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Janeway, C. A., Jr., and R. Medzhitov. 1998. Introduction: the role of innate immunity in the adaptive immune response. Semin. Immunol. 10: 349–350. [DOI] [PubMed] [Google Scholar]
- 15.Komoriya, K., N. Shibano, T. Higano, N. Azuma, S. Yamaguchi, and S. I. Aizawa. 1999. Flagellar proteins and type III-exported virulence factors are the predominant proteins secreted into the culture media of Salmonella typhimurium. Mol. Microbiol. 34: 767–779. [DOI] [PubMed] [Google Scholar]
- 16.Liaudet, L., F. Feihl, A. Rosselet, M. Markert, J. M. Hurni, and C. Perret. 1996. Beneficial effects of L-canavanine, a selective inhibitor of inducible nitric oxide synthase, during rodent endotoxaemia. Clin. Sci. 90: 369–377. [DOI] [PubMed] [Google Scholar]
- 17.Liaudet, L., D. Fishman, M. Markert, C. Perret, and F. Feihl. 1997. l-Canavanine improves organ function and tissue adenosine triphosphate levels in rodent endotoxemia. Am. J. Respir. Crit. Care Med. 155: 1643–1648. [DOI] [PubMed] [Google Scholar]
- 18.Lynn, W. A., and J. Cohen. 1995. Adjunctive therapy for septic shock: a review of experimental approaches. Clin. Infect. Dis 20: 143–158. [DOI] [PubMed] [Google Scholar]
- 19.McDermott, P. F., F. Ciacci-Woolwine, J. A. Snipes, and S. B. Mizel. 2000. High-affinity interaction between gram-negative flagellin and a cell surface polypeptide results in human monocyte activation. Infect. Immun. 68: 5525–5529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moors, M. A., L. Li, and S. B. Mizel. 2001. Activation of interleukin-1 receptor-associated kinase by gram-negative flagellin. Infect. Immun. 69: 4424–4429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mulder, M. F., A. A. van Lambalgen, G. C. van den Bos, and L. G. Thijs. 1996. The fall of cardiac output in endotoxemic rats cannot explain all changes in organ blood flow: a comparison between endotoxin and low venous return shock. Shock 5: 135–140. [DOI] [PubMed] [Google Scholar]
- 22.Namba, K., I. Yamashita, and F. Vonderviszt. 1989. Structure of the core and central channel of bacterial flagella. Nature 342: 648–654. [DOI] [PubMed] [Google Scholar]
- 23.Poltorak, A., X. He, I. Smirnova, M. Y. Liu, C. V. Huffel, X. Du, D. Birdwell, E. Alejos, M. Silva, C. Galanos, M. Freudenberg, P. Ricciardi-Castagnoli, B. Layton, and B. Beutler. 1998. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science 282: 2085–2088. [DOI] [PubMed] [Google Scholar]
- 24.Pompe, J. C., J. Kesecioglu, H. A. Bruining, and C. Ince. 1996. Nebulization of endotoxin during mechanical ventilation: an experimental model of ARDS in pigs. Adv. Exp. Med. Biol. 388: 599–602. [PubMed] [Google Scholar]
- 25.Qureshi, S. T., L. Lariviere, G. Leveque, S. Clermont, K. J. Moore, P. Gros, and D. Malo. 1999. Endotoxin-tolerant mice have mutations in Toll-like receptor 4 (Tlr4). J. Exp. Med. 189: 615–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rabinovici, R., P. J. Bugelski, K. M. Esser, L. M. Hillegass, J. Vernick, and G. Feuerstein. 1993. ARDS-like lung injury produced by endotoxin in platelet-activating factor-primed rats. J. Appl. Physiol. 74: 1791–1802. [DOI] [PubMed] [Google Scholar]
- 27.Ring, A., and W. Stremmel. 2000. The hepatic microvascular responses to sepsis. Semin. Thromb. Hemost. 26: 589–594. [DOI] [PubMed] [Google Scholar]
- 28.Spapen, H., H. Zhang, and J. L. Vincent. 1997. Potential therapeutic value of lazaroids in endotoxemia and other forms of sepsis. Shock 8: 321–327. [DOI] [PubMed] [Google Scholar]
- 29.Steiner, T. S., J. P. Nataro, C. E. Poteet-Smith, J. A. Smith, and R. L. Guerrant. 2000. Enteroaggregative Escherichia coli expresses a novel flagellin that causes IL-8 release from intestinal epithelial cells. J. Clin. Investig. 105: 1769–1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Szabo, C. 1995. Alterations in nitric oxide production in various forms of circulatory shock. New Horizons 3: 2–32. [PubMed] [Google Scholar]
- 31.van Lambalgen, A. A., N. Bouriquet, and D. Casellas. 1996. Effects of endotoxin on tone and pressure-responsiveness of preglomerular juxtamedullary vessels. Pfluegers Arch. 432: 574–577. [DOI] [PubMed] [Google Scholar]
- 32.Wheeldon, E. B., M. E. Walker, D. J. Murphy, and C. R. Turner. 1992. Intratracheal aerosolization of endotoxin in the rat: a model of the adult respiratory distress syndrome (ARDS). Lab. Anim. 26: 29–37. [DOI] [PubMed] [Google Scholar]
- 33.Wray, G. M., C. G. Millar, C. J. Hinds, and C. Thiemermann. 1998. Selective inhibition of the activity of inducible nitric oxide synthase prevents the circulatory failure, but not the organ injury/dysfunction, caused by endotoxin. Shock 9: 329–335. [DOI] [PubMed] [Google Scholar]
- 34.Zhang, G., and S. Ghosh. 2001. Toll-like receptor-mediated NF-kappaB activation: a phylogenetically conserved paradigm in innate immunity. J. Clin. Investig. 107: 13–19. [DOI] [PMC free article] [PubMed] [Google Scholar]