A cleft lip/palate deformity occurs in approximately one in every 700 live births in the USA (1). Jaw growth in the population of patients with unrepaired cleft lip and palate is generally favorable (2–6). No significant difference exists between patients with and those without such deformities in the distribution of vertical or anteroposterior skeletal jaw relationships, except that posterior crossbites (deficiency in the width of the upper jaw, with the upper teeth biting inside the lower teeth) may be more common in patients with a cleft deformity. However, significant disturbances of growth of the jaws, particularly the maxilla (upper jaw), can occur in patients with cleft deformities as a result of surgical repairs of the cleft lip and palate or other factors. The maxilla can become underdeveloped, affecting the alveolus (bone supporting the teeth), dentition (teeth), and associated soft-tissue structures. The following surgical procedures, commonly performed during childhood, can have an unfavorable effect on facial growth:
Cleft lip repair. Commonly performed within the first 3 months of life, this procedure can adversely affect the anterior maxillary alveolar morphology, which is probably related to the discontinuity defect in the alveolar cleft and the extent of soft-tissue undermining and subsequent fibrosis. Other changes in the craniofacial complex are usually minimal (7–12).
Cleft palate repair. These procedures can affect the vertical, anteroposterior, and transverse development of the maxilla and alveolar processes (13–15). Periosteal stripping at the time of surgery and the resulting fibrosis are the most likely reasons for this response.
Alveolar cleft repair. Bone grafting of alveolar cleft defects, when performed in early childhood, can severely inhibit maxillary growth. Several authors have reported early and intermediate repairs using specific techniques that may have fewer unfavorable effects on craniofacial growth (16–20). Bone grafting usually adversely affects vertical and horizontal growth of the maxilla. Ideally, alveolar cleft bone grafting should be delayed as long as possible, until just before the permanent cuspid teeth erupt into the cleft area (age 9 to 12 years), thus allowing more maxillary growth before surgical intervention (21).
Pharyngeal flap. With posterior pharyngeal flaps, a surgical procedure used to correct hypernasal speech problems, a tissue flap from the posterior pharyngeal wall is attached to the soft palate. This flap can have a profound effect on facial growth and development, decreasing the anteroposterior and transverse growth of the maxilla and, in many cases, increasing the vertical component of maxillary growth (22, 23). The increased vertical maxillary growth may be the result of altered breathing patterns, since the pharyngeal flap can result in a mouth-open breathing posture.
Patients with a cleft deformity may have missing permanent teeth, deformed teeth, or even supernumerary teeth in the cleft area. Some patients reach adolescence or adulthood with un-repaired oronasal fistulas (open communications between the mouth and nose) and alveolar clefts (bone discontinuity defects in the bone supporting the teeth), even though the primary cleft defect has been repaired. The severity of residual deformities of the repaired cleft lip and nose may contribute to functional and aesthetic concerns.
As a result of all these factors, moderate to severe deformities of the jaws can develop, affecting not only the basal bone and alveolus, but also the alignment and position of the primary and permanent dentition, as well as the overlying soft tissues. In adolescents and adults who have undergone cleft defect repair, common consequences include anterior and posterior crossbites; midface hypoplasia; anteroposterior, vertical, and transverse maxillary deficiency; residual lip and nasal deformities; and speech problems.
Since orthognathic surgery (corrective jaw surgery) can have a significant untoward effect on facial growth and development in patients with cleft lip and palate, end-stage reconstruction should be considered when these patients have completed most of their facial growth, which is usually age 15 years for females and 17 to 18 years for males. If surgery is done prior to completion of facial growth, the subsequent adverse effect on maxillary growth and continued growth of the mandible will result in recurrence of the facial deformity and malocclusion. It is important to understand that delaying surgery until growth is complete can result in worsening of the facial deformity, creating major functional, aesthetic, and psychosocial problems at an important stage in human psychosocial development. If such problems are severe, surgery can be done at an earlier age with the understanding that it may need to be repeated after growth is complete.
PRESURGICAL ORTHODONTICS
Orthodontic treatment is usually required before surgical correction of jaw deformities. A number of dental considerations must be assessed prior to proceeding with orthodontics, including 1) dental alignment issues, such as crowding, rotations, malposition, and crossbites; 2) approximation of teeth to the alveolar cleft; 3) missing, supernumerary, or malformed teeth; and 4) periodontal disease or defects, oral hygiene, and dental caries. The basic orthodontic principles are to align and level teeth over the basal bones of the maxilla and mandible.
If the lateral incisor tooth is missing (a common occurrence in patients with a cleft), then the posterior bone segment and teeth in unilateral clefts or the bilateral posterior bone segments and teeth in bilateral clefts can be advanced forward to close the space, and the cuspid tooth can be used as a lateral incisor, eliminating the need for a bridge or dental implant. The cuspid is reshaped to look like a lateral incisor to facilitate a better fit of the occlusion at surgery. Another option for managing a missing lateral incisor is to replace it after surgery with a bridge or dental implant.
TREATMENT SEQUENCING IN THE PATIENT UNDERGOING ENDSTAGE CLEFT REPAIR
In adolescents and adults with a cleft defect, it is usually best to correct the underlying dental, maxillary, mandibular, and infraorbital deformities before other functional and cosmetic soft-tissue repairs. This sequencing allows the overlying soft tissues to adjust to the altered underlying dento-osseous structures. For predictable results, external nasal reconstruction and lip revisions are preferably done as a secondary procedure. However, concomitant orthognathic surgery, lip revisions, and major rhinoplasty surgery can be performed in selected patients with unilateral clefts. In patients with bilateral clefts, particularly those with coexisting bilateral alveolar clefts, it is important to stage the lip/ nose and external rhinoplasty procedures separately from the orthognathic procedures so that the vascular supply to the anterior portion of the maxilla (premaxilla) is not jeopardized (24).
Generally, orthognathic surgical sequencing follows a specific order to improve the predictability of the procedures. Some patients will require surgical procedures on both the maxilla and mandible. We perform the mandibular osteotomies with rigid fixation first (25). This is followed by surgery to reposition the maxilla with rigid fixation, including closure of oronasal fistulas, autogenous bone grafting of the alveolar clefts, and synthetic bone grafting to the maxillary osteotomy sites to stabilize the area and facilitate healing. If this new sequencing is followed, rigid-fixation bone plates and screws are mandatory to maximize long-term stability.
MAXILLARY OSTEOTOMY DESIGN AND STABILIZATION
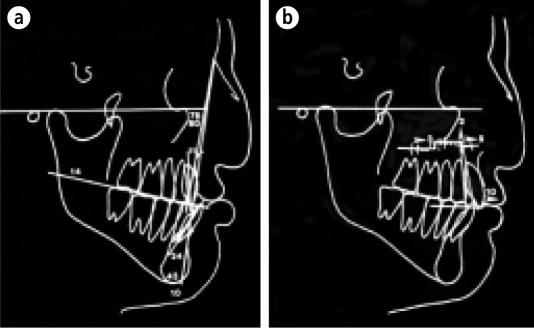
For orthognathic surgical procedures on unilateral or bilateral cleft deformities, we use the maxillary step osteotomy (26) (Figure 1). This design permits more accurate determination of advancement and vertical repositioning of the maxilla. Also, the step area provides an additional area to graft bone.
Figure 1.
(a) Patients with a cleft deformity may present with maxillary hypoplasia and an alveolar cleft (unilateral or bilateral). (b) Maxillary advancement with rigid fixation, closure of oronasal fistulas, and bone grafting to the alveolar cleft can be done in one operation.
Stabilization of maxillary osteotomies is more difficult in the patient with a cleft defect than in the patient without a cleft. Specific steps are incorporated into the procedure to minimize risk of relapse. Adequate mobilization must be achieved with minimal tension on the maxilla when placed in the new position. Four bone plates are used to stabilize the maxilla. Each plate is secured with a minimum of 4 bone screws: 2 above and 2 below the osteotomy line. Bone grafting or placement of synthetic bone grafts is usually necessary to fill osseous defects. We use porous block hydroxyapatite (PBHA) (Interpore 200; Interpore Inc, Irvine, Calif) to provide and maintain vertical, anteroposterior, and transverse stability of the maxilla (27–29). We have previously reported similar good stability in patients with and without clefts undergoing maxillary advancements and/or down-grafting when rigid fixation and PBHA grafts were used (29).
Wolford (25, 30) developed a technique for closure of the oronasal fistulas associated with the alveolar clefts. This technique efficiently utilizes the soft tissues in the cleft area to close the nasal and palatal areas by rotating flaps from within the alveolar clefts. This flap design minimizes the necessity to reflect tissue off the maxilla, enabling concomitant closure of the oronasal fistula(s), bone grafting of the alveolar cleft(s), and performance of the orthognathic procedure during a single surgical operation.
Autogenous cancellous bone is the grafting material of choice in the alveolar cleft, particularly if the teeth are to be orthodontically moved into the cleft or eruption of teeth through the cleft is anticipated (18). PBHA should not be used to graft alveolar clefts because of the significant risk of infection and loss of the graft. This situation should not be confused with the very favorable stability and healing properties of PBHA grafts in the maxillary osteotomy sites, even with the PBHA grafts communicating directly with the maxillary sinus.
TRANSVERSE MAXILLARY EXPANSION
Often the cleft maxilla is narrow and may require surgical expansion. We have previously described 3 soft-tissue techniques that we use to permit surgical expansion of the maxilla while maintaining a viable blood supply to the segments, namely, vomer flaps, split-thickness palatal flaps, and midpalatal incision (24). The split-thickness palatal flap is the technique that we use most often. A palatal soft-tissue incision is made over the lateral aspect of the horizontal palatal bone on one side of the cleft. A split-thickness dissection of the tissues is made, extending to the bony cleft margin. This procedure allows expansion of the maxilla with soft-tissue coverage over the expanded palatal area and helps prevent oronasal fistula development. Careful design and extreme care must be employed so that the split-thickness flap and osseous segments remain viable.
CASE PRESENTATIONS
Case 1
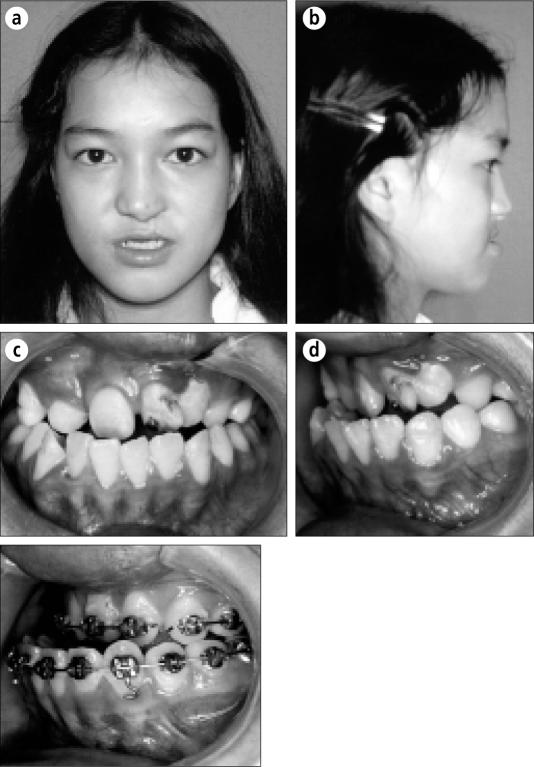
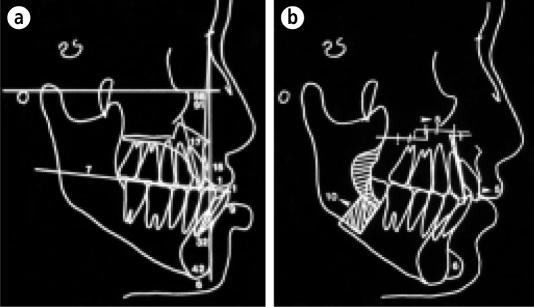
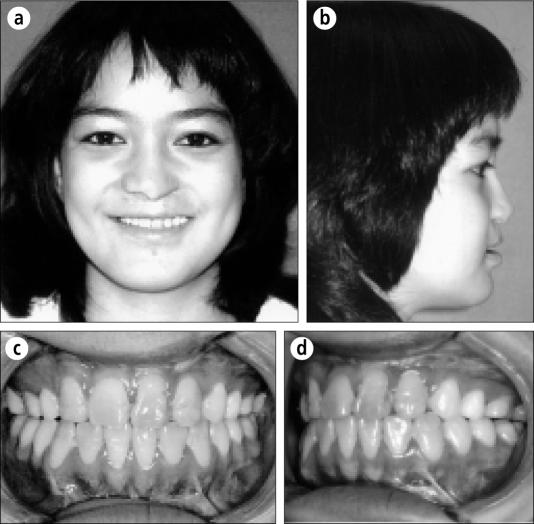
This girl was born with a unilateral left cleft lip and palate and had her primary repairs performed in early childhood with good results but untoward effects on subsequent maxillary growth. Her diagnosis at age 13 years included maxillary hypoplasia (upper jaw underdevelopment), mandibular prognathism (lower jaw overdevelopment), class III occlusion (lower teeth out in front of upper teeth), missing maxillary lateral incisors, left oronasal fistula, and left maxillary alveolar cleft (Figure 2). Presurgical cephalometric analysis was done after presurgical orthodontics were completed, when the patient was aged 15 years, and shows the retruded maxilla and protrusive mandible (Figure 3a). Treatment included 1) orthodontics to align and level the teeth in each jaw; 2) surgery at age 15 years, including maxillary advancement and expansion, mandibular set-back, closure of the oronasal fistula, bone graft to the left maxillary relationship has been established. alveolar cleft, and chin implant (Figure 3b); 3) postsurgical orthodontics to refine the occlusion; and 4) dental restorations. In Figure 4, the patient is pictured 1 year after treatment, demonstrating good facial balance and occlusion.
Figure 2.
(a, b) A 13-year-old girl with a repaired unilateral left cleft lip and palate presents with maxillary hypoplasia and mandibular prognathism. (c, d) She has a class III malocclusion (lower teeth in front of upper teeth): (c) frontal view, (d) left lateral view. (e) Presurgical orthodontics have been completed, aligning the teeth over the basal bone. The magnitude of the bite problem is seen (intraoral left lateral view).
Figure 3.
(a) Cephalometric analysis following completion of the presurgical orthodontics demonstrates the underdeveloped maxilla and overdeveloped mandible. (b) The prediction tracing shows the planned osteotomies, including maxillary advancement, mandibular set-back, and chin augmentation.
Figure 4.
(a, b) The patient is seen 1 year after treatment, demonstrating good facial balance. (c, d) A good functional occlusal relationship has been established.
Case 2
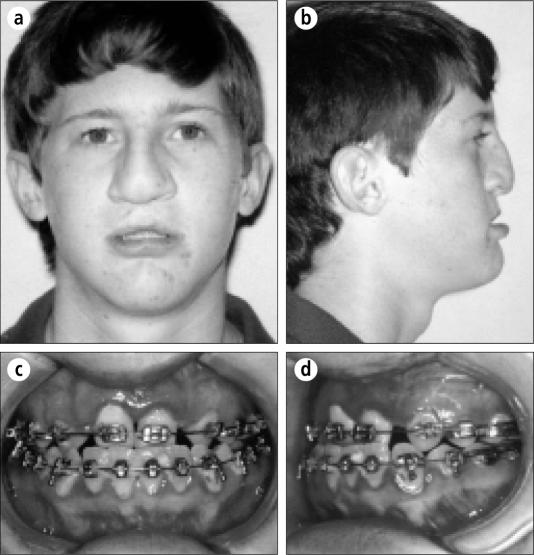
This boy was born with a bilateral cleft lip and palate and had his primary repairs performed in early childhood with resultant deficient growth of the maxilla. His diagnosis at age 16 years included maxillary hypoplasia, class III occlusion, bilateral oronasal fistulas, bilateral alveolar clefts, and missing maxillary lateral incisors (Figures 5, 6a). The treatment included 1) presurgical orthodontics to align and level the teeth in each dental arch; 2) stage 1 surgery at age 17 years, including maxillary osteotomies to advance, expand, and open space for the maxillary lateral incisors, closure of the bilateral oronasal fistulas, and bone grafts to the bilateral alveolar clefts (Figure 6b); 3) postsurgical orthodontics; 4) restorative dentistry to replace the maxillary lateral incisors; and 5) stage 2 surgery, including external rhinoplasty and columella reconstruction with cartilage grafting and revision of the bilateral cleft lip. In Figure 7, the patient is pictured 1 year after completion of treatment.
Figure 5.
(a, b) This 16-year-old boy was born with a bilateral cleft lip and palate. He demonstrates maxillary hypoplasia and a severe nasal deformity. (c, d) He has a class III malocclusion and is missing the maxillary lateral incisors.
Figure 6.
(a) Cephalometric analysis shows the maxillary underdevelopment. (b) The prediction tracing shows the calculated surgical changes of advancing the maxilla.
Figure 7.
(a, b) The patient is seen 1 year after treatment, demonstrating improved facial balance. (c, d) A good functional occlusion has been established, with an anterior bridge to replace the missing maxillary lateral incisors.
CONCLUSION
Cleft deformities of the lip and palate create a challenge for health care professionals who treat these patients. A team approach is required for optimal care. End-stage reconstruction can be very complex, requiring precise surgical techniques to maintain viability of the maxilla and to achieve optimal functional and aesthetic outcomes. Major components in the surgical treatment of these patients include surgery to repair the cleft lip and palate, bone grafting to stabilize the dental arch, orthodontics, orthognathic surgery to correct any skeletal deformities, restorative dentistry, facial reconstruction of lip/nose deformities, and correction of speech problems. When proper care is rendered to patients with deformities associated with clefts of the lip and palate, optimal functional and aesthetic results can be achieved, allowing these individuals to live relatively normal lives.
References
- 1.Gorlin RJ, Cervenka J, Pruzansky S. Facial clefting and its syndromes. In: Bergsma D, editor. The Clinical Delineation of Birth Defects. Part XI, Orofacial Structures. Vol. 7. Baltimore: Williams & Wilkins; 1971. pp. 3–46. [PubMed] [Google Scholar]
- 2.Subtelny JD. Width of the nasopharynx and related anatomic structure in normal and unoperated cleft palate children. Am J Orthod. 1955;41:889–909. [Google Scholar]
- 3.Ortiz-Monasterio F, et al. Cephalometric measurements on adult patients with non-operated cleft palates. Plast Reconstr Surg. 1959;24:53. doi: 10.1097/00006534-195907000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Ortiz-Monasterio F, Serrano A, Barrera G, Rodriguez-Hoffman H, Vinageras E. A study of untreated adult cleft palate patients. Plast Reconstr Surg. 1966;38:36–41. doi: 10.1097/00006534-196607000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Mestre JC, De Jesus J, Subtelny JD. Unoperated oral clefts at maturation. Angle Orthod. 1960;30:78–82. [Google Scholar]
- 6.Atherton JD. Morphology of facial bones in skulls with unoperated unilateral cleft palate. Cleft Palate J. 1967;4:18–30. [PubMed] [Google Scholar]
- 7.Abyholm FE. Primary closure of cleft lip and palate. In: Turvey TA, Vig KWL, Fonseca RJ, editors. Facial Clefts and Craniosynostosis. Philadelphia: WB Saunders; 1996. pp. 370–383. [Google Scholar]
- 8.Bishara SE, Krause CJ, Olin WH, Weston D, Ness JV, Felling C. Facial and dental relationships of individuals with unoperated clefts of the lip and/or palate. Cleft Palate J. 1976;13:238–252. [PubMed] [Google Scholar]
- 9.Normando AD, da Silva Filho OG, Capelozza Filho L. Influence of surgery on maxillary growth in cleft lip and/or palate patients. J Craniomaxillofac Surg. 1992;20:111–118. doi: 10.1016/s1010-5182(05)80092-7. [DOI] [PubMed] [Google Scholar]
- 10.Bardach J, Eisbach KJ. The influence of primary unilateral cleft lip repair on facial growth. Part I. Lip pressure. Cleft Palate J. 1977;14:88–97. [PubMed] [Google Scholar]
- 11.Eisbach KJ, Bardach J, Klausner EC. The influence of primary cleft lip repair on facial growth. Part II. Cleft Palate J. 1978;15:109–117. [Google Scholar]
- 12.Silva Filho OG, Rocha R, Capelozza Filho L. Padra o facial do paciente portador de fissura pré-forame incisivo unilateral completa. Rev Bras Cirurg. 1989;79:197. [Google Scholar]
- 13.Hall DH, Werther JR. Conventional alveolar cleft bone grafting. Oral Maxillofac Surg Clin North Am. 1991;3:609–616. [Google Scholar]
- 14.Dahl E. Craniofacial morphology in congenital clefts of the lip and palate. An x-ray cephalometric study of young adult males. Acta Odontol Scand. 1970;28(Suppl 57):11. [PubMed] [Google Scholar]
- 15.Ross BR. Treatment variables affecting growth in cleft lip and palate. Part 6: Techniques of palate repair. Cleft Palate J. 1987;24:64–70. [PubMed] [Google Scholar]
- 16.Ross BR. Treatment variables affecting facial growth in complete unilateral cleft lip and palate. Part 1: Treatment affecting growth. Cleft Palate J. 1987;24:5–23. [PubMed] [Google Scholar]
- 17.Rosenstein SW, Monroe CW, Kernahan DA, Jacobson BN, Griffith BH, Bauer BS. The case of early bone grafting in cleft lip and cleft palate. Plast Reconstr Surg. 1982;70:297–309. doi: 10.1097/00006534-198209000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Semb G. Effect of alveolar bone grafting on maxillary growth in unilateral cleft lip and palate patients. Cleft Palate J. 1988;25:288–295. [PubMed] [Google Scholar]
- 19.Ross RB. Treatment variables affecting facial growth in complete cleft lip and palate. Part 3: Alveolus repair and bone grafting. Cleft Palate J. 1987;24:33–44. [PubMed] [Google Scholar]
- 20.Nelson CL. Primary alveolar cleft bone grafting. Oral Maxillofac Surg Clin North Am. 1991;3:599–608. [Google Scholar]
- 21.Keller EE. Maxillary discontinuity defects: tissue-integration reconstruction. In: Branemark PI, Tolman DE, editors. Osseointegration in Craniofacial Reconstruction. Carol Stream, Ill: Quintessence; 1998. pp. 187–189. [Google Scholar]
- 22.Ross BR. Facial growth in cleft lip and palate. In: McCarthy JG, editor. Plastic Surgery, vol 4. Cleft Lip and Palate and Craniofacial Anomalies. Philadelphia: WB Saunders; 1990. pp. 2553–2580. [Google Scholar]
- 23.Long RE, Jr, McNamara JA., Jr Facial growth following pharyngeal flap surgery: skeletal assessment on serial lateral cephalometric radiographs. Am J Orthod. 1985;87:187–196. doi: 10.1016/0002-9416(85)90039-9. [DOI] [PubMed] [Google Scholar]
- 24.Wolford LM, Cottrell DA. End-stage reconstruction in the complex lip/ palate patient. In: Turvey TA, Vig KWL, Fonseca RJ, editors. Facial Cleft and Craniosynostosis: Principles and Management. Philadelphia: WB Saunders; 1996. pp. 504–535. [Google Scholar]
- 25.Cottrell DA, Wolford LM. Altered orthognathic surgical sequencing and a modified approach to model surgery. J Oral Maxillofac Surg. 1994;52:1010–1020. doi: 10.1016/0278-2391(94)90164-3. [DOI] [PubMed] [Google Scholar]
- 26.Bennett MA, Wolford LM. The maxillary step osteotomy and Steinmann pin stabilization. J Oral Maxillofac Surg. 1985;43:307–311. doi: 10.1016/0278-2391(85)90297-6. [DOI] [PubMed] [Google Scholar]
- 27.Holmes RE, Wardrop RW, Wolford LM. Hydroxyapatite as a bone graft substitute in orthognathic surgery: histologic and histometric findings. J Oral Maxillofac Surg. 1988;46:661–671. doi: 10.1016/0278-2391(88)90109-7. [DOI] [PubMed] [Google Scholar]
- 28.Moenning JE, Wolford LM. Coralline porous hydroxyapatite as a bone graft substitute in orthognathic surgery: 24-month follow-up results. Int J Adult Orthodon Orthognath Surg. 1989;4:105–117. [PubMed] [Google Scholar]
- 29.Wardrop RW, Wolford LM. Maxillary stability following downgraft and/or advancement procedures with stabilization using rigid fixation and porous block hydroxyapatite implants. J Oral Maxillofac Surg. 1989;47:336–342. doi: 10.1016/0278-2391(89)90333-9. [DOI] [PubMed] [Google Scholar]
- 30.Epker BN, Wolford LM. Dentofacial Deformities: Surgical-orthodontic Correction. St. Louis: Mosby; 1980. pp. 332–368. [Google Scholar]