Abstract
Knee motion has been routinely analyzed using radiographic techniques in a static setting. Over the past decade, techniques of in vivo dynamic knee motion analysis have emerged, which have shed light on normal and pathologic knee motion. Most of these methods are either invasive or restricted to small indoor laboratories. This paper describes a new device that records in vivo dynamic knee motion without the restrictions of current techniques and shows results when this device is used with a patient with an anterior cruciate impairment. We believe that dynamic knee motion studies are critical to a full assessment of the effect of an injury and to subsequent rehabilitation and recovery and that this new device can be a useful diagnostic tool.
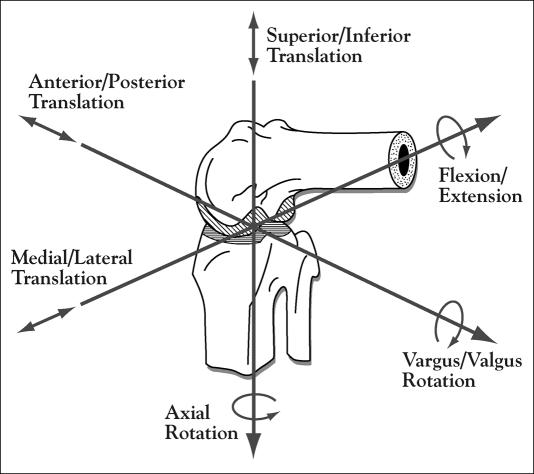
Over the past decade, new techniques of in vivo dynamic knee motion analysis have emerged that have shed new light on normal and pathologic knee motion. Knee joint anatomy and kinematics (i.e., movements) are complex. The knee joint is not a pure hinge joint but moves with a complex set of translations and rotations. It is a bicondylar, modified-hinge joint that exhibits 6 degrees of motion during dynamic activities. These 6 degrees of motion may be characterized as 3 rotations (flexion and extension, external and internal rotation, varus and valgus angulation) and 3 translations (anterior and posterior glide, medial and lateral shift, compression and distraction) (Figure 1).
Figure 1.
Six degrees of freedom of the knee joint, which include 3 rotational and 3 translational motions.
During routine knee flexion, tibiofemoral motion is a combination of sliding and rolling between the contacting tibia and femoral condyle surfaces (1). Motions between the femur and the tibia are constrained by the geometry of the bony structures of the knee joint, the menisci, the muscular attachments via tendons, and the ligaments. Tibiofemoral motion is produced by a combination of the various groups of muscles acting across the knee joint.
The ligaments of the knee joint include the patellar ligament, the medial and lateral collateral ligaments, and the anterior (ACL) and posterior (PCL) cruciate ligaments. The ACL is composed of 2 major bands, the anteromedial band, which is taut in flexion, and the posterolateral band, which becomes tight in extension. The ACL is the key ligament of the knee, controlling forward gliding of the tibia on the femur, lateral mobility in flexion and extension, rotation in flexion and extension, and hyperflexion and hyperextension (2).
Methods for clinical evaluation of knee joint stability comprise manual testing, radiographic studies, electromechanical studies, and arthrometry. Three common manual manipulations used to assess ligament laxity are the classic anterior/posterior drawer test, the Lachman test introduced by Torg et al (3), and the pivot shift test first described by Galway and Macintosh (4). The drawer test is done with the knee at 90° of flexion and the examiner sitting on the patient's foot. The examiner places his hands on the leg so that his thumbs can detect the amount of movement between the tibia and femur. The examiner moves the tibia forward and backward to demonstrate anterior-posterior translation between the tibia and femur. The Lachman test is done in a similar manner but with the knee in only 30° of flexion. The pivot shift test is done while the patient is in a relaxed supine position with the leg extended. The examiner supports the leg by the upper tibia and flexes the knee while applying a slight valgus stress to the knee. A normal knee with no ACL ligament injury or instability flexes and extends smoothly. However, in a knee with ACL impairment, the femur sags backward on the tibia (or conversely, the tibia moves forward on the femur), creating a subluxation of the lateral tibiofemoral compartment. At approximately 30A of flexion, the subluxed tibia suddenly reduces and externally rotates about the femur. The subluxation and the sudden reduction of the knee joint during flexion are termed the “pivot shift.”
Radiographic imaging studies primarily involve stress x-rays or fluoroscopic studies, in which a force is applied to the tibia to produce a subluxation and then an x-ray is taken. Such studies can provide a way of quantifying the amount of laxity. However, the most widely used and clinically accepted knee laxity measurement device is the KT-2000 (formerly the KT-1000) knee ligament arthrometer, which is the current gold standard for arthrometers. The KT-2000 is used to measure only anteroposterior displacement of the tibia with respect to the femur. This device was designed to quantify knee joint laxity, but the results vary among devices and examiners.
Manual manipulation techniques can give the clinician only an idea of the amount of laxity or instability of the knee joint, as the results are subjective and are based on a clinical grading scale that can vary from surgeon to surgeon. Manual testing also requires complete patient relaxation. The greatest disadvantage of both manual testing and arthrometry is that they are static measurements and do not reflect what happens during dynamic activities.
Since the early 1970s, several techniques have been used to evaluate the 3-dimensional kinematics of the knee joint during dynamic activities. In 1972, Kinzel et al described a mathematical formulation for treating and interpreting data from a 6 degree-of-freedom electrogoniometer (5, 6). Based in part on their work, a new type of electrogoniometer was designed and developed under guidance of the senior author (R.W.J.) (1, 7). In 1989, Marans et al used this instrumented spatial linkage device (ISLD) to describe anterior translation of the tibia on the femur during swing phase in a study of patients with ACL impairments.
Lafortune et al studied the relative angular and linear movements between the tibia and femur during walking (8). They implanted intracortical pins directly into the femur and the tibia of volunteers. Each pin had 3 orthogonal markers attached at the ends, which were followed using close-range photogrammetry to provide 3-dimensional reconstruction of the segments. This method eliminated any soft-tissue motion error, but its invasiveness and risk of subsequent infection made this technique inappropriate for clinical use. To avoid this problem, Andriacchi et al described in 1998 a technique called the “point cluster method,” which utilized a series of external reflective markers on the thigh and shank that reduced the nonrigid body-motion artifacts during dynamic motion testing (9). The markers were recorded using high-resolution video cameras, which subsequently yielded 6 degree-of-freedom tibiofemoral motion after some mathematical manipulation. The practical limitation of this system is the overabundance of markers on each segment of the leg, which can lead to difficulties in tracking and labeling the individual markers. Furthermore, these methods are restricted to a small area, usually indoors in a laboratory.
This article describes a new ISLD that can record in vivo dynamic knee motion.
METHODS
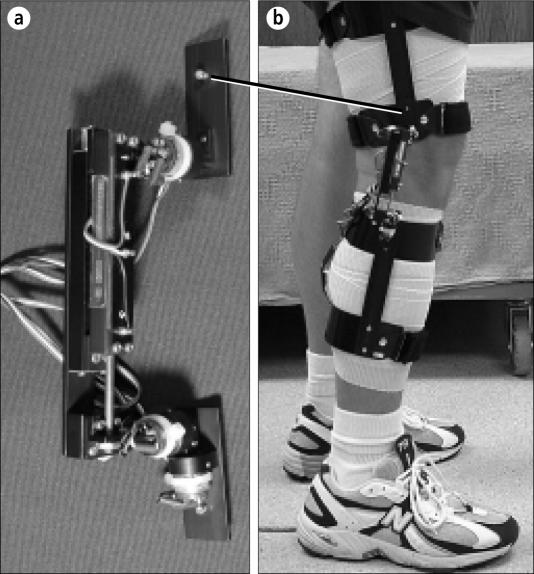
The original ISLD developed by Jackson and colleagues was bulky and heavy and had an unstable and uncomfortable leg attachment system that greatly restricted motion during patient test procedures. The original device also used an 8-channel pen recorder to gather data. Several revisions of the instrument and the recording apparatus followed. In 1998, a miniaturized ISLD with 5 rotary potentiometers and 1 linear potentiometer mounted in an aluminum frame became available (Figure 2a). The ends of the device are flat, with rectangular aluminum plates or “arms” that slide into rails mounted onto leg cuffs made of a flexible aluminum material. The leg cuffs provide a comfortable and stable attachment to the leg (Figure 2b). The thigh and shank cuff attachments allow full range of motion during most dynamic activities.
Figure 2.
The instrumented spatial linkage device. (a) Close-up view. (b) Attached to the leg of a patient.
Using mathematical coordinate transformations, the spatial relationship between the ends of the device (which are attached to, and represent, the femur and tibia) is derived from the output voltages of the 6 potentiometers, which are fed into a computer using an analog-to-digital converter. The data are displayed with rotations measured in degrees and translations measured in millimeters. The ISLD has been tested to be accurate to within ±0.8 mm in translation and ±1.4° in rotation, without taking into account the effects of extraneous soft-tissue motion (10).
As an example, we report on the results of one patient with an ACL impairment on whom both knees were tested with the ISLD during various dynamic activities. We chose this patient because he had an ACL tear confirmed by arthroscopy and he was tested in the acute phase after his ACL injury. The knee motion patterns from his affected side were compared with those of his unaffected side; thus, he was his own control. For the test, the subject was asked to walk at a self-selected speed on a treadmill with a decline of 8°. This downhill test was chosen because it places the ACL-impaired patient in an unstable situation. The results of several steps for each side were normalized to the gait cycle and averaged for graphical purposes.
RESULTS
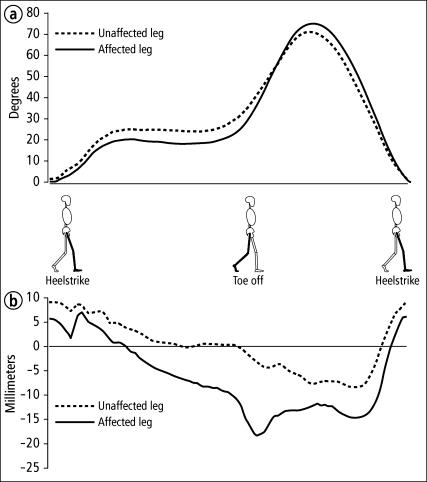
The ACL-impaired patient was a 32-year-old man who injured his left knee in December 2000 while playing basketball. On clinical examination, he had a positive Lachman sign, a positive drawer sign, and a positive pivot shift test result. Magnetic resonance imaging showed evidence of an ACL tear. This patient was tested approximately 4 weeks after the injury. His averaged results from 6 walking cycles are shown in Figure 3.
Figure 3.
Patient tested by the instrumented spatial linkage device during downhill treadmill walking. (a) Average flexion-extension angle. (b) Average anteriorposterior tibial translation.
Figure 3a shows knee flexion and extension during one walking cycle. The graphs show less knee flexion on his affected side during stance phase as well as during swing phase. Figure 3b shows anterior and posterior tibial translation, with respect to the femur, during one walking cycle. During stance phase, there was a larger posterior tibial translation in the affected leg. Hardly any translation was present in the stance phase of the unaffected leg. During swing phase there was an anterior shift in tibial motion in the injured side compared with the uninjured side.
The decreased knee flexion seen in this patient may be indicative of a “quadriceps avoidance”–type gait pattern. This pattern is typical of patients with ACL impairments, as they subconsciously attempt to avoid high knee extension demands, which would place their impaired knee in an unstable situation. This extra posterior shift of the tibia in the affected leg during stance phase could be due to less quadriceps activity and more hamstring activity. It is postulated that excessive hamstring activity becomes a compensation mechanism for the loss of the ACL and therefore minimizes the anterior translation of the tibia. Such patients might be described as “copers,” who have adapted to an unstable situation by muscle re-education. The anterior shift in the tibia during swing phase may be a result of the loss of the protective constraint of the ACL. The activation of the knee extensors during swing phase to advance the leg forward may be causing this anterior shift, which would normally be restrained by the ACL.
CONCLUSION
We believe that dynamic knee motion studies are critical to a full assessment of the effect of an injury and to subsequent rehabilitation and recovery. Patients who seem unstable on clinical examination may be fully stable under weight-bearing dynamic activities. This type of information should help a physician decide whether to surgically repair the instability or treat the condition conservatively.
The case study we presented demonstrated patterns similar to those described by Andriacchi (11): i.e., in ACL-impaired patients, the tibia is slightly anteriorly translated during heel strike and then shifts posteriorly back into place during the stance phase of gait. Most likely, this type of repeated tibiofemoral motion is what leads to early degenerative changes in ACL-impaired knees, and early detection of these subtle abnormalities could prevent secondary conditions. Therefore, we believe that dynamic knee motion studies will become a standard diagnostic tool to better meet patients' immediate and long-term joint care needs.
References
- 1.Townsend MA, Izak M, Jackson RW. Total motion knee goniometry. J Biomech. 1977;10:183–193. doi: 10.1016/0021-9290(77)90057-4. [DOI] [PubMed] [Google Scholar]
- 2.Smillie I. Injuries of the Knee Joint. Edinburgh and London: E&S Livingstone; 1970. [Google Scholar]
- 3.Torg JS, Conrad W, Kalen V. Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med. 1976;4:84–93. doi: 10.1177/036354657600400206. [DOI] [PubMed] [Google Scholar]
- 4.Galway HR, MacIntosh DL. The lateral pivot shift: a symptom and sign of anterior cruciate ligament insufficiency. Clin Orthop. 1980;147:45–50. [PubMed] [Google Scholar]
- 5.Kinzel GL, Hillberry BM, Hall AS, Jr, Van Sickle DC, Harvey WM. Measurement of the total motion between two body segments. II. Description of application. J Biomech. 1972;5:283–293. doi: 10.1016/0021-9290(72)90045-0. [DOI] [PubMed] [Google Scholar]
- 6.Kinzel GL, Hall AS, Jr, Hillberry BM. Measurement of the total motion between two body segments. I. Analytical development. J Biomech. 1972;5:93–105. doi: 10.1016/0021-9290(72)90022-x. [DOI] [PubMed] [Google Scholar]
- 7.Marans HJ, Jackson RW, Glossop ND, Young C. Anterior cruciate ligament insufficiency: a dynamic three-dimensional motion analysis. Am J Sports Med. 1989;17:325–332. doi: 10.1177/036354658901700303. [DOI] [PubMed] [Google Scholar]
- 8.Lafortune MA, Cavanagh PR, Sommer HJ, III, Kalenak A. Three-dimensional kinematics of the human knee during walking. J Biomech. 1992;25:347–357. doi: 10.1016/0021-9290(92)90254-x. [DOI] [PubMed] [Google Scholar]
- 9.Andriacchi TP, Alexander EJ, Toney MK, Dyrby C, Sum J. A point cluster method for in vivo motion analysis: applied to a study of knee kinematics. J Biomech Eng. 1998;120:743–749. doi: 10.1115/1.2834888. [DOI] [PubMed] [Google Scholar]
- 10.Calton E. Mathematical and Software Design and Development of a Six Degree- of-Freedom Knee Measurement Device [master's thesis] Dallas: The University of Texas Southwestern Medical Center; 2000. [Google Scholar]
- 11.Andriacchi TP, Dyrby C, Dillingham M. Paper presented at the 48th Annual Meeting of the Orthopaedic Research Society. Dallas: Tex; February 10–13, 2002. ACL injury causes rotational abnormalities at the knee during walking. [Google Scholar]