Abstract
The efficacy of passive immunization as a postexposure prophylactic measure for treatment of guinea pigs intranasally infected with Bacillus anthracis spores was evaluated. Antisera directed either against the lethal toxin components (PA or LF) or against a toxinogenic strain (Sterne) were used for this evaluation. All antisera exhibited high enzyme-linked immunosorbent assay titers against the corresponding antigens, high titers of neutralization of cytotoxicity activity in an in vitro mouse macrophages cell line (J774A.1), as well as in vivo neutralization of toxicity when administered either directly to Fisher rats prior to challenge with the lethal toxin or after incubation with the lethal toxin. In these tests, anti-LF antiserum exhibited the highest neutralization efficiency, followed by anti-Sterne and anti-PA. The time dependence and antibody dose necessary for conferring postexposure protection by the various antibodies of guinea pigs infected with 25 50% lethal doses of Vollum spores was examined. Rabbit anti-PA serum was found to be the most effective. Intraperitoneal injections of anti-PA serum given 24 h postinfection protected 90% of the infected animals, whereas anti-Sterne and anti-LF were less effective. These results further emphasizes the importance of anti-PA antibodies in conferring protection against B. anthracis infection and demonstrated the ability of such antibodies to be effectively applied as an efficient postexposure treatment against anthrax disease.
Infection with Bacillus anthracis spores via the respiratory route causes a severe disease. Following pulmonary deposition, the spores are phagocytosed by the alveolar macrophages, transferred through the lymphatic channels to the tracheobronchial lymph nodes (after 4 h), where the spores germinate, grow as vegetative cells (18 h) that enter the bloodstream causing a systemic disease (32). The disease is known as wool sorter disease, reported to attack workers with animal hair or its derivatives (3). The severity of inhalation disease was described in detail following an accidental burst of B. anthracis spores over Sverdlovsk in 1979 that caused the death of 64 out of 96 infected people from anthrax. In descending order of frequency, the symptoms reported included fever, dyspnea, cough, headache, vomiting, chills, weakness, abdominal pain, and chest pain (26).
The virulence of the B. anthracis strains is attributed to the anthrax toxin complex and its capsule (11, 27, 35). The exotoxins are composed of three proteins: protective antigen (PA), lethal factor (LF), and edema factor (EF). Toxic activity is expressed only when PA is combined with LF, forming the lethal toxin (LT), or with EF, forming the edema toxin (ET). Lethal toxin causes severe pulmonary edema and death in Fisher 344 rats (1) and in vitro lysis of macrophages and macrophage-like cell lines (6, 8, 13, 14, 21). Consistent with the central role of PA in anthrax toxin action, preexposure vaccination with PA-based vaccines induces protective immunity to anthrax (2, 5, 12, 29, 31, 34).
Treatment of infected animals may be achieved by antibiotic treatment either alone or in combination with active immunization with PA-based vaccines or by passive immunization with anti-PA serum (9, 17, 23, 25; Little et al., Abstr. 94th Annu, Meet. Am. Soc. Microbiol. 1994, abstr. E-64). The disease is readily responsive to early antibiotic treatment by penicillin, doxycycline, and ciprofloxacin (9, 17), but, as has been pointed out, death is due to the activity of the lethal toxin and delayed treatment may sterilize the blood and tissues while not preventing death. In these cases, passive immunization with antitoxin antibodies that neutralize the activity of the lethal toxin may be an effective adjunct or alternative treatment. Passive immunization may also be efficient as preexposure treatment when the prolonged vaccination schedule is not applicable and antibiotic treatment is not efficient, as in the case of infection with antibiotic-resistant strains (4) or in immunocompromised persons.
At the beginning of the previous century, prior to the antibiotic era, people infected with anthrax were treated with antiserum obtained from animals that were immunized with virulent strains (19). Scalvo (1903–1905; cited in reference 36) treated cutaneous anthrax patients, of whom 6% died, compared to 24% who died among the untreated patients. However, the use of antianthrax serum for human treatment was abandoned years ago in most Western countries as being of negligible value.
Passive protection in rabbits was demonstrated with sheep hyperimmune serum produced by immunizing with noncapsulated toxigenic strain following immunization with a virulent strain. Injection of large volumes of serum (5 to 10 ml) 24 h prior to infection with Vollum spores protected 50 to 75% of the infected animals (10). Passive protection in experimental inhalation-infected animals was carried out in monkeys and guinea pigs. Henderson (17) treated infected monkeys with horse anti-Sterne hyperimmune serum using either a single (day 1 postinfection) or two injections (days 1 and 6 postinfection). As a result, 40% to 45% of the animals survived, and the mean time to death (MTTD) of the treated animals was delayed from day 5 to days 20 and 28 (in the one- and two-injection groups, respectively).
The delay in the development of a fatal disease may provide time for active immunization with a PA-based vaccine. Lincoln et al. treated infected monkeys with antibiotic plus hyperimmune anti-Sterne serum (22) and cured about 68% of the infected animals. Successful treatment of septicemic monkeys was achieved by combined treatment with antibiotic plus anti-Sterne serum plus PA vaccine, a treatment that cured 84% of the infected animals (23).
Little and coworkers (25; abstract) treated intramuscularly infected guinea pigs with Ames spores by three injections of antibodies 6 h prior infection and 48 and 96 h postinfection. They tested the efficiency of treatment with different antibodies against the bacterial toxin components and cellular antigens. Only treatment with polyclonal anti-PA serum was successful in saving 50 to 67% of the infected animals. Treatments with rabbit anti-Sterne, guinea pig anti-PA, guinea pig anti-AVA (human anthrax vaccine), or guinea pig anti-Sterne serum or monoclonal antibodies (MAbs) against PA, LF, or EF failed to protect the infected animals.
Here, we report on a study aimed to evaluate the efficacy of several antisera as a postexposure treatment for intranasally infected guinea pigs with a lethal dose of Vollum spores. The hyperimmune sera consist of polyclonal anti-PA, anti-LF, anti-Sterne, and monoclonal anti-PA. We examined the correlation between immunoassay values and protection potency, and the value of these tests as a prediction of the efficacy of antiserum to ensure protection from experimental anthrax.
MATERIALS AND METHODS
Strains.
Vollum (ATCC 14578, a Tox+ Cap+ strain) spores were used for intranasal infection of guinea pigs. ATCC 14185 (a Tox+ Cap− strain) was used for the isolation of the B. anthracis crude lethal toxin, which consists of PA (30 μg/ml) and LF (5 μg/ml), and for the purification of PA and LF proteins (30) for animal immunization and enzyme-linked immunosorbent assays (ELISAs). The veterinary vaccine strain Sterne (a Tox+ Cap− strain) was used for vaccination of rabbits (28, 33).
Media.
Bacterial spores were harvested from sporulation medium G (16). For B. anthracis toxins, the bacteria were grown in RM medium (20), for 22 h, and the supernatant was filter sterilized through a 0.22-μm membrane.
Production of polyclonal anti-PA and anti-LF rabbit sera.
Three New Zealand rabbits (2 kg) were immunized with either purified PA or purified LF by subcutaneous injections. For the first injection, 200 μg of the immunogen was emulsified with complete Freund adjuvant, whereas for the following four boosts given at 2-week intervals, the same amount of immunogen was injected with incomplete Freund adjuvant. Two weeks after the last injection, the rabbits were bled several times at 2-week intervals.
Production of anti-Sterne rabbit serum.
Sterne spores were administered to three rabbits in five intramuscular injections of 5 × 106 spores at 4-week intervals. Starting 2 weeks after the last injection, the rabbits were bled several times at 2-week intervals.
Production of mouse monoclonal anti-PA antibodies.
monoclonal antibodies against PA were produced according the methodology described by Little et al. (24).
ELISA.
For ELISA, purified PA and LF were diluted to 1 μg/ml with 0.05 M carbonate buffer (pH 9.6), and 0.1 ml/well was added to 96-well microtiter plates. The plates were incubated overnight at 4°C, washed with phosphate-buffered saline (PBS)-0.05% Tween 20 (PT), incubated with (0.1 ml/well) PT-2% bovine serum albumin (PBT) for 60 min at 37°C, and washed again with PT. Serial dilutions of the tested sera were added (0.1 ml/well) and the plates were incubated for 60 min at 37°C. The plates were washed with PT and incubated with (0.1 ml/well) alkaline phosphatase-conjugated rabbit anti-GP antibodies (Sigma) for 30 min at 37°C. The plates were washed with PT and incubated with (0.1 ml/well) alkaline phosphatase substrate (according to Sigma instructions) for 60 min at 37°C. Plates were read on a MicroElisa reader at a wavelength of 405 nm. Readings higher than 3-fold the negative controls were scored as positive reactions.
Determination of the cytotoxicity inhibitory titer.
In vitro neutralization of cytotoxicity activity of the B. anthracis lethal toxin (LT) was measured according to the previously described assay (18), with small modifications. LT in 0.1 μg of PA plus 0.016 μg of LF was preincubated with serial dilutions of the tested sera for 1 h at 37°C. The neutralized LT was added to monolayers of the mouse macrophage cell line J774A.1 that were further incubated for 3 h at 37°C. Cell viability was estimated by the 3-(4,5-dimethylthiazole-2-yl)-2,5-diphenylmethyltetrazolium bromide (MTT) method (15). The cytotoxicity inhibitory titer was defined as the reciprocal of the highest dilution of a given serum that prevented the cytotoxic effect of the lethal toxin.
Prevention of the lethal toxin effect on rats.
The effect of the lethal toxin was assayed in male Fisher 344 rats (200 to 250 g) by intravenously injecting 1-ml dilutions of crude toxin. Diluted crude toxin (1 ml containing 6 μg of PA and 1 μg of LF) caused the death of the rats by 100 min and was used as the test dose.
This assay was used to estimate the in vitro neutralization and the in vivo inhibition of the lethal effect by the different antisera. For the in vitro-in vivo assay, serial dilutions of the tested antiserum (1 ml) were incubated with the LT test dose for 1 h at 37°C, and the resulting mixtures were injected intravenously into the rats’ tail vein. The neutralizing titer was defined as the reciprocal of the highest dilution of the antiserum that neutralized the lethal effect of the toxin. The in vivo protection assay was performed by intraperitoneal injection of various amounts of the tested antisera, 24 h prior to intravenous challenge of the rats with the LT test dose. The protective titer was defined as the reciprocal of the minimal volume of injected antiserum that prevented the lethal effect of the B. anthracis lethal toxin.
Efficacy of protection by passive immunization.
Female Hartley guinea pigs (250 to 300 g) were intranasally infected by unilateral instillation (50 μl) with approximately 106 Vollum spores (25 50% lethal doses [LD50]). Groups of 8 to 10 animals were injected intraperitoneally with immune serum given at different times pre- and postinfection. The animals were observed for at least 30 days for survivors.
To monitor the acquired immunity of the surviving animals against establishment of the anthrax disease, the animals were tested for antibodies to PA and resistance to rechallenge by intramuscular injection of 103 (20 LD50) Vollum spores.
Clearance of heterologous antibodies from the circulation of guinea pigs.
The clearance of rabbit polyclonal antiserum and mouse monoclonal antibody from the circulation of guinea pigs was determined by intraperitoneal injection of 1 ml of the relevant anti-PA antibodies to three naive animals. Blood samples were drawn at different times postinjection, and the anti-PA activity was determined by ELISA.
RESULTS
Characterization of the tested sera.
The sera used in the passive protection assays were characterized by their reactivity and titers in ELISAs against purified PA and LF, inhibition of cytotoxicity of the LT on a macrophage cell line, and in vivo neutralization of the lethal effect of LT (containing 6 μg of PA and 1 μg of LF). The results are summarized in Table 1. All sera exhibited high binding titers in ELISA to the corresponding antigen, but varied in their ability to inhibit the cytotoxic activity of the lethal toxin on the macrophage cell line.
TABLE 1.
ELISA titers, neutralization of cytotoxicity, and lethality titers of anti-PA, anti-LF, and anti-Sterne antibodies
| Antiserum tested | ELISA titer against:
|
Inhibition titer of LT cytotoxicitya | Neutralization titer of LT in rat lethality assayb | Amount of antiserum required to protect rats against LT activityc (ml) | |
|---|---|---|---|---|---|
| PA | LF | ||||
| Rabbit anti-PA | 2 × 106 | 0 | 1.6 × 103 | 3 × 101 | 1 |
| Rabbit anti-LF | 0 | 5 × 105 | 1 × 104 | 4 × 102 | 0.1 |
| Rabbit anti-Sterne | 2 × 105 | 1 × 105 | 3 × 103 | 6 × 101 | 0.25 |
| Anti PA MAb 35 | 2 × 106 | 0 | 0 | 0 | ND |
| Anti PA MAb 36 | 8 × 105 | 0 | 8 × 101 | 1 × 101 | 10 |
| Normal rabbit serum | 0 | 0 | 0 | 0 | >10 |
The cytotoxicity inhibitory titer is defined as the reciprocal of the highest dilution of a given serum that prevented the cytotoxic effect of the lethal toxin in J774.A mouse macrophages.
The neutralization titer is defined as the reciprocal of the highest dilution of the antiserum that neutralized in vitro the lethal toxin (6 μg of PA and 1 μg of LF) and prevented the death of rats following injection of the toxin-antiserum mixture.
Protection is defined as the minimal amount of antiserum that was injected 24 h prior to challenge with LT that prevented the death of rats. ND, not determined.
The anti-LF serum was the most efficient inhibitor (titer of 104), followed by anti-Sterne, anti-PA, and monoclonal antibody anti-PA. The anti-PA monoclonal antibodies, although exhibiting high binding activity to PA (8 × 105 and 2 × 106), showed minimal (titer of 8 × 101 and less) neutralization of the LT cytotoxicity. These results demonstrate the lack of correlation between the binding activity of the antibodies, as assayed by ELISA, and their neutralizing activity, as measured by the cytotoxicity inhibition assay. The rabbit anti-PA serum demonstrated high anti-PA titer (2 × 106) and high neutralization of cytotoxicity titer (1.6 × 103). The anti-Sterne antibodies contained antibodies against PA and LF (2 × 105 and 1 × 105, respectively), and neutralization of cytotoxicity neutralization antibodies (titer of 3 × 103).
Further characterization of the antisera was carried out by use of two assay variants of inhibition of LT toxicity in rats. The neutralization of toxicity of the tested antisera was estimated by in vitro incubation of the sera with crude anthrax toxin following intravenous injection of the LT-antiserum mixture to rats. In a second assay, simulating passive immunization, the tested sera were injected intramuscularly to rats, 24 h prior to intravenous challenge with a lethal dose of LT.
The results obtained in both assays demonstrate the ability of the sera to neutralize the toxicity of the LT in rats. A correlation between cytotoxicity inhibitory titer, in vitro neutralization titer, and in vivo protection could be demonstrated.
In all these assays, the rabbit anti-LF serum was the most effective: toxin neutralization titer of 400 and 0.1 ml of the antiserum protected the animals from LT lethality. The second effective antiserum was anti-Sterne, which contained toxin neutralization titer of 60, and the animals were protected following injection of 0.25 ml of antiserum. The rabbit anti-PA antiserum was the third effective antibody, containing toxin neutralization titer of 30, and the animals were protected following injection of 1 ml of the antibodies. Monoclonal antibody anti-PA 36 had a low toxin neutralization titer of 10, and up to 10 ml of the antibodies was needed to protect the animals against lethal toxin activity. Monoclonal antibody anti-PA 35 did not show any neutralizing activity and was therefore not used in the following experiments.
Clearance rate of heterologous antibodies from guinea pig serum.
In order to evaluate the clearance rate of the rabbit and mice antibodies in the guinea pig serum following passive immunization, rabbit anti-PA serum and mouse monoclonal antibody anti-PA 36 were injected into naive guinea pigs. The titer of anti-PA in the animals’ serum was tested at different days postinjection. The results for rabbit anti-PA indicated that the antibodies remain in the guinea pig serum for a significant time (t1/2 ≅ 9 to 10 days), while the monoclonal antibody anti-PA showed high clearance rate from the guinea pig serum (t1/2 ≅ 3 to 4 days) (data not presented). These results indicated that a single antibody injection might be sufficient for the passive immunization using polyclonal antibodies, whereas multiple injections are needed for treatment with monoclonal antibodies.
Passive protection of infected guinea pigs with rabbit anti-PA serum.
To evaluate the efficacy of passive protection against B. anthracis infection, the following parameters were tested: type of antiserum, serum concentration, and treatment interval from time of infection. The following antisera were evaluated: rabbit anti-PA, anti-LF, a mixture of anti-PA plus anti-LF, and anti-Sterne (which contained antibodies against PA, LF, EF, and cellular antigens). Passive protection assays were performed following intranasal infection of guinea pigs with 25 LD50 of Vollum spores.
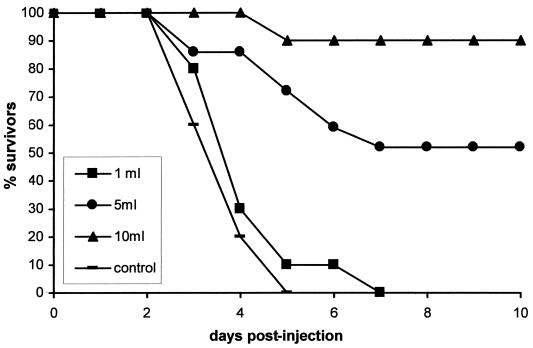
A correlation between antibody concentration and survival is described in the experiment that is presented in Fig. 1. In this experiment guinea pigs were infected with 25 LD50 of Vollum spores, and at 24 h postinfection the animals were injected intraperitoneally with 10, 5, and 1 ml of rabbit anti-PA serum. At 10 ml and 5 ml and antibodies protected 90% and 50% of animals, respectively, while 1 ml did not protect. These results indicated that the protection exhibited by the rabbit anti-PA serum was dose dependent.
FIG. 1.
Dose dependence of protection against B. anthracis in intranasally infected guinea pigs by rabbit anti-PA serum. The protective effect of anti-PA serum was assayed as described in Materials and Methods.
The effective doses of 5 and 10 ml were used to determine the time postinfection for the start of an effective treatment (Table 2). The results showed that there is no difference in the percentage of survival between the groups that received the 5-ml antiserum either 24 h prior to or after infection (50% and 42.8% survival, respectively). In both groups the difference in terms of survival rate compared to treatment with normal rabbit serum is significant (P < 0.05). However, delaying the injection of the antibodies to 36 or 48 h postinfection diminished the protective effect (12.5% survival in the 36-h treated group, and 11% and 25% survival in the groups receiving 5 and 10 ml of antiserum 48 h postinfection, respectively).
TABLE 2.
Time and dose dependence of protection of intranasally infected guinea pigs treated with rabbit anti-PA antibodies
| Serum injected | Amount injected (ml) | Time of injection (h relative to infection) | No. dead/no. infected | No. dead (day) | MTTD (days) | % Survivorsa |
|---|---|---|---|---|---|---|
| Rabbit anti-PA | 10 | +24 | 2/18b | 1 (5), 1 (10) | 7.5 | 88.8* |
| +36 | 7/8 | 1 (2), 4 (3), 2 (5) | 3.4 | 12.5 | ||
| +48 | 6/8 | 1 (2), 4 (3), 1 (4) | 3.0 | 25 | ||
| 5 | −24 | 5/10 | 2 (6), 1 (8), 1 (18), 1 (24) | 12.4 | 50* | |
| +24 | 12/21b | 3 (3), 2 (5), 2 (6), 1 (7), 3 (11), 1 (13) | 7 | 42.8* | ||
| +48 | 8/9 | 7 (3), 1 (7) | 3.5 | 11 | ||
| Normal rabbit serum | 10 | +24 | 8/8 | 3 (3), 3 (5), 1 (11), 1 (15) | 6.2 | 0 |
| 5 | +24 | 7/7 | 5 (4), 1 (6), 1 (8) | 4.8 | 0 |
*, difference from normal rabbit serum-treated groups is significant (P < 0.05).
Cumulative results from two experiments.
Comparison of the MTTD between the groups that were injected with antiserum before or after the infection indicated that in the preexposure-treated group the MTTD was delayed (day 12) in relation to the postinfection-treated group (day 7).
Acquired immunity to B. anthracis in the surviving animals treated with rabbit anti-PA serum.
The animals that were treated with rabbit anti-PA serum were observed for 35 days for survivors, after which the animals were tested for acquired immunity against anthrax by following the development antibodies to PA and by testing their resistance to rechallenge with Vollum spores. The presence of anti-PA antibodies was determined by ELISA tests, and the results indicated that all the animals developed anti-PA antibodies with titers of 400 to 12,800, with a geometric mean titer (GMT) of 1,449. Rechallenge of the animals showed that almost all (85 to 100%) of the surviving guinea pigs were resistant to fatal infection (Table 3).
TABLE 3.
Acquired immunity against B. anthracis infection by survivors among intranasally infected guinea pigs treated with rabbit anti-PA antibodies, as determined by resistance to intramuscular rechallenge
| Serum injected | Amount injected (ml) | Time of injection (h) | No. of survivors tested | Resistance to rechallengea
|
||
|---|---|---|---|---|---|---|
| No. dead (day) | MTTD (days) | % Survivors | ||||
| Rabbit anti-PA | 10 | +24 | 16 | 1 (11), 1 (15) | 13 | 87.5 |
| 5 | +24 | 7 | 1 (4) | 4 | 85.6 | |
| 5 | −24 | 5 | 100.0 | |||
| Control | 1 (2), 3 (3), 1 (4) | 3 ± 0.7 | 0.0 | |||
Intramuscular injection of 2 × 103 (40 LD50) Vollum spores.
Passive protection of infected guinea pigs with monoclonal anti-PA antibodies.
Infected guinea pigs were injected on days 1 and 2 postinfection with 10 ml of anti-PA monoclonal antibody 36. The treatment failed to exhibit any protective activity, and the animals died with a MTTD of 4.4 days, similar to the control animals which were injected with normal mouse serum. Clearance of the monoclonal antibody from the circulation is rapid (undetectable levels by day 10), yet this finding cannot explain the total lack of protective activity, and the finding that monoclonal antibody did not cause any delay in the onset of the disease and death. We must assume that the low affinity of the monoclonal antibody to PA (as shown in the various neutralization assays) is the main reason for its failure to protect infected guinea pigs.
Passive protection of infected guinea pigs with rabbit anti-LF serum.
Rabbit anti-LF serum was shown to be highly efficient in neutralization of the cytotoxic and lethal effect of the B. anthracis LT, as described in Table 1. Passive protection experiments of intranasally infected guinea pigs, described in Table 4, show that the antibodies had a minor protective effect; 5 ml of the anti-LF serum, injected 24 h postinfection, protected only 25% of the infected animals (not a significant difference from control groups in relation to survivors). However, comparison of the MTTD of the treated guinea pigs with that of the control animals indicated a delay in time to death (MTTD of 10.3 and 3.1, respectively). Coadministration of anti-LF and anti-PA sera showed a statistically significant increase in protection of the infected animals. These results indicated the possibility of an additive effect; however, larger groups of experimental animals are required to substantiate this conclusion.
TABLE 4.
Efficacy of passive protection against B. anthracis in intranasally infected guinea pigs treated with rabbit anti-LF antibodies
| Serum tested | Amount of antibodies (ml) | No. dead/no. infected | No. dead (day) | MTTD (days) | % Survivorsa |
|---|---|---|---|---|---|
| Rabbit anti-LF | 5 | 6/8 | 1 (4), 2 (6), 1 (7), 1 (8), 1 (31) | 10.3 | 25 |
| 2 | 8/8 | 2 (3), 3 (4), 1 (6), 2 (7) | 4.8 | 0 | |
| Rabbit anti-LF + rabbit anti-PA | 2 + 2 | 5/8 | 1 (2), 1 (4), 1 (6), 1 (13), 1 (16) | 8.2 | 37.5* |
| Rabbit anti-PA | 2 | 7/8 | 2 (4), 1 (7), 1 (10), 1 (14), 1 (15), 1 (17) | 10.1 | 12.5 |
| Normal rabbit serum | 5 | 8/8 | 2 (2), 4 (3), 1 (4), 1 (5) | 3.1 | 0 |
*, difference from normal rabbit serum-treated group is significant (P < 0.05).
Passive protection of infected guinea pigs with rabbit anti-Sterne serum.
Immunization of animals with the toxinogenic nonencapsulated Sterne spores is known to elicit the production of antibodies to the three components of the B. anthracis toxin, PA, LF, and EF, and to several vegetative antigens (17). Treatment of infected animals with rabbit anti-Sterne serum showed (Table 5) that 10 ml, 5 ml, and 2 ml of serum resulted in survival of 44.4%, 37.5%, and 30% of the infected animals, respectively, which is statistically significant (P < 0.05). The protective efficacy with anti-Sterne antibodies is less effective than with rabbit anti-PA serum. However, it may be of interest that the slope of the dose dependency with rabbit anti-Sterne antibodies seems to be shallow, showing protection of 30% of the infected guinea pigs with 2 ml of the antiserum, compared to 12.5% with 2 ml of anti-PA serum.
TABLE 5.
Efficacy of passive protection against B. anthracis in intranasally infected guinea pigs treated with rabbit anti-Sterne antibodies
| Serum injected | Amount Binjected (ml) | No. dead/no. infected | No. dead (day) | MTTD (days) | % Survivorsa |
|---|---|---|---|---|---|
| Rabbit anti-Sterne | 10 | 10/18 | 1 (3), 3 (4), 1 (5), 1 (6), 1 (7), 1 (8), 1 (9), 1 (14) | 6.4 | 44.4* |
| 5 | 10/16 | 1 (2), 2 (3), 4 (4), 1 (5), 1 (10), 1 (15) | 5.4 | 37.5* | |
| 2 | 7/10 | 1 (2), 1 (3), 1 (5), 2 (6), 1 (7), 1 (10) | 5.5 | 30.0* | |
| Normal rabbit serum | 10 | 8/8 | 1 (2), 3 (3), 2 (4), 1 (5), 1 (6) | 3.9 | 0.0 |
*, Differences from normal rabbit serum-treated group are significant (P < 0.05).
Acquired immunity to B. anthracis in challenge-surviving animals treated with rabbit anti-Sterne serum.
The infected animals that survived due to passive protection with rabbit anti-Sterne serum developed antibodies to PA with titers of 400 to 6,400, with a GMT of 2,400. At 35 days postinfection the surviving animals from treatment with 10 ml of serum were rechallenged with 40 LD50 of Vollum spores injected intramuscularly, and all the animals survived (data not shown).
DISCUSSION
This study was aimed to evaluate the efficacy of passive immunization as a postexposure prophylactic measure against anthrax. Such a treatment might be of value in bacteremic patients, for whom treatment with antibiotics might cause an enhanced release of the bacterial lethal (LT) and edema (ET) toxins, causing death.
Passive protection assays were performed with guinea pigs infected by intranasal administration of 25 LD50 of Vollum spores. Such infection results in a pulmonary anthrax disease in which bacteria can be detected in the blood approximately 30 h postinfection (data not shown), causing death with a MTTD of 3 to 5 days. We analyzed the efficiency of various antianthrax antibody preparations to prevent the development of a fatal infection. The antibodies that were tested were directed either against the LT components PA and LF or the bacterial toxins LT and ET, as well as vegetative antigens, obtained by immunization with the Sterne strain (7, 34).
We tested the time dependence of efficiency of protection conferred by postinfection antiserum administration as well as the development of protective immunity postchallenge, as evaluated by anti-PA antibody titer and resistance to a 40 LD50 spore challenge. Development of protective immunity is an important issue, as such a response might confer resistance to growth of residual spores present in the lungs. Presence of residual spores was demonstrated in monkeys exposed to inhalation anthrax and treated with antibiotics, where it was shown that even after more than 42 days postinfection, 15% to 20% of the initial infective spore dose was still present in the lungs (17).
In this study, the protective efficacy of the following antisera was tested: rabbit anti-PA, anti-LF, and anti-Sterne and mouse monoclonal anti-PA. Since the major cause of mortality is attributed to the LT, the initial antiserum screening test was based on their ability to inhibit the cytotoxic and lethal effect of B. anthracis LT. Inhibition of cytotoxicity and rat lethality assays indicated that rabbit anti-LF antibodies were the most potent in preventing cytotoxicity and lethality (Table 1). Antibody titer of 104 inhibited cytotoxicity; serum dilution of 4 × 102 neutralized the lethal toxin activity, and injection of 0.1 ml of antibodies 24 h prior to intravenous challenge of the lethal toxin prevented lethality for rats.
The rabbit anti-Sterne and anti-PA antibodies were 4-fold and 10-fold less potent, respectively. However, when tested for their capacity to protect against intranasal Vollum spore infection, the polyclonal anti-PA antibodies were shown to be the most efficient, providing significant protection, resulting in approximately 90% survival. Polyclonal anti-Sterne and anti-LF were less effective, resulting in 40% and 25% survival, respectively (Tables 3, 4 and 5).
Similar results were described by Little et al. (25), who tested the efficiency of guinea pig polyclonal anti-PA, anti-AVA, and anti-Sterne and mouse monoclonal anti-PA, anti-LF, and anti-EF antibodies for passive protection against intramuscular infection with 40 LD50 of Ames strain spores. Antisera were administered 6 h prior to and 48 and 96 h after spore challenge. While anti-PA and anti-AVA exhibited some protective activity, anti-Sterne was not protective (8% survival), and none of the monoclonal antibodies were protective.
Recently published results (30) provide additional proof of the protective potential of guinea pig anti-PA antibodies. In passive transfer experiments, a correlation between cytotoxicity neutralization titers and protection against intradermal administration of 20 LD50 of Vollum spores was found. Neutralizing antibody titer above 220 confers full protection, and 50% protection was achieved at a titer of 80 (± 40).
Although the anti-PA serum was shown to provide significant protection against intranasal infection, several findings can impair or limit the possible use of passive immunization treatment. Large quantities of hyperimmune serum are required to obtain effective protection. Purified high-affinity neutralizing antibodies can be a more adequate and efficient reagent for this purpose. Another drawback may be the dependence of the efficacy of the antitoxin serum treatment on the time of administration. In the situation described here, starting the treatment 36 h and 48 h postinfection gave limited protection. However, it should be stressed that the time to death in this type of infection is about 3 to 5 days, and it may be that the efficacy of the treatment is a function of the interval between serum administration and the onset of symptoms.
Although anti-LF antiserum was less effective than anti-PA in conferring protection against spore infection, the observation that anti-LF was shown to be 10-fold more potent as an inhibitor of LT activity both in vitro and in vivo may serve as an indication of its putative protective potential. This could be studied through enhancing anti-LF antibody concentration and/or affinity, synergism or additivity with anti-PA, etc.
Most of the surviving guinea pigs developed an active immune response, becoming resistant to future challenge with B. anthracis spores. This finding implies that the passive immunization allowed a certain degree of growth of the B. anthracis bacteria and did not interfere with the development of an active immune response.
The results presented herein demonstrate that passive immunization with anti-PA serum can provide protection against anthrax infection in guinea pigs. Additional experiments and development of more potent monoclonal antibodies are required to further evaluate the potential efficacy of such treatment for human use.
Acknowledgments
We thank Gideon Halperin for performing statistical analysis and Nili Rothschild, Pinchas Parnes, Joseph Shlomovich, Yoel Papir, Lea Silberman, and Shlomo Habusha for excellent technical assistance.
Editor: R. N. Moore
REFERENCES
- 1.Beall, F. A., M. J. Taylor, and C. B. Thorne. 1962. Rapid lethal effect in rats of a third component found upon fractionating the toxin of Bacillus anthracis. J. Bacteriol. 83:1274–1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Belton, F. C., and R. E. Strange. 1954. Studies on a protective antigen produced in vitro from Bacillus anthracis: medium and methods of production. 1954. Br. J. Exp. Pathol. 35:144–152. [PMC free article] [PubMed] [Google Scholar]
- 3.Brachman, P. S., S. A. Plotkin, F. H. Bumford, and M. M. Atchison. 1960. An epidemic of inhalation anthrax: the first in the twentieth century. Am. J. Hyg. 72:6–23. [DOI] [PubMed] [Google Scholar]
- 4.Bradaric, N., and V. Punda-Polic. 1992. Cutaneous anthrax due to penicillin–resistant Bacillus anthracis transferred by an insect bite. Lancet 340:306–307. [DOI] [PubMed] [Google Scholar]
- 5.Cohen, S., I. Mendelson, Z. Altboum, D. Kobiler, E. Elhanany, T. Bino, M. Leitner, I. Inbar, H. Rosenberg, Y. Gozes, R. Barak, M. Fisher, C. Korman, B. Valan, and A. Shafferman. 2000. Attenuated nontoxinogenic and nonencapsulated recombinant Bacillus anthracis spore vaccines protect against anthrax. Infect. Immun. 68:4549–4558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ezzell, J. W., B. E. Ivins, and S. H. Leppla. 1984. Immunoelectrophoretic analysis, toxicity, and kinetics of in vitro production of the protective antigen and lethal factor components of Bacillus anthracis toxin. Infect. Immun. 45:761–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ezzell, J. W., and T. G. Abshire. 1988. Immunological ananlysis of cell-associated antigens of Bacillus anthracis. Infect. Immun. 56:349–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Friedlander, A. M. 1986. Macrophages are sensitive to anthrax lethal toxin through an acid-dependent process. J. Biol. Chem. 261:7123–7126. [PubMed] [Google Scholar]
- 9.Friedlander, A. M., S. L. Welkos, M. L. M. Pitt, J. W. Ezzell, P. L. Worsham, K. J. Rose, B. E. Ivins, J. R. Lowe, G. B. How, P. Mikesell, and W. B. Lawrence. 1993. Postexposure prophylaxis against experimental inhalation anthrax. J. Infect. Dis. 167:1239–1242. [DOI] [PubMed] [Google Scholar]
- 10.Gladston, G. P. 1946. Immunity to anthrax: protective antigen present in cell-free culture filtrates. Br. J. Exp. Pathol. 27:394–418. [PMC free article] [PubMed] [Google Scholar]
- 11.Green, B. D., L. Battisti, T. M. Koehler, C. B. Thorne, and B. E. Ivins. 1985. Demonstration of a capsule plasmid in Bacillus anthracis. Infect. Immun. 49:291–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hambleton, P., and P. C. B. Turnbull. 1990. Anthrax vaccine development: a continuing story. Adv. Biotechnol. Processes 13:105–122. [PubMed] [Google Scholar]
- 13.Hanna, P. C., D. Acosta, and R. J. Collier. 1993. On the role of macrophages in anthrax. Proc. Natl. Acad. Sci. USA 90:10198–10201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hanna, P. C., S. Kouchi, and R. J. Collier. 1992. Biochemical and physiological changes induced by anthrax lethal toxin in J774 macrophage-like cells. Mol. Biol. Cell 3:1269–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hansen, M. B., S. E. Nielsen, and K. Berg. 1989. Re-examination and further development of a precise and rapid dye method for measuring cell growth/cell kill. J. Immunol. Methods 119:203–210. [DOI] [PubMed] [Google Scholar]
- 16.Hanson, R. S., S. Sirinvassen, and H. O. Halverson. 1963. Biochemistry of sporulation. I. Metabolism of acetate by vegetative and sporulating cells. J. Bacteriol. 85:451–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Henderson, D. W., S. Peacock, and F. C. Belton. 1956. Observations on the prophylaxis of experimental pulmonary anthrax in the monkey. J. Hyg. 54:28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ivins, B. E., M. L. M. Pitt, P. F. Fellows, J. W. Farchaus, et al. 1998. Comparative efficacy of experimental anthrax vaccine candidates against inhalation anthrax in rhesus macaques. Vaccine 16:1141–1148. [DOI] [PubMed] [Google Scholar]
- 19.Knudson, G. B. 1986. Treatment of anthrax in man: history and current concept. Mil. Med. 151:71–77. [PubMed] [Google Scholar]
- 20.Leppla, S. H. 1988. Production and purification of anthrax toxin. Methods Enzymol. 165:103–116. [DOI] [PubMed] [Google Scholar]
- 21.Leppla, S. H., B. E. Ivins, and J. W. Ezzell. 1985. Anthrax toxin, p. 63–66. In L. Levine (ed.), Microbiology—1985. ASM Press, Washington, D.C.
- 22.Lincoln, R. E., J. S. Walker, F. Klein, and B. W. Haines. 1964. Anthrax. Adv. Vet. Sci. 9:327–368. [Google Scholar]
- 23.Lincoln R.E. F. Klein, J. S. Walker, B. W. Haines, W. I. Jones, B. G. Mahlandt, and R. H. Friedman. 1965. Successful treatment of rhesus monkey for septicemic anthrax. Antimicrob. Agents Chemother. 4:759–763. [PubMed] [Google Scholar]
- 24.Little, S. F., S. H. Leppla, and A. M. Friedlander. 1990. Production and characterization of monoclonal antibodies against the lethal factor component of Bacillus anthracis lethal toxin. Infect. Immun. 58:1606–1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Little, S. F., B. E. Ivins, P. F. Fellows, and A. M. Friedlander. 1997. Passive protection by polyclonal antibodies against Bacillus anthracis infection in guinea pigs. Infect. Immun. 65:5171–5175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Messelson, M., J. Guilemin, M. Hugh-Jones, A. Langmur, I. Popova, A. Shelokov, and O. Fampolskaya. 1994. The Sverdlovsk anthrax outbreak of 1979. Science 266:1202–1208. [DOI] [PubMed] [Google Scholar]
- 27.Mikesell, P., B. E. Ivins, J. D. Ristroph, and T. M. Dreier. 1983. Evidence for plasmid-mediated toxin production in Bacillus anthracis. Infect. Immun. 39:371–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Presoneus, G. M. S. Cooper, and R. C. Pervical. 1956. Studies on an anthrax vaccine prepared from nonencapsulated variants of Bacillus anthracis. Am. J. Vet. Res. 153–156. [PubMed]
- 29.Puziss, M., L. C. Manning, J. E. Lynch, E. Barclay, I. Abelow, and G. G. Wright. 1963. Large-scale production of protective antigen of Bacillus anthracis in anaerobic cultures. Appl. Microbiol. 11:330–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reuveny, S., M. D. White, Y. Y. Adar, Y. Kafri, Z. Altboum, Y. Gozes, D. Kobiler, A. Shafferman, and B. Velan. 2001. Search for correlates of protective immunity conferred by anthrax vaccine. Infect. Immun. 69:2888–2893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ristroph, J., and B. E. Ivins. 1983. Elaboration of Bacillus anthracis antigens in a new, defined culture medium. Infect. Immun. 39:483–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ross, J. M. 1957. The pathogenesis of anthrax following the administration of spores by respiratory route. J. Path. Bact. 73:485–494. [Google Scholar]
- 33.Sterne, M. 1939. The use of anthrax vaccines prepared from avirulent (uncapsulated) variants of Bacillus anthracis. Onderstepoort J. Vet. Sci. Anim. Industry 13:307–312. [Google Scholar]
- 34.Turnbull, P. C. B., S. H. Leppla, M. G. Broster, C. P. Quinnand, and J. Melling. 1988. Antibodies to anthrax toxin in humans and guinea pigs and their relevance to protective immunity. Med. Microbiol. Immunol. 177:293–303. [DOI] [PubMed] [Google Scholar]
- 35.Uchida, I., T. Sekizaki, K. Hashimoto, and N. Terakado. 1985. Association of the encapsulation of Bacillus anthracis with a 60 megadalton plasmid. J. Gen. Microbiol. 131:363–367. [DOI] [PubMed] [Google Scholar]
- 36.Wilson, G. S., and A. Miles (ed.). 1952. Anthrax, p. 1954. In Topley and Wilson’s principles of bacteriology and immunity, 4th ed. Edward Arnold Publishers Ltd., London, England.