Abstract
Suicide ranks among the main causes of death in most Western countries and is, thus, an important public health problem. Over the last few years, it has been increasingly recognized that people who attempt or commit suicide have a certain individual predisposition, partly resulting from certain personality traits, in particular, impulsive–aggressive behaviors. The evidence suggests that impulsive–aggressive traits are part of a developmental cascade that increases suicide risk among a subset of suicides. These personality traits may also mediate familial transmission of suicidal behavior, defining a behavioral endophenotype that could be useful in molecular genetic studies of suicide. On the other hand, not all suicides are associated with impulsive–aggressive behaviors. There is a need to better understand the mechanisms mediating suicide among individuals with no history of impulsive–aggressive behaviors.
Medical subject headings: impulsive–aggressive behaviors, personality traits, psychopathology, risk factors, suicidal behavior, suicide
Abstract
Le suicide est au nombre des principales causes de mortalité dans la plupart des pays occidentaux et constitue donc un important problème de santé publique. Depuis quelques années, on reconnaît de plus en plus que les gens qui essaient de se suicider ou qui réussissent à le faire ont une certaine prédisposition individuelle qui découle en partie de certains traits de personnalité, et en particulier de comportements impulsifs–agressifs. Les données probantes indiquent que les traits impulsifs–agressifs font partie d'une cascade du développement qui augmente le risque de suicide dans un sous-ensemble de cas. Ces traits de personnalité peuvent aussi entraîner la transmission familiale de comportements suicidaires, définissant un endophénotype comportemental qui pourrait être utile dans les études de génétique moléculaire portant sur le suicide. Par ailleurs, on n'associe pas tous les suicides à des comportements impulsifs–agressifs. Il faut mieux comprendre les mécanismes à l'origine du suicide chez des personnes qui n'ont aucun antécédent de comportements impulsifs–agressifs.
Introduction
The World Health Organization reports that suicide accounts for almost 2% of the world's deaths.1 In Canada, as well as in most of the developed world, suicide is among the 10 leading causes of death for individuals of all ages2,3 and is the leading cause of death for males aged less than 40 years.2,3 In Quebec, suicide is a particularly important problem, because this province has one of the highest suicide rates in North America, with about 1500 cases per year, which accounts for almost one-third of all suicides in Canada.2 Because suicide has a substantially larger impact among young age groups, not surprisingly, it ranks among the main causes of years of potential life lost2,4,5 and, as such, it has been referred to as the “leading cause of unnecessary and premature death.”6 It is clear that suicide takes a terrible toll on our society.
Clinical predictors of suicide
Suicide is a complex behaviour that is most probably the result of the interaction of several different factors (Fig. 1). A positive history of suicide attempts, certain demographic variables such as gender and marital status, clinical symptoms and issues related to social and medical support, such as discharge from psychiatric care, have been found to be particularly associated with suicide.7,8,9,10,11,12 However, these known risk factors are of little help in improving the clinical detection of suicide, and studies that have attempted to predict suicide based on models incorporating these factors have failed to do so.13 The presence of psychopathology is probably the single most important predictor of suicide. Accordingly, about 90% of individuals who commit suicide meet criteria for a psychiatric disorder, particularly major depression, substance use disorders and schizophrenia.14,15 However, it is only a minority of people with these diagnoses who will eventually commit suicide, indicating that a psychiatric disorder may be a necessary, but insufficient, risk factor for suicide. For instance, the lifetime mortality risk for suicide in major depression is estimated to vary between 2% and 7%, with a strong gender effect.16,17 Why do certain patients commit suicide while others with the same psychiatric problem do not? This is a question that has long puzzled clinicians and is of enormous clinical relevance.18 In fact, assessing suicide risk is probably one of the most — if not the most — difficult task mental health professionals face in their clinical practice.
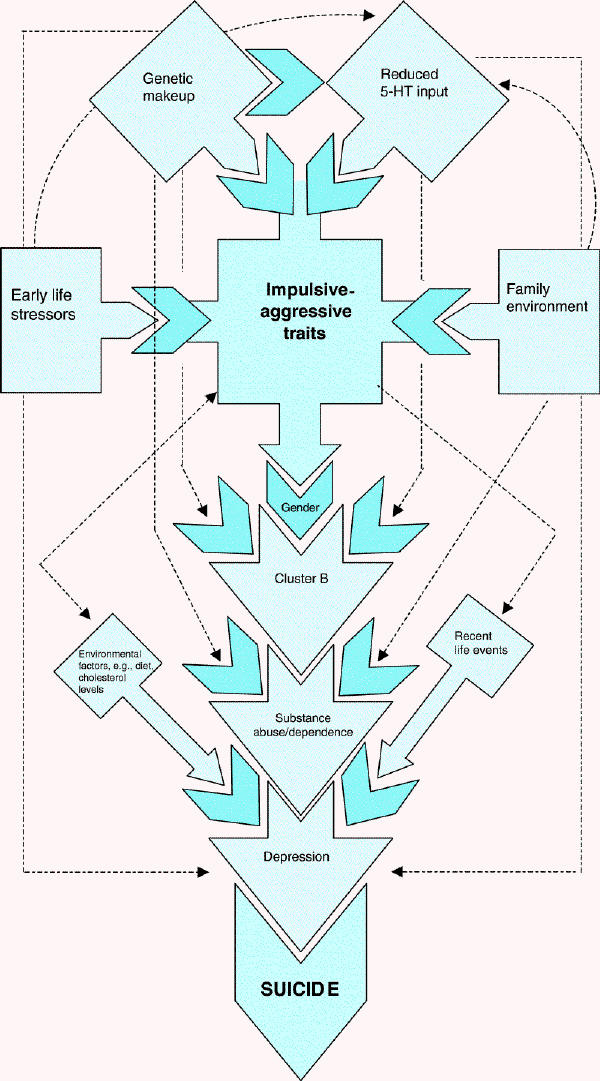
Fig. 1: The hypothesized relations between different risk factors for suicide in major depression, with emphasis on the mediating role of impulsive–aggressive behaviours. 5-HT = serotonin.
Is there a predisposition to suicide?
Over the last few decades, it has become increasingly clear that people who commit suicide have a certain individual predisposition.19,20,21 However, the relation between this predisposition, which is to a large extent conferred by the individual's biological makeup, and suicide is not direct, but seems to be mediated and moderated by a number of different factors. Among these factors are clinical and demographic risk factors, such as those listed earlier, history of early life sexual and physical abuse,22,23,24,25,26,27 personality variants such as behavioural traits28,29,30,31,32,33,34,35,36,37,38,39,40 and recent life events.41,42,43,44,45,46,47,48,49 This review will focus on the role of personality traits in predisposition to suicide and, particularly, on the relation between impulsive–aggressive traits and suicide.
Personality traits and suicide risk
Personality traits represent emotional, behavioural, motivational, interpersonal, experiential and cognitive styles that help us relate to and cope with the world.50,51,52
Personality traits are determined by environment, individual genes, and gene–gene and gene–environment interactions.53,54,55,56,57,58,59,60,61 Structural models suggest that personality has a hierarchical organization with multiple narrow or basic traits coalescing into about 3–5 higher-order dimensions.62,63,64,65,66 Depending on the model, the latter are defined as extroversion, psychoticism and neuroticism;62 harm avoidance, novelty seeking, reward dependence and persistence;67 neuroticism, agreeableness, openness to experience, conscientiousness and extroversion;68 or emotional instability, compulsivity, antagonism and inhibition.63
Over the last 3 decades, interest in the contribution of personality trait profiles to complex behavioural phenomena such as suicidal behaviour has increased.29,51,61,69,70 Suicidal behaviours may result from reciprocal interactions between maladaptive cognitions, affect, and behavior, occurring subsequently to an environmental/internal precipitant.71,72
Clinical and community research suggest links between suicidality, on the one hand, and “extreme” personality profiles, on the other hand.51,69,73,74,75,76,77 For instance, both undercontrolled and inhibited 3-year-old children were found to be more likely to attempt suicide as young adults.78 In general, introverted/negativistic/avoidant/dependent/neurotic as well as impulsive/hostile/antisocial personality features may cluster in suicidal individuals,71,79,80 and possibly in a gender-specific fashion.69
Personality traits have several properties that make them attractive targets for suicidality research and intervention. First, they affect variables that may contribute to the diathesis for suicide, namely, our perception of and adaptations to the environment and “self.”55,81 Second, their maturational patterns may render them more suitable for long-term public health interventions compared with other, more changeable risk factors. More specifically, even though traits are amenable to modification only relatively early in life, any intervention that is carried out at this time would have longer-lasting effects.65,82 Third, they may be useful in early identification of subgroups of suicidal individuals, such as repeated attempters83 and older completers.84 Finally, gender-specific personality differences may contribute to gender dissimilarities observed in suicide attempts and completions.85,86
Personality variants mediating suicide: the role of impulsive behaviours
Impulsivity may be conceptualized as the inability to resist impulses, which, from the strict phenomenologic point of view, refer to explosive and instantaneous, automatic or semi-automatic psychomotor actions that are characterized by their sudden and incoercible nature.87,88 A more behavioural definition considers impulsivity as a drive, stimulus or behaviour that occurs without reflection or consideration for the consequences of such behaviour.89 The concept of impulsivity spans a wide range of behaviours that are usually risky or inappropriate to the situation, and whose outcomes are often undesirable.89 There is considerable debate in the literature about how to define and measure impulsivity, yet the term is often understood to reflect a continuum of a personality feature or trait. Although not all studies provide consistent findings supporting the role of impulsivity in suicidal behaviour, most studies indicate that suicide attempters and suicide completers tend to have higher levels of impulsive behaviour. For instance, positive associations with suicide attempts have been reported in clinical populations,90 including patients with major depression and pathological gambling,22,91 as well as patients who have made a suicide attempt with a high degree of lethality.92 Impulsivity, as assessed by the novelty-seeking Temperament and Character Inventory (TCI ) dimension, measured at the age of 16 years, was also found to be an important predictor of risk of a future suicide attempt in cohort studies.23,49 Similarly, there is also evidence suggesting that suicide completers, particularly younger ones, have higher levels of impulsivity than controls.28,93 On the other hand, a few other studies failed to find a significant relation between impulsivity and suicidal behaviour.94,95
The findings of our group in investigating impulsive traits are consistent with an overall effect of impulsivity in suicidal behaviour. In a cohort of young adults representative of the Quebec general population, we investigated the relation between personality variants and suicide attempts, as well as serious suicidal ideation. Both attempters and serious ideators had higher scores of impulsivity as measured by the Barratt impulsivity scale (BIS v.11).96 Attempters and nonattempters had mean scores, respectively, of 69.05 (standard deviation [SD] 10.53) and 64.97 (SD 9.80) (p < 0.001), whereas serious ideators and nonideators had, respectively, mean scores of 69.32 (SD 9.31) and 64.83 (SD 9.82) (p < 0.001).97
Studying unselected suicide completers from the general Quebec population, we found higher levels of impulsivity and related behaviours when compared with healthy controls or controls with psychiatric disorders (Dr. Hana Zouk et al, McGill Group for Suicide Studies, Montréal: unpublished observations, 2005).39,98 Mean impulsivity scores among suicide completers using the BIS adapted to proxy-based interviews, as carried out in psychological autopsies, were normally distributed, but had higher amplitude than those seen in the healthy population. Thus, more extreme levels of impulsivity were more commonly observed among suicide completers, and BIS scores averaged 84.5 (standard error of the mean [SEM] 0.75) among the most impulsive completers (Zouk et al, unpublished observations, 2005). We also found that subjects who used the so-called violent methods of suicide tended to have significantly higher levels of impulsivity (mean BIS scores of 69.33 [SEM 1.38]) than those who used non-violent suicide methods (64.01 [SEM 2.53]).39 In addition, impulsive suicides were more likely to have increased comorbidity than nonimpulsive suicides (Zouk et al, unpublished observations, 2005).
Personality variants and axis I psychopathology
An important question that the studies reviewed here and other studies of suicide completers did not address is whether or not the association between impulsivity and suicide risk is at least partly explained by axis I psychopathology. This issue has not been properly addressed because most psychological autopsy studies of suicide have exclusively investigated unselected suicides compared with healthy controls and, in general, lacked a psychiatric control group. To address this question, we recently carried out studies comparing subjects who committed suicide during an episode of major depression with age- and sex-matched living control subjects with a history of major depressive disorder and a current major depressive episode of sufficient severity to warrant treatment in a specialized psychiatric outpatient clinic, but without a history of medically serious suicide attempts.39,40 Controlling, by nature of the design for the presence of primary psychopathology — in this case, major depressive disorder — and using comparable methodology in both groups (i.e., proxy-based interviews), our results indicated that suicide completers had higher levels of impulsivity and a lifetime history of aggressive behaviours, comorbidity with cluster B personality disorders, particularly antisocial personality disorder and borderline personality disorders, as well as comorbidity with alcohol- and drug-related disorders.40 Therefore, it seems clear that excess impulsivity in suicide is not a consequence of major depression.
To what extent this is also generalizable to suicides associated with other common axis I diagnoses, such as schizophrenia, remains to be investigated. In fact, personality variants generally identified as risk factors for suicide have not been associated with an increased risk among individuals with schizophrenia99,100 and, in our clinical studies, suicides with a history of schizophrenia did not show evidence of increased comorbidity with conditions characterized by the presence of impulsive and aggressive behaviours such as cluster B personality disorders.101
Personality variants mediating suicide: the role of aggressive behaviours
It follows from the studies discussed here,28,31,102 however, that it is not the exclusive presence of impulsivity in either its motor, focal or planning dimensions that is often observed associated with suicide. Rather, among suicides, impulsivity is comorbid with other personality traits, particularly aggressive behaviours, which have often been present since childhood. In our series of suicide completers, high levels of impulsivity correlate strongly and significantly with high levels of aggressive behaviour or hostility. For instance, impulsive suicide completers — defined as those with BIS scores above 75 — had significantly higher levels of a lifetime history of aggressive behaviours, as measured by the Brown–Goodwin Lifetime Aggression instrument (mean score 19.73 [standard deviation {SD} 3.02]) as compared with nonimpulsive suicides (mean score 6.89 [SD 1.17]) (p < 0.001). Similarly, scores on the Buss-Durkee Hostility Inventory were higher among impulsive suicides (36.02 [SD 1.05]) as compared with nonimpulsive suicides (27.85 [SD 0.98]) (p < 0.001) (Zouk et al, unpublished observations, 2005). As such, it is clear that suicides tend to have high levels of aggressive–destructive impulsive behaviours, generally referred to as impulsive–aggressive behaviours. These have been operationally defined in suicide studies as a tendency to react with animosity or overt hostility without consideration to possible consequences, when piqued or under stress.
Impulsive–aggressive behaviours and comorbidity
Psychiatric comorbidity, defined as the presence of more than 1 psychiatric diagnosis, has been commonly reported in suicides.103,104,105 Studies of suicide attempters have found comorbidity in 56%–82% of cases, and subjects with comorbid psychopathology have a higher odds of attempting suicide than those without any diagnosis.34,106,107 Several groups have also reported a high occurrence of comorbidity in suicide completers. When compared with nonsuicidal controls, child and adolescent suicide completers have consistently shown higher rates of overall comorbidity,108,109 a finding that has been replicated in studies of adults.104,110 A large psychological autopsy study of suicide completers conducted in Finland found that only 12% of suicides had an axis I diagnosis without comorbidity.104 In a 1999 comparison with matched community controls, a significant increase in suicide risk in the presence of axis I–axis II comorbidity was reported (odds ratio 346.0, p < 0.001).46 It is clear that the presence of multiple diagnoses of psychiatric disorders is an important factor that should be taken into account when assessing suicide risk. We carried out latent class analyses to investigate patterns of comorbidity in unselected suicide completers from the general population and matched controls.101 Latent class analysis is a method derived from factor analysis that can be used to identify homogeneous subgroups within a larger group by analyzing patterns of the presence or absence of measured variables. Using this technique, we found 3 subgroups that differed significantly in the amount and pattern of comorbidity. Comorbidity was particularly found in subjects with disorders characterized by the presence of impulsive and impulsive–aggressive traits, whereas subjects without these traits had levels of comorbidity that were not significantly different from those of controls. Interestingly, the group with higher levels of comorbidity was characterized by suicides with a life trajectory beginning early in childhood. They presented a high proportion of childhood disorders associated with impulsive–aggressive traits such as ADHD, oppositional defiant disorder and conduct disorder, as well as a higher incidence of antisocial personality disorder.101 This suggests that impulsive–aggressive suicide may be a developmental problem beginning early on in life and translated by large psychopathological loading that presents as diagnostic comorbidity.
Impulsive–aggressive behaviours and suicide: Is there an age effect?
It has long been suggested that younger and older suicides may be different entities.43,44,111,112,113,114,115,116,117 However, it remains to be better investigated whether suicide is the same phenomenon across the life cycle or whether it has a different meaning and set of risk factors when it occurs in childhood or in older age. Unfortunately, most researchers studying suicide have viewed age as a confounding variable to be controlled for, rather than as a variable of interest.118 As a result, most data available regarding age differences in suicide come from post hoc comparative analyses of unselected suicide samples.
The Finnish National Suicide Prevention Project provides some clues to this question.37,104,119 This large-scale study collected information about all suicides committed in Finland over a period of 1 year between 1987 and 1988. A total of 1397 cases were studied by means of psychological autopsies. Their findings suggest that suicide in young subjects may be a different phenomenon from suicide later in life. Accordingly, the psychiatric profiles of these 2 groups seem to be different. Major depression is significantly more common among older people who commit suicide,116 whereas the presence of axis II comorbidity is more often observed in younger people who commit suicide.30,116 Other psychological studies confirm these observations, indicating that a considerable percentage of elderly suicide cases (> 55 yr) meet criteria not only for major recurrent depression but also for other chronic depressive conditions such as dysthymia.120 Conwell et al120 also found that youthful suicide was different from elderly suicide because the former was associated with more substance abuse or dependence, a finding that is supported by psychological studies in young completers.105,108,121,122
Studies indicate that an important proportion of elderly people who commit suicide have made a previous suicide attempt.118 Consistent with this notion, studies in elderly attempters suggest that subjects with early onset of major depression have a higher chance of presenting suicidal behaviour.123,124 These observations are in agreement with data from a prospective long-term follow-up study by Angst et al,125 who observed that the cumulative risk of suicide continued to increase with successive episodes of the illness. On the other hand, studies of suicidal behaviour in young patients suggest that the risk of suicide attempts does not seem to be randomly distributed in the course of the disorder. In other words, young patients who attempt suicide often do so early in the course of the disease.126 Indeed, this is also consistent with data from psychological autopsies in our sample of young suicide completers, which indicate that among subjects diagnosed with major depression, almost 60% of the individuals committed suicide during the first episode of the illness. Therefore, these results seem to indicate that suicidal behaviour has a different “natural history” in younger and older subjects, even when the underlying psychopathology is similar. Thus, in our study comparing depressed suicides with depressed controls described earlier,40 an important age effect was observed, suggesting that impulsive–aggressive behaviours play a substantial role primarily in young suicide completers. Conversely, among unselected suicide completers, the presence of impulsive–aggressive behaviours is more likely to be observed among younger than among older suicide completers (Zouk et al., unpublished observations, 2005) and, interestingly, when impulsive and nonimpulsive suicides are compared, no differences are found in rates of associated mood disorders.
Further data suggesting the different role of impulsive–aggressive behaviours and possibly the different nature of youthful and elderly suicide come from studies by Conwell et al.118,120 These authors assessed age differences in behaviours leading to completed suicide and found that older age was significantly associated with more determined and planned self-destructive acts, less violent methods and fewer warnings of suicidal intent. Taken together, these results seem to suggest that young and elderly subjects who commit suicide have different diatheses. Indeed, there is support for the notion that younger suicides are more likely to be the result of an impulsive–aggressive act, often facilitated by alcohol or drug intoxication, or both, in subjects who have a pervasive problem in their personality structure and are affected by an axis I disorder. Moreover, this tragic event is frequently associated with a stressful life event, which in itself frequently seems to be associated with the subject's underlying personality traits. On the other hand, elderly suicide is more often the consequence of a planned, less impulsive act often in a physically ill and depressed subject, who has been enduring difficult life events that are more commonly related to the medical illness or to events that are intrinsic to the age group.
Impulsive–aggressive behaviours: the role of environmental factors
There has been substantial interest in the investigation of the relation between history of childhood abuse and suicidal behaviour.27,127,128 Comparing impulsive and nonimpulsive suicide completers based on data obtained with the Childhood Experience of Care and Abuse (CECA) interviews, our group found that history of parental rejection, negligence, indifference and abuse were more likely to be reported among those suicides with high levels of impulsivity (Zouk et al, unpublished observations, 2005). We might speculate that early life stressors, particularly those listed here, may trigger dysfunctional behaviour providing a platform for abnormal expression of impulsivity comorbid with aggressive behaviour. This is consistent with suggestions that impulsivity per se may, at least in part, be linked to negative early life experiences, including a history of physical or sexual abuse.90 This, in turn, may be associated with risk of personality disorders129 and self-destructive behaviour in adulthood.22,130 Indeed, adolescents admitted to a psychiatric hospital who report a history of childhood abuse are typified by increased levels of violence, impulsivity, suicidality and substance use problems,131 suggesting that this constellation of psychological and behavioural symptoms belongs to a common early behavioural pathway that is affected by the influence of negative life events. Moreover, in a model attempting to explain the mechanism of the development of borderline personality disorder, it has been speculated that the negative affect and reactivity characteristic of borderline personality disorder, also seen in many impulsive suicides, when interacting with an abusive environment, may result in impulsive and self-destructive behaviour.132 This, in turn, may reinforce impulsivity and emotional dysregulation leading to hypersensitivity to stressful events encountered in the future.133 It has also been suggested that the expression of such impulsive and suicidal behaviours in borderline personality disorder may be part of a mechanism to cope with the stress that is brought on by this innate hypersensitivity to interpersonal and environmental stimuli.134 Thus, it is possible that impulsive suicide is partly a developmental problem associated with a dysfunctional developmental cascade. Recent studies by our group on developmental trajectories in suicide completers support this view, particularly among young suicides.
We have recently concluded a study of all suicide deaths in New Brunswick, Canada, between April 2002 and May 2003.135 A total of 102 suicides (of 109 suicides that occurred over that period) were investigated. Life trajectories were studied and rated using a life calendar investigating 12 developmental spheres to trace the events that marked the individual's life. Four different life trajectories were identified. Interestingly, the youngest suicides were those who had a life trajectory with the largest number of adversity factors reported since early life, including neglect, mistreatment, major family conflict and history of abuse. These subjects presented important comorbidity with personality disorders, including cluster B diagnoses, which are characterized by the presence of impulsive–aggressive behaviours. This is consistent with the data from our comorbidity studies101 and suggests that impulsive–aggressive suicide is the result of developmental problems that begin early in life.
Familial factors in the transmission of suicide
The notion that suicide aggregates in families is not new. Indeed, as early as 1790, Charles Moore in his book entitled A Full Enquiry into the Subject of Suicide noted that propensity to suicide is hereditary. This hypothesis has been tested by a number of family-history studies, which have clearly shown that suicidal behaviour aggregates in families. In a seminal paper investigating the clinical features of 100 suicide completers, Barraclough et al136 reported that 4% of these subjects had at least 1 first-degree relative who died by suicide, as confirmed by a death certificate. Other studies of completers reported similar results137,138 and showed that positive family history increased considerably when suicide attempts in the relatives were also taken into account.45,122,139,140,141 Consistent findings were reported by studies assessing the risk of suicidal behaviour in patients with a positive family history of suicide.142 Similar results were found by family-history studies of probands who attempted suicide.36,126,143,144,145,146 Family- history studies have a number of methodological shortcomings and, though important, their conclusions should be validated by more powerful designs, such as family studies with direct and blind assessment of recurrent risks in relatives. Only a few controlled family studies with direct interviews with relatives have been carried out, and the findings of these studies are consistent with the findings from family-history studies.93,147,148 A recent meta-analysis with quantitative synthesis of the results of family studies indicates that relatives of suicides have about a 5-fold greater recurrent risk than relatives of controls.149 Therefore, it is clear that relatives of subjects who committed or attempted suicide have a higher risk of suicidal behaviour than do relatives of controls. However, considering that suicidal behaviour is associated with the presence of psychiatric disorders, which in turn also tend to aggregate in families, whether or not the familial aggregation observed for suicidal behaviour is conditional on the familial loading of psychiatric disorders has been an important question that some studies have attempted to address.
Overall, studies suggest that the familial aggregation of suicide is conditional on — but independent from — the loading of psychiatric morbidity.93,147,150 In a well-known family study in the Old Order Amish, Egeland and Sussex150 showed that while mood disorders aggregated in a number of different multigenerational families, co-segregation with suicide was observed in only a few of them. Accordingly, the 26 suicides that were recorded in 100 years of history of that community clustered in only 4 families. Although this study was only descriptive, it clearly indicated that the presence of the affective disorder is necessary but not sufficient to commit suicide. This is consistent with data suggesting that patients with bipolar disorder and a positive family history of bipolar disorder and suicide have different familial loading for suicidal behaviour (suicide tendencies and attempted suicide) from patients with bipolar disorder and a positive family history of bipolar disorder but without suicide.151 Similarly, a familial history of suicide was found to significantly increase the risk of suicidal behaviour among patients with major depression.152 The risk of suicide completion conferred by a positive family history has been estimated in psychiatric inpatients to be around 4.6.138 Brent et al93 investigated 58 adolescent suicide completers and 56 healthy controls and found a risk of recurrence of suicide attempts and completions of 14% and 4.6%, respectively, for first- and second-degree relatives of suicide probands and 3% and 1% for relatives of controls, with an estimated relative risk for first-degree relatives of 5.3. The same group carried out a family study of probands who had attempted suicide, which was also supportive of familial clustering, providing relative risk estimates around 2.3.147 Our group has recently completed a controlled family study investigating 247 relatives of 25 adult male suicides and 171 relatives of 25 matched controls.148 We found consistent results with those reported by Brent et al, because the relatives of suicides were over 10 times more likely than relatives of controls to have attempted or completed suicide, after controlling for psychopathology. Although the relatives of suicides were not more likely to have exhibited suicidal ideation, they had more severe suicidal ideation than relatives of controls.
Impulsive–aggressive behaviours: Behavioural endophenotype?
As discussed here, susceptibility to suicide may be regarded as the result of triggering factors such as major depression mediating the effect of predisposing factors such as personality structure and levels of impulsive–aggressive behaviours. One of the hypotheses that have been put forward speculates that part of the familial liability to suicide may be transmitted through impulsive–aggressive behaviours. These behaviours aggregate in families,153,154,155,156 and twin studies suggest that at least part of the familial aggregation is the result of genetic factors.157,158 Interestingly, in the family study by Brent et al,93 some measures of aggressive behaviour were administered in probands and relatives, and an important observation was that probands who had attempted suicide and had high scores of aggression had much greater familial loading for suicide attempts and completions than less aggressive probands who had attempted suicide. Moreover, the relatives of the individuals who had committed suicide presented higher rates of those personality disorders that are associated with impulsive–aggressive behaviours, particularly antisocial and borderline personality disorder, as well as a history of conduct disorder and substance abuse. More recently, the same group investigated the offspring of individuals with a mood disorder, some of whom had attempted suicide and some of whom had not, and found a 6-fold increased risk of attempts among the offspring of those who had attempted suicide.25 Factors increasing risk of aggregation included increased levels of impulsive aggression. In a reanalysis of these data,159 the same group reported that a positive family history of suicidal behaviour, as measured by concordance with a sibling, and lifetime impulsive–aggressive behaviours predicted not only recurrence of attempts in offspring of suicide attempters, but also younger age at onset of suicidal behaviour. This is consistent with data from our family study suggesting that first-degree relatives of suicides were more likely to exhibit aggression than relatives of controls.148 These findings were more pronounced in families where the proband had a cluster B diagnosis. Other studies provided congruent results.36,152 Similar findings were also reported with probands who had attempted suicide.147 Taken together, these studies indicate that relatives of probands with suicidal behaviour have an increased likelihood of exhibiting higher levels of impulsive–aggressive behaviours. These, in turn, may play a role in mediating familial transmission of suicidal behaviour and, as such, may be considered as a behavioural endophenotype in genetic studies of suicide.
Serotonin, impulsive aggression and suicidal behaviour
The role of impulsive aggression in suicidal behaviour is also supported by other lines of evidence, including findings from neurochemical, animal and genetic investigation. Indeed, a large volume of neurobiological data has been produced over the last 20 years. The results from these studies jointly indicate that patients with suicidal behaviour have reduced central serotonergic activity.19,160 Interestingly, studies investigating subjects with impairment of impulse control and violent behaviours have found similar alterations.161,162,163 Thus, it is plausible that reduced serotonergic activity may be linked to impulsive–aggressive behaviours, which in turn may increase susceptibility to suicide. Support for a relation between low serotonergic neurotransmission and suicidal behaviour comes from several lines of evidence, including studies of cerebrospinal fluid 5-HIAA (5-hydroxyindoleacetic acid), neuroendocrine challenges, platelet studies, postmortem brain studies and, more recently, brain imaging studies. Although it is still too early to draw definite conclusions based on the brain imaging data in suicidal behaviour, postmortem brain studies have generated a large volume of data that, when taken together, mostly indicate a decrease in presynaptic serotonin (5-HT) transporter in the prefrontal cortex, particularly in ventral areas,164 and an increase in presynaptic 5-HT1A binding in the raphe nuclei,165 as well as a possible upregulation of postsynaptic 5-HT receptors, particularly 5-HT1A166 and 5-HT2.167,168 These alterations suggest reduced serotonergic input into this brain region, which is believed to be involved in the brain circuitry controlling impulse and violent behaviour regulation.163,169,170 It is thus possible that subjects with low serotonergic input into this part of the brain may be more likely to act impulsively and self- aggressively when exposed to stressful life events, such as those associated with major depression, and, in some instances, this may result in suicide. Therefore, the neurobiological data suggest a similar neurobiological substrate for suicide and impulsive aggression and provide further support for the idea that, at least in a subgroup of suicides, impulsive–aggressive traits may help define a behavioural endophenotype.
Non-impulsive–aggressive suicide
As reviewed here, there is overwhelming evidence to support the role of impulsive and, more appropriately stated, impulsive–aggressive behaviours in suicide. However, not all suicides are mediated by impulsive–aggressive behaviours, and this seems to be more likely to be the case among older individuals. The question that follows, thus, at least at the phenomenological level, is whether there are other behavioural or personality traits mediating suicide risk in cases that have no evidence of highly impulsive–aggressive behaviours. This issue has remained practically unexplored, because most of the research investigating behavioural traits in suicide has focused on cluster B traits. Data from our sample of unselected suicide completers indicate that subjects without impulsive–aggressive behaviours have lower rates of comorbidity than impulsive–aggressive suicides and, in fact, they have levels of comorbidity that are not significantly different from healthy controls.101 Moreover, non-impulsive–aggressive suicides have lower comorbidity with substance-related disorders and do not display evidence of higher levels of specific behavioural measures. Our study of suicide and depression indicated that total levels of cluster C personality trait loading and cluster C personality disorders were not associated with an increased risk of suicide when directly controlling for major depressive disorder. This is in contrast with previous findings46,171 and suggests that the evidence of excess cluster C personality disorders in suicides is accounted for by the high frequency of mood disorders in suicides rather than by a direct effect of these personality disorders on suicide risk. However, in the study that we have recently carried out investigating the relation between personality traits and suicidal behaviour in a sample representative of the Quebec general population, we found that the interaction between compulsivity and depressed mood played a central role in predicting suicidal behaviour (Dr. Jelena Brezo et al, McGill Group for Suicide Studies, Montréal: unpublished observations, 2005), suggesting that perhaps interactions between specific cluster C traits and axis I disorders, particularly depressive disorders, may help increase risk for suicide in individuals with no history of impulsive–aggressive behaviors. As such, one may speculate that individuals with high levels of compulsivity, because of their tendency to be rigid and to engage in thought rumination, may, when depressed, be at higher risk of attempting suicide, because these subjects will be less likely to contemplate alternative solutions to deal with life stressors or perceived failures or weaknesses and would more easily engage in a ruminant pattern of negatively charged self-directed thoughts.
Conclusion
The role of impulsive–aggressive behaviours in risk of suicide has been well substantiated by several lines of evidence, including case–control studies in clinical populations, cohort studies in epidemiological samples, retrospective studies of completed suicides and case registries. The association between impulsive–aggressive behaviours and suicide is primarily seen among young people and seems to be independent from the role of associated axis I psychopathology, particularly major depression. High levels of impulsive–aggressive behaviours have been linked to early life environmental stressors such as childhood abuse and neglect, and these stressors are also more commonly seen among impulsive–aggressive suicides (Fig. 1). In addition, studies of life trajectories of suicides indicate that impulsive–aggressive suicides are likely to have had a trajectory characterized by the cumulative effects of negative life stressors and abuse, suggesting that a subset of suicides may, at least in part, be the result of a dysfunctional developmental cascade with onset early in life and mediated by excessive impulsive–aggressive behaviours. This is interesting because family studies of suicidal behaviour also suggest that these personality traits may mediate familial loading of suicide attempts and completions. Moreover, neurobiological correlates of suicidal behaviour are similar in nature to those reported for patients with impairment of impulse control and violent behaviours, which would further suggest that impulsive–aggressive behaviours may help define a behavioural endophenotype of suicide. This should be taken into account when planning studies investigating molecular genetic factors in suicide. On the other hand, not all suicides are associated with impulsive–aggressive behaviours. There is a need to better understand the mechanisms mediating suicide among individuals with no history of impulsive–aggressive behaviors.
Acknowledgments
The author is a Canadian Institutes of Health Research (CIHR) Scholar, and part of the author's group's work discussed in this review was supported by CIHR grants MOP-38078 and MOP-53321. The author would like to thank Jelena Brezo and Hana Zouk for their input in sections of this manuscript.
Footnotes
2003 CCNP Young Investigator Award Paper
Competing interests: None declared.
Correspondence to: Dr. Gustavo Turecki, McGill Group for Suicide Studies, Douglas Hospital Research Centre, McGill University, 6875 LaSalle Blvd., Montréal QC H4H 1R3; fax 514 762-3023; gustavo.turecki@mcgill.ca
Submitted June 27, 2005; Accepted Sept. 2, 2005
References
- 1.World Health Organization. World health report 2000: health systems: improving performance. Geneva: WHO; 2000.
- 2.Statistics Canada. Suicides, and suicide rate, by sex, by age group. Report no. 82F0075XCB. Ottawa: Statistics Canada; 1997.
- 3.Mao Y, Hasselback P, Davies JW, Nichol R, Wigle DT. Suicide in Canada: an epidemiological assessment. Can J Public Health 1990;81:324-28. [PubMed]
- 4.Mercier G, Saint-Laurent D. S'entraider pour la vie : stratégie québécoise d'action face au suicide. Québec: Ministère de la santé et des services sociaux; 1998.
- 5.Saint-Laurent D, Tennina S. Résultats de l'enquete portant sur les personnes décédées par suicide au Québec entre le 1er septembre et le 31 decembre 1996. Québec: Ministère de la santé et des services sociaux; 2000.
- 6.Maris RW, Berman AL, Silverman MM. Comprehensive textbook of suicidology. New York: The Guilford Press; 2000.
- 7.Barraclough BM, Pallis DJ. Depression followed by suicide: a comparison of depressed suicides with living depressives. Psychol Med 1975;5:55-61. [DOI] [PubMed]
- 8.Fawcett J, Scheftner WA, Fogg L, Clark DC, Young MA, Hedeker D, et al. Time-related predictors of suicide in major affective disorder. Am J Psychiatry 1990;147:1189-94. [DOI] [PubMed]
- 9.Beck AT, Brown G, Berchick RJ, Stewart BL, Steer RA. Relationship between hopelessness and ultimate suicide: a replication with psychiatric outpatients. Am J Psychiatry 1990;147:190-5. [DOI] [PubMed]
- 10.Beck AT, Steer RA, Kovacs M, Garrison B. Hopelessness and eventual suicide: a 10-year prospective study of patients hospitalized with suicidal ideation. Am J Psychiatry 1985;142:559-63. [DOI] [PubMed]
- 11.Beck AT, Brown G, Steer RA. Prediction of eventual suicide in psychiatric inpatients by clinical ratings of hopelessness. J Consult Clin Psychol 1989;57:309-10. [DOI] [PubMed]
- 12.Goldacre M, Seagroatt V, Hawton K. Suicide after discharge from psychiatric inpatient care. Lancet 1993;342:283-6. [DOI] [PubMed]
- 13.Goldstein RB, Black DW, Nasrallah A, Winokur G. The prediction of suicide. Sensitivity, specificity, and predictive value of a multivariate model applied to suicide among 1906 patients with affective disorders. Arch Gen Psychiatry 1991;48:418-22. [DOI] [PubMed]
- 14.Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med 2003;33:395-405. [DOI] [PubMed]
- 15.Arsenault Lapierre G, Kim C, Turecki G. 3500 cases of suicide: a systematic review. BMC Psychiatry 2004;4:34-7. [DOI] [PMC free article] [PubMed]
- 16.Blair-West GW, Cantor CH, Mellsop GW, Eyeson-Annan ML. Lifetime suicide risk in major depression: sex and age determinants. J Affect Disord 1999;55:171-8. [DOI] [PubMed]
- 17.Angst F, Stassen HH, Clayton PJ, Angst J. Mortality of patients with mood disorders: follow-up over 34-38 years. J Affect Disord 2002;68:167-81. [DOI] [PubMed]
- 18.Jacobs DG. Depression screening as an intervention against suicide. J Clin Psychiatry 1999;60(Suppl 2):42-5. [PubMed]
- 19.Mann JJ. The neurobiology of suicide. Nat Med 1998;4:25-30. [DOI] [PubMed]
- 20.Turecki G. Suicidal behavior: Is there a genetic predisposition? Bipolar Disord 2001;3:335-49. [DOI] [PubMed]
- 21.Roy A, Rylander G, Sarchiapone M. Genetics of suicides. Family studies and molecular genetics. Ann N Y Acad Sci 1997;836:135-57. [DOI] [PubMed]
- 22.Brodsky BS, Oquendo M, Ellis SP, Haas GL, Malone KM, Mann JJ. The relationship of childhood abuse to impulsivity and suicidal behavior in adults with major depression. Am J Psychiatry 2001;158: 1871-7. [DOI] [PubMed]
- 23.Fergusson DM, Beautrais AL, Horwood LJ. Vulnerability and resiliency to suicidal behaviours in young people. Psychol Med 2003; 33: 61-73. [DOI] [PubMed]
- 24.Angst J, Degonda M, Ernst C. The Zurich Study: XV. Suicide attempts in a cohort from age 20 to 30. Eur Arch Psychiatry Clin Neurosci 1992;242:135-41. [DOI] [PubMed]
- 25.Brent DA, Oquendo M, Birmaher B, Greenhill L, Kolko D, Stanley B, et al. Familial pathways to early-onset suicide attempt: risk for suicidal behavior in offspring of mood-disordered suicide attempters. Arch Gen Psychiatry 2002;59:801-7. [DOI] [PubMed]
- 26.Ystgaard M, Hestetun I, Loeb M, Mehlum L. Is there a specific relationship between childhood sexual and physical abuse and repeated suicidal behavior? Child Abuse Negl 2004;28:863-75. [DOI] [PubMed]
- 27.Van der Kolk BA, Perry JC, Herman JL. Childhood origins of self-destructive behavior. Am J Psychiatry 1991;148:1665-71. [DOI] [PubMed]
- 28.Brent DA, Johnson BA, Perper J, Connolly J, Bridge J, Bartle S, et al. Personality disorder, personality traits, impulsive violence, and completed suicide in adolescents. J Am Acad Child Adolesc Psychiatry 1994;33:1080-6. [DOI] [PubMed]
- 29.Duberstein PR, Conwell Y, Seidlitz L, Denning DG, Cox C, Caine ED. Personality traits and suicidal behavior and ideation in depressed inpatients 50 years of age and older. J Gerontol B Psychol Sci Soc Sci 2000;55:P18-26. [DOI] [PubMed]
- 30.Isometsa ET, Henriksson MM, Heikkinen ME, Aro HM, Marttunen MJ, Kuoppasalmi KI, et al. Suicide among subjects with personality disorders. Am J Psychiatry 1996;153:667-73. [DOI] [PubMed]
- 31.Soloff PH, Lis JA, Kelly T, Cornelius J, Ulrich R. Risk factors for suicidal behavior in borderline personality disorder. Am J Psychiatry 1994;151:1316-23. [DOI] [PubMed]
- 32.Nordstrom P, Schalling D, Asberg M. Temperamental vulnerability in attempted suicide. Acta Psychiatr Scand 1995;92:155-60. [DOI] [PubMed]
- 33.Joffe RT, Regan JJ. Personality and suicidal behavior in depressed patients. Compr Psychiatry 1989;30:157-60. [DOI] [PubMed]
- 34.Beautrais AL, Joyce PR, Mulder RT, Fergusson DM, Deavoll BJ, Nightingale SK. Prevalence and comorbidity of mental disorders in persons making serious suicide attempts: a case-control study. Am J Psychiatry 1996;153:1009-14. [DOI] [PubMed]
- 35.Brent DA, Johnson B, Bartle S, Bridge J, Rather C, Matta J, et al. Personality disorder, tendency to impulsive violence, and suicidal behavior in adolescents. J Am Acad Child Adolesc Psychiatry 1993;32:69-75. [DOI] [PubMed]
- 36.Pfeffer CR, Normandin L, Kakuma T. Suicidal children grow up: suicidal behavior and psychiatric disorders among relatives. J Am Acad Child Adolesc Psychiatry 1994;33:1087-97. [DOI] [PubMed]
- 37.Marttunen MJ, Aro HM, Henriksson MM, Lonnqvist JK. Mental disorders in adolescent suicide. DSM-III-R axes I and II diagnoses in suicides among 13- to 19-year-olds in Finland. Arch Gen Psychiatry 1991;48:834-9. [DOI] [PubMed]
- 38.Lesage AD, Boyer R, Grunberg F, Vanier C, Morissette R, Menard-Buteau C, et al. Suicide and mental disorders: a case-control study of young men. Am J Psychiatry 1994;151:1063-8. [DOI] [PubMed]
- 39.Dumais A, Lesage AD, Lalovic A, Seguin M, Tonsignant M, Chawky N, et al. Is violent method of suicide a behavioral marker of lifetime aggression? Am J Psychiatry 2005;162(7):1375-8. [DOI] [PubMed]
- 40.Dumais A, Lesage A, Dumont M, Chawky N, Benkelfat C, Turecki G. Risk factors for suicide completion in major depression: a case-control study of impulsive and aggressive behaviors in males. Am J Psychiatry. In press. [DOI] [PubMed]
- 41.Brent DA, Perper JA, Moritz G, Baugher M, Roth C, Balach L, et al. Stressful life events, psychopathology, and adolescent suicide: a case control study. Suicide Life Threat Behav 1993;23:179-87. [PubMed]
- 42.Heikkinen ME, Henriksson MM, Isometsa ET, Marttunen MJ, Aro HM, Lonnqvist JK. Recent life events and suicide in personality disorders. J Nerv Ment Dis 1997;185:373-81. [DOI] [PubMed]
- 43.Heikkinen ME, Isometsa ET, Aro HM, Sarna SJ, Lonnqvist JK. Age-related variation in recent life events preceding suicide. J Nerv Ment Dis 1995;183:325-31. [DOI] [PubMed]
- 44.Rich CL, Warstadt GM, Nemiroff RA, Fowler RC, Young D, Warsradt GM. Suicide, stressors, and the life cycle. Am J Psychiatry 1991;148:524-7. [DOI] [PubMed]
- 45.Gould MS, Fisher P, Parides M, Flory M, Shaffer D. Psychosocial risk factors of child and adolescent completed suicide. Arch Gen Psychiatry 1996;53:1155-62. [DOI] [PubMed]
- 46.Foster T, Gillespie K, McClelland R, Patterson C. Risk factors for suicide independent of DSM-III-R axis I disorder. Case-control psychological autopsy study in Northern Ireland. Br J Psychiatry 1999; 175:175-9. [DOI] [PubMed]
- 47.Hagnell O, Rorsman B. Suicide in the Lundby study: a controlled prospective investigation of stressful life events. Neuropsychobiology 1980;6:319-32. [DOI] [PubMed]
- 48.Cavanagh JT, Owens DG, Johnstone EC. Life events in suicide and undetermined death in south-east Scotland: a case-control study using the method of psychological autopsy. Soc Psychiatry Psychiatr Epidemiol 1999;34:645-50. [DOI] [PubMed]
- 49.Fergusson DM, Woodward LJ, Horwood LJ. Risk factors and life processes associated with the onset of suicidal behaviour during adolescence and early adulthood. Psychol Med 2000;30:23-39. [DOI] [PubMed]
- 50.McCrae RR, Costa PT Jr. Personality trait structure as a human universal. Am Psychol 1997;52:509-16. [DOI] [PubMed]
- 51.Krueger RF, Caspi A, Moffitt TE. Epidemiological personology: the unifying role of personality in population-based research on problem behaviors. J Pers 2000;68:967-98. [DOI] [PubMed]
- 52.Cloninger CR. Temperament and personality. Curr Opin Neurobiol 1994;4:266-73. [DOI] [PubMed]
- 53.Furnham A. Personality and activity preference. Br J Soc Psychol 1981; 20:57-67.
- 54.Plomin R, Owen MJ, McGuffin P. The genetic basis of complex human behaviors. Science 1994;264:1733-9. [DOI] [PubMed]
- 55.Harkness A, Lilienfield S. Individual differences science for treatment planning: personality traits. Psychol Assess 1997;9:349-60.
- 56.Ebstein RP, Gritsenko I, Nemanov L, Frisch A, Osher Y, Belmaker RH. No association between the serotonin transporter gene regulatory region polymorphism and the Tridimensional Personality Questionnaire (TPQ) temperament of harm avoidance. Mol Psychiatry 1997;2:224-6. [DOI] [PubMed]
- 57.Kuhn KU, Meyer K, Nothen MM, Gansicke M, Papassotiropoulos A, Maier W. Allelic variants of dopamine receptor D4 (DRD4) and serotonin receptor 5HT2c (HTR2c) and temperament factors: replication tests. Am J Med Genet 1999;88:168-72. [PubMed]
- 58.Lesch KP, Merschdorf U. Impulsivity, aggression, and serotonin: a molecular psychobiological perspective. Behav Sci Law 2000;18:581-604. [DOI] [PubMed]
- 59.Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 2003;301:386-9. [DOI] [PubMed]
- 60.Strobel A, Gutknecht L, Rothe C, Reif A, Mossner R, Zeng Y, et al. Allelic variation in 5-HT1A receptor expression is associated with anxiety- and depression-related personality traits. J Neural Transm 2003;110:1445-53. [DOI] [PubMed]
- 61.Reif A, Lesch KP. Toward a molecular architecture of personality. Behav Brain Res 2003;139:1-20. [DOI] [PubMed]
- 62.Eysenck H. Genetic and environmental contributions to individual differences: the three major dimensions of personality. J Pers 1990;58:245-61. [DOI] [PubMed]
- 63.Livesley WJ, Jang KL, Vernon PA. Phenotypic and genetic structure of traits delineating personality disorder. Arch Gen Psychiatry 1998;55:941-8. [DOI] [PubMed]
- 64.Livesley WJ, Schroeder ML, Jackson DN, Jang KL. Categorical distinctions in the study of personality disorder: implications for classification. J Abnorm Psychol 1994;103:6-17. [DOI] [PubMed]
- 65.McCrae R, Costa P, editors. Personality in adulthood. New York: Guilford Press; 1990.
- 66.Cloninger CR, Przybeck TR, Svrakic DM, Wetzel RD. The temperament and character inventory (TCI): a guide to its development and use. St. Louis (MO): Center for Psychobiology of Personality, Washington University; 1994.
- 67.Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character. Arch Gen Psychiatry 1993;50:975-90. [DOI] [PubMed]
- 68.Costa P, McCrae R. From catalog to classification: Murray's needs and the five-factor model. J Pers Soc Psychol 1988;55:258-65.
- 69.Street S, Kromrey JD. Relationships between suicidal behavior and personality types. Suicide Life Threat Behav 1994;24:282-92. [PubMed]
- 70.Beautrais AL, Joyce PR, Mulder RT. Personality traits and cognitive styles as risk factors for serious suicide attempts among young people. Suicide Life Threat Behav 1999;29:37-47. [PubMed]
- 71.Rudd MD, Ellis TE, Rajab MH, Wehrly T. Personality types and suicidal behavior: an exploratory study. Suicide Life Threat Behav 2000;30:199-212. [PubMed]
- 72.Esposito C, Spirito A, Boergers J, Donaldson D. Affective, behavioral, and cognitive functioning in adolescents with multiple suicide attempts. Suicide Life Threat Behav 2003;33:389-99. [DOI] [PubMed]
- 73.Adam KS, Sheldon-Keller A, West M. Attachment organization and history of suicidal behavior in clinical adolescents. J Consult Clin Psychol 1996;64:64-72. [DOI] [PubMed]
- 74.Sourander A, Helstela L, Haavisto A, Bergroth L. Suicidal thoughts and attempts among adolescents: a longitudinal 8-year follow-up study. J Affect Disord 2001;63:59-66. [DOI] [PubMed]
- 75.Verona E, Patrick CJ, Joiner TE. Psychopathy, antisocial personality, and suicide risk. J Abnorm Psychol 2001;110:462-70. [DOI] [PubMed]
- 76.Sanches H. Risk factor model for suicide assessment and intervention. Prof Psychol Res Pr 2001;32:351-8.
- 77.Hukkanen R, Sourander A, Bergroth L. Suicidal ideation and behavior in children's homes. Nord J Psychiatry 2003;57:131-7. [DOI] [PubMed]
- 78.Caspi A, Moffitt TE, Newman DL, Silva PA. Behavioral observations at age 3 years predict adult psychiatric disorders. Longitudinal evidence from a birth cohort. Arch Gen Psychiatry 1996;53:1033-9. [DOI] [PubMed]
- 79.Engstrom G, Alling C, Gustavsson P, Oreland L, Traskman-Bendz L. Clinical characteristics and biological parameters in temperamental clusters of suicide attempters. J Affect Disord 1997;44:45-55. [DOI] [PubMed]
- 80.Catanzaro S. In: Joiner T, Rudd D, editors. Suicide science: expanding the boundaries. Boston: Kluwer; 2000.
- 81.Dean PJ, Range LM, Goggin WC. The escape theory of suicide in college students: testing a model that includes perfectionism. Suicide Life Threat Behav 1996;26:181-6. [PubMed]
- 82.Roberts BW, DelVecchio WF. The rank-order consistency of personality traits from childhood to old age: a quantitative review of longitudinal studies. Psychol Bull 2000;126:3-25. [DOI] [PubMed]
- 83.Evans J, Platts H, Liebenau A. Impulsiveness and deliberate self-harm: a comparison of “first-timers' and “repeaters'. Acta Psychiatr Scand 1996;93:378-80. [DOI] [PubMed]
- 84.Conner KR, Duberstein PR. Predisposing and precipitating factors for suicide among alcoholics: empirical review and conceptual integration. Alcohol Clin Exp Res 2004;28(5 Suppl):6S-17S. [DOI] [PubMed]
- 85.McCrae RR, Costa PT Jr, Pedroso de Lima M, Simoes A, Ostendorf F, Angleitner A, et al. Age differences in personality across the adult life span: parallels in five cultures. Dev Psychol 1999;35:466-77. [DOI] [PubMed]
- 86.Widiger TA, Anderson KG. Personality and depression in women. J Affect Disord 2003;74:59-66. [DOI] [PubMed]
- 87.Kempf EJ. Psychopathology. New York: Arno Press; 1976.
- 88.Nobre de Melo AL. Psiquiatria. Rio de Janeiro: Editora Guanabara; 1983.
- 89.Evenden JL. Varieties of impulsivity. Psychopharmacology (Berl) 1999;146:348-61. [DOI] [PubMed]
- 90.Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry 1999;156:181-9. [DOI] [PubMed]
- 91.Kausch O. Suicide attempts among veterans seeking treatment for pathological gambling. J Clin Psychiatry 2003;64:1031-8. [DOI] [PubMed]
- 92.Oquendo MA, Placidi GP, Malone KM, Campbell C, Keilp J, Brodsky B, et al. Positron emission tomography of regional brain metabolic responses to a serotonergic challenge and lethality of suicide attempts in major depression. Arch Gen Psychiatry 2003;60:14-22. [DOI] [PubMed]
- 93.Brent DA, Bridge J, Johnson BA, Connolly J. Suicidal behavior runs in families. A controlled family study of adolescent suicide victims. Arch Gen Psychiatry 1996;53:1145-52. [DOI] [PubMed]
- 94.Oquendo MA, Lizardi D, Greenwald S, Weissman MM, Mann JJ. Rates of lifetime suicide attempt and rates of lifetime major depression in different ethnic groups in the United States. Acta Psychiatr Scand 2004;110:446-51. [DOI] [PubMed]
- 95.Apter A, van Praag HM, Plutchik R, Sevy S, Korn M, Brown SL. Interrelationships among anxiety, aggression, impulsivity, and mood: A serotonergically linked cluster? Psychiatry Res 1990;32:191-9. [DOI] [PubMed]
- 96.Barratt E. Barratt impulsiveness scale. 1959.
- 97.Brezo J, Paris J, Tremblay R, Vitaro F, Hebert M, Turecki G. Personality traits as correlates of suicidal attempts and ideation in young adults. In press. [DOI] [PubMed]
- 98.Ernst C, Lalovic A, Lesage A, Seguin M, Tousignant M, Turecki G. Suicide and no axis I psychopathology. BMC Psychiatry 2004;4:7. [DOI] [PMC free article] [PubMed]
- 99.Fenton WS. Depression, suicide and suicide prevention in schizophrenia. Suicide Life Threat Behav 2000;30:34-49. [PubMed]
- 100.Sinclair JMA, Mullee MA, King EA, Baldwin DS. Suicide in schizophrenia: a retrospective case-control study of 51 suicides. Schizophr Bull 2004;30:803-11. [DOI] [PubMed]
- 101.Kim C, Lesage A, Seguin M, Lipp O, Vanier C, Turecki G. Patterns of comorbidity in male suicide completers. Psychol Med 2003;33:1299-309. [DOI] [PubMed]
- 102.Apter A, Kotler M, Sevy S, Plutchik R, Brown SL, Foster H, et al. Correlates of risk of suicide in violent and nonviolent psychiatric patients. Am J Psychiatry 1991;148:883-7. [DOI] [PubMed]
- 103.Foster T, Gillespie K, McClelland R. Mental disorders and suicide in Northern Ireland. Br J Psychiatry 1997;170:447-52. [DOI] [PubMed]
- 104.Henriksson MM, Hillevi MA, Marttunen MJ, Heikkinen ME, Isometsa ET, Kuoppasalmi KI, et al. Mental disorders and comorbidity in suicide. Am J Psychiatry 1993;150:935-40. [DOI] [PubMed]
- 105.Lesage AD, Boyer R, Grunberg F, Vanier C, Morissette R, Menard-Buteau C, et al. Suicide and mental disorders: a case-control study of young men. Am J Psychiatry 1994;151:1063-8. [DOI] [PubMed]
- 106.Hawton K, Houston K, Haw C, Townsend E, Harriss L. Comorbidity of axis I and axis II disorders in patients who attempted suicide. Am J Psychiatry 2003;160:1494-500. [DOI] [PubMed]
- 107.Suominen K, Henriksson M, Suokas J, Isometsa E, Ostamo A, Lonnqvist J. Mental disorders and comorbidity in attempted suicide. Acta Psychiatr Scand 1996;94:234-40. [DOI] [PubMed]
- 108.Shaffer D, Gould MS, Fisher P, Trautman P, Moreau D, Kleinman M, et al. Psychiatric diagnosis in child and adolescent suicide. Arch Gen Psychiatry 1996;53:339-48. [DOI] [PubMed]
- 109.Shafii M, Steltz-Lenarsky J, Derrick AM, Beckner C, Whittinghill JR. Comorbidity of mental disorders in the post-mortem diagnosis of completed suicide in children and adolescents. J Affect Disord 1988;15:227-33. [DOI] [PubMed]
- 110.Isometsa ET, Henriksson MM, Aro HM, Lonnqvist JK. Suicide in bipolar disorder in Finland. Am J Psychiatry 1994;151:1020-4. [DOI] [PubMed]
- 111.Conwell Y, Brent D. Suicide and aging. I: Patterns of psychiatric diagnosis. Int Psychogeriatr 1995;7:149-64. [DOI] [PubMed]
- 112.Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L. Age- and sex-related risk factors for adolescent suicide. J Am Acad Child Adolesc Psychiatry 1999;38:1497-505. [DOI] [PubMed]
- 113.Rifai AH, Reynolds CF, Mann JJ. Biology of elderly suicide. Suicide Life Threat Behav 1992;22:48-61. [PubMed]
- 114.Gould MS, Wallenstein S, Kleinman MH, O'Carroll P, Mercy J. Suicide clusters: an examination of age-specific effects. Am J Public Health 1990;80:211-2. [DOI] [PMC free article] [PubMed]
- 115.Prigerson HG, Slimack MJ. Gender differences in clinical correlates of suicidality among young adults. J Nerv Ment Dis 1999;187:23-31. [DOI] [PubMed]
- 116.Henriksson MM, Marttunen MJ, Isometsa ET, Heikkinen ME, Aro HM, Kuoppasalmi KI, et al. Mental disorders in elderly suicide. Int Psychogeriatr 1995;7:275-86. [DOI] [PubMed]
- 117.Bharucha AJ, Satlin A. Late-life suicide: a review. Harv Rev Psychiatry 1997;5:55-65. [DOI] [PubMed]
- 118.Conwell Y, Duberstein PR, Cox C, Herrmann J, Forbes N, Caine ED. Age differences in behaviors leading to completed suicide. Am J Geriatr Psychiatry 1998;6:122-6. [PubMed]
- 119.Isometsa ET, Heikkinen ME, Henriksson MM, Aro HM, Marttunen MJ, Lonnqvist JK. Parenthood, completed suicide and mental health. Arch Gen Psychiatry 1996;53:1061-2. [DOI] [PubMed]
- 120.Conwell Y, Duberstein PR, Cox C, Herrmann JH, Forbes NT, Caine ED. Relationships of age and axis I diagnoses in victims of completed suicide: a psychological autopsy study. Am J Psychiatry 1996;153:1001-8. [DOI] [PubMed]
- 121.Brent DA, Perper JA, Moritz G, Allman C, Friend A, Roth C, et al. Psychiatric risk factors for adolescent suicide: a case-control study. J Am Acad Child Adolesc Psychiatry 1993;32:521-9. [DOI] [PubMed]
- 122.Shafii M, Carrigan S, Whittinghill JR, Derrick A. Psychological autopsy of completed suicide in children and adolescents. Am J Psychiatry 1985;142:1061-4. [DOI] [PubMed]
- 123.Reynolds CF III, Dew MA, Frank E, Begley AE, Miller MD, Cornes C, et al. Effects of age at onset of first lifetime episode of recurrent major depression on treatment response and illness course in elderly patients. Am J Psychiatry 1998;155:795-9. [DOI] [PubMed]
- 124.Cassano GB, Akiskal HS, Savino M, Soriani A, Musetti L, Perugi G. Single episode of major depressive disorder. First episode of recurrent mood disorder or distinct subtype of late-onset depression? Eur Arch Psychiatry Clin Neurosci 1993;242:373-80. [DOI] [PubMed]
- 125.Angst J, Stassen HH, Gross G. In: Maneros A, Tsuang M, editors. Affective and schizoaffective disorders. Berlin: Springer; 1990.
- 126.Malone KM, Haas GL, Sweeney JA, Mann JJ. Major depression and the risk of attempted suicide. J Affect Disord 1995;34:173-85. [DOI] [PubMed]
- 127.Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA 2001;286:3089-96. [DOI] [PubMed]
- 128.Gladstone G, Parker G, Wilhelm K, Mitchell P, Austin MP. Characteristics of depressed patients who report childhood sexual abuse. Am J Psychiatry 1999;156:431-7. [DOI] [PubMed]
- 129.Johnson JG, Cohen P, Skodol AE, Oldham JM, Kasen S, Brook JS. Personality disorders in adolescence and risk of major mental disorders and suicidality during adulthood. Arch Gen Psychiatry 1999;56:805-11. [DOI] [PubMed]
- 130.Soloff PH, Lynch KG, Kelly TM. Childhood abuse as a risk factor for suicidal behavior in borderline personality disorder. J Personal Disord 2002;16:201-14. [DOI] [PubMed]
- 131.Grilo CM, Sanislow C, Fehon DC, Martino S, McGlashan TH. Psychological and behavioral functioning in adolescent psychiatric inpatients who report histories of childhood abuse. Am J Psychiatry 1999;156:538-43. [DOI] [PubMed]
- 132.Clarkin JF, Posner M. Defining the mechanisms of borderline personality disorder. Psychopathology 2005;38:56-63. [DOI] [PubMed]
- 133.Lieb K, Zanarini MC, Schmahl C, Linehan MM, Bohus M. Borderline personality disorder. Lancet 2004;364:453-61. [DOI] [PubMed]
- 134.Figueroa E, Silk KR. Biological implications of childhood sexual abuse in borderline personality disorder. J Personal Disord 1997;11:71-92. [DOI] [PubMed]
- 135.Seguin M, Lesage A, Turecki G, Daigle F, Guy A. (ed. Department of Health and Wellness, M. H. S. D.) Research project on deaths by suicide in New Brunswick between April 2002 and May 2003. 1-32 Government of New Brunswick; 2005.
- 136.Barraclough B, Bunch J, Nelson B, Sainsbury P. A hundred cases of suicide: clinical aspects. Br J Psychiatry 1974;125:355-73. [DOI] [PubMed]
- 137.Tsuang M. Risk of suicide in the relatives of schizophrenics, manics, depressives, and controls. J Clin Psychiatry 1983;44:396-400. [PubMed]
- 138.Powell J, Geddes J, Deeks J, Goldacre M, Hawton K. Suicide in psychiatric hospital in-patients. Risk factors and their predictive power. Br J Psychiatry 2000;176:266-72. [DOI] [PubMed]
- 139.Runeson BS. History of suicidal behaviour in the families of young suicides. Acta Psychiatr Scand 1998;98:497-501. [DOI] [PubMed]
- 140.Vijayakumar L, Rajkumar S. Are risk factors for suicide universal? A case-control study in India. Acta Psychiatr Scand 1999;99:407-11. [DOI] [PubMed]
- 141.Cheng AT, Chen TH, Chen CC, Jenkins R. Psychosocial and psychiatric risk factors for suicide. Case-control psychological autopsy study. Br J Psychiatry 2000;177:360-5. [DOI] [PubMed]
- 142.Roy A. Family history of suicide. Arch Gen Psychiatry 1983;40:971-4. [DOI] [PubMed]
- 143.Robins E, Schmidt EH, O'Neal P. Some interrelations of social factors and clinical diagnosis in attempted suicide: a study of 109 patients. Am J Psychiatry 1957;114:221-31. [DOI] [PubMed]
- 144.Woodruff RA, Clayton PJ, Guze SB. Suicide attempts and psychiatric diagnosis. Dis Nerv Syst 1972;33:617-21. [PubMed]
- 145.Murphy GE, Wetzel RD. Family history of suicidal behavior among suicide attempters. J Nerv Ment Dis 1982;170:86-90. [DOI] [PubMed]
- 146.Roy A. Relation of family history of suicide to suicide attempts in alcoholics. Am J Psychiatry 2000;157:2050-51. [DOI] [PubMed]
- 147.Johnson BA, Brent DA, Bridge J, Connolly J. The familial aggregation of adolescent suicide attempts. Acta Psychiatr Scand 1998; 97: 18-24. [DOI] [PubMed]
- 148.Kim CD, Seguin M, Therrien N, Riopel G, Chawky N, Lesage AD, et al. Familial aggregation of suicidal behaviour: a family study of male suicide completers from the general population. Am J Psychiatry 2005;162(5):1017-9. [DOI] [PubMed]
- 149.Baldessarini RJ, Hennen J. Genetics of suicide: an overview. Harv Rev Psychiatry 2004;12:1-13. [DOI] [PubMed]
- 150.Egeland JA, Sussex JN. Suicide and family loading for affective disorders. JAMA 1985;254:915-8. [PubMed]
- 151.Mitterauer B, Leibetseder M, Pritz WF, Sorgo G. Comparisons of psychopathological phenomena of 422 manic-depressive patients with suicide-positive and suicide-negative family history. Acta Psychiatr Scand 1988;77:438-42. [DOI] [PubMed]
- 152.Linkowski P, de Maertelaer V, Mendlewicz J. Suicidal behaviour in major depressive illness. Acta Psychiatr Scand 1985;72:233-8. [DOI] [PubMed]
- 153.Mattes JA, Fink M. A controlled family study of adopted patients with temper outbursts. J Nerv Ment Dis 1990;178:138-9. [DOI] [PubMed]
- 154.Mattes JA, Fink M. A family study of patients with temper outbursts. J Psychiatr Res 1987;21:249-55. [DOI] [PubMed]
- 155.Stewart MA, Leone L. A family study of unsocialized aggressive boys. Biol Psychiatry 1978;13:107-17. [PubMed]
- 156.Coccaro EF, Silverman JM, Klar HM, Horvath TB, Siever LJ. Familial correlates of reduced central serotonergic system function in patients with personality disorders. Arch Gen Psychiatry 1994;51:318-24. [DOI] [PubMed]
- 157.Coccaro EF, Bergeman CS, Kavoussi RJ, Seroczynski AD. Heritability of aggression and irritability: a twin study of the Buss-Durkee aggression scales in adult male subjects. Biol Psychiatry 1997;41:273-84. [DOI] [PubMed]
- 158.Coccaro EF, Bergeman CS, McClearn GE. Heritability of irritable impulsiveness: a study of twins reared together and apart. Psychiatry Res 1993;48:229-42. [DOI] [PubMed]
- 159.Brent DA, Oquendo M, Birmaher B, Greenhill L, Kolko D, Stanley B, et al. Peripubertal suicide attempts in offspring of suicide attempters with siblings concordant for suicidal behavior. Am J Psychiatry 2003;160:1486-93. [DOI] [PubMed]
- 160.Asberg M, Traskman L, Thoren P. 5-HIAA in the cerebrospinal fluid. A biochemical suicide predictor? Arch Gen Psychiatry 1976;33:1193-7. [DOI] [PubMed]
- 161.Coccaro EF. Central serotonin and impulsive aggression. Br J Psychiatry Suppl 1989;8:52-62. [PubMed]
- 162.New AS, Trestman RL, Mitropoulou V, Benishay DS, Coccaro E, Silverman J, et al. Serotonergic function and self-injurious behavior in personality disorder patients. Psychiatry Res 1997;69:17-26. [DOI] [PubMed]
- 163.Davidson RJ, Putnam KM, Larson CL. Dysfunction in the neural circuitry of emotion regulation–a possible prelude to violence. Science 2000;289:591-4. [DOI] [PubMed]
- 164.Mann JJ, Huang Y, Underwood MD, Kassir SA, Oppenheim S, Kelly TM, et al. A serotonin transporter gene promoter polymorphism (5-HTTLPR) and prefrontal cortical binding in major depression and suicide. Arch Gen Psychiatry 2000;57:729-38. [DOI] [PubMed]
- 165.Stockmeier CA, Shapiro LA, Dilley GE, Kolli TN, Friedman L, Rajkowska G. Increase in serotonin-1A autoreceptors in the midbrain of suicide victims with major depression-postmortem evidence for decreased serotonin activity. J Neurosci 1998;18:7394-401. [DOI] [PMC free article] [PubMed]
- 166.Arango V, Underwood MD, Gubbi AV, Mann JJ. Localized alterations in pre- and postsynaptic serotonin binding sites in the ventrolateral prefrontal cortex of suicide victims. Brain Res 1995;688:121-33. [DOI] [PubMed]
- 167.Turecki G, Brière R, Dewar K, Antonetti T, Lesage A, Séguin M, et al. Prediction of level of serotonin 2A receptor binding by serotonin receptor 2A genetic variation in postmortem brain samples from subjects who did or did not commit suicide. Am J Psychiatry 1999;156:1456-8. [DOI] [PubMed]
- 168.Hrdina PD, Demeter E, Vu TB, Sotonyi P, Palkovits M. 5-HT uptake sites and 5-HT2 receptors in brain of antidepressant-free suicide victims/depressives: increase in 5-HT2 sites in cortex and amygdala. Brain Res 1993;614:37-44. [DOI] [PubMed]
- 169.Davidson RJ, Irwin W. The functional neuroanatomy of emotion and affective style. Trends Cogn Sci 1999;3:11-21. [DOI] [PubMed]
- 170.Davidson RJ, Jackson DC, Kalin NH. Emotion, plasticity, context, and regulation: perspectives from affective neuroscience. Psychol Bull 2000;126:890-909. [DOI] [PubMed]
- 171.Cheng AT, Mann AH, Chan KA. Personality disorder and suicide. A case-control study. Br J Psychiatry 1997;170:441-6. [DOI] [PubMed]


