Abstract
Chemokines (CK) are potent leukocyte activators and chemoattractants and aid in granuloma formation, functions critical for the immune response to Mycobacterium tuberculosis. We hypothesized that infection of alveolar macrophages (AM) with different strains of M. tuberculosis elicits distinct profiles of CK, which could be altered by human immunodeficiency virus (HIV) infection. RANTES, macrophage inflammatory protein-1α (MIP-1α), and MIP-1β were the major β-CK produced in response to M. tuberculosis infection. Virulent M. tuberculosis (H37Rv) induced significantly less MIP-1α than did the avirulent strain (H37Ra), while MIP-1β and RANTES production was comparable for both strains. MIP-1α and MIP-1β were induced by the membrane, but not cytosolic, fraction of M. tuberculosis. M. tuberculosis-induced CK secretion was partly dependent on tumor necrosis factor alpha (TNF-α). AM from HIV-infected individuals produced less TNF-α and MIP-1β than did normal AM in response to either M. tuberculosis strain. We tested the functional significance of decreased β-CK secretion by examining the ability of β-CK to suppress intracellular growth of M. tuberculosis. MIP-1β and RANTES suppressed intracellular growth of M. tuberculosis two- to threefold, a novel finding. Thus, β-CK contribute to the innate immune response to M. tuberculosis infection, and their diminution may promote the intracellular survival of M. tuberculosis.
Alveolar macrophages (AM) constitute the initial defense against mycobacteria inhaled into the lung. Resident AM phagocytose and kill arriving mycobacteria, which may survive and multiply intracellularly (10). Successful parasitization of AM depends on the ability of Mycobacterium tuberculosis to evade or manipulate the innate immune response. Persistent infection is contained by recruitment and activation of circulating leukocytes to the nidus of infection, providing fresh phagocytes and T cells to lyse infected cells and secrete Th1 cytokines (10, 11). Infection of AM with M. tuberculosis induces release of multiple factors, including the early inflammatory cytokines tumor necrosis factor alpha (TNF-α) and interleukin-1β (IL-1β), which have autocrine activating effects and promote the recruitment of circulating leukocytes (19, 22).
We hypothesized that M. tuberculosis infection of AM evokes local production of specific chemokines (CK), potent chemotactic and activating factors for leukocytes that are influenced by M. tuberculosis virulence and by human immunodeficiency virus (HIV) infection. The β-CK, including macrophage inflammatory protein-1α (MIP)-1α, MIP-1β, RANTES (for regulated upon activation, normal T cell expressed and secreted), and monocyte chemotactic protein-1 (MCP-1), promote chemotaxis and/or transendothelial migration of mononuclear cells (29, 31). MIP-1α, MIP-1β, and RANTES induce activation and proliferation of T cells (32) and of macrophages (Mφ) (9, 20), and MIP-1α promotes Th1 cell differentiation (15, 16). These β-CK, particularly RANTES, play significant roles in granuloma formation (7). The α-CK IP-10 is a potent T-cell chemoattractant (1, 29). The ability of CK to attract and activate T cells and monocytes suggests that CK may have a role in modulating immune responses to M. tuberculosis infection. Poor granuloma formation is a characteristic finding in M. tuberculosis infection in advanced HIV type 1 disease (12, 24, 25) and suggests that β-CK production may be deficient. Virulence or host-associated differences in M. tuberculosis-induced CK production may also contribute to failure to contain the infection.
We compared the in vitro abilities of avirulent and virulent M. tuberculosis to induce CK production in AM obtained from healthy control and HIV-infected individuals. Although there was wide variation in M. tuberculosis-induced CK production within these two groups, we found a reduced ability of AM from HIV-infected individuals to produce MIP-1β and, to a lesser extent, RANTES in response to either avirulent (H37Ra) or virulent (H37Rv) M. tuberculosis. We found that M. tuberculosis-induced β-CK expression was partly regulated by TNF-α, secretion of which was also attenuated in AM from HIV-infected individuals.
Pursuing the functional significance of diminished M. tuberculosis-induced β-CK secretion, we hypothesized that β-CK, rather than acting solely as leukocyte chemoattractants, participate in regulating the Mφ response to M. tuberculosis. Recently, MIP-1α, MIP-1β, and RANTES were reported to increase phagocytosis and killing of another intracellular organism, Trypanosoma cruzi (35). We found that MIP-1β and RANTES suppress growth of M. tuberculosis within Mφ. This is the first report that β-CK inhibit intracellular growth of M. tuberculosis. Therefore, an attenuated β-CK response to M. tuberculosis, as we found in AM from HIV-infected individuals, could affect this aspect of the innate immune response to M. tuberculosis.
MATERIALS AND METHODS
Subjects.
Institutional Review Board approval was obtained for performance of these studies. Healthy control volunteers were recruited from the medical center community, while HIV-infected individuals without concomitant illnesses were recruited from the Immunodeficiency Clinic of Boston Medical Center. Several of the HIV-infected individuals and one of the normal volunteers were smokers. HIV-infected individuals had CD4 cell counts that ranged from 100 to 400 cells/dl.
Preparation of mycobacterial stocks.
Titers of stocks were determined by serial dilution, culture on 7H10 plates, and colony counting at 4 weeks. The stocks were tested by Limulus amebocyte lysate QCL-1000 assay (BioWhittaker, Walkersville, Md.) to ascertain that the stock was free of endotoxin, courtesy of Matthew Fenton (Boston University).
Preparation and infection of human Mφ.
Bronchoalveolar lavage (BAL) was performed according to a protocol recommended by the American Thoracic Society (3). Recovered BAL fluid was filtered through a sterile single layer of gauze, centrifuged for 10 min at 500 × g, and washed twice with RPMI (Mediatech, Reston, Va.). Cells were resuspended in RPMI with 10% fetal calf serum (Sigma, St. Louis, Mo.) and cefotaxime (50 μg/ml) (Calbiochem, La Jolla, Calif.) to a concentration of 200,000 to 400,000 cells/ml and incubated at 37°C in polystyrene dishes. After 18 to 24 h, medium and nonadherent cells were aspirated, and fresh medium was added to the same concentration of cells to minimize the artifact of adhesion-induced CK expression (17). H37Ra or H37Rv was added to plates at M. tuberculosis-to-cell ratios of approximately 20:1. In certain experiments, neutralizing antibodies to TNF-α, gamma interferon (IFN-γ), or IL-1β were added at 2 μg/ml. Supernatants were harvested after 48 h, frozen, and later assayed by enzyme-linked immunosorbent assay (ELISA) for CK. In other experiments, nonviable membrane or cytosolic fractions of H37Rv or of lipoarabinomannan (TB Research Materials and Vaccine Testing Contract, Colorado State University, Fort Collins) were added instead of intact M. tuberculosis. Membrane and cytosolic fractions were free of cell wall components.
Assessment of M. tuberculosis intracellular growth.
AM were isolated and incubated overnight as described above. H37Rv was added at a multiplicity of infection of 10:1, or 106 organisms per 105 AM. After 4 h of continuous rocking at 37°C, cells were washed, and either control or neutralizing antibody to MIP-1α, MIP-1β, or RANTES at 10 μg/ml was added. After 6 days of incubation at 37°C, Mφ were lysed with 0.25% sodium dodecyl sulfate for 10 min at 37°C, and then 50 μl of 20% bovine serum albumin was added. Two dilutions of lysates (1:10 and 1:100) were prepared in sterile saline solution with 0.85% Tween 80 and inoculated onto 7H11 agar plates. Mycobacterial growth was assessed by counting the number of CFU present at 3 weeks.
ELISAs for CK.
Antigenic TNF-α, MIP-1α, MIP-1β, RANTES, MCP-1, and IP-10 in AM supernatants were quantitated by using a modification of a double-ligand ELISA method, as previously described (8). In neutralizing-antibody experiments and in M. tuberculosis fraction studies, ELISA kits from R & D (Minneapolis, Minn.) were utilized. Cytokine data were expressed as the means of duplicate readings in nanograms per milliliter per million cells.
Statistics.
The Statview 4.51 software package (Abacus Concepts Inc., Berkeley, Calif.) was used for statistical calculations. The Mann-Whitney U test was used to compare data from unpaired groups, while the Wilcoxon signed rank test was used to compare data from paired groups. Student's t test was used if the experimental numbers did not allow nonparametric testing. The Spearman rank correlation test was used to analyze associations between cytokines.
RESULTS
H37Rv induces significantly less MIP-1α than does H37Ra.
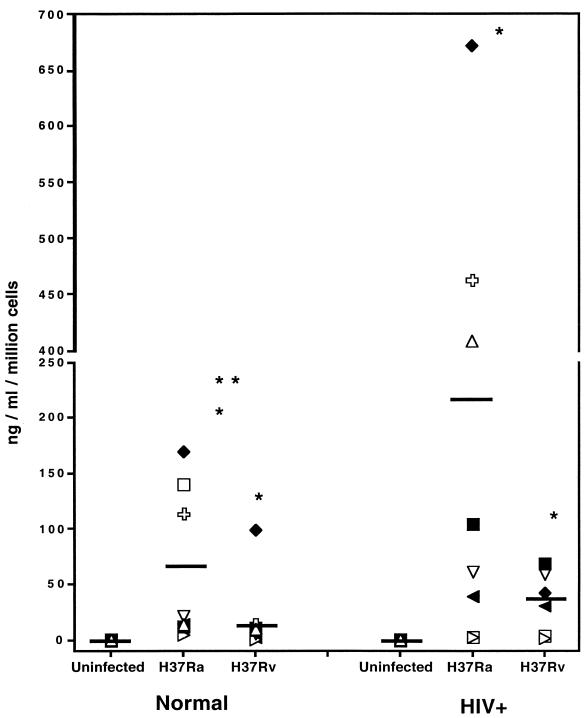
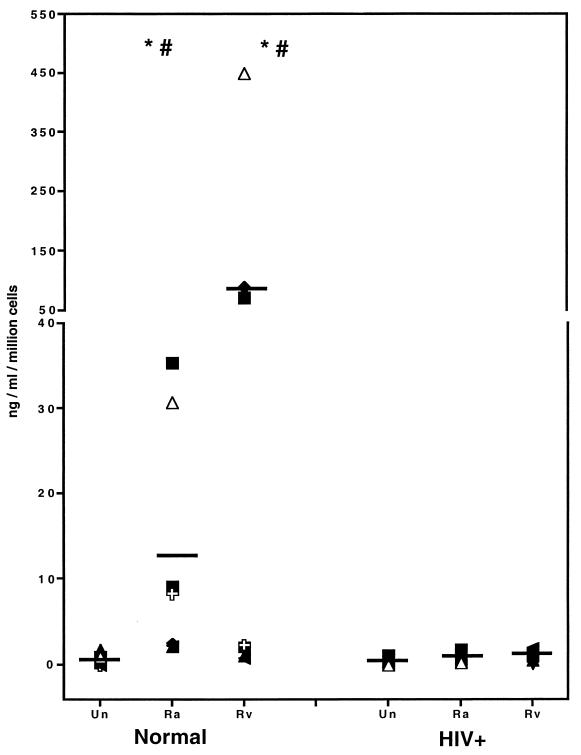
Secretion of MIP-1α from normal AM, shown in Fig. 1, was significantly induced by both H37Ra (61 ± 24; P = 0.012) (all values shown refer to mean CK concentration, in nanograms per milliliter per million cells, ± standard error of the mean) and H37Rv (19.9 ± 11.4; P = 0.012) compared to uninfected AM (0.02 ± 0.01). However, induction of MIP-1α by H37Rv was significantly lower than that by H37Ra (a threefold difference) (P = 0.036). AM from HIV-infected individuals also produced significant amounts of MIP-1α when infected with H37Ra (219 ± 91; P = 0.0117) and H37Rv (34 ± 11; P = 0.0277) compared to control AM (0.06 ± 0.02; P = 0.02). AM from the HIV-infected group tended to produce less MIP-1α in response to H37Rv than in response to H37Ra (P = 0.075) (a sixfold difference), but did not achieve statistical significance.
FIG. 1.
Less induction of MIP-1α by H37Rv than by H37Ra. AM from normal (n = 8) and HIV-infected (n = 8) individuals were infected with M. tuberculosis for 72 h at 37°C, and the resulting supernatants were assayed by ELISA for MIP-1α. Both H37Ra and H37Rv induced significant quantities of MIP-1α compared to uninfected control AM. H37Rv induced significantly less MIP-1α production than did H37Ra in normal AM. Single asterisks indicate a significant difference compared to uninfected AM; double asterisks indicate a significant difference compared to H37Ra-infected AM from HIV-positive individuals.
M. tuberculosis-induced MIP-1β secretion is reduced in AM from HIV-infected individuals.
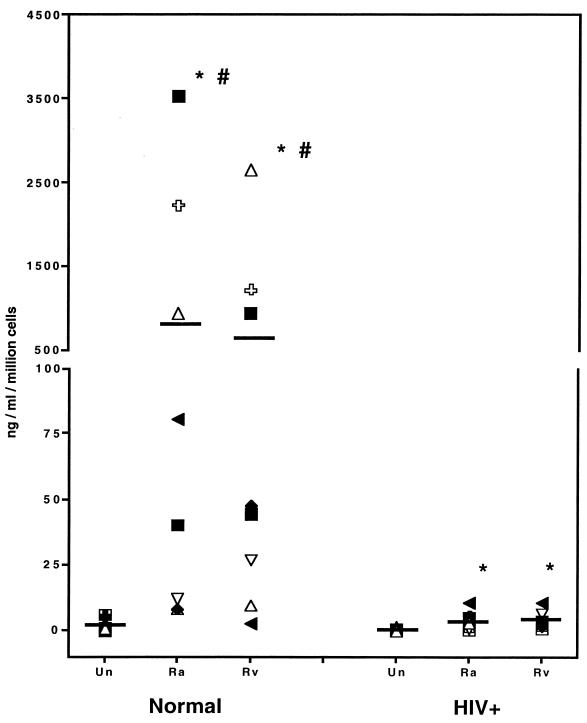
Infection of normal AM with H37Ra induced significant quantities of MIP-1β (855 ± 471; P = 0.012), as did infection with H37Rv (618 ± 337; P = 0.012), compared to uninfected AM (1.5 ± 0.8) (Fig. 2). There was no significant difference in MIP-1β induction between H37Ra and H37Rv (P = 0.89). Similarly, AM from HIV-infected individuals also produced significant amounts of MIP-1β when infected with H37Ra (3.5 ± 1.2; P = 0.012) or H37Rv (4.0 ± 1.5; P = 0.028) compared to uninfected AM (0.2 ± 0.1). However, AM from normal individuals produced significantly more MIP-1β than did AM from HIV-infected individuals in response to infection with H37Ra (855 ± 471 versus 3.5 ± 1.2; P = 0.002) or H37Rv (618 ± 337 versus 4.0 ± 1.5; P = 0.01) (more than 200- and 100-fold differences, respectively). MIP-1β secretion tended to be more pronounced than that of MIP-1α in normal AM, without a direct correlation between the two CK.
FIG. 2.
AM from HIV-positive individuals produce less MIP-1β than control AM in response to M. tuberculosis. Supernatants of AM from normal (n = 8) and HIV-infected (n = 8) individuals were infected with M. tuberculosis as described for Fig. 1 and assayed by ELISA for MIP-1β. Induction of MIP-1β in normal AM was comparable for both H37Ra and H37Rv. AM from the HIV group produced significantly less MIP-1β than did normal AM in response to both H37Ra and H37Rv. Asterisks indicate a significant difference compared to uninfected (Un) AM. Number signs indicate a significant difference compared to the corresponding condition for AM from HIV-infected individuals.
Infection of AM with M. tuberculosis induces production of RANTES.
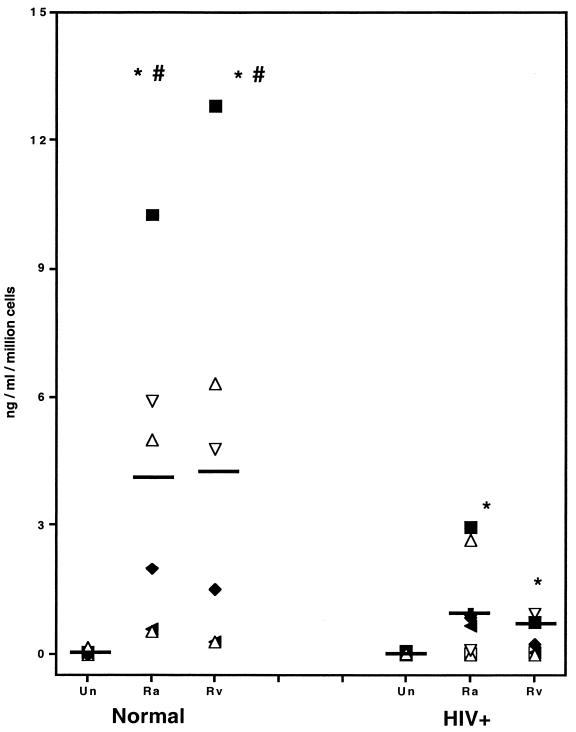
Secretion of RANTES in response to M. tuberculosis in both groups largely paralleled that of MIP-1β. H37Ra induced significant increases in RANTES secretion (4.0 ± 1.5; P = 0.028), as did H37Rv (4.4 ± 1.7; P = 0.028), compared to uninfected AM (0.04 ± 0.03) (Fig. 3). AM from HIV-infected individuals also produced statistically significant amounts of RANTES when infected with H37Ra (1.0 ± 0.4; P = 0.018) or with H37Rv (0.4 ± 0.2; P = 0.043) compared to uninfected AM (0.02 ± 0.01). Although AM from normal individuals appeared to produce 4- to 10-fold more RANTES than did those from HIV-infected individuals in response to infection with H37Ra (P = 0.052) or H37Rv (P = 0.055), these differences did not achieve statistical significance. The level of M. tuberculosis-induced RANTES was substantially less than those of MIP-1α and MIP-1β. However, RANTES is bioactive at a concentration 1 log unit lower than the other β-CK (29, 32). There was no direct correlation between secretion of RANTES and other cytokines.
FIG. 3.
Infection of AM with M. tuberculosis induces production of RANTES. RANTES in supernatants from AM infected as described for Fig. 1 was assayed by ELISA. Although both H37Ra and H37Rv induced significant quantities of RANTES in AM from normal subjects (n = 6) and from HIV-infected individuals (n = 8), AM from the latter group produced significantly less RANTES than did normal AM. Asterisks indicate a significant difference compared to uninfected (Un) AM, and number signs indicate a P value of 0.055 (not statistically significant).
In vitro M. tuberculosis infection of AM induces production of other CK.
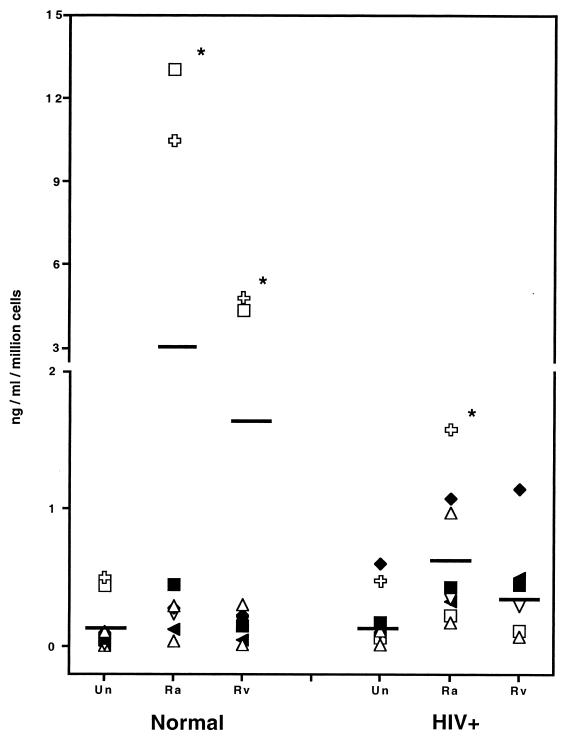
Statistically significant increases in MCP-1 were induced by infection of AM from control individuals with both H37Ra (3.1 ± 1.9; P = 0.0117) and H37Rv (1.3 ± 0.7; P = 0.0117), compared to uninfected control AM (0.16 ± 0.07). Significant increases in MCP-1 secretion were also found with AM from HIV-infected individuals infected with H37Ra (0.65 ± 0.18; P = 0.0115), but not those infected with H37Rv (0.43 ± 0.16; P = 0.17), compared to uninfected HIV AM (0.21 ± 0.08) (Fig. 4). However, the quantity of MCP-1 detected after 48 h of infection was less than what is generally believed to biologically active (21, 33).
FIG. 4.
Infection of AM with M. tuberculosis induces production of MCP-1. MCP-1 in supernatants from AM infected as described for Fig. 1 was assayed by ELISA. Statistically significant increases in MCP-1 were seen with H37Ra and H37Rv in control AM. Only H37Ra induced statistically significant increases in MCP-1 in AM from HIV-infected individuals. Asterisks indicate a significant difference compared to uninfected (Un) AM.
AM from normal control individuals produced IP-10 significantly in response to H37Ra (13.6 ± 6.2; P = 0.028) and to H37Rv (102 ± 71; P = 0.028) compared to uninfected AM (0.6 ± 0.2) (Fig. 5). AM from normal individuals produced significantly more IP-10 than did AM from HIV-infected individuals in response to H37Ra (13.6 ± 6.2 versus 0.7 ± 0.2, respectively; P = 0.0039) or H37Rv (102 ± 71 versus 0.8 ± 0.3, respectively; P = 0.045). In AM from HIV-infected individuals, H37Ra and H37Rv failed to produce IP-10 in quantities distinguishable from those in uninfected AM (0.4 ± 0.2; P > 0.05).
FIG. 5.
Infection of control AM with M. tuberculosis induces production of IP-10. IP-10 in supernatants from AM infected as described for Fig. 1 was assayed by ELISA. Infection with either H37Ra or H37Rv induced significant quantities of IP-10 in control AM compared to uninfected AM but not compared to AM from HIV-infected individuals. Asterisks indicate a significant difference compared to uninfected (Un) AM, and number signs indicate a significant difference between control AM and AM from HIV-infected individuals.
Mycobacterial membrane fraction induces MIP-1α and MIP-1β production by AM.
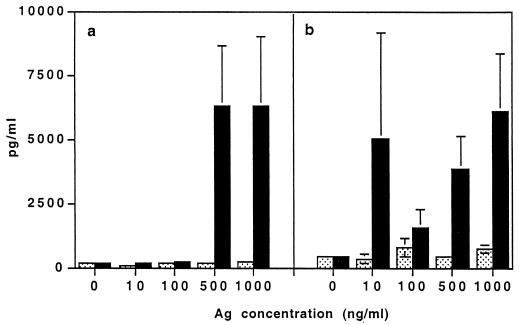
We sought to determine what component of M. tuberculosis induced MIP-1α and MIP-1β production by stimulating normal AM with soluble nonviable membrane or cytosolic extracts of H37Rv. We found that membrane extracts induced secretion of both of these β-CK, while cytosolic extracts did not (Fig. 6). In two experiments, we found that lipoarabinomannan, a component of the cell wall, in concentrations of up to 1,000 ng/ml, did not significantly induce these CK (data not shown). Thus, soluble mycobacterial components associated with the bacterial membrane were sufficient to induce CK production.
FIG. 6.
The mycobacterial membrane fraction induces AM production of MIP-1α and MIP-1β. AM from normal individuals were treated with either soluble membrane (black bars) or cytosolic (stippled bars) fractions of H37Rv for 72 h at 37°C. Supernatants were assayed by ELISA for MIP-1α (a) and MIP-1β (b) (n = 5). Both of these β-CK were induced by the membrane fraction but not by the cytosolic fraction, especially at higher doses. Error bars indicate standard errors of the means. Ag, antigen.
Production of β-CK is partly dependent on M. tuberculosis-induced TNF-α.
We sought to determine if M. tuberculosis-related CK production was regulated by other M. tuberculosis-induced cytokines, such as TNF-α, IFN-γ, and IL-1β, which are known inducers of β-CK (6, 27). Neutralizing antibodies to TNF-α added to H37Ra-infected AM cultures significantly reduced, but did not completely block, MIP-1α and MIP-1β (P = 0.046) secretion compared to control antibody-treated, H37Ra-infected AM (Table 1). In a limited number of experiments we found that M. tuberculosis-induced MIP-1α and MIP-1β secretion was not dependent on either IFN-γ or IL-1β, while, as expected, IP-10 was IFN-γ dependent (data not shown). Reduction of IP-10 in the presence of neutralizing antibody to IFN-γ demonstrated that the quantity of neutralizing antibody added to cultures was sufficient. The partial blockade of MIP-1α and MIP-1β secretion by anti-TNF-α suggested that other mechanisms might be operative in promoting secretion of these β-CK. Thus, TNF-α has a significant, but not the only, role in promoting secretion of MIP-1α and MIP-1β in response to M. tuberculosis infection.
TABLE 1.
TNF-α helps regulate M. tuberculosis-induced MIP-1α and MIP-1βa
| β-CK | Expt | Concn (pg/ml) with:
|
|
|---|---|---|---|
| H37Ra + control antibody | H37Ra + anti-TNF-α | ||
| MIP-1α | 1 | 70 | 15 |
| 2 | 1,941 | 397 | |
| 3 | 3,606 | 1,494 | |
| 4 | 13,726 | 1,758 | |
| 5 | 4,580 | 3,670 | |
| 6 | 61,775 | 4,190 | |
| Mean | 14,283 | 1,921 | |
| SEM | 9,692 | 692 | |
| MIP-1β | 1 | 3,191 | 4,157 |
| 2 | 25,554 | 16,920 | |
| 3 | 14,389 | 6,503 | |
| 4 | 25,654 | 6,899 | |
| 5 | 8,364 | 6,141 | |
| 6 | 18,611 | 9,811 | |
| Mean | 15,960 | 8,405 | |
| SEM | 3,725 | 1,858 | |
AM were infected with H37Ra in the presence of either 2 mg of control antibody or 2 μg of neutralizing anti-TNF-α per ml, and after 72 h supernatants were assayed by ELISA for MIP-1α or MIP-1β. Neutralization of TNF-α significantly reduced M. tuberculosis-induced production of both of these β-CK, in both cases there is a significant difference compared to isotype control antibody-treated cells.
TNF-α production in response to M. tuberculosis infection.
AM from HIV-infected individuals produced significantly less TNF-α than did control AM in response to H37Ra (7.1 ± 53 versus 140 ± 63; P = 0.419) (Table 2). There was no significant difference in the ability of H37Ra to induce TNF-α compared to H37Rv. MIP-1β, but not MIP-1α, production correlated with TNF-α secretion when control and HIV values were considered together (r = 0.643; P = 0.0198).
TABLE 2.
Attenuated TNF-α production in response to M. tuberculosis infection by AM from HIV-infected individualsa
| AM | TNF-α, mean ± SEM (ng/ml/million cells)
|
||
|---|---|---|---|
| Uninfected | H37Ra infected | H37Rv infected | |
| Control | 0.1 ± 0.05 | 140 ± 63 | 117 ± 53 |
| HIV positive | 0.1 ± 0.04 | 7.1 ± 5.7b | 0.8 ± 0.4 |
AM were infected as described for Fig. 1, and supernatants were assayed by ELISA for TNF-α.
Significantly different from control value.
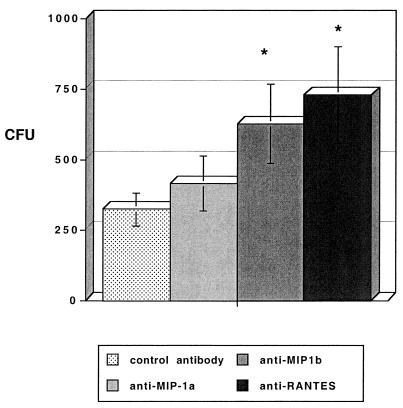
The β-CK MIP-1β and RANTES suppress intracellular growth of M. tuberculosis.
Growth of H37Rv within AM was significantly augmented by neutralizing antibodies to either MIP-1β (mean CFU ± standard error of the mean, 626 ± 140; P = 0.0207) or RANTES (729 ± 172; P = 0.0029) compared to M. tuberculosis-infected AM treated with control antibody (323 ± 58) (Fig. 7). Neutralizing antibody to MIP-1α did not significantly increase intracellular growth of H37Rv cells (414 ± 98; P = 0.593) relative to control antibody.
FIG. 7.
MIP-1β and RANTES suppress intracellular growth of M. tuberculosis. AM from control individuals (n = 11) were infected for 4 h with H37Rv and washed, and either isotype control or neutralizing antibodies to MIP-1α, MIP-1β, or RANTES were added. After 6 days of culture, cells were lysed and cultured on Middlebrook 7H11 agar for 21 days, and the number of CFU was counted at 21 days. Neutralization of MIP-1β or RANTES induced significant growth enhancement of M. tuberculosis within AM compared to control antibody-treated AM Asterisks indicate a significant difference compared to the isotype control. Error bars indicate standard errors of the means.
DISCUSSION
We examined specific differences in CK induction by AM from control and HIV-infected individuals challenged with avirulent and virulent M. tuberculosis strains. Although there was wide variation in β-CK production by AM from both groups, MIP-1α, MIP-1β, and RANTES were the predominant β-CK induced by infection with M. tuberculosis. We found that virulent M. tuberculosis induced significantly less MIP-1α than did avirulent M. tuberculosis in normal AM. However, AM from HIV-infected individuals produced significantly less MIP-1β and RANTES than did AM from controls. Induction of MIP-1α and MIP-1β was related to the membrane, not cytosolic, fraction of M. tuberculosis. Secretion of M. tuberculosis-induced MIP-1α and MIP-1β was significantly inhibited, but clearly not abolished, by neutralizing antibody to TNF-α. Our data also demonstrated that MIP-1β and RANTES inhibited the intracellular growth of M. tuberculosis, a novel finding.
We found that biologically significant quantities of both α- and β-CK were induced by M. tuberculosis infection of human AM. Specifically, IP-10 was induced among the former, while MIP-1α, MIP-1β, and RANTES were induced among the β-CK. Although M. tuberculosis-induced MCP-1 secretion did reach statistically significant levels, the quantities produced were biologically of far less significance than those of the other β-CK secreted (21, 33). Others have reported that in vitro M. tuberculosis infection of monocytoid and other cells is accompanied by secretion of both α- and β-CK. Murine Mφ infected in vitro with M. tuberculosis display rapid induction of mRNAs for IP-10, MIP-1α, MIP-2, and MCP-1 (28). M. tuberculosis infection of AM induces production of mRNAs and proteins for MCP-1, MIP-1α, RANTES, MCP-1, and IL-8 (30). BAL and pleural fluid from individuals with M. tuberculosis infection have increased levels of RANTES and MCP-1 compared to those from healthy individuals (10, 18). The low level of M. tuberculosis-induced MCP-1 secretion found in our study underscores recent findings in mouse models of granuloma formation, indicating that MIP-1α and RANTES are important in fostering a Th1-type response, while MCP-1 is more prominent in promoting Th2 responses (7, 15, 16).
We found strain- and host-related differences in M. tuberculosis induction of β-CK. The virulent M. tuberculosis strain H37Rv induced significantly less MIP-1α production than did the avirulent M. tuberculosis strain H37Ra. In contrast, the secretion of MIP-1β and RANTES was not significantly different for AM infected by H37Ra or H37Rv. AM from HIV-infected subjects showed a reduced ability to produce IP-10, MIP-1β, and, in most instances, RANTES compared to normal AM. M. tuberculosis-induced MIP-1α secretion by AM from HIV-infected individuals did not differ from that of the control group. MIP-1β production was more than 100-fold (P = 0.01) and 200-fold (P = 0.02) greater in AM from normal subjects than in those from HIV-infected individuals in response to H37Rv and H37Ra, respectively. Our study is the first to demonstrate the differential ability of M. tuberculosis strains to elicit specific profiles of CK secretion and the reduced ability of AM from HIV-infected individuals to produce specific CK.
M. tuberculosis-induced CK secretion appears to be regulated by a complex interplay of host and infecting-organism determinants. We determined that β-CK were elicited in response to soluble M. tuberculosis membrane antigens rather than by the cytosolic fraction. The mycobacterial cell wall component lipoarabinomannan (4), which has been reported to induce secretion of IL-8 in monocytes (28), did not elicit CK secretion in AM. Since lipoarabinomannan binds the Mφ mannose receptor (10) and CD14 (26), engagement of other specific cell surface adhesion molecules for M. tuberculosis may lead to β-CK secretion. We have recently found that engagement of AM Toll receptors 2 and 4, which both bind M. tuberculosis (23), by a heat-stable soluble mycobacterial cell wall component can elicit the secretion of β-CK (14). Since mycobacterial components alone can elicit secretion of these β-CK, live M. tuberculosis is not necessary for this effect. Thus, M. tuberculosis elicits secretion of β-CK through engagement of surface (membrane or cell wall) components rather than as a result of AM exposure to cytosolic components through killing of M. tuberculosis.
We found that the regulation of M. tuberculosis-induced β-CK secretion was significantly, but not exclusively, dependent on TNF-α, which is itself induced by M. tuberculosis (19). Several cytokines, including IFN-γ, IL-1β, and TNF-α, can induce production of β-CK in a variety of cells (5, 6). We found that the addition of neutralizing antibody to TNF-α significantly reduced H37Ra-induced MIP-1α and MIP-1β secretion. AM from HIV-infected individuals produced significantly less TNF-α than controls in this in vitro system. Others have reported significantly attenuated TNF-α mRNA in AM infected with HIV following lipopolysaccharide stimulation (34). We found a statistical correlation between M. tuberculosis-induced TNF-α and MIP-1β production. It is possible that attenuated TNF-α production may be partly responsible for the reduced β-CK secretion observed in AM from HIV-infected individuals.
There are clearly additional mechanisms beyond TNF-α in determining M. tuberculosis-induced β-CK secretion. Secretion of MIP-1α and MIP-1β was not completely blocked by antibody to TNF-α, which may reflect incomplete neutralization, induction by other cytokines, direct induction of these β-CK by M. tuberculosis, or release of preformed β-CK. Neutralizing antibodies to IL-1β and IFN-γ failed to block secretion of MIP-1α and MIP-1β, although anti-IFN-γ did block IP-10, as expected. We have recently found that AM do contain intracellular stores of preformed β-CK, which may be released in response to infection with M. tuberculosis (unpublished data). Thus, M. tuberculosis induces β-CK secretion through TNF-α-dependent and -independent mechanisms.
We subsequently examined the functional impact of β-CK production in influencing the intracellular survival of M. tuberculosis. We found that neutralization of MIP-β and RANTES significantly augmented intracellular growth of H37Rv within AM. Although the effect observed was moderate in this in vitro system, the magnitude of the response may reflect incomplete neutralization despite the high concentration of neutralizing antibody used, variations in CK receptor expression on AM, or simply that the effect of any single β-CK is modest. Our report is the first description of β-CK suppression of intracellular M. tuberculosis growth. These findings are particularly significant since we also found that AM from HIV-infected individuals produced significantly less MIP-1β and RANTES in response to M. tuberculosis than control AM. We speculate that the relative ability to produce these β-CK may constitute a host susceptibility factor or could play a role in the defective granuloma formation seen in HIV-infected individuals (12, 24, 25).
There are several potential mechanisms by which β-CK may influence the intracellular growth of M. tuberculosis. MIP-1α, MIP-1β, and RANTES activate Mφ, causing tyrosine phosphorylation of multiple proteins within minutes (20). MIP-1α induces Mφ production of TNF-α, IL-1β, and IL-6, while MIP-1β can modulate MIP-1α-induced TNF-α production (9). Recent reports indicate that MIP-1α, MIP-1β, and particularly RANTES can increase phagocytosis and killing of T. cruzi trypomastigotes (20) through enhanced nitric oxide production (35). Thus, we speculate that M. tuberculosis-induced β-CK could, in an autocrine manner, potentially activate and regulate several Mφ responses to M. tuberculosis.
M. tuberculosis intracellular growth inhibition is clearly not an exclusive property of β-CK, since other cytokines have been clearly shown to have similar effects. TNF-α, IFN-γ, and IL-6 have been reported to inhibit growth of M. tuberculosis either within human Mφ or in murine systems (2, 13). Thus, MIP-1β and RANTES join a group of cytokines that may work in concert to inhibit intracellular growth of M. tuberculosis. Furthermore, these interrelated cytokines constitute only part of the innate immune response to M. tuberculosis.
We have identified strain- and host-specific differences in the induction of β-CK by M. tuberculosis. Relative deficiencies in the production of one or more CK may have impact on both innate and acquired immune responses to M. tuberculosis infection. Virulent M. tuberculosis induced significantly less MIP-1α than did avirulent M. tuberculosis. AM from HIV-infected individuals produced 100- to 200-fold less MIP-1β and less RANTES than did normal AM. We found that MIP-1β and RANTES were capable of inhibiting intracellular growth of M. tuberculosis. While it has been presumed that β-CK secretion serve only to recruit mononuclear cells to the site of infection, these β-CK have roles in T-cell activation and Th1 cell differentiation (7, 9, 15, 16, 20, 32). Thus, we speculate that despite potential redundancies offered by other CK and cytokines, deficiencies in the ability to produce β-CK might lead to defects in the acquired immune response, as well as in AM intracellular killing of M. tuberculosis.
Acknowledgments
Special thanks go to Marie Burdick for technical assistance in the performance of the initial ELISA studies.
This work was supported by the Parker B. Francis Foundation and NHLBI grants 1 R29 HL53249-02 and 1 RO1 HL 62977-01. H.K. is supported by NHLBI grant HL 43510. J.K. is supported by NIH grant HL-03964, the Massachusetts Thoracic Society, and the American Lung Association of Massachusetts.
Editor: J. T. Barbieri
REFERENCES
- 1.Agostini, C., M. Facco, M. Siviero, D. Carollo, S. Galvan, A. M. Cattelan, R. Zambello, L. Trentin, and G. Semenzato. 2000. CXC chemokines IP-10 and mig expression and direct migration of pulmonary CD8+/CXCR3+ T cells in the lungs of patients with HIV infection and T-cell alveolitis. Am. J. Respir. Crit. Care Med. 162:1466-1473. [DOI] [PubMed] [Google Scholar]
- 2.Appelberg, R. 1994. Protective role of interferon-γ, tumor necrosis factor-α, and interleukin-6 in Mycobacterium tuberculosis and M. avium infections. Immunobiology 191:520-525. [DOI] [PubMed] [Google Scholar]
- 3.BAL Cooperative Group Steering Committee. 1990. Bronchoalveolar lavage constituents in healthy individuals, idiopathic pulmonary fibrosis, and selected comparison groups. Am. Rev. Respir. Dis. 141:S169-S175. [DOI] [PubMed] [Google Scholar]
- 4.Barnes, P., D. Chatterjee, J. Abrams, S. Lu, E. Wang, M. Yamamura, P. Brennan, and R. Modlin. 1992. Cytokine production induced by Mycobacterium tuberculosis lipoarabinomannan: relationship to chemical structure. J. Immunol. 149:541-547. [PubMed] [Google Scholar]
- 5.Bosco, M., G. Gusella, I. Espinoza-Delgado, D. Longo, and L. Varesio. 1994. Interferon-γ upregulates interleukin-8 gene expression in human monocytic cells by a posttranscriptional mechanism. Blood 83:537-542. [PubMed] [Google Scholar]
- 6.Brown, Z., M. Gerritsen, W. Caley, R. Strieter, S. Kunkel, and J. Westwick. 1994. Chemokine gene expression and secretion by cytokine-activated human microvascular endothelial cells. Am. J. Pathol. 145:913-921. [PMC free article] [PubMed] [Google Scholar]
- 7.Chensue, S., K. Warmington, E. Allenspach, B. Lu, C. Gerard, S. Kunkel, and N. Lukacs. 1999. Differential expression and cross-regulatory function of RANTES during mycobacterial (type 1) and schistosomal (type 2) antigen-elicited granulomatous inflammation. J. Immunol. 163:165-173. [PubMed] [Google Scholar]
- 8.Evanoff, H., M. Burdick, S. Moore, S. Kunkel, and R. Strieter. 1992. A sensitive ELISA for the detection of human monocyte chemoattractant protein-1 (MCP-1). Immunol. Invest. 21:39-45. [DOI] [PubMed] [Google Scholar]
- 9.Fahey, T., K. Tracey, P. Tekamp-Olson, L. Cousens, W. Jones, G. Shires, A. Cerami, and B. Sherry. 1992. Macrophage inflammatory protein-1 modulates macrophage function. J. Immunol. 148:2764-2769. [PubMed] [Google Scholar]
- 10.Fenton, M., and M. Vermeulen. 1996. Immunopathology of tuberculosis: roles of macrophages and monocytes. Infect. Immun 64:683-690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fenton, M. 1998. Macrophages and tuberculosis. Curr. Opin. Hem. 5:72-78. [DOI] [PubMed] [Google Scholar]
- 12.Fischl, M., G. Daikos, R. Uttamchandani, R. Pblete, J. Moreno, R. Reyes, A. Boota, L.Thompson, T. Cleary, and S. Oldham. 1992. Clinical presentation and outcome of patients with HIV infection and tuberculosis caused by multiple drug resistant bacilli. Ann. Intern. Med. 117:184-190. [DOI] [PubMed] [Google Scholar]
- 13.Hirsch, C. S., J. J. Ellner, D. G. Russell, and E. A. Rich. 1994. Complement receptor-mediated uptake and tumor necrosis factor-α-mediated growth inhibition of Mycobacterium tuberculosis by human alveolar macrophages. J. Immunol. 152:743-753. [PubMed] [Google Scholar]
- 14.Jones, B., K. Heldwein, T. Means, J. Saukkonen, and M. Fenton. 2001. Differential roles of toll-like receptors in the elicitation of pro-inflammatory responses by macrophages. Ann. Rheum. Dis. 60(Suppl. 3):III6-III12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karpus, J., and K. Kennedy. 1997. MIP-1α and MCP-1 differentially regulate acute and relapsing autoimmune encephalomyelitis as well as Th1/Th2 lymphocyte differentiation. J. Leukoc. Biol. 62:681-687. [PubMed] [Google Scholar]
- 16.Karpus, J., N. Lukacs, K. Kennedy, W. Smith, S. Hurst, and T. Barrett. 1997. Differential CC chemokine-induced enhancement of T helper cell cytokine production. J. Immunol. 158:4129-4136. [PubMed] [Google Scholar]
- 17.Kasahara, K., R. Strieter, S. Chensue, T. Standiford, and S. Kunkel. 1991. Mononuclear cell adherence induces neutrophil chemotactic factor/interleukin-8 gene expression. J. Leukoc. Biol. 50:287-295. [DOI] [PubMed] [Google Scholar]
- 18.Kurashima, K., M. Mukaida, M. Fujimura, M. Yasui, Y. Nakazumi, T. Matsuda, and K. Matsushima. 1997. Elevated chemokine levels in bronchoalveolar lavage fluid of tuberculosis patients. Am. J. Respir. Crit. Care Med. 155:1474-1477. [DOI] [PubMed] [Google Scholar]
- 19.Law, K., M. Weiden, T. Harkin, K. Tchou-Wong, C. Chi, and W. Rom. 1996. Increased release of interleukin-1β, interleukin-6 and tumor necrosis factor-α by bronchoalveolar cells lavaged from involved sites in pulmonary tuberculosis. Am. J. Respir. Crit. Care Med. 153:799-804. [DOI] [PubMed] [Google Scholar]
- 20.Lima, M., Y. Zhang, and F. Villalta. 1997. β-chemokines that inhibit HIV-1 infection of human macrophages stimulate uptake and promote destruction of Trypanosoma cruzi by human macrophages. Cell Mol. Biol. 43:1067-1076. [PubMed] [Google Scholar]
- 21.Loetscher, P., M. Seitz, I. Clark-Lewis, M. Baggiolini, and B. Moser. 1994. Monocyte chemotactic proteins MCP-1, MCP-2, and MCP-3 are major attractants for human CD4+ and CD8+ T lymphocytes. FASEB J. 8:1055-1060. [DOI] [PubMed] [Google Scholar]
- 22.May, M., and A. Ager. 1992. ICAM-1 independent lymphocyte transmigration across high endothelium: differential up-regulation by interferon-γ, tumor necrosis factor-α, and interleukin-1β. Eur. J. Immunol. 22:219-226. [DOI] [PubMed] [Google Scholar]
- 23.Means, T. K., S. Wang, E. Lien, A. Yoshimura, D. T. Golenbock, and M. J. Fenton. 1999. Human toll-like receptors mediate cellular activation by Mycobacterium tuberculosis. J. Immunol. 163:3920-3927. [PubMed] [Google Scholar]
- 24.Miro, A., E. Gibilara, S. Powell, and S. Kamholz. 1992. The role of fiberoptic bronchoscopy for diagnosis of pulmonary tuberculosis in patients at risk for AIDS. Chest 101:1211-1214. [DOI] [PubMed] [Google Scholar]
- 25.Muller, H., and S. Kruger. 1994. Immunohistochemical analysis of cell composition and in situ cytokine expression in HIV- and non-HIV-associated tuberculous lymphadenitis. Immunobiology 191:354-368. [DOI] [PubMed] [Google Scholar]
- 26.Peterson, P., G. Gekker, S. Hu, W. Sheng, W. Anderson, R.Ulevitch, P. Tobias, K. Gustafson, T. Molitor, and C. Chao. 1995. CD14 receptor-mediated uptake of nonopsonized Mycobacterium tuberculosis by human microglia. Infect. Immun. 63:1598-1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rathanaswami, P., M. Hachicha, M. Sadick, T. Schall, and S. McColl. 1993. Expression of the cytokine RANTES in human rheumatoid synovial fibroblasts. Differential regulation of RANTES and interleukin-8 genes by inflammatory cytokines. J. Biol. Chem. 268:5834-5839. [PubMed] [Google Scholar]
- 28.Rhoades, E., A. Cooper, and I. Orme. 1995. Chemokine response in mice infected with Mycobacterium tuberculosis. Infect. Immun. 63:3871-3877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roth, S., M. Carr, and T. Springer. 1995. C-C chemokines, but not the C-X-C chemokines, interleukin-8 and interferon-γ inducible protein-10, stimulate transendothelial chemotaxis of T lymphocytes. Eur. J. Immunol. 25:3482-3488. [DOI] [PubMed] [Google Scholar]
- 30.Sadek, M., E. Sada, Z. Toossi, S. Schwander, and E. Rich. 1999. Chemokines induced by infection of mononuclear phagocytes with mycobacteria and present in lung alveoli during active pulmonary tuberculosis. Am. J. Respir. Cell Mol. Biol. 19:513-521. [DOI] [PubMed] [Google Scholar]
- 31.Taub, D., K. Conlon, A. Lloyd, J. Oppenheim, and D. Kelvin. 1993. Preferential migration of activated CD4+ and CD8+ T cells in response to MIP-1α and MIP-1β. Science 260:355-358. [DOI] [PubMed] [Google Scholar]
- 32.Taub, D., S. Turcovski-Corrales, M. Key, D. Longo, and W. Murphy. 1996. Chemokines and T lymphocyte activation: β-chemokines costimulate human T lymphocyte activation in vitro. J. Immunol. 156:2095-2103. [PubMed] [Google Scholar]
- 33.Taub, D., P. Proost, W. Murphy, M. Anver, D. Longo, J. van Damme, and J. Oppenheim. 1995. Monocyte chemotactic protein-1 (MCP-1), -2, and -3 are chemotactic for human T lymphocytes. J. Clin. Investig. 95:1370-1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tsai, W., K. Hrose, P. Nara, Y. Kuang, S. Conley, B. Li, H. Kung, and K. Matsushima. 1991. Decrease in cytokine production by HIV-infected macrophages in response to LPS-mediated activation. Lymphokine Cytokine Res. 10:421-429. [PubMed] [Google Scholar]
- 35.Villalta, F., Y Zhang, K. Bibb, J. Kappes, and M. Lima. 1998. The cysteine-cysteine family of chemokines RANTES, MIP-1α, and MIP-1β induce trypanocidal activity in human macrophages via nitric oxide. Infect. Immun. 66:4690-4695. [DOI] [PMC free article] [PubMed] [Google Scholar]