Abstract
To control tuberculosis worldwide, the burden of adult pulmonary disease must be reduced. Although widely used, Mycobacterium bovis BCG vaccination given at birth does not protect against adult pulmonary disease. Therefore, postexposure vaccination of adults with mycobacterial antigens is being considered. We examined the effect of various mycobacterial antigens on mice with prior M. tuberculosis infection. Subcutaneous administration of live or heat-treated BCG with or without lipid adjuvants to infected mice induced increased antigen-specific T-cell proliferation but did not reduce the bacterial load in the lungs and caused larger lung granulomas. Similarly, additional mycobacterial antigen delivered directly to the lungs by aerosol infection with viable M. tuberculosis mixed with heat-killed Mycobacterium tuberculosis (1:1) also did not reduce the bacillary load but caused increased expression of tumor necrosis factor alpha (TNF-α) and interleukin 6 (IL-6), which was associated with larger granulomas in the lungs. When M. tuberculosis-infected mice were treated with recombinant BCG that secreted cytokines shown to reduce disease in a preinfection vaccine model, the BCG secreting TNF-α, and to a lesser extent, IL-2 and gamma interferon (IFN-γ), caused a significant increase in granuloma size in the lungs. Moreover, treatment of M. tuberculosis-infected mice with recombinant murine TNF-α resulted in increased inflammation in the lungs and accelerated mortality without affecting the bacillary load. Taken together, these studies suggest that administration of mycobacterial antigens to mice with prior M. tuberculosis infection leads to immune activation that may exacerbate lung pathology via TNF-α-induced inflammation without reducing the bacillary load.
The idea of immune modulation to treat tuberculosis is not new. In 1890, at the World Congress of Medicine, Robert Koch announced that he had prepared “substances” that completely cured guinea pigs in the late stages of tuberculosis (TB) (14). The substance, later called “old tuberculin,” was a glycerin extracted filtrate of cultures of the tubercle bacillus. With much fanfare, patients were treated with this bacterial extract. Unfortunately, the treatment caused florid local and systemic reactions in many of the patients with relatively mild disease. In addition, of the 230 patients with advanced cavitary disease who received this treatment, 30 died. This intense reaction to extracts of Mycobacterium tuberculosis and the associated clinical worsening became known as the “Koch phenomenon” (11).
The practical implications of the Koch phenomenon should be reconsidered in light of recent efforts to develop a new anti-TB vaccine. The goal of vaccination is protection against adult pulmonary TB. Neonatal Mycobacterium bovis BCG vaccination, which is widely used throughout the world, does not protect against adult pulmonary disease, even when it protects against the more severe forms of childhood TB (8). New strategies have therefore been proposed, including vaccination of adults with BCG or other mycobacterial preparations (7). The latter approach may be problematic. In areas of high endemicity, many individuals will have already been infected and may even have subclinical disease. If they now receive a strong immunogen, the ensuing host response may result in exacerbation of the occult disease leading to severe toxicities (Koch phenomenon).
The effect of administration of mycobacterial preparations on the outcome of disease has recently been studied by a number of investigators (1, 10, 21). Lowrie et al. showed that postexposure vaccination with either BCG or DNA encoding the M. tuberculosis heat shock protein Hsp70 or ESAT6 had little or no effect on bacillary load in the spleens or lungs of infected mice (16). However, repeated vaccination with DNA encoding Mycobacterium leprae Hsp65 reduced the number of bacilli in lungs and spleen by 1 log10 and 2 log10 at 2 and 5 months postintervention, respectively. In contrast, Turner and colleagues explored the use of two other new candidate vaccines (a subunit vaccine and a DNA vaccine, both containing M. tuberculosis Ag85) as immunotherapeutic agents in mice (23). When administered to mice already infected with M. tuberculosis, neither BCG nor these two candidate vaccines caused any improvement in the course of infection. Furthermore, repeated BCG vaccination of infected mice resulted in exacerbation of the granulomatous response in the lungs (23).
To further examine the effect of mycobacterium-induced immune activation on the host response during M. tuberculosis infection, we infected mice by aerosol with virulent M. tuberculosis. Then, 5 weeks later, the infected mice were inoculated with various preparations containing BCG or with BCG secreting murine cytokines. In addition, to determine whether the presence of additional antigen in the lungs might have an impact on outcome, naïve mice were infected by aerosol with live M. tuberculosis or a mixture of live and dead M. tuberculosis. Finally, M. tuberculosis-infected mice were treated directly with recombinant cytokines via intranasal delivery. The course of the infection was monitored by enumeration of bacilli in infected tissues, histologic examination of the lungs, quantitation of cytokine mRNA induced in the lungs, and peripheral T-cell proliferation in response to mycobacterial antigens.
MATERIALS AND METHODS
Mice.
Seven- to 8-week-old female (B6 × D2)/F1 mice, free of common pathogens, were obtained from Charles River Laboratories, Wilmington, Mass., and housed in the BSL3 (Biosafety Level 3) Animal Facility of The Rockefeller University for the duration of these experiments. All protocols were approved by the Animal Use and Care Committee of The Rockefeller University.
Infection of mice.
Aerosol infection was carried out according to a protocol developed in this laboratory (17). Briefly, mice were inoculated via the respiratory route by exposure to an aerosolized suspension of M. tuberculosis (see below) generated by a Lovelace nebulizer using a nose-only exposure system (In-Tox Products, Albuquerque, N.M.) (22). For each experiment 24 mice were exposed for 30 min to the aerosol. This procedure resulted in implantation of approximately 100 organisms into the lungs of mice, as confirmed by plating lung homogenates 3 h after infection. In some experiments M. tuberculosis was autoclaved and then mixed 1:1 with live bacilli prior to aerosol infection.
M. tuberculosis and M. bovis strains.
M. tuberculosis strain Erdman was provided as multiple stock vials by J. Belisle, Colorado State University (Fort Collins, Colo.); M. tuberculosis H37Rv was from the Trudeau Mycobacterial Culture Collection (Trudeau Institute, Saranac Lake, N.Y.). The M. tuberculosis clinical isolate HN878 was provided by J. M. Musser (20). BCG was obtained from Statens Serum Institute, Copenhagen, Denmark (BCG vaccine SSI, batch 9854). BCG strain Montreal, which was used to generate recombinant BCG expressing murine cytokines, including BCG expressing gamma interferon (BCG-IFN-γ), tumor necrosis factor alpha (BCG-ΤNF-α), and interleukin 2 (BCG-IL-2) and the control strain of BCG, carrying the plasmid vector only (BCG vector), was obtained from Richard Young, The Whitehead Institute, Cambridge, Mass. (18). All mycobacteria were grown on Middlebrook 7H9 medium (Difco, Detroit, Mich.), and bacillary stocks were stored at 107 to 108 bacilli/ml and kept at −70°C until use.
BCG preparations for postinfection inoculation.
Lyophilized BCG (SSI) (1.5 mg) was reconstituted in 2 ml of diluent (Sauton; Statens Serum Institute), according to the manufacturer's instructions (viable BCG). In addition, BCG was reconstituted in 200 μl of diluent as described above and was heated in a water bath at 60°C for 10 min. No growth of heat-treated BCG was noted using culture on egg-based solid media (Lowenstein-Jensen) or 4 weeks of growth in the BACTEC system (Bactec 4600; Becton Dickinson, Sparks, Md.). L3 adjuvant was prepared using 0.62 mg of solid monooleate (analytic grade; Kebo AB, Stockholm, Sweden), 0.48 mg of oleic acid (analytic grade; Kebo AB), and 180 mg of soybean oil (pharmaceutical grade; Karlshamn AB, Karlshamn, Sweden) and was liquefied by gentle heat at 30°C (manuscript in preparation). For injection, 200 μl of the heat-treated BCG was mixed in the L3 adjuvant, probe sonicated for 10 to 15 s, and brought to volume (2.25 ml) with 0.1 M Tris buffer, pH 7.5 (heat-treated BCG). For boosting of mice, 200 μl of heat-treated BCG was mixed in half the amount of L3 adjuvant (see above) and brought to volume (2.25 ml) with 0.1 M Tris buffer, pH 7.5.
Vaccination of infected mice with BCG preparations.
Five weeks after the initial infection with M. tuberculosis H37Rv, mice were divided into four groups. Groups 1 and 2 received 0.1 ml of viable BCG subcutaneously (s.c.). Group 3 received 0.1 ml of heat-treated BCG in L3 adjuvant s.c., while group 4 received no treatment. Three weeks later, groups 2 and 3 were boosted with heat-treated BCG in L3 adjuvant by intranasal administration of 10 μl (5 μl per nostril). Mice were evaluated at 12 weeks. In another experiment, either 6 weeks before or 5 weeks after the aerosol infection, mice were vaccinated s.c. with one of the recombinant BCG strains (BCG-IFN-γ, BCG-TNF-α, BCG-IL-2, or BCG vector) (18) at a dose of 106 organisms per mouse. Three weeks after the initial vaccination, the mice received a boost with the same dose of recombinant BCG. A control group of mice received no BCG. Mice were evaluated at 12 and 20 weeks postchallenge with M. tuberculosis.
Intranasal treatment of infected mice.
Recombinant murine TNF-α was obtained from Endogen (Boston, Mass.), reconstituted in 1% bovine serum albumin-phosphate-buffered saline to a final concentration of 2 × 105 IU/ml, and kept at 4°C. The cytokine was administered intranasally for 5 consecutive days per week for 4 weeks (6). Five microliters was applied directly to the nostrils of each mouse (final dose of TNF-α, 103 IU per mouse per day). Recombinant murine IFN-γ was obtained from Valbiotech (Paris, France) and reconstituted in 1% bovine serum albumin-phosphate-buffered saline to a final concentration of 106 IU/ml. Ten microliters was applied into the nostrils of each mouse as described above (final dose of IFN-γ, 104 IU per mouse per day). Control mice were untreated.
CFU assay.
The number of viable mycobacteria in lungs, livers, and spleens of infected mice were evaluated at designated time points. Tenfold serial dilutions of organ homogenates were plated onto 7H11 agar (Becton Dickinson) and were incubated at 37°C. The number of viable bacilli was evaluated by counting individual colonies after 2 to 3 weeks of growth.
Cytokine mRNA levels in the infected lung.
Total cellular RNA from lungs of infected mice was obtained at designated time points following aerosol infection. Tissues were homogenized in 3 ml of RNAzolB (Cinna/Biotcx Lab. Inc., Houston, Tex.), and RNA was extracted according to the manufacturer's instructions. The reverse transcription-PCR was carried out as previously described (15). Briefly, 1 μg of RNA was reverse transcribed using a Moloney murine leukemia virus reverse transcriptase and was amplified with Taq polymerase according to procedures given in the GeneAmp RNA PCR kit (Perkin-Elmer, Branchburg, N.J.). Primers for cytokines and β-actin were used as described (17). Densitometry of the amplified bands was carried out using a PhosphorImager (Molecular Dynamics, Sunnyvale, Calif.). Results were normalized to the density of β-actin.
Lymphocyte proliferation assay.
Spleen and draining lymph nodes were removed at each time point and were processed as described (4). Briefly, cells isolated from spleen and lymph nodes were cultured at 2 × 105 cells/100 μl in 96-well U-bottom plates in RPMI 1640 medium (Gibco BRL, Gaithersburg, Md.) and were supplemented with 10% fetal bovine serum, penicillin, and streptomycin (final concentration, 50 μg/ml) (all obtained from Gibco BRL). The cells were incubated with concanavalin A (final concentration, 5 μg/ml) (Sigma, St. Louis, Mo.) or M. tuberculosis H37Ra sonicate (final concentration, 50 μg/ml) at 37°C for 3 or 5 days, respectively, and were then pulsed with [H3]thymidine (1 μCi/well) for an additional 18 h. Incorporation of [H3]thymidine was measured by β-scintillation counting. Values were expressed as mean counts per minute in the cultures.
Histopathology.
At various time points after infection, lungs were fixed in 10% neutral buffered formalin, embedded in paraffin, and processed for histology. Sections were stained with hematoxylin and eosin and Ziehl-Neelsen for histologic evaluation and photography.
Morphometric evaluation of granuloma size.
Morphometry of the lesions was performed using Microcomp, a computer-based image analysis system (Southern Micro Institute, Atlanta, Ga.) and/or Sigmascan Pro 5:0 (SPSS Science Inc., Chicago, Ill.). A calibration micrometer (in square micrometers) slide was used to determine the area evaluated.
Statistical analysis.
Data were analyzed using an independent Student t test. A P of <0.05 was considered statistically significant. Kaplan-Meier analysis was used to determine statistical significance of the differences in survival time of mice.
RESULTS
The effect of postinfection exposure to mycobacterial antigens.
To determine whether the course of established disease is altered by immune stimulation with mycobacterial antigens, mice were first infected by aerosol with 100 CFU of M. tuberculosis H37Rv. At 5 weeks after infection, prior to any additional treatment, the number of CFU in the lungs was approximately 6.6 log10. At this time, infected mice were split into four groups, and mice in groups 1 and 2 were vaccinated with viable BCG while mice in group 3 received heat-treated BCG in L3 adjuvant. Three weeks later mice in groups 2 and 3 were boosted with heat-treated BCG in L3 adjuvant, as described above (Materials and Methods). Four weeks later (at 12 weeks after the initial infection), the numbers of CFU in lungs, livers, and spleens of mice in all four groups were evaluated and found to be similar (Fig. 1A). Thus, postinfection immunotherapy with these BCG preparations had no effect on the bacillary loads in the organs of any of the infected mice.
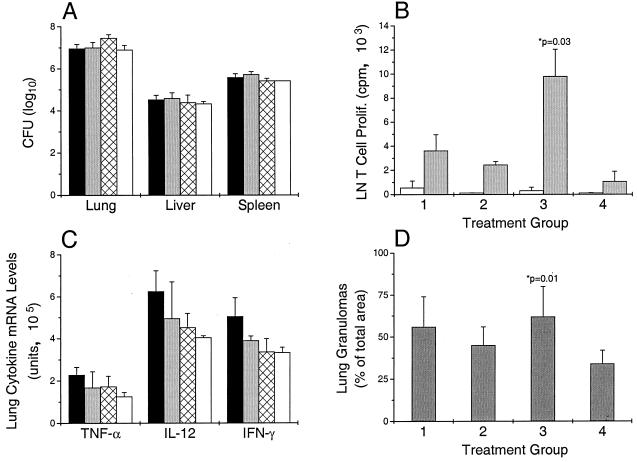
FIG. 1.
Effect of postinfection vaccination on bacillary load (CFU) (A), lymph node (LN) T-cell proliferation (B), lung cytokine mRNA levels (C), and area of lung occupied by granulomas (D). (A and C) M. tuberculosis-infected mice were vaccinated according to the protocol described in Materials and Methods. Group 1, viable BCG (black bar); group 2, viable BCG followed by boost with heat-treated BCG in L3 adjuvant (gray bar); group 3, heat-treated BCG in L3 adjuvant and boosted as above (hatched bar); group 4, no vaccination (empty bar). (B) Lymph node cells stimulated with H37Ra sonicate (gray bars) or unstimulated control (empty bar). (D) Percentage of lung parenchyma occupied by granuloma. Results are from four animals per group at 12 weeks post-initial infection, expressed as means ± standard deviation. ∗, P compared to unvaccinated controls (group 4).
An evaluation of the systemic T-cell response of the infected mice was also carried out. Cells were isolated from the draining lymph nodes of infected and vaccinated mice at 12 weeks and stimulated in vitro with M. tuberculosis H37Ra sonicate. Compared to the control infected mice (group 4), an increased proliferative response was noted in all treatment groups and was significant for group 3 (Fig. 1B). Lymph node cells from infected animals that received heat-treated BCG in L3 adjuvant followed by intranasal boosting with heat-treated BCG in L3 adjuvant (group 3) showed the largest increase in proliferative responses in vitro compared to the other treatment group and the unvaccinated controls (P = 0.03). Cells isolated from the spleens of the infected, vaccinated animals showed similar patterns of proliferative responses, although these were much lower (not shown). To examine the immune stimulation in the lungs of infected, vaccinated animals, cytokine mRNA was prepared from the lungs at 12 weeks. When compared to the infected, unvaccinated controls (group 4), the vaccinated, infected animals (groups 1 to 3) had only slightly higher levels of TNF-α mRNA in the lungs (Fig. 1C). Animals in group 1 also had somewhat higher levels of mRNAs for IL-12 and IFN-γ; all these differences were not statistically significant.
When the lungs of the mice in the four treatment groups were examined histologically at week 12, granulomas were larger in the infected animals that had received heat-treated BCG in L3 adjuvant and were then boosted intranasally (group 3). Morphometric analysis revealed that 69% of the lung parenchyma was occupied by granulomas, compared to 56% in group 1, 47% in group 2, and 36% in the control animals (group 4) (Fig. 1D). Thus, although the levels of systemic immune activation as measured by antigen-specific T-cell proliferation increased, the vaccine-induced immune stimulation did not affect the number of CFU in the lungs. However, the immune activation was associated with an exacerbation of pathology, as indicated by the size of the granulomas in the lungs (compare Fig. 1B and D).
Effect of additional antigen on the host response to M. tuberculosis infection.
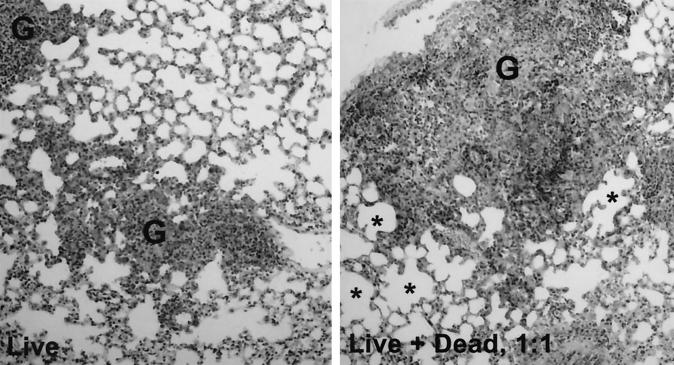
To examine whether the presence of additional mycobacterial antigen in the infected lung changed the course of infection, mice were infected with either viable M. tuberculosis strain Erdman (100 CFU) or the same dose of viable bacilli (100 CFU) mixed with an equivalent dose of heat-killed organisms (1:1). The presence of additional heat-killed organisms in the infecting inoculum had no significant effect on the subsequent bacillary load (CFU) in the lung, spleen, and liver of infected mice (Table 1). In mice that received the live infection only, levels of mRNA for TNF-α and for IL-6 increased over the first 3 weeks of infection (Table 1). When mice were infected with the mixture of live plus dead M. tuberculosis, even higher expression of cytokine mRNA for TNF-α and for IL-6 was noted. The difference was most pronounced at week 3 (P < 0.05); by week 4 the difference was no longer seen (Table 1). In the lungs of mice infected with the mixture of viable and heat-killed bacilli, the higher cytokine mRNA levels were associated with larger granulomas (Fig. 2). In the mice infected with live plus dead organisms, the mean size of lesions at 4 weeks postinfection was 6.17 mm3 ± 1.3 mm3, compared to 4.38 mm3 ± 0.64 mm3 in those infected with live organisms only. Distended alveolar spaces (edematic lung) were also seen, suggesting a relative loss of lung function (Fig. 2). These results indicate that the additional mycobacterial antigen in the lungs of mice receiving the mixed infection induces a stronger local inflammatory response (increased TNF-α and IL-6 production; Table 1), leading to increased lung pathology without altering the bacillary burden.
TABLE 1.
Infection with viable and viable plus heat-killed M. tuberculosis
| Type of infection and no. of wk | No. of CFUa (log10) in:
|
Amt of lung cytokine mRNAa (units) for:
|
|||
|---|---|---|---|---|---|
| Lung | Spleen | Liver | TNF-α | IL-6 | |
| Viable bacilli | |||||
| 1 | 3.7 ± 0.1 | 0 | 1.4 ± 1.2 | 63 ± 22 | 46 ± 10 |
| 2 | 5.2 ± 0.3 | 1.6 ± 1.5 | 1.9 ± 1.6 | 69 ± 30 | 174 ± 17 |
| 3 | 5.5 ± 0.1 | 3.9 ± 0.2 | 3.2 ± 0.6 | 144 ± 53 | 233 ± 33 |
| 4 | 6.0 ± 0.3 | 4.1 ± 0.1 | 2.6 ± 0.3 | 151 ± 51 | 161 ± 15 |
| Viable + heat-killed bacilli | |||||
| 1 | 3.5 ± 0.4 | 0 | 1.8 ± 1.7 | 33 ± 5 | 46 ± 5 |
| 2 | 5.1 ± 0.2 | 0.9 ± 0.5 | 2.8 ± 0.8 | 111 ± 9 | 243 ± 25 |
| 3 | 5.5 ± 0.1 | 3.6 ± 0.2 | 3.2 ± 0.2 | 269 ± 24b | 384 ± 37b |
| 4 | 5.8 ± 0.2 | 3.9 ± 0.6 | 3.4 ± 0.2 | 132 ± 81 | 149 ± 27 |
Number of mice per group per time point (n = 5).
P < 0.05 compared to infection with viable bacilli only.
FIG. 2.
Effect of additional antigen on the granulomatous response in the lungs of mice at 3 weeks post-aerosol infection with viable M. tuberculosis (live) or viable plus heat-killed M. tuberculosis (live + dead, 1:1). G, granuloma; ∗, distended alveolar spaces (edematic lung). Ziehl-Neelsen stain, magnification, ×10.
Effect of vaccination with recombinant BCG secreting murine cytokines on the bacillary load and granuloma size in infected organs.
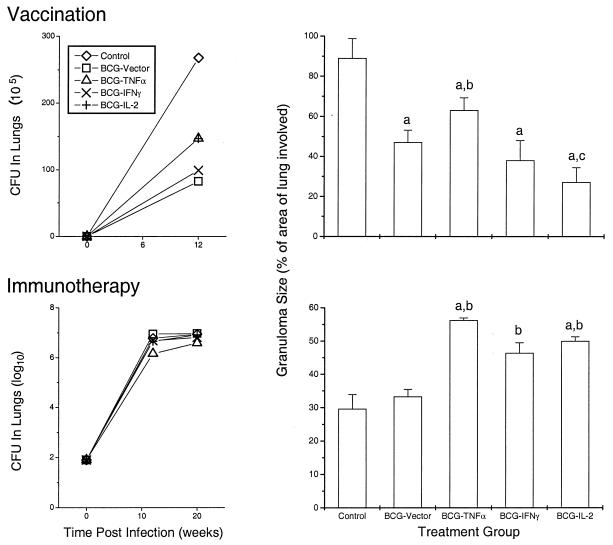
To determine whether particular cytokines could enhance the BCG-induced protective immune response to M. tuberculosis, mice were vaccinated s.c. with recombinant BCG secreting murine cytokines (BCG vector, BCG-TNF-α, BCG-IFN-γ, or BCG-IL-2) followed by M. tuberculosis H37Rv challenge, as described (Materials and Methods). In these experiments, the recombinant BCG used was prepared from BCG strain Montreal, a known weak immunogen for mice (19). By 12 weeks after M. tuberculosis challenge, the bacilli in the lungs had grown to a concentration of 3 × 107 CFU in control (nonvaccinated) mice (Fig. 3, top). Vaccination with BCG vector resulted in a bacillary load reduced by about fourfold. Cytokine secretion by the recombinant BCG did not improve the control of the bacillary growth in the lungs. At 12 weeks postinfection, the lungs of unvaccinated controls showed an extensive inflammatory infiltrate composed of macrophages, lymphocytes, and neutrophils within the alveolar space consistent with a pneumonic process in addition to large, coalescent granulomas. The size of the granulomas was reduced by about 50% in BCG vector-vaccinated mice compared to unvaccinated controls (P < 0.05) (Fig. 3, top). Vaccination with BCG secreting IL-2 or BCG secreting IFN-γ resulted in even smaller granulomas than the BCG vector-vaccinated mice (P < 0.05). However, BCG-TNF-α vaccination resulted in larger granulomas than did vaccination with BCG vector (P < 0.05), though the granulomas were still smaller than in nonvaccinated mice (P < 0.05). Thus, of the cytokines tested, IL-2 together with BCG appeared to impart the most protection in terms of limiting immunopathology in the lungs; the presence of TNF-α appeared to exacerbate the pathology.
FIG. 3.
Effect of vaccination (preinfection, top) and immunotherapy (postinfection, bottom) with cytokine-secreting BCG on number of CFU in lung at 12 and 20 weeks post-initial infection (left panels) and on granuloma size at 12 weeks (right panels). Results are from four animals per group per time point, expressed as means ± standard deviation. a, P < 0.05 compared to unvaccinated controls; b, P < 0.05, higher than for BCG vector-vaccinated mice; c, P < 0.05, lower than for BCG vector-vaccinated mice.
Effect of postinfection vaccination with cytokine-producing BCG.
To determine whether particular cytokines could render BCG vaccination more effective against ongoing M. tuberculosis infection, recombinant strains of BCG producing various murine cytokines were used to treat infected mice. Mice infected with H37Rv were vaccinated twice (at 5 and 8 weeks) postinfection with 106 organisms of viable BCG-TNF-α, BCG-IL-2, BCG-IFN-γ, or BCG vector. No effect on the number of CFU in the lungs or spleens was observed at weeks 12 and 20 postinfection compared to in the organs of unvaccinated, infected mice (Fig. 3, bottom). Postinfection administration of recombinant BCG secreting cytokines did, however, affect the size of the granulomas. Larger granulomas involving 56.2% of the lung were observed in the infected mice that had received recombinant BCG-TNF-α, compared to 29.6% in the control unvaccinated mice (P = 0.02) (Fig. 3, bottom). Infected mice treated with BCG-IL-2 or BCG-IFN-γ had intermediate-sized granulomas (50 or 46.4%, respectively). Thus, the combination of the immune-stimulatory cytokines with BCG resulted in exacerbation of lung pathology; the worst effect was seen when BCG was combined with TNF-α.
Effect of exogenous TNF-α on course of M. tuberculosis infection.
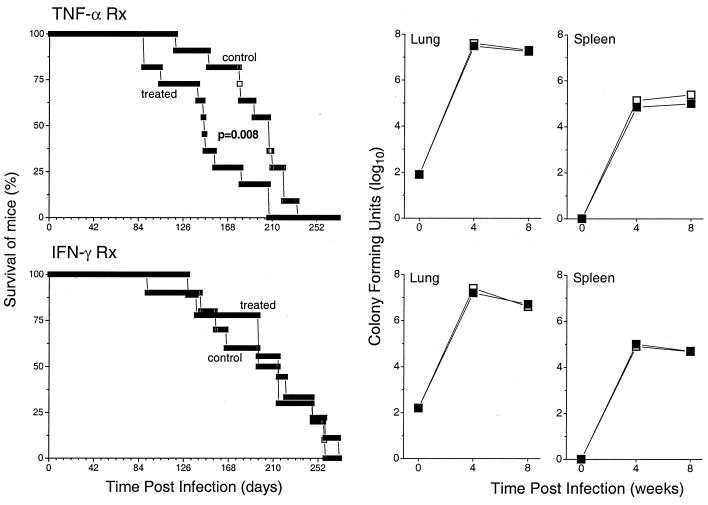
The previous experiments suggested that the deleterious component of the immune response to mycobacterial antigens is excess TNF-α. To directly examine the effect of excess TNF-α on lung pathology, mice infected with 80 CFU of M. tuberculosis were treated intranasally with recombinant murine TNF-α for the first 4 weeks of infection. At 4 weeks and then 8 weeks after infection and treatment, the numbers of CFU in lungs and spleens were similar (Fig. 4, top). However, survival of the mice was substantially altered. Mice infected with M. tuberculosis and treated with TNF-α succumbed to the infection significantly earlier than mice that had not received the cytokine treatment (P = 0.008) (Fig. 4, top). In contrast, when infected mice (100 CFU at baseline) were treated intranasally with IFN-γ, no effect on survival or number of CFU in lungs and spleens was noted (Fig. 4, bottom).
FIG. 4.
Effect of exogenous recombinant cytokines on the bacillary load (right panels) and survival of infected mice (left panels). Mice were infected with M. tuberculosis and treated intranasally with recombinant murine TNF-α (top panels) or IFN-γ (bottom panels). Solid squares, cytokine-treated mice; empty squares, control untreated mice. Results for survival are from 11 mice per group and for numbers of CFU from four mice per group per time point.
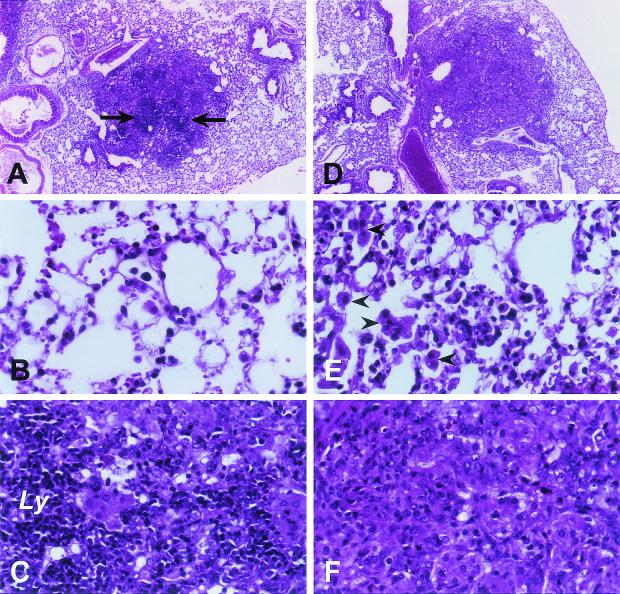
TNF-α treatment of infected mice was associated with increased cellularity of the lungs, including higher numbers of polymorphonuclear leukocytes in the granulomas and larger numbers of foamy macrophages in the alveolar spaces at 4 weeks (Fig. 5). The macrophages did not appear to be more activated, as there was no increase in the mRNA levels of inflammatory cytokines in the lungs (IL-6, IL-10, IL-12, and TNF-α) (not shown). The lungs of the infected, untreated mice appeared to have higher numbers of small lymphocytes (Fig. 5). Again, the lymphocytes did not appear to be more activated, since the IFN-γ mRNA levels were similar or even somewhat lower (about 40%) in the lungs of TNF-α-treated mice at 4 and 8 weeks (not shown). Thus, TNF-α treatment appeared to result in the exacerbation of lung pathology without significant changes in the bacillus burden. On the other hand, IFN-γ treatment did not affect these parameters.
FIG. 5.
Effect of exogenous TNF-α on the granulomatous response in the lungs. Mice were infected with M. tuberculosis and treated intranasally with recombinant murine TNF-α, and the lungs were examined at 4 weeks postinfection. (A to C) Untreated mice. (D to F) TNF-α-treated mice. Note extensive lymphocyte infiltration in arrows (A) and Ly (C). In response to TNF-α treatment (E), large macrophages are present in the alveolar spaces (arrowheads). Hematoxylin and eosin stain. (A and D) Magnification, ×4. (B, C, E, and F) Magnification, ×40.
DISCUSSION
Our results, as well as those of others, demonstrate how difficult it is to change the course of existing M. tuberculosis infection in the lungs by immunotherapy with vaccines. Indeed, Koch himself did not claim that his treatment with “tuberculin lymph” killed the bacteria (5). In our postinfection experiments, vaccination with BCG, BCG plus other antigens, recombinant BCG secreting murine cytokines, or heat-killed M. tuberculosis did not reduce the bacterial load in the lungs of infected mice. Even those vaccines that were shown to be effective as preexposure vaccines (Fig. 3) failed to reduce the number of CFU when administerred as postinfection vaccines. Analogous results have been obtained by other investigators. Turner et al. tested three different vaccines in infected mice and guinea pigs as immunotherapy: (i) BCG Pasteur, (ii) a subunit vaccine containing purified culture filtrate proteins of M. tuberculosis emulsified in an adjuvant together with recombinant murine IL-2, and (iii) a DNA vaccine consisting of a vector expressing the gene for M. tuberculosis Ag85A (23). The candidate vaccines were selected because they had shown efficacy as preexposure vaccines in protecting naïve animals against challenge with M. tuberculosis (1, 10). However, all three of these vaccines, although protective as preexposure vaccines, failed to reduce the bacterial load in the lungs of mice with prior tuberculosis infection. Similarly, Lowrie et al. tested a number of DNA vaccines encoding M. leprae Hsp65 or M. tuberculosis Hsp70 or ESAT-6 as postinfection treatments (16). Only the DNA vaccine encoding M. leprae Hsp65 resulted in some reduction in bacterial load in the lungs of infected mice.
Interestingly, when preexisting infection had been eliminated with antibiotic therapy, repeated postexposure vaccination did protect against reactivation of disease (16). Thus, it is possible that immune modulation in the presence of antituberculous therapy may facilitate bacillary clearance in the lungs (9). Indeed, in a previous pilot study of patients with multidrug-resistant pulmonary TB, we observed that administration of recombinant IL-2 as adjunctive therapy combined with anti-TB chemotherapy resulted in accelerated sputum clearance and improved radiographic appearance of the lungs (12).
As we have clearly shown here, increased immune activation is associated with exacerbation of pathology at the sites of preexisting TB. This had originally been noted by Koch. In response to the treatment with “tuberculin lymph,” infected tissues became inflamed and necrotic and partially sloughed often in association with clinical worsening. The English physician and writer A. Conan Doyle wrote about Koch's treatment, “It may also be remarked that the fever after the injection is in some cases so very high (41°C) that it is hardly safe to use in the case of a debilitated patient” (in Review of Reviews, December 1890) (5). Our experiments in mice suggest that the cause of the worsening pathology and fever observed by Koch in patients may be excess TNF-α at the site of infection. In our murine experiments, the increased size and cellularity of the granulomas were accompanied by increased expression of TNF-α mRNA in the lung. Consistent with this, vaccination of mice with BCG-TNF-α resulted in an increase in the size of lung granulomas. Also, treatment of infected mice with recombinant murine TNF-α resulted in increased inflammation in the lung and accelerated death. In a previous study, in which mice were infected with BCG-TNF-α, we noted that high levels of TNF-α at the BCG infection site resulted in much severer lung pathology and decreased survival (2). Furthermore, TNF-α-associated clinical worsening has been observed in patients with severe TB upon initiation of anti-TB chemotherapy (3). This was probably due to death of the organisms and release of mycobacterial components. Mycobacteria and their products have previously been shown to induce TNF-α production through signaling of the macrophage Toll-like receptors (24, 25).
In addition to the safety issues associated with postinfection vaccination and the Koch phenomenon, there is also an operational consideration for any trial designed to test postexposure vaccine. Vaccination of adults in an area of high endemicity might reveal occult disease, which might confound interpretation of the results, since the number of TB cases in the vaccine arm would be selectively increased compared to that in the untreated arm. This may have been the case in the BCG vaccine trial carried out in the Karonga region of Malawi, where significantly higher rates of pulmonary TB were reported among scar-positive persons who had received a second dose of BCG (13). Thus, for both safety (immune-mediated pathology) and study design (subclinical disease scored as a newly acquired TB), any study of candidate postexposure vaccines must ensure that recruited participants do not have undiagnosed disease.
Acknowledgments
These studies were supported by NIH grants AI22616 and AI42056 (to G.K.) and AITRP TW00231 (to L.-G.B.) and by Direct Effect (New York, N.Y.). A.L.M. was supported by a grant from the Pott's Foundation.
We thank Judy Adams for preparation of the figures and Marguerite Nulty for secretarial assistance.
L.T. and A.L.M. contributed equally to the paper.
Editor: S. H. E. Kaufmann
REFERENCES
- 1.Baldwin, S. L., C. D'Souza, A. D. Roberts, B. P. Kelly, A. A. Frank, M. A. Lui, J. B. Ulmer, K. Huygen, D. M. McMurray, and I. M. Orme. 1998. Evaluation of new vaccines in the mouse and guinea pig model of tuberculosis. Infect. Immun. 66:2951-2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bekker, L.-G., A. L. Moreira, A. Bergtold, S. Freeman, B. Ryffel, and G. Kaplan. 2000. Immunopathologic effects of tumor necrosis factor alpha in murine mycobacterial infection are dose dependent. Infect. Immun. 68:6954-6961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bekker, L.-G., G. Maartens, L. Steyn, and G. Kaplan. 1998. Selective increase in plasma TNF-alpha and concomitant clinical deterioration after initiating therapy in patients with severe tuberculosis. J. Infect. Dis. 178:580-584. [DOI] [PubMed] [Google Scholar]
- 4.Caruso, A. M., N. Serbina, E. Klein, K. Triebold, B. R. Bloom, and J. L. Flynn. 1999. Mice deficient in CD4 T cells have only transiently diminished levels of IFN-gamma, yet succumb to tuberculosis. J. Immunol. 162:5407-5416. [PubMed] [Google Scholar]
- 5.Dubos, R., and J. Dubos. 1952. The white plague. Little, Brown & Co., Boston, Mass.
- 6.Eid, P., J. F. Meritet, C. Maury, A. Lasfar, D. Weill, and M. G. Tovey. 1999. Oromucosal interferon therapy: pharmacokinetics and pharmacodynamics. J. Interferon Cytokine Res. 19:157-169. [DOI] [PubMed] [Google Scholar]
- 7.Fine, P. E. 1998. Vaccines, genes and trials. Novartis Found. Symp. 217:57-69. [DOI] [PubMed] [Google Scholar]
- 8.Fine, P. E. 1995. Variation in protection by BCG: implications of and for heterologous immunity. Lancet 346:1339-1345. [DOI] [PubMed] [Google Scholar]
- 9.Glassroth, J. 2000. Clinical considerations in designing trials of vaccines for tuberculosis. Clin. Infect. Dis. 30:S229-S232. [DOI] [PubMed] [Google Scholar]
- 10.Huygen, K., J. Content, O. Denis, D. L. Montgomery, A. M. Yawman, R. R. Deck, C. M. DeWitt, I. M. Orme, S. Baldwin, C. D'Souza, A. Drowart, E. Lozes, P. Vandenbussche, J.-P. Van Vooren, M. A. Liu, and J. B. Ulmer. 1996. Immunogenicity and protective efficacy of a tuberculosis DNA vaccine. Nat. Med. 2:893-899. [DOI] [PubMed] [Google Scholar]
- 11.Iseman, M. D. 2000. A physician’s guide to tuberculosis. Lippincott Williams & Wilkins, Philadelphia, Pa.
- 12.Johnson, B. J., L.-G. Bekker, R. Rickman, S. Brown, M. Lesser, S. Ress, P. Willcox, L. Steyn, and G. Kaplan. 1997. rhuIL-2 adjunctive therapy in multidrug resistant tuberculosis: a comparison of two treatment regimes and placebo. Tuber. Lung Dis. 78:195-203. [DOI] [PubMed] [Google Scholar]
- 13.Karonga Prevention Trial Group. 1996. Randomised controlled trial of single BCG, repeated BCG, or combined BCG, and killed Mycobacterium leprae vaccine for prevention of leprosy and tuberculosis in Malawi. Lancet 348:17-24. [PubMed] [Google Scholar]
- 14.Koch, R. 1890. Weitere. Mitteilungen uber ein Heilmittel gegen Tuberkulose. Dtsch. Med. Wochenschr. 16:1029-1032. [Google Scholar]
- 15.Laochumroonvorapong, P., J. Wang, C.-C. Liu, W. Ye, A. L. Moreira, K. B. Elkon, V. Freedman, and G. Kaplan. 1997. Perforin, a cytotoxic molecule which mediates cell necrosis, is not required for early control of mycobacterial infection in mice. Infect. Immun. 65:127-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lowrie, D. B., R. E. Tascon, V. L. Bonato, V. M. Lima, L. H. Faccioli, E. Stavropoulos, M. J. Colston, R. G. Hewinson, K. Moelling, and C. L. Silva. 1999. Therapy of tuberculosis in mice by DNA vaccination. Nature 400:269-271. [DOI] [PubMed] [Google Scholar]
- 17.Moreira, A. L., L. Tsenova-Berkova, J. Wang, P. Laochumroonvorapong, S. Freeman, V. H. Freedman, and G. Kaplan. 1997. Effect of cytokine modulation by thalidomide on the granulomatous response in murine tuberculosis. Tuber. Lung Dis. 78:47-55. [DOI] [PubMed] [Google Scholar]
- 18.Murray, P. J., A. Aldovini, and R. A. Young. 1996. Manipulation and potentiation of antimycobacterial immunity using recombinant bacille Calmette-Guerin strains that secrete cytokines. Proc. Natl. Acad. Sci. USA 93:934-939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Orme, I. M., and F. M. Collins. 1984. Demonstration of acquired resistance in Bcgr inbred mouse stains infected with a low dose of BCG montreal. Clin. Exp. Immunol. 56:81-88. [PMC free article] [PubMed] [Google Scholar]
- 20.Sreevatsan, S., X. Pan, K. E. Stockbauer, N. D. Connell, B. N. Kreiswirth, T. S. Whittam, and J. M. Musser. 1997. Restricted structural gene polymorphism in the Mycobacterium tuberculosis complex indicates evolutionarily recent global dissemination. Proc. Natl. Acad. Sci. USA 94:9869-9874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tascon, R. E., M. J. Colston, S. Ragno, E. Stavropoulos, D. Gregory, and D. B. Lowrie. 1996. Vaccination against tuberculosis by DNA injection. Nat. Med. 2:888-892. [DOI] [PubMed] [Google Scholar]
- 22.Tsenova, L., A. L. Moreira, E. Party, V. H. Freedman, and G. Kaplan. 1997. Aerosol infection of mice with mycobacteria using a nose-only exposure device. J. Am. Biol. Safety Assoc. 2:20-31. [Google Scholar]
- 23.Turner, J., E. R. Rhoades, M. Keen, J. T. Belisle, A. A. Frank, and I. M. Orme. 2000. Effective preexposure tuberculosis vaccines fail to protect when they are given in an immunotherapeutic mode. Infect. Immun. 68:1706-1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Underhill, D. M., A. Ozinsky, A. M. Hajjar, A. Stevens, C. B. Wilson, M. Bassetti, and A. Aderem. 1999. The Toll-like receptor 2 is recruited to macrophage phagosomes and discriminates between pathogens. Nature 401:811-815. [DOI] [PubMed] [Google Scholar]
- 25.Underhill, D. M., A. Ozinsky, K. D. Smith, and A. Aderem. 1999. Toll-like receptor-2 mediates mycobacteria-induced proinflammatory signaling in macrophages. Proc. Natl. Acad. Sci. USA 96:14459-14463. [DOI] [PMC free article] [PubMed] [Google Scholar]