Abstract
The diagnosis of functional visual loss—reduced visual performance in the absence of an organic cause—is usually made by exclusion. We conducted a pilot study to evaluate pupil perimetry in three patients (aged 14, 43 and 50) with visual field loss presumed to be functional on clinical grounds and having no cause identified by visual electrophysiology or magnetic resonance imaging. A modified automated perimeter was used to examine visual and pupil responses to a light stimulus (size 1.7°) presented at five locations in the visual field (fixation and in each of the four quadrants).
In each patient, the pupil responses were normal in those test quadrants which showed apparent visual field loss.
Pupil perimetry provides objective evidence for a diagnosis of functional visual field loss in selected patients and may circumvent the need for other investigations.
INTRODUCTION
Functional visual loss refers to reduced visual performance in the absence of an organic cause. The diagnosis is usually made by exclusion, and this can be time-consuming and expensive. Ideally, the diagnosis should be made by demonstration of normal visual function. When the visual acuity is apparently reduced, normal acuity can often be confirmed by clinical methods, such as testing of acuity under binocular conditions with the normal eye fogged, or more objectively by the pattern onset visual evoked potential (VEP). In the case of functional visual field loss with good visual acuity, a different approach is needed to objectively measure function in the visual periphery. Pupil perimetry is a new technique that combines the techniques of automated static perimetry and video pupillography1. By recording the pupil responses to light stimuli presented at different visual field loci, it offers an objective method of visual field assessment. In this pilot study, pupil perimetry was performed in three patients with presumed functional visual field loss.
METHODS
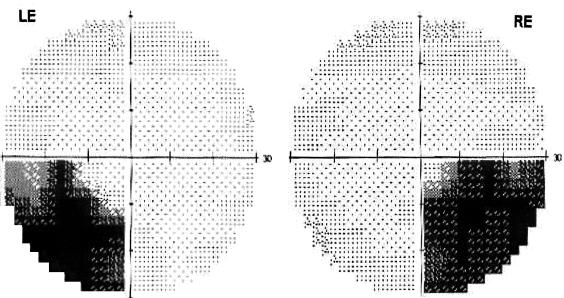
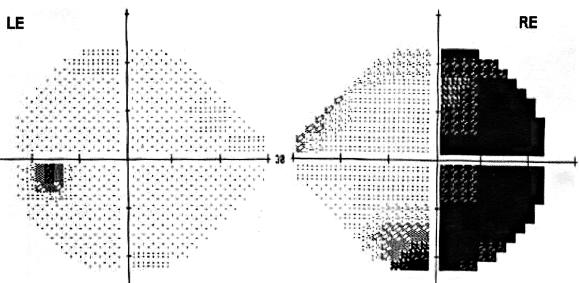
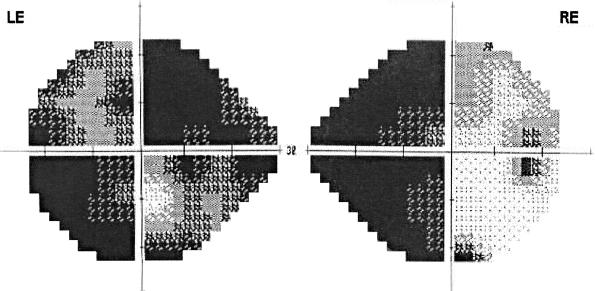
Three patients aged 14, 43 and 50 years with normal visual acuities and presumed functional visual field loss underwent pupil perimetry. The visual field defects in the first two of these patients, when tested with automated visual perimetry (Humphrey Field Analyser, 30-2 programme), were bitemporal inferior quadrantanopia (Figure 1) and temporal hemianopia in the right eye (Figure 2), respectively. The third patient showed generalized field loss in the left eye and a nasal hemianopia in the right eye (Figure 3). The visual perimetry in these patients satisfied the reliability criteria and were repeatable. In all cases the pattern of field loss implied lesions predominantly of the anterior visual pathways, and should therefore be associated with attenuation of the pupil light reflex. An organic basis for the visual field loss was excluded by visual electrophysiology (electroretinograms, pattern electroretinograms and visual evoked potentials were all normal) and normal brain/optic nerve MRI imaging.
Figure 1.
Case 1: Conventional computerized automated visual perimetry showing bitemporal inferior quadrantanopia (RE=right eye, LE=left eye)
Figure 2.
Case 2: Computerized automated visual perimetry showing temporal hemianopia in right eye
Figure 3.
Case 3: Computerized automated visual perimetry showing generalized field loss in the left eye and nasal hemianopia in the right eye
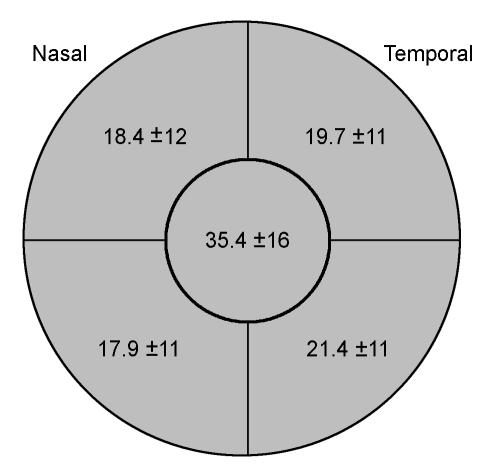
Pupil responses were evaluated by means of the Octopus 1-2-3 automated perimeter fitted with an infrared video camera for real-time monitoring of pupil size2. Five stimulus locations were tested—fixation and at 17° eccentricity along the 45/135° meridians in the supero-temporal, inferotemporal, superonasal and inferonasal quadrants. The stimulus parameters for intensity, size and duration were 4000 asb, 1.7° (Goldmann V), and 500 ms, respectively, with a background illumination of 31.4 apostilb. The amplitudes of the pupil responses (expressed as percentage constriction of the pupil area) were measured for all five test locations in both eyes. The results were compared with pupil responses recorded from age-matched healthy controls (n=23) (Figure 4).
Figure 4.
The five retinal quadrants tested in pupil perimetry and their normal values (percentage constriction of pupil area ±2 standard deviations)
RESULTS
Mean amplitudes of pupil responses at each stimulus location are shown in Table 1. In all three patients, pupil perimetry was normal in the quadrants of visual field identified as abnormal by conventional perimetry. In case 3 the diagnosis of functional visual loss led to reinvestigation of diabetes insipidus and to an amended diagnosis of psychogenic polydipsia.
Table 1.
Pupil responses in patients with presumed functional visual field loss showing normal pupil responses in the quadrants of visual field loss detected by conventional visual field testing
|
Case 1 (bitemporal inferior quadrantanopia)
|
Case 2 (right temporal hemianopia)
|
Case 3 (right nasal hemianopia, left generalized loss)
|
|||||
|---|---|---|---|---|---|---|---|
| Quadrant | RE | LE | RE | LE | RE | LE | Normal pupil responses (% constriction of pupil area ±2 SD) |
| Superotemporal | 20.3 | 17.7 | 19.1 | 19.4 | 17.1 | 19.6 | 19.7 ± 11 |
| Superonasal | 16.8 | 14.6 | 16.7 | 15.4 | 15.7 | 16.8 | 18.4 ± 12 |
| Fixation | 37.6 | 35.2 | 35.2 | 34.2 | 33.2 | 34.6 | 35.4 ± 16 |
| Inferotemporal | 22.8 | 22.9 | 19.2 | 18.4 | 18.4 | 19.1 | 21.4 ± 11 |
| Inferonasal | 21.2 | 19.5 | 17.2 | 15.4 | 16.1 | 15.9 | 17.9 ± 11 |
RE, LE=Right eye, left eye
DISCUSSION
The pupil light reflex is mediated by retinal ganglion cells which project directly to the pretectum. Lesions of the optic nerve, chiasm and tract therefore all produce loss of both visual perception and pupil light responses in corresponding areas of the visual field3. In the three patients described here, pupil perimetry confirmed normal function in allegedly blind areas of the visual field, thereby providing objective evidence of the functional nature of their visual field loss. There are reports that retrogeniculate lesions can also affect the pupil light reflex4. This is an indirect influence presumably mediated by corticotectal pathways, but because the anatomy is not yet understood we would not recommend the use of pupil perimetry to distinguish functional from organic field loss in these cases.
Pupil perimetry was originally developed to replace conventional perimetry in the assessment of patients with genuine visual field defects. However, its sensitivity is limited by the need for a larger size, intensity and duration of stimulus than used in conventional threshold perimetry, and greater variability in the measurements5. Furthermore, its use is limited by the need to exclude all patients with midbrain lesions, parasympathetic neuropathy, and orbital or ocular conditions that could affect the pupil measurements. The most useful applications of the technique are in patients unable to perform conventional perimetry, or in whom the visual loss is thought to be functional. A larger series of patients would be required to establish the sensitivity and specificity of this technique.
We conclude that, in patients with presumed functional visual field loss where the pattern is not consistent with retro-chiasmal disease, pupil perimetry can provide objective evidence for normal visual fields, thus circumventing the need for time-consuming and expensive investigations.
References
- 1.Kardon RH, Kirkali PA, Thompson HS. Automated pupil perimetry: pupil field mapping in patients and normal subjects. Ophthalmology 1991;98: 485-96 [DOI] [PubMed] [Google Scholar]
- 2.Bremner FD, Shallo-Hoffmann J, Riordan-Eva P, Smith SE. Comparing pupil function with visual function in patients with Leber's hereditary optic neuropathy. Invest Ophthalmol Vis Sci 1999;40: 2528-34 [PubMed] [Google Scholar]
- 3.Yoshitomi T, Matsui T, Tanakadate A, Ishikawa S. Comparison of threshold visual perimetry and objective pupil perimetry in clinical patients. J Neuro-Ophthalmol 1999;19: 89-99 [PubMed] [Google Scholar]
- 4.Cibis GW, Campos EC, Aulhorn E. Pupillary hemiakinesia in suprageniculate lesions. Arch Ophthalmol 1975;93: 1322-7 [DOI] [PubMed] [Google Scholar]
- 5.Hong S, Narkiewicz J, Kardon RH. Comparison of pupil perimetry and visual perimetry in normal eyes: decibel sensitivity and variability. Invest Ophthalmol Vis Sci 2001;42: 957-65 [PubMed] [Google Scholar]