Metastatic sepsis is a life-threatening complication of pyogenic liver abscess. Usually, only a single extrahepatic site is affected.
CASE HISTORY
A Chinese man aged 57 reported fever and malaise of one week's duration, associated with abdominal discomfort and a loss of appetite. 4 years previously he had been found to have non-insulin-dependent diabetes mellitus, complicated by retinopathy and neuropathy. Nothing remarkable was found on clinical examination. His white cell count was raised at 18.1 × 109/L and liver function tests showed an albumin of 22 g/L, serum bilirubin 26 μmol/L, alanine aminotransferase 23 U/L, aspartate aminotransferase 37 U/L and alkaline phosphatase 69 U/L. A chest radiograph was normal.
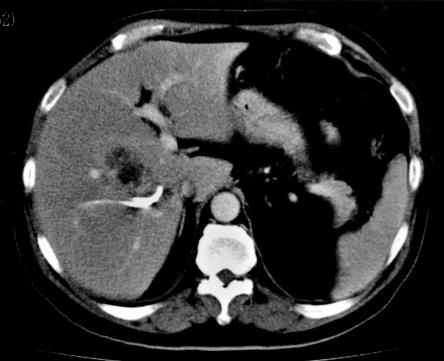
Ultrasound of the hepatobiliary system revealed a 5 cm lesion in the right lobe of the liver, and CT of the abdomen showed this to be a loculated abscess in segment V. The abscess was drained percutaneously. Blood cultures and pus cultures from the abscess yielded Klebsiella pneumoniae. He was treated with intravenous ciprofloxacin and metronidazole and initially there was a good response with resolution of fever. However, the patient deteriorated on the seventh day after percutaneous drainage, with hypotension, spiking fever and urinary frequency. He also developed a persistent unproductive cough. A repeat chest radiograph revealed multiple cavitating lesions in the right lung suggestive of abscesses, and lower respiratory cultures were positive for Klebsiella. On urine microscopy there were 15 white cells per high power field, with micro-organisms. Repeat CT of the abdomen and pelvis showed adequate drainage of the liver abscess (Figure 1) but multiple prostatic abscesses (Figure 2). These were drained transurethrally and cultures grew Klebsiella with superimposed Morganella morganii. Since the Morganella was resistant to ciprofloxacin, intravenous aztreonam was added to the antibiotic regimen. Treatment for the lung abscesses also included supplemental oxygen and intensive chest physiotherapy.
Figure 1.
Liver abscess drained via a percutaneous catheter (day 7) inserted under ultrasound guidance
Figure 2.
Bilobar prostatic abscess metastatic from liver abscess
The fever and symptoms gradually subsided over the next seven days. He was switched to oral ciprofloxacin for another four weeks and then discharged. Follow-up CT at three months showed complete resolution of the lung, liver and prostatic abscesses.
COMMENT
Although pyogenic abscesses commonly result in septicaemia, subsequent formation of septic foci is rare1. When it occurs, it is usually confined to a single extrahepatic site2, though multiple sites have been described3. For unknown reasons the commonest remote site of infection from a metastatic pyogenic liver abscess is the eye. Endogenous endophthalmitis occurs in up to 61% of patients with disseminated sepsis1, and can lead to grave visual loss4. Warning signs are orbital pain, blurring of vision and conjunctival chemosis. Other sites of visceral involvement are lung and brain.
What is the explanation for this metastatic phenomenon? First, it seems to be related to the virulence of the gram-negative organism K. pneumoniae, which is the main organism isolated from pyogenic liver abscesses in Asia5 and is also on the rise in western countries6. The underlying nature of its virulence remains unclear; the serotype K1 is reported to be particularly associated with metastatic endophthalmitis7. Secondly, these patients tend to have underlying diabetes mellitus. Two-thirds of the patients in the series of Cheng et al. had this comorbidity. Diabetic patients have impaired chemotaxis, phagocytosis and bactericidal function. The intimal vascular abnormality seen in diabetes may also contribute to haematogenous seeding. Thirdly, diagnosis and treatment are often delayed because of a subtle clinical presentation4 with only vague abdominal symptoms.
Awareness of the natural history of Klebsiella liver abscess in diabetic patients is important for clinical management. To detect extrahepatic sites of involvement, repeated imaging and cultures should be considered if fever or leucocytosis persist after initial treatment.
References
- 1.Cheng DL, Liu YC, Yen MY, Liu CY, Wang RC. Septic metastatic lesions of pyogenic liver abscess. Arch Intern Med 1991;151: 1557-9 [PubMed] [Google Scholar]
- 2.Liu YC, Cheng DL, Lin CL. Klebsiella pneumonia liver abscess associated with septic endophthalmitis. Ann Intern Med 1986;146: 1913-16 [PubMed] [Google Scholar]
- 3.Wang JH, Liu YC, Lee SSJ, et al. Primary liver abscess due to Klebsiella pneumonia in Taiwan. Clin Infect Dis 1998;26: 1424-8 [DOI] [PubMed] [Google Scholar]
- 4.Tan YM, Chong CK, Chow PKH. Pyogenic liver abscess complicated by endogenous endophthalmitis. Aust NZ J Surg 2001;71: 744-6 [DOI] [PubMed] [Google Scholar]
- 5.Chu KM, Fan ST, Lai ECS, Lo CM, Wong J. Pyogenic liver abscess. Arch Surg 1996;131: 148-52 [DOI] [PubMed] [Google Scholar]
- 6.Huang CJ, Pitt HA, Lipsett PA, et al. Pyogenic hepatic abscess. Changing trends over 42 years. Ann Surg 1996;223: 600-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fung CP, Chang YF, Lee SC, et al. A global emerging disease of Klebsiella pneumoniae liver abscess: is serotype K1 an important factor for complicated endophthalmitis? Gut 2002;50: 420-4 [DOI] [PMC free article] [PubMed] [Google Scholar]