Abstract
Despite a high prevalence of alcohol-related disabilities and the availability of cost-effective interventions, alcohol abuse and dependence commonly go undetected in hospital inpatients. In a university teaching hospital we compared three well validated screening methods for sensitivity and specificity—the Alcohol Use Disorders Identification Test (AUDIT, with various cut-off scores), CAGE (a four-question screening tool), and a 10-question version of the Michigan Alcoholism Screening Test (BMAST). A subset of patients also completed the DSM IV structured clinical interview for diagnosis. 1133 adult patients were randomly selected from all hospital admissions, with exclusion of day cases and patients too ill to be interviewed.
Two-thirds of the patients were interviewed, most of the remainder being unavailable at the time. 30% of the men and 8% of the women met the DSM IV criteria for alcohol abuse or dependence. Sensitivities and specificities of the screening tools were as follows: AUDIT (with cut-off score >8) 89% and 91%; CAGE 77% and 99%; BMAST 37% and 100%. 255 case records of patients scoring above the cut-off on one or more questionnaires were subsequently reviewed. The admitting team recognized an alcohol problem in only 46, of whom 17 were referred for appropriate follow up.
As in previous hospital surveys, alcohol abuse and dependence was not receiving proper attention. The most efficient screening tool was the CAGE questionnaire.
INTRODUCTION
Hospital-based surveys indicate that up to one-third of men admitted to medical and surgical wards have alcohol-related problems1. In patients attending accident and emergency the figure may be as high as 40%3,4.
The effectiveness of brief single-session interventions is well recognized. In a UK study, male inpatients who were identified as having problem drinking showed substantial improvement over the subsequent year after a single counselling session with an experienced nurse.5 The cost of the intervention was about £50 per session but the savings in terms of medical care were much greater. Similar results have been reported in general practice6.
Despite the availability of simple screening tools and low-cost interventions few populations are routinely screened for excessive alcohol use6,7,8. Because of the high prevalence in hospital patients both the Royal College of Physicians9 and the Royal College of Psychiatrists10 have recommended that every inpatient should be screened with a questionnaire such as the CAGE, for alcohol-related problems. In a university teaching hospital we have conducted a study with the following objectives: (a) to quantify the prevalence of alcohol abuse and dependence among inpatients; (b) to compare the sensitivity and specificity of three well-validated screening tools in the detection of alcohol abuse and dependency; (c) to assess current rates of identification by medical staff and referral for treatment.
METHODS
The study was conducted in the Mater Misericordiae Hospital, Dublin, in the last seven months of 1999. The three screening questionnaires chosen for comparison were: the Alcohol Use Disorders Identification Test (AUDIT)11, the CAGE questionnaire12 and the ‘brief’ 10-question version of the 25-item Michigan Alcoholism Screening Test (BMAST)13. The AUDIT is a 10-item questionnaire designed by the World Health Organization to screen for current ‘hazardous or harmful’ alcohol intake. The range of possible scores is 0-40. The cut-off score is greater than 811,14,15. It can be completed in less than three minutes and is reported to have a sensitivity of >90% in medical inpatients with a positive predictive value of 60%16,17. The CAGE is a four question-screening tool which identifies people with a lifetime risk of alcohol abuse or dependence. A point is scored for each positive answer and a score of 2 or more indicates probable alcohol abuse12. Sensitivities of >80%, specificities >85% and a positive predictive value of 82% have been reported4,17,18. The BMAST assesses lifetime prevalence of alcoholism. A score of 5 or more indicates probable alcohol dependence13. The BMAST questionnaire is reported as having low sensitivity (35%)17 in general patient populations but a high specificity for alcohol dependence syndrome (>88%)4,19.
Patients were selected daily from all hospital admissions by means of a table of random numbers. Day cases were excluded because the admission was too brief to allow assessment. Patients admitted to the coronary care or intensive care units, or who were too ill or confused to be interviewed, were also excluded. A single trained researcher (AC) interviewed the patients selected, using the AUDIT, CAGE, and BMAST screening questionnaires. The group of patients interviewed were not identified to their admitting team.
In addition to completing the screening questionnaires, all patients presenting in the four months between 1 September and 31 December who scored above the standard cut-off points on one or more of the questionnaires, and a sample of patients who did not score above any cut-off point, completed the Structured Clinical Interview for Diagnosis20 (SCID) of the American Psychiatric Association's Diagnostic and Statistical Manual, 4th edition (DSM IV) to confirm the diagnosis. The case notes of all patients who scored above the standard cut-off points on one or more of the questionnaires were reviewed to ascertain whether the admitting team had identified potential alcohol-related problems and referred the patient for appropriate follow-up.
RESULTS
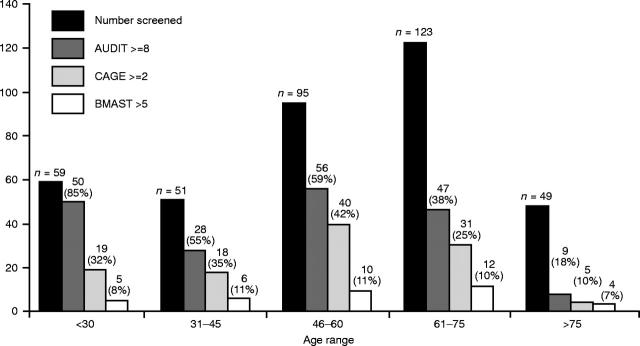
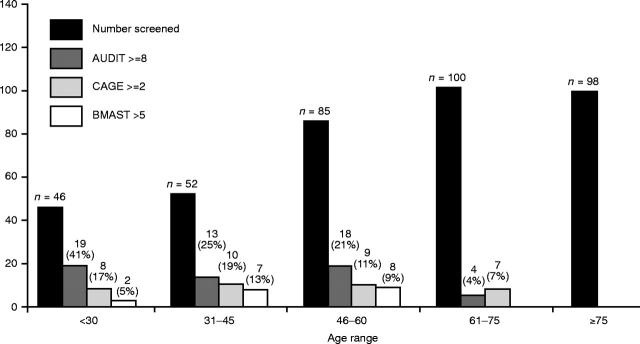
1133 patients were selected and 759 (67%) were interviewed (378 men, 381 women). 315 were either not available (e.g. in theatre, or having investigations) or had been discharged; 43 were too ill to be interviewed; 5 had died; 5 were not interviewed because of a communication difficulty; 3 had been admitted twice and were not reinterviewed; and 3 refused. Of the 759 patients interviewed, 273 (36%, 213 men and 61 women) scored above the cut-off point on one or more of the questionnaires. Figures 1 and 2 summarize the results in men and women.
Figure 1.
Number and age distribution of men scoring at or above the standard cut-off points on the questionnaires
Figure 2.
Number and age distribution of women scoring at or above the standard cut-off points on the questionnaires
424 patients were interviewed between 1 September and 31 December. Of the 134 who scored above the cut-off point on one or more of the questionnaires 37 (28%) were diagnosed (DSM IV) as alcohol abusers (28 men, 9 women) and 42 (31%) as having alcohol dependence syndrome (36 men, 6 women); in other words, 59% of patients who scored above a cut-off point were alcohol abusers or dependent on alcohol. None of the 28 patients scoring below the cut-off points on all questionnaires were so diagnosed. 19% of all patients screened between 1 September and 31 December met the DSM IV criteria for alcohol abuse or dependence. Table 1 compares the sensitivity, specificity and positive predictive value of the three questionnaires.
Table 1.
The sensitivity, specificity and positive predictive value of the three questionnaires (n=424)
|
SCID
|
||||||||
|---|---|---|---|---|---|---|---|---|
| Screening questionnaire | Cut-off score | No. with less than cut-off score | Abuse | Dependence | Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Efficiency |
| CAGE | > =2 | 70 (16%) | 24 | 37 | 77 | 99 | 94 | 95 |
| AUDIT | > 8 | 111 (26%) | 34 | 36 | 89 | 91 | 70 | 90 |
| > 10 | 74 (17%) | 26 | 33 | 75 | 97 | 84 | 93 | |
| > 12 | 55 (13%) | 19 | 30 | 60 | 98 | 88 | 91 | |
| BMAST | > =5 | 30 (7%) | 5 | 25 | 37 | 100 | 100 | 88 |
255 (93%) of the case records of patients scoring above the cut-off point on one or more questionnaires were subsequently examined. Of these, 80% had some reference to alcohol consumption in the admission note (e.g. ‘C2H5OH socially’ or ‘C2H5OH++’). However, only 46% had a record of actual weekly or daily consumption. A questionnaire was used in 3 admissions (CAGE). In only 46 (18%) was an alcohol problem recognized by the admitting team. In two-thirds of these the alcohol problem was either the primary complaint or directly related to the presenting medical condition. The alcohol problem was only recorded in 64% of the discharge summaries of patients where the problem had been recognized. Just 17 of those recognized were referred for follow-up of their alcohol problem.
DISCUSSION
Our findings are consistent with previous studies on the prevalence (and lack of recognition) of alcohol-related disorders in acute hospital inpatients4. We have, however, highlighted important potential drawbacks of the AUDIT questionnaire, currently the most widely promoted screening tool for detection of alcohol misuse. Developed by the World Health Organization for use in primary care, AUDIT is a ten-item self-administered questionnaire which can be cumbersome in busy medical settings. A cut-off score of 8 or more is recommended for the detection of hazardous drinking (defined as > 14 units per week for women and > 21 units per week for men). In our study the AUDIT with standard cut-off score identified up to 28% of inpatients as hazardous drinkers. When used to specifically identify patients who satisfy DSM IV criteria for alcohol abuse (where secondary alcohol-related problems have developed) or alcohol dependence (physiological dependence) the AUDIT had a false-positive rate of 30%. 85% of men under the age of thirty had an AUDIT score of 8 or more with a specificity (for a DSM IV diagnosis) of less than 47%. The AUDIT therefore had high sensitivity in this population but lacked sufficient specificity to be practical for the purpose of screening for alcohol abuse/dependence. Increasing the cut-off score to greater than 10 substantially improved the specificity with only a modest reduction in sensitivity. The sensitivity with a cut-off score of 12 was unacceptably low.
The CAGE has distinct advantages as a screening tool in the acute hospital setting. It is a simple four-item questionnaire which can quickly be administered by the admitting house officer. In the present study the CAGE questionnaire, with the standard cut-off score of 2, identified 16% of inpatients as having a probable DSM IV diagnosis of alcohol abuse or dependency with a false positive rate of only 6%. Used in this way, CAGE provides good case/non-case discrimination for alcohol abuse/dependence syndrome. In a previous study, MacKenzie et al. tested CAGE with a cut-off score of 1 as a means to detect hazardous drinking behaviour. A high false-positive rate suggested that the CAGE is an impractical screening tool for the detection of hazardous drinking that does not fulfil DSM IV criteria.
Our results with the BMAST questionnaire are consistent with those of others in that it has high specificity for alcohol dependence syndrome but a low sensitivity that makes it unsuitable as a screening tool in general inpatients.
Alcohol co-morbidity continues to be neglected in acute medical conditions. Although in this study admitting doctors enquired about alcohol consumption in 80% of admissions they recorded actual consumption in only 46%. Screening questionnaires were rarely used. The admitting medical team recognized only 18% of patients with probable alcohol problems and a minority of those were referred for appropriate follow up. If a patient's alcohol problem was not directly related to the presenting complaint it was unlikely to be recognized. Even where a serious alcohol problem was recognized it was recorded in only two-thirds of discharge summaries, which has implications for inpatient activity statistics and resource allocation.
Why are patients with alcohol-related problems so seldom identified and referred? Doctors may underestimate the importance of alcohol as a co-morbid risk factor and fail to understand the benefits of early brief interventions. There may also be uncertainty in the accurate quantification of alcohol consumption and a lack of awareness of the efficiency of existing screening tools. Alternatively there may be a lack of local resources for the treatment of excessive alcohol consumption. To be successful, a strategy aimed at health promotion and secondary prevention of alcohol related disabilities in the general hospital must address several issues. First, doctors and other health professionals need to become more aware of the importance of alcohol consumption as a co-morbid risk factor. Second, all inpatients should be systematically screened for excessive alcohol consumption. The choice of screening tool will depend on whether all inpatients with hazardous drinking behaviour are to be identified or whether screening is to identify inpatients with established alcohol-related problems. Little work has been done on the relative cost-effectiveness of intervention aimed at primary (hazardous drinking) versus secondary (DSM IV criteria) prevention.
Acknowledgments
This study was supported by Merck Pharmaceuticals.
References
- 1.UK Alcohol Forum. Guidelines for the Management of Alcohol Problems in Primary Care and General Psychiatry. Tangent Medical Education; 1997
- 2.Conniffe D, McCoy D. Alcohol Use in Ireland: Some Economic and Social Implications. Dublin: ESRI; 1993
- 3.Conigrave K, Burns FH, Reznik RB, Saunders JB. Problem drinking in emergency department patients: the scope for early intervention. Med J Aust 1991;154: 801-5 [DOI] [PubMed] [Google Scholar]
- 4.Soderstrom CA, Smith GS, Kufera JA, et al. The accuracy of the CAGE, the Brief Michigan Alcoholism Screening Test, and the Alcohol Use Disorders Identification Test in screening trauma center patients for alcoholism. J Trauma 1997;43: 962-9 [DOI] [PubMed] [Google Scholar]
- 5.Chick J, Lloyd G, Crombie E. Counselling problem drinkers in medical wards: a controlled study. BMJ Clin Res 1985;290: 965-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wallace P, Cutler S, Haines A. Randomised controlled trial of general practitioner intervention in patients with excessive alcohol consumption. BMJ 1988;297: 663-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: a review. Addiction 1993;88: 315-35 [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization Brief Intervention Study Group. A cross-national trial of brief intervention with heavy drinkers. Am J Publ Health 1996;86: 948-55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Royal College of Physicians. A Great and Growing Evil: the Medical Consequences of Alcohol Abuse. London; Tavistock, 1987
- 10.Royal College of Psychiatrists. The Psychological Care of Medical Patients: Recognition of Need and Service Provision. London: Tavistock, 1995 [PMC free article] [PubMed]
- 11.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption—II. Addiction 1993;88: 791-804 [DOI] [PubMed] [Google Scholar]
- 12.Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA 1984;252: 1905-7 [DOI] [PubMed] [Google Scholar]
- 13.Pokorny AD, Miller BA, Kaplan HB. The brief MAST: a shortened version of the Michigan Alcoholism Screening Test. Am J Psychiatry 1972;129: 342-5 [DOI] [PubMed] [Google Scholar]
- 14.Saunders JB, Aasland OG, Amundsen A, Grant M. Alcohol consumption and related problems among primary health care patients: WHO collaborative project on early detection of persons with harmful alcohol consumption—I. Addiction 1993;88: 349-62 [DOI] [PubMed] [Google Scholar]
- 15.Conigrave KM, Hall WD, Saunders JB. The AUDIT questionnaire: choosing a cut-off score. Alcohol Use Disorders Identification Test. Addiction 1995;90: 1349-56 [DOI] [PubMed] [Google Scholar]
- 16.Piccinelli M, Tessari E, Bortolomasi M, et al. Efficacy of the alcohol use disorders identification test as a screening tool for hazardous alcohol intake and related disorders in primary care: a validity study. BMJ 1997;314: 420-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mackenzie D, Langa A, Brown TM. Identifying hazardous or harmful alcohol use in medical admissions: a comparison of audit, cage and brief mast. Alcohol Alcoholism 1996;31: 591-9 [DOI] [PubMed] [Google Scholar]
- 18.Chan AW, Pristach EA, Welte JW. Detection by the CAGE of alcoholism or heavy drinking in primary care outpatients and the general population. J Substance Abuse 1994;6: 123-35 [DOI] [PubMed] [Google Scholar]
- 19.Chan AW, Pristach EA, Welte JW. Detection of alcoholism in three populations by the brief-MAST. Alcoholism: Clin Exp Res 1994;18: 695-701 [DOI] [PubMed] [Google Scholar]
- 20.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I). American Psychiatric Press, 1997