Abstract
Emergency telephone calls for an ambulance (999 calls) are usually dealt with first-come first-served. We have devised and assessed criteria that ambulance dispatch might use to prioritize responses. Data were collected retrospectively on consecutive patients presenting to an accident and emergency (A&E) department after a 999 call. An unblinded researcher abstracted data including age, date, time, caller, location, reason for call and A&E diagnosis and each case was examined for ten predetermined criteria necessitating an immediate ambulance response—namely, cardiac arrest; chest pain; shortness of breath; altered mental status/seizure; abdominal/loin pain >65 years old; fresh haematemesis; fall >2m; stabbing; major burns.
471 patients were recruited, 55% male, median age 50 years. 406 calls came from bystanders or the patients themselves, 36 from general practitioners, 8 from other hospitals and 21 from the police. 52% of patients were admitted. 44% met at least one of the above criteria.
Most patients did not meet the criteria for an immediate ambulance response but might nonetheless be suitable for an urgent response. The criteria used in this study have the advantage of being based on the history provided by the caller. The introduction of a priority-based dispatch system could reduce response times to those who are seriously ill, and also improve road safety.
INTRODUCTION
The emergency ambulance service was originally designed to provide an immediate response to those with a serious illness or injury. In the Tayside area, demand for emergency ambulances (999 calls) increased from 18 645 calls in 1996-1997 to 22 222 calls in 1999-2000—a 19% rise that was not matched by an increase in resources. At present, in many regions of the UK, all 999 calls demand immediate response from ambulance crews since there is no system in place for prioritization. As a result, calls are dealt with first-come first-served, whatever the nature of the complaint. There is some evidence that many of these calls are inappropriate1,2,3 and delay the response to patients with true emergencies. Various endpoints have been used to judge the appropriateness of the call—for example, clinical diagnosis, interventions and hospital admission1,2,3,4,5,6—but these criteria require medical assessment and will not help an ambulance dispatcher in triage. There are no published studies in which a lay person's description of symptoms is used as a triage tool. This would be a more pragmatic approach, since it requires no medical knowledge on the part of the caller.
The aim of this pilot study is to evaluate the appropriateness of 999 calls for patients attending an accident and emergency (A&E) department by applying triage criteria that might realistically be used by ambulance dispatch.
METHODS
The study was conducted in the A&E department of a teaching hospital which sees 65 000 new attendances each year and which serves a population of 250 000. Data were collected over three separate 7 day periods between January and February 2001. Before data collection, a set of triage criteria was devised which the authors considered encompassed those conditions requiring emergency transport to hospital—namely, cardiac arrest; chest pain; shortness of breath; altered mental status/seizure; abdominal/loin pain >65 years old; fresh haematemesis; fall >2m; stabbing; major burns. The criteria were based on symptoms or mechanisms of injury that could potentially be identified by the person making the 999 call.
The prehospital report forms (PRF) and A&E records of all patients brought by ambulance to the department during this time were then examined and details were recorded on a proforma. Only those patients brought by emergency ambulance were included in the study: urgent transports were excluded. The age and sex of the patient, time and location of the incident, person identified as calling the ambulance and reason for request were noted from the PRF. The A&E records were reviewed for diagnosis and disposal of the patient. The worst documented respiratory rate, heart rate and blood pressure were also collected from PRF and A&E notes. The presenting condition of the patient was then compared with the triage criteria to evaluate whether or not the patient had a condition requiring immediate transport to hospital.
RESULTS
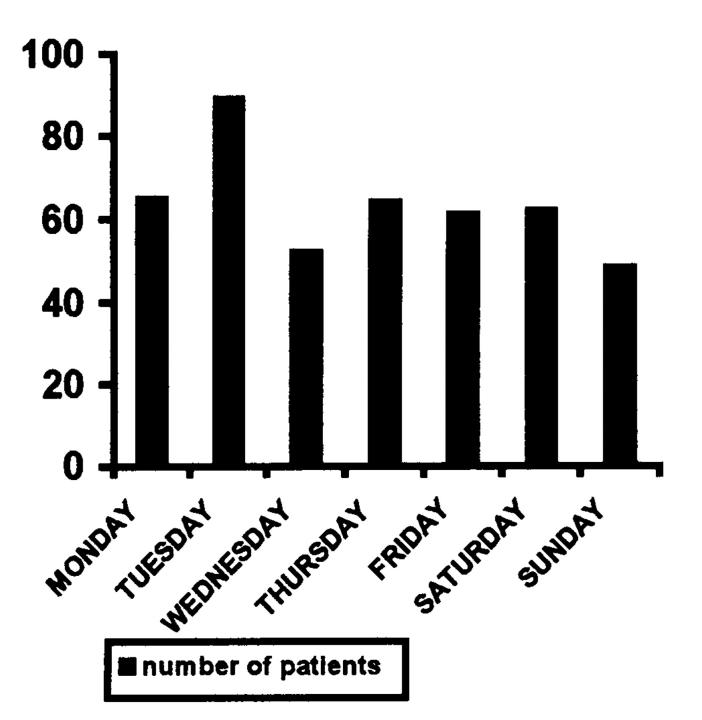
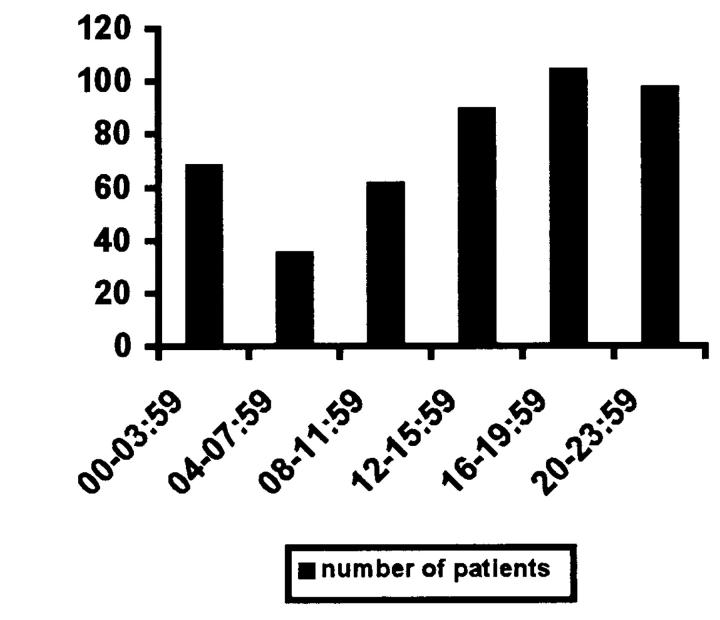
Over the 21-day period 471 patients were brought to A&E by an emergency ambulance following a 999 call. Attendance was highest on Tuesdays, with a roughly even spread over the rest of the week (Figure 1). There were more attendances between 4pm and midnight than during the remainder of the day (Figure 2). 55% of patients were male; mean age was 49, median 50 years. 86% of calls were initiated by bystanders or patients themselves, 7.6% by general practitioners, 1.6% by other hospitals and 4.4% by the police. 249 patients (52%) were admitted, 180 were discharged, 20 were given outpatient appointments and 12 took their own discharge from hospital.
Figure 1.
Day of attendance
Figure 2.
Time of attendance
210 patients (44.5%) fulfilled one or more of the predetermined triage criteria (Table 1). Altered mental status was the most common criterion to be met, followed by chest pain and shortness of breath. 53 of the 72 patients with altered mental status actually had a Glasgow coma score (GCS) of less than 15 on arrival in A&E. There were no patients with a reduced GCS in the group not meeting triage criteria. 24 patients had a systolic blood pressure below 100 mmHg; 4 of these were in the group not meeting the triage criteria. None of these patients had an abnormal heart rate or reduced conscious level; one had biliary colic, one had a fractured humerus, one had a fractured distal radius and the other had taken an overdose. 67% of the patients who met the triage criteria were admitted to hospital compared with 41% of those not meeting the criteria.
Table 1.
Number of patients who met triage criteria
| Triage criteria | No. |
|---|---|
| Cardiac arrest | 4 |
| Chest pain | 56 |
| Shortness of breath | 29 |
| Drowsiness or seizure | 70 |
| Fall greater than 2 m | 4 |
| Road traffic accident | 30 |
| Penetrating injury | 4 |
| Abdominal pain, over 65 years of age | 7 |
| Extensive burn | 0 |
| Fresh haematemesis | 2 |
Diagnoses in patients not meeting the criteria are shown in Table 2. Most were soft tissue injuries, limb injuries or head/facial injuries with normal conscious levels. Alcohol intoxication was a primary diagnosis in 14 patients; overall, 87 patients were affected by alcohol. The patients attending with smoke inhalation had been exposed only briefly, were not short of breath and were fully conscious; they were all discharged from the A&E department. Both patients diagnosed with diabetic acidosis had a normal conscious level on arrival at A&E. The hypoglycaemic patient had been given glucose before the ambulance was called and was recovering by the time the crew arrived.
Table 2.
Diagnoses of patients not meeting triage criteria for emergency ambulance
| Diagnosis | No. |
|---|---|
| STI/burn/wound | 44 |
| Head/facial injury GCS 15 | 43 |
| Fractured limb | 40 |
| OD/DSH | 24 |
| Alcohol intoxication | 14 |
| Abdominal pain | 12 |
| Collapse unknown cause, fully conscious | 12 |
| CVA/TIA, fully conscious | 8 |
| Smoke inhalation not short of breath | 8 |
| Chest wall injury | 7 |
| Seizure, fully recovered | 6 |
| Infection | 6 |
| Anxiety | 5 |
| Epistaxis | 4 |
| Mild pulmonary oedema | 3 |
| Headache unknown cause, fully conscious | 3 |
| COPD | 2 |
| Gastrointestinal bleed | 2 |
| Renal colic | 2 |
| Haemoptysis | 2 |
| Constipation | 2 |
| DKA or HONK | 2 |
| Arrhythmia | 1 |
| Hypoglycaemia | 1 |
| Fall, no injury | 1 |
| Corneal abrasion | 1 |
| STI=soft tissue injury; GCS=Glasgow coma score; OD=overdose; DSH=deliberate self harm; CVA=cerebrovascular accident; TIA=transient ischaemic attack; COPD=chronic obstructive pulmonary disease; DKA=diabetic ketoacidosis; HONK=hyperosmolar non-ketotic acidosis | |
DISCUSSION
The response to true emergency calls can be delayed if an ambulance is dealing with some minor incident. An immediate response puts ambulance personnel and other road users at risk and may make no difference to the outcome of the patient.
Currently there is a statutory obligation for the ambulance service to arrive on scene in 7 minutes for 50% of emergency calls, and in 14 minutes for 90% of calls. Reviewing Ambulance Performance Standards in 1996, the NHS Executive suggested that if 90% of life-threatening calls were answered within 8 minutes then an additional 300 000 patients would receive care within this critical time frame7. If ambulances responded to 90% of cardiac arrests within 8 minutes then a further 3200 patients would survive, half of whom would be aged less than 70. In a recent cohort study of 10 654 patients with out-of-hospital cardiac arrest, Pell et al. concluded that reduction of ambulance response times to 5 minutes could almost double survival rates in arrests not witnessed by ambulance personnel8. Ambulance personnel must therefore be relieved of inappropriate requests for an emergency response so that they can deal promptly and effectively with patients genuinely requiring immediate care.
The key issue is to direct emergency ambulances to the right patients in an appropriate timeframe. However, parallel issues are equally important—in particular, the safety of the attending crew. From April 2000 to April 2001 there were 328 road traffic accidents involving ambulance vehicles (Scottish Ambulance Statistics). Undoubtedly if the number of immediate responses was reduced to deal only with those patients in genuine need of ‘blue lights and sirens’, then the number of ambulance vehicle accidents would fall, and crew safety would improve.
The fact that many requests for immediate response are not appropriate is already recognized and acknowledged. Our conclusion that 55% of calls for emergency ambulances do not merit an immediate response reflects findings in other studies2,3,4,5,6,7,8,9. Reviewing ten studies Snooks et al. found that nine reported inappropriate use in 30-50% of patients brought to A&E departments by 999 ambulance10. But ‘inappropriate use’ can be difficult to define. Many studies have used retrospective and subjective opinion based on evaluations by ambulance personnel or medical staff1,9,11. Others have used admission to hospital as an endpoint—though admission to hospital does not translate into the need for an immediate transfer. In a study of paediatric patients brought to hospital by ambulance, Kost et al. used a set of criteria based on the medical records following attendance to the emergency department to assess whether an emergency ambulance was justified, and found that in 28% of cases it was not5. While these studies illustrate that a sizeable proportion of 999 requests are inappropriate, they start at the point of knowing the patient's diagnosis and make a judgment from there. A practical solution has to be based on the caller's description of the problem.
This study may be criticized on several grounds: data abstraction was unblinded; the investigation was retrospective and the sample was small; our taking the reason for calls from the PRF was not ideal, but listening to taped transcripts of all calls was not feasible. The results should be viewed as pilot data providing groundwork for further studies. Such studies should be prospective with criteria applied consistently and follow-up in terms of patient outcome and acceptability to patients and medical staff.
It has been suggested that there is a void in public education and awareness of how to use the emergency ambulance service11. However, it is unreasonable to expect a layperson caller to make an informed judgment on level of response required. Many ‘inappropriate’ 999 calls are perceived as justified by the caller3. A system is therefore needed which allows a decision to be made by the ambulance dispatcher based on the information available at the time of the call. Predetermined criteria such as those described in this study, which can be easily understood by the caller and which represent symptoms that may require immediate transfer to hospital, are a practical solution. This then empowers the ambulance dispatcher to decide where best to disperse resources, directing emergency ambulance to those needing immediate attention, and arranging a response in an appropriate timeframe (e.g. 30 minutes) to those needing urgent transfer only. Triage criteria must be effective in excluding those calls which do not require an emergency response yet be safe enough to ensure that patients who genuinely need a rapid response are not missed. They therefore tend to be over-inclusive so as to be safe. This would appear to be the case in this study where 23% of patients warranting an immediate dispatch were discharged without admission.
The emergency response system may be better served by a two-tier response—immediate or urgent. This would allow the ambulance service to respond to more true emergencies within 8 minutes. Restriction of blue lights and siren responses to genuine emergencies would also improve road safety.
References
- 1.Gardner GJ. The use and abuse of the emergency ambulance service: some of the factors affecting the decision to call an emergency ambulance. Arch Emerg Med 1990;7: 81-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O'Leary Bury G, McCabe M, et al. Ambulance user analysis in an accident and emergency department. Ir Med J 1987;80: 422-3 [PubMed] [Google Scholar]
- 3.Victor CR, Peacock JL, Chazot C, Walsh S, Holmes D. Who calls 999 and why? A survey of the emergency workload of the London Ambulance Service. J Accid Emerg Med 1999;16: 174-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brown E, Sindelar J. The emergent problem of ambulance misuse. Ann Emerg Med 1993;22: 646-50 [DOI] [PubMed] [Google Scholar]
- 5.Kost S, Arruda J. Appropriateness of ambulance transportation to a suburban pediatric emergency department. Prehosp Emerg Care 1999;3: 187-90 [DOI] [PubMed] [Google Scholar]
- 6.Rademaker AW, Powell DG, Read J. Inappropriate use and unmet need in paramedic and non-paramedic ambulance systems. Ann Emerg Med 1987;16: 553-6 [DOI] [PubMed] [Google Scholar]
- 7.Department of Health. Review of Ambulance Performance Standards. Final report of the Steering Group. London: NHS Executive, 1996
- 8.Pell JP, Sirrel JM, Marsden AK, Ford I, Cobbe AM. Effect of reducing ambulance response times on deaths from out of hospital cardiac arrest: cohort study. BMJ 2001;322: 1385-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morris DL, Cross AB. Is the emergency ambulance service abused? BMJ 1980;281: 121-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Snooks H, Wrigley H, George S, Thomas E, Smith H, Glasper A. Appropriateness of use of emergency ambulances. J Accid Emerg Med 1998;15: 212-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palazzo FF, Warner O, Harron M, Sadana A. Misuse of the London Ambulance Service: how much and why? J Accid Emerg Med 1998;15: 368-70 [DOI] [PMC free article] [PubMed] [Google Scholar]