Campbell Greig De Morgan was born at Clovelly near Bideford in 1811. After training at University College Hospital he became a house surgeon at the Middlesex Hospital where he remained for the rest of his career and life. He was said to have been ‘a man of great accomplishment and unusual ability’ and his interests extended beyond surgery. Thus he was actively involved in the Middlesex Hospital Medical School after its foundation in 1835 and worked closely with its founder, Sir Charles Bell. He became a lecturer in forensic medicine in 1841 and professor of anatomy in 1845, and in 1853 he was elected a Fellow of the Royal Society on the basis of a paper on the structure and development of bone. He also described the small benign dermal angiomas associated with advancing years which, to this day, are known as Campbell De Morgan spots.
De Morgan was said to have been a humble, unassuming and kind man of high moral character, somewhat reticent, totally indifferent to worldly success and held in high esteem by his colleagues and students. He was a talented musician, with an interest in the science of music, and was a gifted caricaturist.
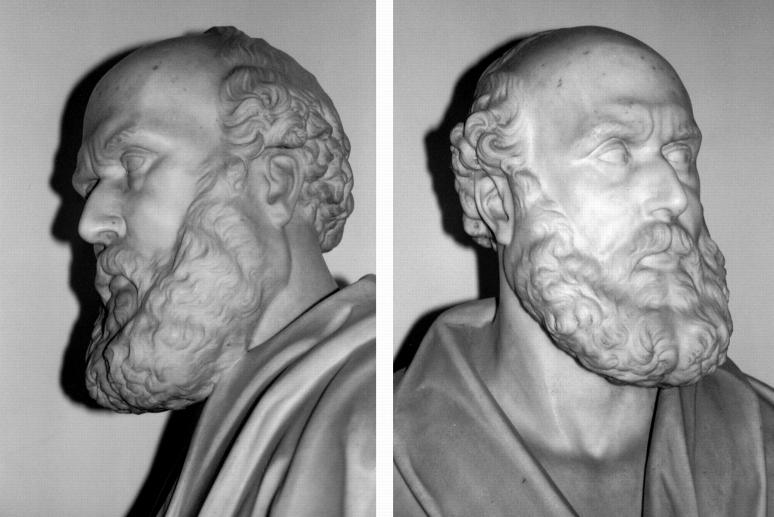
His death in 1876 was the result of a characteristic act of kindness and caring. In March of that year his friend the artist John Graham Lough presented the Middlesex Hospital with a marble bust (Figure 1) of De Morgan as ‘a token of affection and gratitude’. Just a few days later, Lough became critically ill with pneumonia and De Morgan, whose own state of health had become a cause of anxiety to his colleagues, sat by his friend's bed throughout the night of 6 April, until his death the following morning. As a result, De Morgan himself developed pneumonia and pleurisy from which he died on 12 April, in the presence of one of his two sons. As recorded in his obituary, ‘Few can doubt that in this last act of friendly devotion Campbell De Morgan sacrificed his own life. Greater love hath no man than this’.
Figure 1.
Bust of Campbell De Morgan, presented to the Middlesex Hospital by John Graham Lough
THE FOCAL ORIGIN OF CANCER
Over 34 years De Morgan conducted a detailed clinical study of cancer and became a recognized authority on the subject. In a series of publications between 1871 and 1874 he argued, rationally and logically, that cancer arose locally and then spread, first to the lymph nodes and then further afield1,2,3. He stressed the great practical relevance of this to treatment: ‘Today the glands may be free; tomorrow they may be affected. Today all disease may be within range of an operation; tomorrow disease may be distributed far beyond’. De Morgan also noted that at the time of onset of cancer, the patient usually had no sign of constitutional disturbance.
The presentation by De Morgan of his thesis to the Pathological Society of London on 3 March 1874 led to a wide-ranging debate at that meeting and a further one on 21 April4. De Morgan's concept of the focal origin of cancer was opposed by Sir James Paget, who argued that the apparent hereditary nature of cancer implied that it was a constitutional disease, but others pointed out that an inherited disposition was not incompatible with a focal origin of the disease process. Indeed, De Morgan fully accepted that the local development of a tumour was influenced by host susceptibility factors. He remarked that, although irritation could cause cancer of the lip in pipe smokers or scrotal cancer in chimney sweeps, not all at such risk developed the disease—‘The majority will not become cancerous, irritate how you will’.
De Morgan received considerable support from Jonathan Hutchinson who, on the basis of his own extensive observations, favoured the focal origin of cancer. Hutchinson regarded cancer as a rebellion of the cells and compared cancerous cells to the Celts, ‘whose disposition it was to throw off the shackles of orderly government and to aggrandise themselves’.
There can be little doubt that the clear and concise reasoning of De Morgan and his presentation of his thesis to the Pathological Society of London settled the debate, that had raged for at least half a century, as to whether cancer was of generalized or focal origin. During the debate, one member of the audience, Dr Greenhow, drew attention to a close resemblance between cancer and tuberculosis—in the way that both began as local foci of disease and then spread to local lymph nodes and subsequently to many organs. Greenhow also noted that latent periods occurred in both disease processes and the similarity in the constitutional symptoms encountered in both diseases at their advanced states.
COLEY TOXINS
In his opening address to the Pathological Society, De Morgan referred to the fact that cancers occasionally underwent spontaneous regression—‘A remarkable and not very explicable phenomenon is the arrest of cancer growth and the gradual wasting of the diseased mass. This is an occasional event which is very important as it encourages us to hope that a cure may yet be found for the disease’. He added that the wasting of the tumour was not simply due to necrosis subsequent to obliteration of the blood vessels leading to it, although that undoubtedly did occur. In this context he noted that, in some cases, spontaneous regression of cancer was associated with infections and, particularly, with the onset of tuberculosis, although he added that there were insufficient data to be sure that the two diseases were antagonistic. He did, however, observe that cancer was uncommon in, and rarely coexisted in, families affected by tuberculosis.
Not long after De Morgan's death, other workers confirmed his observation that regressions and even complete resolutions of cancer were occasionally associated with severe infections, notably erysipelas5. One such observation was to have important consequences6. Dismayed by the dismal outcome of the surgical treatment of sarcoma, an American surgeon, William Coley, searched the records of patients with bone cancer for any clue as to how their outcome could be improved. This search revealed one patient regarded as being terminally ill who, after developing erysipelas caused by Streptococcus pyogenes, made a complete recovery. Coley's initial attempts to induce erysipelas therapeutically with locally isolated strains of S. pyogenes were unsuccessful. When, however, he used a more virulent strain obtained from Robert Koch in 1891, he successfully induced erysipelas in a patient with advanced sarcoma of the neck and to his (and presumably the patient's) delight the tumour disappeared completely.
As the use of live streptococci was beset with risks, Coley experimented with bacteria-free extracts and eventually found that a mixture of extracts of S. pyogenes and Serratia marcescens (‘Bacillus prodigiosus’) was as effective as living streptococci7. The use of this so-called Coley toxin gave impressive results but also led to acrimonious controversy, and by the early 1950s this form of therapy had ceased in the USA8.
Ironically, in 1953, around the time that Coley toxins were abandoned, tumour-specific antigens were discovered, and over the ensuing thirty years there were numerous attempts to treat cancer patients by various strategies designed to boost their immune reactions. The results were disappointing, and by 1986 enthusiasm had largely given way to despair and cynicism9. But in that year a new wave of interest was triggered by the first report of successful immunotherapy with autologous cytotoxic lymphocytes specific for the patient's tumour antigens10. This discovery raised hopes of developing vaccines against melanoma and other tumours, and research is currently being actively pursued in this field.
In retrospect, a major problem of the extensive work between 1953 and the late 1980s is that the immune responses in cancer were poorly understood and the aim of the various forms of immunotherapy was simply to boost immune responses. This is reminiscent of Sir Ralph Bloomfield Bonington's cry of ‘Stimulate the phagocytes’ in George Bernard Shaw's play The Doctor's Dilemma.
RATIONAL IMMUNOTHERAPY
Are we now at the stage when, in the light of advances in immunology and cell biology, the immunotherapy of cancer can evolve from an empirical art to a rational science? It is now realized that immune responses show considerable qualitative variation and that a given stimulus may generate a range of responses, some protective and some antagonistic to protection. An understanding of the qualitative differences in immune responses has been made possible by the discovery in the early 1990s that T helper cells mature along (at least) two distinct pathways, yielding Th1 and Th2 cells11. These T cell types produce or induce different cytokines and thereby affect a range of quite different immune reactions. Accordingly, it is now possible to analyse immune responses in detail and to design therapeutic strategies to induce protective responses and to down-regulate inappropriate ones.
In this context, there is increasing evidence that Th1 reactivity mediates protection against tumours and that many common cancers are associated, as either cause or effect, with immune dysregulation leading to a drift towards Th2 reactivity12,13,14. It has been postulated that rapid environmental changes in the industrialized nations favour immune dysregulation and a drift towards Th2 reactivity and this may account for the increase in the rates of cancer in these nations15. Furthermore, in the same context, protection against tuberculosis is likewise mediated by Th1 reactivity and patients with progressive disease show a Th2 drift16. This finding sheds light on Campbell De Morgan's speculation that there might be some relation between the host's responses to tuberculosis and cancer, and Greenhow's observation that the two diseases have features in common. One disease is characterized by intrinsically abnormal cells and the other by cells rendered abnormal by intracellular parasitism. Both diseases may progress relentlessly; but, especially in tuberculosis, even advanced and widespread disease may undergo spontaneous resolution. Also, in both cases there may be long periods of latency, suggesting that the disease processes are under some from of restrictive control. The similarities between tuberculosis and cancer suggest useful parallels in the design of immunotherapeutic measures against the two diseases17.
The above observations raise the question of whether Mycobacterium tuberculosis, BCG or other mycobacteria are able to induce useful degrees of anti-cancer immunity. Certainly there have been claims that BCG vaccination protects against cancer18. BCG has been used as a non-specific immune stimulant in the therapy of melanoma19, although with variable results, and is increasingly administered intravesically with good outcomes for the treatment of superficial bladder cancer20. In the latter case, the induction of Th1 immune response is essential to success. In the case of tuberculosis, however, it is clear that the ability of BCG to protect against this disease varies considerably from region to region, and in some regions BCG may even predispose to tuberculosis21. This considerable variation is illustrated by the results of some major BCG vaccination trials shown in Table 1. The variation seems to be due to contact with various populations of mycobacteria that live freely in the environment which, by sensitizing the human population, prime them for Th1 or Th2 responses. Accordingly, BCG vaccination of such sensitized populations may either confer protection against tuberculosis or antagonize protective responses.
Table 1.
The results of nine major BCG vaccine trials against tuberculosis
| Region | Year of start | Age range | Protection afforded (%) |
|---|---|---|---|
| North America* | 1935 | 0-20 years | 80 |
| Chicago, USA | 1937 | 3 months | 75 |
| Georgia, USA | 1947 | 6-17 years | 0 |
| Illinois, USA | 1948 | Young adults | 0 |
| Puerto Rico | 1949 | 1-18 years | 31 |
| Georgia, USA | 1950 | 5 years | 14 |
| Great Britain | 1950 | 14-15 years | 78 |
| South India | 1950 | All ages | 31 |
| South India | 1968 | All ages | 0† |
Amerindian population
Initial follow-up at 7.5 years showed a slightly higher incidence of tuberculosis in those vaccinated, and 15-year follow-up showed some protection in those vaccinated in infancy
On the other hand, BCG always induces Th1 reactivity and confers protection against tuberculosis when given neonatally22. By direct analogy, there have been conflicting reports on the ability of BCG to protect against cancer in children and young adults. In an extensive study by Rosenthal in Chicago23, neonatal BCG vaccination led to a 74% reduction in the incidence of leukaemia and other cancers during the first 20 years of life; whereas, when BCG was administered to older children and young adults in Puerto Rico24, where protection against tuberculosis was only moderate (29%), there was a slight though non-significant increase in the incidence of lymphomas in the vaccinated group. An analysis of the results of these, together with other studies in Canada, New Zealand, Israel and Austria, suggested that protection against cancer occurred only where the vaccine had been given neonatally and where it afforded good protection against tuberculosis18.
As BCG seems to be a ‘two-edged sword’ inasmuch as it can induce both protective and adverse immune reactions, there is a need to seek bacterial adjuvants that are able to induce protective responses and down-regulate inappropriate ones, even when the latter have been induced by environmental sensitization, for use in the prevention and therapy of cancer. Preliminary data indicate that environmental mycobacteria and related genera may be a source of such adjuvants and a heat-killed preparation of M. vaccae is under investigation for this purpose25.
CONCLUSION
With the notable exception of the use of intravesical BCG for bladder cancer, no vaccines or immunotherapeutic agents are yet in widespread clinical use in oncology. There has, however, been an enormous resurgence of interest in this subject in recent years. A survey conducted in the USA (where over $104 billion is spent on cancer research each year) on behalf of the Association of the British Pharmaceutical Industry showed that vaccines or immunotherapeutic agents feature prominently among the almost 400 anticancer products under development26. In conclusion, the whole subject of cancer immunology has come a long way since the observations of Cambell De Morgan in the 1870s and the first attempts at immunotherapy by Coley in 1891. New observations and discoveries have brought us to the point when we can move from the empirical to the rational approach. Many regarded as far-fetched the claims of Sir Almroth Wright that ‘the physician of the future will be an immunizer’, and he was unkindly nicknamed ‘Sir Almost Right’. Yet in the field of cancer he may well be proved right. Certainly, our modern understanding of cancer and the immune phenomena associated with it gives us confidence to repeat Campbell De Morgan's assertion that we are encouraged to hope that a simple and highly effective cure may yet be found for the disease.
References
- 1.De Morgan C. The Origin of Cancer. Considered with Reference to the Treatment of Disease. London: Churchill, 1872
- 2.De Morgan C. On cancer. Retrospect of Medicine 1874;69: 34-9 [Google Scholar]
- 3.De Morgan C. Observations on cancer. Lancet 1874;i: 323-9 [Google Scholar]
- 4.Pathological Society of London. Discussion on cancer. Lancet 1874;i: 334-6 [Google Scholar]
- 5.Bruns P. Die Heilwirkung des Erysipels auf Geschwülste. Beitr Klin Chir 1888 1887;3: 443 [Google Scholar]
- 6.Coley WB. The treatment of malignant tumors by repeated inoculations of erysipelas (reprinted). Clin Orthop 1991;262: 3-11 [PubMed] [Google Scholar]
- 7.Coley WB. Treatment of inoperable malignant tumour with the toxins of erysipelas and Bacillus prodigiosus. Trans Am Surg Assoc 1894;12: 183-96 [Google Scholar]
- 8.Nauts HC, McLaren JR. Coley's toxins—the first century. Adv Exp Biol Med 1990;267: 483-500 [DOI] [PubMed] [Google Scholar]
- 9.Takeuchi S. A new look at the history of tumour immunotherapy—for its fruitful future through overcoming the widespread cynicism. Hum Cell 1996;9: 1-10 [in Japanese, with English abstract] [PubMed] [Google Scholar]
- 10.Rosenberg SA, Spiess P, Lafreniere R. A new approach to the adoptive immunotherapy of cancer with tumour-infiltrating lymphocytes. Science 1986;233: 1318-21 [DOI] [PubMed] [Google Scholar]
- 11.Dong C, Flavell RA. Th1 and Th2 cells. Curr Opin Hematol 2001;8: 47-51 [DOI] [PubMed] [Google Scholar]
- 12.Clerici M, Clerici E, Shearer GM. Tumor enhancement phenomenon: reinterpretation from a Th1/Th2 perspective. J Natl Cancer Inst 1996;88: 461-2 [DOI] [PubMed] [Google Scholar]
- 13.Nishimura T, Nakui M, Sato M, et al. The critical role of Th1-dominant immunity in tumor immunology. Cancer Chemother Pharmacol 2000;46 (suppl): s52-61 [DOI] [PubMed] [Google Scholar]
- 14.Orditura M, Romano C, De Vita F, et al. Behaviour of interleukin-2 serum levels in advanced non-small-cell lung cancer patients: relationship with response to therapy and survival. Cancer Immunol Immunother 2000;49: 530-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stanford JL, Stanford CA, Grange JM. Environmental echoes. Science Progr 2001;84: 105-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rook GAW, Zumla A. Advances in the immunopathogenesis of pulmonary tuberculosis. Curr Opin Pulm Med 2001;7: 116-23 [DOI] [PubMed] [Google Scholar]
- 17.Grange JM, Stanford JL, Rook GAW. Tuberculosis and cancer: parallels in host responses and therapeutic approaches? Lancet 1995;345: 1350-2 [DOI] [PubMed] [Google Scholar]
- 18.Grange JM, Stanford JL. BCG vaccination and cancer. Tubercle 1990;71: 61-4 [DOI] [PubMed] [Google Scholar]
- 19.Tan JK, Ho VC. Pooled analysis of the efficacy of bacille Calmette—Guérin (BCG) immunotherapy in malignant melanoma. J Dermatol Surg Oncol 1993;19: 985-90 [DOI] [PubMed] [Google Scholar]
- 20.Brandau S, Böhle A. Therapy of bladder cancer with BCG: the mechanism behind a successful immunotherapy. Mod Asp Immunobiol 2001;2: 37-41 [Google Scholar]
- 21.Fine PE. BCG: the challenge continues. Scand J Infect Dis 2001;33: 243-5 [DOI] [PubMed] [Google Scholar]
- 22.Marchant A, Goetghebuer T, Ota MO, et al. Newborns develop a Th1-type immune response to Mycobacterium bovis bacillus Calmette—Guérin vaccination. J Immunol 1999;163: 2249-55 [PubMed] [Google Scholar]
- 23.Crispin RG, Rosenthal SR. BCG vaccination and cancer mortality. Cancer Immunol Immunother 1976;1: 139-42 [Google Scholar]
- 24.Comstock GW, Martinez I, Livesay VT. Efficacy of BCG vaccination in the prevention of cancer. J Natl Cancer Inst 1975;54: 835-9 [PubMed] [Google Scholar]
- 25.Stanford JL, Stanford CA, Baban B, Grange JM. Therapeutic vaccination for cancer: the potential value of mycobacterial products. Int J Pharmaceut Med 1999;12: 191-5 [Google Scholar]
- 26.Association of the British Pharmaceutical Industry. Oncology Mission Report, US East Coast, November 2000. London: Association of the British Pharmaceutical Industry, 2001