ABSTRACT
Purpose
To evaluate the effectiveness of graded (adjustable intraoperatively) partial vertical rectus muscle tenotomy at the insertion in correcting small degrees of hypertropia.
Methods
All patients with best-corrected visual acuity of better than 6/30 in both eyes who over a 30-month period underwent partial tenotomy of vertical rectus muscle(s) only (no concurrent oblique muscles) were included. Improvement was evaluated 6 weeks postoperatively as change in alignment in prism diopters (PD) in primary gaze and in the field of action of the affected rectus muscle(s). Binocular function was evaluated by Titmus stereoacuity and the Worth 4-light tests.
Results
All 24 patients who met criteria for inclusion had diplopia preoperatively versus seven patients (29%) postoperatively (P < .005, Student’s paired t test). Prisms were used by six preoperatively versus two postoperatively (P < .05, Student’s paired t test). The average vertical deviation in primary gaze decreased from 8 PD to 2 PD (P < .005, Student’s paired t test). In the field of action of the treated rectus muscle, hypertropia decreased from an average of 8 PD to 3 PD (P < .005, Student’s paired t test). For the preoperative and the postoperative assessments available, stereoacuity improved after 10 (56%) of the 18 procedures and Worth 4-light testing showed improvement or maintenance of fusion after 15 (79%) of 19 procedures.
Conclusions
Graded vertical rectus partial tenotomy can effectively reduce small degrees of hypertropia and associated diplopia, improve binocular function, and reduce or eliminate the need for prism correction.
INTRODUCTION
Vertical strabismus may occur as a result of decompensated congenital strabismus, or it may be acquired as the result of trauma or a disease process that affects the orbit or its contents. Although small degrees of horizontal misalignment can be corrected by horizontal vergence movements, small amounts of acquired vertical misalignment of the visual axes often cannot, and thus they will produce diplopia.1
Comitant hypertropias that are small in size and symptomatic are often treated successfully with prisms. However, if the prism requirement increases, patients will complain of image distortion, glasses will become heavy, and patients will object to wearing spectacles. Deviations that are incomitant respond poorly to treatment with prisms. In these situations, surgical correction of the vertical deviation becomes a consideration.
In 2000, Alan B. Scott, MD,2 described a rectus muscle weakening procedure called “graded rectus muscle tenotomy,” which he performed with the patient under local anesthesia, to treat small degrees of vertical strabismus. The procedure consists of making successive small cuts in the tendon of a rectus muscle at the insertion until the desired effect is achieved.
Tenotomy of a rectus muscle is not a new procedure. During the middle of the 19th century, use of the procedure to correct strabismus evolved as an extension of its use in orthopedic surgery. The first procedures to correct strabismus were tenotomies, partial or complete. Dieffenbach, Albrecht and Ferdinand von Graefe, Stromeyer, Cunier, Gibson, and many others performed complete tenotomy of one or more rectus muscles to correct large degrees of strabismus.3,4
Lucien Howe,5 in his 1908 summary of surgical techniques of the day, devoted a chapter to partial tenotomy of a rectus muscle for correction of strabismus. Partial tenotomy has also been called “graduated tenotomy.”5 Modifications of this technique followed, but as instrumentation improved and finer suture materials became available, tenotomy was replaced by surgical recession.6
After Scott’s description of the usefulness of partial tenotomy for treating small degrees of vertical strabismus, we evaluated this procedure in our own patients with diplopia, to improve binocular function and to eliminate or reduce the power of prisms in those patients with prisms in their spectacles.
METHODS
This study was presented to the University of Pittsburgh Medical Center Institutional Review Board, which determined that this study was outside of their jurisdiction. In conformity with US Health Insurance Portability and Accountability Act (HIPAA) guidelines for maintaining patient confidentiality, our surgical coordinator identified all patients in our private practice surgical log who had undergone partial tenotomy of a vertical rectus muscle during the 30-month study period after we started to perform the procedure and who had been followed for at least 3 months postoperatively.
Patients were excluded from the study if they had concomitant oblique muscle (but not horizontal rectus muscle) surgery or if they had best-corrected visual acuity in one eye of less than 6/30. The remaining patients gave permission to include their pooled data in the study and in study publications. Each patient’s clinical record was then assigned a study reference number, and data were collected under that number, without inclusion of personally identifying information.
All patients had undergone comprehensive ophthalmologic evaluation, and most had undergone measurement of their ocular alignment on at least two occasions prior to the procedure.
Partial Tenotomy Procedure
We performed each partial tenotomy procedure in a surgicenter with the patient under intravenous sedation and monitoring supervised by an anesthesiologist. The partial tenotomy procedure is performed as follows. After the patient has been sedated and the surgical field prepared, 0.10 mL of mepivacaine 2% is injected under the conjunctiva adjacent to the lateral border of the rectus muscle. An incision is made down to the sclera just lateral and posterior to the muscle’s insertion. The muscle is secured with a Stevens muscle hook that is then replaced with a Jameson hook. A Stevens muscle hook is then used to reflect the conjunctiva and anterior Tenon’s capsule overlying the insertion of the muscle to expose the insertion (Figure 1). Wet-field cautery is used to blanch the anterior ciliary vessels, and then a Westcott scissors is used to cut through approximately 60% of the width of the tendon.
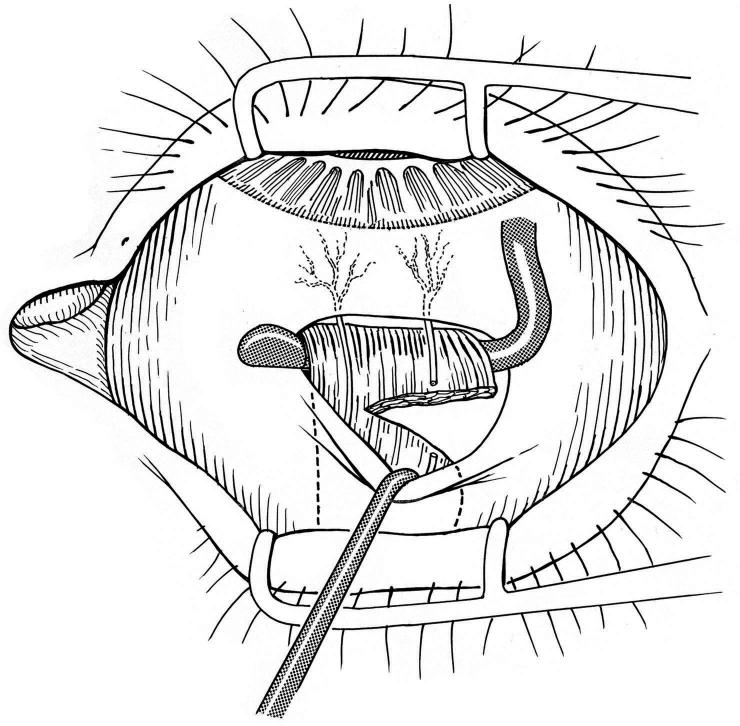
Figure 1.
Drawing showing procedure for graded partial tenotomy of vertical rectus muscle for treatment of hypertropia. With the patient under moderate sedation, the superior rectus is exposed, the tendon is cauterized near its insertion, and a Westcott scissors is used to make a cut in the tendon. The patient is tested with eyeglasses (without prisms), and if correction of vertical deviation is inadequate, the tenotomy is extended successively until the desired effect is achieved.
After partial tenotomy, sedation is suspended, the instruments and drapes are removed, and the patient is helped to a sitting position. The patient’s eyeglasses or, for patients with prisms, eyeglasses created for this step without prisms, are positioned to avoid contaminating the operative area, and cover testing at distance and near is performed using targets that stimulate accommodation.
After testing, the eyeglasses are removed and the surgeon redrapes the field with sterile towels and changes gloves. If the results of cover testing indicate lack of fusion, an additional cut is made in the tendon and then the alignment is tested again. This is repeated until the patient has single binocular vision in the desired gaze positions. An antibiotic-corticosteroid drop is placed on the eye, and the patient is sent home with instructions to instill one drop of the solution daily for the next 3 days.
Patients were scheduled for follow-up visits 3 to 7 days after surgery, 6 weeks after surgery, and thereafter as considered necessary.
Data Collection and Analysis
Data collected from the medical records and analyzed for this study included the patient’s age at surgery, best-corrected visual acuity, presence of diplopia, cause of hypertropia, muscle(s) operated upon, use of prisms, the results of Maddox double-rod testing in patients with symptoms of cyclotropia, and whether the patient and surgeon considered the procedure to have been “successful” or “unsuccessful” in resolving the patient’s diplopia.
Student’s paired t test was used to identify statistically significant differences between group means for preoperative and 6-week postoperative values for proportion of patients complaining of diplopia; use of prisms; deviation measured in prism diopters (PDs) in primary, left, and right gaze and in the reading position; results of the Titmus stereoacuity test; and results of the Worth 4-light test at near (1/3 meter) and far (6 meters).
RESULTS
During the study period, a total of 30 patients underwent tenotomies of vertical rectus muscles. Five patients were excluded from the study either because they had decreased visual acuity in one eye or because surgery on an oblique muscle was performed in conjunction with rectus muscle tenotomy. A sixth patient was excluded because tenotomy was planned but at the time of the procedure it was converted to muscle recession using a suture on account of insufficient effect of the partial tenotomy. The remaining 24 patients who met study inclusion criteria had undergone a total of 26 tenotomy procedures.
The mean age of the 24 patients was 62 years (range, 19 to 83 years), and 16 (67%) of the subjects were male. Twenty-one patients had best-corrected visual acuity between 6/6 and 6/12, one patient had visual acuity of 6/15 in both eyes, one had visual acuity of 6/21 in one eye, and the final patient had best-corrected visual acuity of 6/24 in one eye. Eleven patients had a history of strabismus surgery. The mean follow-up period was 6 months (range, 1 to 29 months).
Effect of Tenotomy on Vertical Alignment
The primary outcome measure was the effect of the tenotomy procedure on vertical alignment in the primary gaze position (Table 1). Compared with the mean preoperative value of 8 PD, hypertropia at the 6-week postoperative visit was a mean of 2 PD. This mean improvement of 6 PD in primary gaze was statistically significant (P < .005, Student’s paired t test).
Table 1.
Deviation in vertical alignment in primary gaze position before and 6 weeks after graded partial tenotomy of vertical rectus muscles for treatment of hypertropia
| Patient no. | Preop deviation (PD) | Treated muscle | Postop deviation (PD) | Postop change (PD) | Diagnosis |
|---|---|---|---|---|---|
| 1 | LHT 9 | LSR | ORTHO | −9 | Cataract |
| 2 | RHT 12 | RSR | RHT 10 | −2 | Cataract |
| 3 | LHT 10 | LSR, RIR | ORTHO | −10 | Cataract |
| 4 | RHT 3 | LIR | ORTHO | −3 | CN IV palsy |
| 5 | RHT 3 | LIR | ORTHO | −3 | CN IV palsy |
| 6 | LHT 7 | RIR | LHT 3 | −4 | HT |
| 7 | LHT 7 | RIR | N/A | N/A | Cataract |
| 8 | LHT 10 | RIR, LSR-Rec | LHT 4 | −6 | Cataract |
| 8* | LHT 10 | RIR, LSR | LHT 9 | −1 | Cataract |
| 9 | LHT 10 | RIR | ORTHO | −10 | CN IV palsy |
| 10 | RHT 1 | LIR | ORTHO | −1 | Cataract |
| 11 | RHT 9 | RSR | ORTHO | −9 | Cataract |
| 12 | RHT 6 | RSR | ORTHO | −6 | Retinal detachment |
| 13 | LHT 2 | RIR | ORTHO | −2 | CN IV and VI palsy |
| 14 | LHT 4 | LSR | ORTHO | −4 | CN IV and VI palsy |
| 15 | RHT 8 | RSR | RHT 3 | −5 | Retinal detachment |
| 16 | LHT 6 | RIR | LHT 2 | −4 | Trauma to orbit |
| 17 | LHT 16 | LSR, RIR | ORTHO | −16 | Graves’ disease |
| 18 | LHT 8 | LSR | LHT 6 | −2 | HT |
| 19 | RHT 7 | LIR | ORTHO | −7 | Tumor, CN IV palsy |
| 20 | RHT 6 | LIR | ORTHO | −6 | Cataract |
| 21 | LHT 6 | LSR | LHT 3 | −3 | HT |
| 22 | RHT 22 | RSR, LIR-Rec LSR-Res | ORTHO | −22 | Cataract |
| 23 | LHT 2 | LSR | LHT 4 | 2 | Ehlers-Danlos, HT |
| 23* | LHT 8 | LSR, RIR | LHT 9 | 1 | Ehlers-Danlos, HT |
| 24 | RHT 16 | LIR | ORTHO | −16 | HT |
| Average | 8 PD | 2 PD | −6 PD | ||
| 95% CI | 6-10 PD | 1-3 PD | −4 to −8 PD | ||
| SD | 5 PD | 3 PD | 6 PD |
CI, confidence interval; CN, cranial nerve; HT, long-standing hypertropia; LHT, left hypertropia; LIR, left inferior rectus; LIR-Rec, left inferior rectus recession; LSR, left superior rectus; LSR-Rec, left superior rectus recession; LSR-Res, left superior rectus resection; N/A, not assessed (patient unable to return for 6-week visit); ORTHO, orthotropia; PD, prism diopters; Preop, preoperative; Postop, postoperative; RHT, right hypertropia; RIR, right inferior rectus; RSR, right superior rectus; SD, standard deviation.
Second procedure.
Among the 21 patients in whom vertical alignment in the primary gaze position was measured both early (at 1 week) and at 6 weeks after the procedure, the average improvement was 7 PD at 1 week compared with 6 PD at 6 weeks. Nine patients who were followed for longer than 6 weeks postoperatively had a mean improvement from the preoperative visit of 5 PD in primary gaze.
We also measured the effect of the tenotomy procedure on deviation in the field of action of the treated rectus muscle by comparing preoperative to 6-week postoperative values (Table 2). Of the 22 patients who underwent testing 6 weeks postoperatively, 18 had undergone unilateral tenotomy and four had vertical rectus tenotomies performed on both eyes. The average preoperative hypertropia in these patients was 8 PD, and the average postoperative hypertropia was 3 PD. The mean improvement of 5 PD was statistically significant (P < .005, Student’s paired t test).
Table 2.
Deviation in vertical alignment in field of action gaze position before and 6 weeks after graded partial tenotomy of vertical rectus muscles for treatment of hypertropia
| Patient no. | Preop deviation (PD) | Treated muscle | Postop deviation (PD) | Postop change (PD) |
|---|---|---|---|---|
| 1 | LHT 8 | LSR | ORTHO | −8 |
| 2 | RHT 12 | RSR | RHT 10 | −2 |
| 3 | LHT 7 | LSR | LHT 2 | −5 |
| 3 | LHT 3 | RIR | ORTHO | −3 |
| 4 | RHT 7 | LIR | RHT 6 | −1 |
| 5 | RHT 4 | LIR | ORTHO | −4 |
| 6 | LHT 6 | RIR | LHT 4 | −2 |
| 7 | LHT 6 | RIR | N/A | N/A |
| 8 | LHT 14 | LSR | LHT 7 | −7 |
| 8* | LHT 8 | LSR | LHT 6 | −2 |
| 8* | LHT 14 | RIR | LHT 12 | −2 |
| 9 | LHT 12 | RIR | RHT 2 | −10 |
| 10 | RHT 2 | LIR | ORTHO | −2 |
| 11 | RHT 9 | RSR | ORTHO | −9 |
| 12 | RHT 6 | RSR | ORTHO | −6 |
| 13 | LHT 6 | RIR | ORTHO | −6 |
| 14 | RHT 2 | LSR | ORTHO | −2 |
| 15 | RHT 4 | RSR | RHT 3 | −1 |
| 16 | LHT 6 | RIR | LHT 2 | −4 |
| 17 | LHT 14 | LSR | LHT 2 | −12 |
| 17* | LHT 10 | RIR | ORTHO | −10 |
| 18 | LHT 9 | LSR | LHT 3 | −6 |
| 19 | RHT 8 | LIR | N/A | N/A |
| 20 | RHT 5 | LIR | ORTHO | −5 |
| 21 | LHT 10 | LSR | ORTHO | −10 |
| 22 | RHT 20 | RSR† | ORTHO | −20 |
| 23 | LHT 2 | LSR | LHT 4 | 2 |
| 23* | LHT 8 | LSR | LHT 9‡ | 1 |
| 23* | LHT 8 | RIR | LHT 9‡ | 1 |
| 24 | RHT 14 | LIR | ORTHO | −14 |
| Average | 8 PD | 3 PD | −5 PD | |
| 95% CI | 7-10 PD | 1-4 PD | −3 to −7 PD | |
| SD | 4 PD | 4 PD | 5 PD |
CI, confidence interval; LHT, left hypertropia; LIR, left inferior rectus; LSR, left superior rectus; N/A, not assessed (patient unable to return for 6-week visit); ORTHO, orthotropia; PD, prism diopters; Preop, preoperative; Postop, postoperative; RHT, right hypertropia; RIR, right inferior rectus; RSR, right superior rectus; SD, standard deviation.
Second procedure.
Combined with a recession of LIR, and resection of the LSR.
Patient could tolerate measurement only in primary gaze.
No patient in this study had an overcorrection in primary gaze. One patient did have a transient overcorrection of 1 PD in the field of action gaze position (Table 2).
No patient has demonstrated an increase in correction with longer follow-up after tenotomy on an inferior rectus muscle.
Stereoacuity and Fusion
Stereoacuity was measured both preoperatively and 6 weeks postoperatively in 17 patients (18 procedures). Stereoacuity improved or remained the same after 10 (56%) of the 18 procedures (Table 3).
Table 3.
Binocular function before and 6 weeks after graded partial tenotomy of vertical rectus muscles for treatment of hypertropia
| Patient no. | Preop stereoacuity (seconds of arc) | Postop stereoacuity (seconds of arc) | Stereoacuity improvement | Preop worth (near, far*) | Postop worth (near, far*) | Worth improvement |
|---|---|---|---|---|---|---|
| 1 | 140 | 100 | Yes | 5,4 | 5,4 | Same |
| 2 | 0 | 140 | Yes | 4,4 | 5,5 | No |
| 3 | 800 | 100 | Yes | 5,5 | 4,4 | Yes |
| 4 | 0 | 100 | Yes | 2,2 | 4,4 | Yes |
| 5 | 100 | N/A | N/A | 4,4 | N/A | N/A |
| 6 | 800 | 0 | No | 3,4 | 4,4 | Yes |
| 7 | N/A | N/A | N/A | N/A | N/A | N/A |
| 8 | N/A | 3000 | N/A | N/A | 5,5 | N/A |
| 8† | N/A | 0 | N/A | N/A | 5,5 | N/A |
| 9 | 60 | 400 | No | 4,4 | 4,4 | Same |
| 10 | 400 | 40 | Yes | 4,4 | 4,4 | Same |
| 11 | 50 | 60 | No | 4,2 | 4,4 | Yes |
| 12 | 80 | 100 | No | 4,4 | 4,4 | Same |
| 13 | 80 | 50 | Yes | 5,4 | 5,5 | No |
| 14 | 140 | 100 | Yes | 4,4 | 4,4 | Same |
| 15 | 3000 | 3000 | Same | 4,4 | 4,4 | Same |
| 16 | 140 | N/A | N/A | 3,3 | N/A | N/A |
| 17 | 200 | 50 | Yes | 3,5 | 4,4 | Yes |
| 18 | N/A | N/A | N/A | N/A | N/A | N/A |
| 19 | 400 | 3000 | No | 4,4 | 3,4 | No |
| 20 | 3000 | 400 | Yes | 5,3 | 4,4 | Yes |
| 21 | N/A | N/A | N/A | N/A | 5,4 | N/A |
| 22 | N/A | 0 | N/A | 3,5 | 4,4 | Yes |
| 23 | 800 | 100 | Yes | 3,4 | 5,5 | No |
| 23† | 800 | 0 | No | 5,5 | 5,5 | Same |
| 24 | 80 | 140 | No | 4,4 | 4,4 | Same |
N/A, not assessed (patient unable to return for 6-week visit); Postop, postoperative; Preop, preoperative.
Near = 1/3 meter, far = 6 meter.
Second procedure.
Worth fusion improved or remained the same in 15 (79%) of 19 patients who were tested both preoperatively and postoperatively (Table 3).
Diplopia
Before surgery, all 24 patients had subjective diplopia. The reasons for diplopia included cataract surgery in nine patients, cranial nerve IV palsy in six patients (one of whom had metastatic breast cancer), surgery to repair a detached retina in two patients, and thyroid eye disease or trauma in one patient each. The remaining five patients had long-standing unexplained hypertropia (Table 1).
At the most recent postoperative visit, 7 (29%) of the 24 patients had persistent diplopia. By Student’s paired t test, the postoperative reduction in proportion of patients with diplopia was statistically significant (P < .005).
Of the seven patients with persistent diplopia, two (one with restrictive strabismus after retinal detachment repair and one after trauma to the orbit) had persistent diplopia in downgaze only and were treated with prisms. Three of the seven patients had intermittent diplopia and elected no additional treatment. The remaining two patients (No. 8 and No. 23 in Table 1) had two separate intraoperative adjustable tenotomy procedures, and both procedures in both patients were considered to be failures. One of the patients had a history of four previous operations for strabismus and was unable to adjust his head position to relieve diplopia. The second patient had diplopia following cataract surgery complicated by endophthalmitis and repair of a retinal detachment. Both of these patients were subsequently, and successfully, treated by incisional surgery combined with adjustable suture techniques.
Prisms
Six (25%) of the 24 patients had prisms in their spectacles before surgery and only two (8%) of the 24 patients required prisms at a reduced power at the most recent visit. By Student’s paired t test, the postoperative reduction in proportion of patients using prisms was statistically significant (P < .05).
Tenotomy Location and Cyclotorsion
We looked for a possible relationship between the location of the tenotomy and the risk of inducing cyclotorsion of the globe. Four of the 26 procedures were performed on the nasal portion of the rectus muscle, and the other 22 procedures were performed on the temporal portion of the muscle. The Maddox double-rod test was performed in several patients both preoperatively and postoperatively but did not show any meaningful change in cyclotorsion of the globe.
DISCUSSION
This pilot study affirms the effectiveness of an intraoperative adjustable partial vertical rectus muscle tenotomy in correcting hypertropia with associated diplopia. In our consecutive series of 24 patients with small vertical deviations and diplopia from a variety of causes, graded partial tenotomy effected mean improvement in vertical alignment in the primary gaze position of 6 PD and mean improvement in lateral gaze in the field of action of the treated muscle of 5 PD. Furthermore, about half of patients had improved binocular function. Finally, diplopia was relieved by surgery in 17 (71%) of the 24 patients, four of six who used prisms preoperatively did not need prisms after surgery, and both the surgeon and the patient rated the surgery “successful” in the majority of cases.
The effects of partial tenotomy seem to stabilize by 6 weeks after surgery, although this should be confirmed by longer follow-up. The insufficient numbers of patients in this series precluded analysis of the causes of vertical misalignment for which the procedure may be most or least successful.
Advantages Over Other Procedures for Hypertropia
Graded partial tenotomy has several advantages over other procedures for managing mild hypertropia. First, compared to the recession procedure, a partial tenotomy is easier to perform under intravenous sedation with subconjunctival anesthesia. Second, adjustments are made to the degree of correction intraoperatively, presumably giving a greater chance for success with the first operation. Third, partial tenotomy requires no suturing, thus avoiding a possible foreign body reaction, and because the sclera is not penetrated, poses less risk of penetration of the globe. Fourth, bleeding is prophylactically controlled with wet-field cautery. Fifth, by placing the incision lateral to the insertion, the conjunctiva covers the cut segment of tendon, thereby reducing the risk for infection compared to incisions placed directly over the insertion. Sixth, in our series, partial tenotomy led to only one case of overcorrection, which was only transient, in the field of action of the treated muscle. In our experience, patients with overcorrected hypertropia are displeased until the overcorrection is remedied. The tendency of this procedure to not overcorrect hypertropia is desirable.
Other Applications
Graded partial tenotomy of vertical rectus muscles may have applications beyond that described in this study. For example, one of us (A.W.B.) combined intraoperative adjustable tenotomy of vertical rectus muscles with surgery on oblique muscles to treat a contracted superior rectus muscle in the presence of a long-standing superior oblique palsy. The procedure has also been performed on the contralateral yoke muscle in combination with surgery on an inferior oblique muscle. We excluded these cases from this study so that we could measure the effect of the procedure solely in the field of action of the vertical rectus muscle.
Limitations of a Graded Partial Tenotomy
Partial graded tenotomy has some limitations. It will not correct large deviations. A graded tenotomy may not be sufficient to correct hypertropia in all cases. One patient was excluded from this study because of insufficient correction with tenotomy; although improvement was observed, it was not sufficient to correct the diplopia. The tenotomy was abandoned; a suture was placed through the tendon, and the muscle was recessed using an intra-operative adjustable suture technique.
A second limitation is suggested. The further reduction of 1 PD of effect in the nine patients followed more than 3 months, when compared to the 3-month follow-up period, suggests a potential diminution in the effect with time.
Limitations of the Study
This study has some limitations. The study was conducted in a retrospective manner. Some measurements were missing in some patients. The presence of constant diplopia in some patients obviated collection of preoperative binocular function data. This would not have been an issue in a prospective study.
The fact that one of the investigators in this study was also involved in caring for the patients could have added bias, especially with regard to subjective results (whether the surgery was considered “successful”). However, the primary outcome measure (vertical alignment) was objective, as was testing for binocular function. Several of the measurements were obtained by staff and residents and fellows.
There is a learning curve in performing any surgical procedure. Thus, the success rate would be expected to be higher for patients operated on later in the series, although we did not analyze this factor.
Future Research
Extended follow-up needs to be completed to determine the long-term results of graded partial tenotomy.
Another area for further investigation is cyclotorsion that might result if a cut in the tendon shifts the vector of force that the muscle exerts on the globe either temporally or nasally, depending on where the partial tenotomy is made. In fact, two patients in this study volunteered during the intraoperative adjustment that there was torsion of the fixation target. As a result, the Maddox double-rod test was performed in several subsequent patients before and after the procedure. No cyclotorsion was detected, although this could have been due to inadequate test sensitivity.
DISCUSSION
Dr Malcolm L. Mazow
Small-angle, vertical deviations of less than 10 diopters become significantly important when they present with uncontrollable, uncomfortable, intermittent or constant diplopia. This problem generally does not present with congenital or infantile strabismus unless decompensation occurs after visual maturation.
However, as mentioned by the authors, this problem frequently occurs in acquired incomitant deviations resulting from mechanical or restrictive problems as well as in paralytic strabismus. In addition, in the initial phase after correction, a patient may be left with residual debilitating diplopia.
Conventional surgery, with or without an adjustable suture, frequently will result in over- or under-correction, leaving as the only alternative glasses with prisms, which often are unacceptable to the patient. Using the adjustable myotomy technique as described by Scott, the authors have shown that small angles of vertical strabismus can be successfully treated to eliminate bothersome diplopia.
Realizing that this was a retrospective study and could not necessarily adhere to principals assessing diplopia, I would offer some suggestions. In evaluating a patient with diplopia, certain further testing would have added to the significance of the results: 1) Repeated measurements at different times of the day and on different visits might reveal a change in the angle of deviation, as would unilateral patching in the office to eliminate fusion, uncovering the maximal deviation that is present. 2) In those patients who had an area of single binocular vision in the preoperative period, binocular fields should have been done and compared to postoperative binocular fields, which would allow the observer to determine whether improvement and enlargement of the binocular fields occurred in the primary and reading positions. These points aside, the results reported are excellent, with a 71 percent elimination of diplopia, binocular improvement in 41 percent and stereoscopic improvement in 50 percent.
In general, statistical analysis may cement the results of any patient population study. With such small angles of deviation, this method of analysis becomes much less significant. Rather, we see a trend to successful elimination of diplopia by the technique utilized here.
The authors state that doing a temporal fornix incision rather than a nasal incision provides better coverage of the muscle and wound, lessening the problems associated with infection. In my experience, infection is a very rare entity in strabismus surgery and coverage seems to be adequate regardless of where the incision is made. It would be interesting to know if there was a difference in results whether the marginal myotomy was done temporally or nasally. One would wonder when the 60 percent marginal myotomy was accomplished initially and adjustment was required, what increment of increase was achieved before it was decided that no further myotomies should be performed. Dr Biglan and his associates have shown that of the 24 patients, 15 (63 percent) were orthotropic in the primary position of gaze and 13 (54 percent) were also ortho in the field of action of the offending muscle. When looking at this analysis in more detail, 12 (80 percent) of the 15 who were ortho in the primary position were also ortho in the field of gaze. Three (20 percent) of the 15 who were ortho in the primary position were not ortho in the field of gaze. One (8 percent) of the 13 who were ortho in the field of gaze was not ortho in the primary position and one (4 percent) of the 24 was overcorrected in the field of gaze. This speaks very well for the technique in avoiding complications. The objective of any strabismus surgery is to make the patient symptom-free in the primary position and in functional fields of gaze, and these results corroborate the goal of this particular strabismus operation.
I applaud their ingenuity in trying to find a technique to correct significant vertical deviations that are seen in acquired strabismus.
Dr Edward L. Raab
Does it matter if you’re going from the nasal to the temporal side? This procedure seems to be analogous to one that has been reported for convergence insufficiency, which was a slanted recession of the medial recti. But, that was not sutureless. Can you, from grading the percentage of transsection, predict where the receded tendon will knock down, because what you have in effect is a hang-back from that portion of the tendon? Can you, by any triangulation or trigonometry, predict where that will reattach? Do you still need an adjustable technique to play with that?
Dr Albert W. Biglan
This is a pilot study. Obtaining diplopia fields, both pre-op and post-op, are constructive suggestions to consider in proceeding with this study and binocular fields should be considered in the evaluation of additional patients.
As part of my evaluation of adults, and some children, I perform prolonged occlusion of the non-dominant eye. I will have the patient (family) place a patch on an hour or more before the patient arrives at the office. When I see the patient and complete the history, I then proceed directly to the measurement. I then remove the patch in doing so, not allowing the patient to become binocular, and perform the cover testing.
As for the infection question: I make the incision either temporal or nasal, as opposed to right over the tendon. I reflect or slide the conjunctiva over the insertion to achieve exposure of the tendon insertion. At the end of the procedure, I replace the conjunctiva so that the insertion is covered. I am attempting to protect the area of surgical procedure by covering it with conjunctiva.
How much can I cut? When you get up to about 90 percent, this gets a little risky since you have the potential of having a “lost muscle.” Another issue is torsion. I performed the Maddox double rod test pre- and post-op on several patients, but the test wasn't sensitive enough for me to pick up a change in torsion. Two patients volunteered during the intraoperative adjustment that they actually noticed that the “E” was tilting while I was making the adjustments. These observations have prompted me to look for torsion before and after the procedure.
The slanting procedures that Nemet1,2 has advocated and that I have also written about,3 were used to reduce AC/A and V patterns. This accomplishes this by slanting the muscle. If you look at the force vectors on the superior and inferior recti, you should be inducing some torsion by laterally translating the vector of pull of the muscles.
Dr Raab asks if this procedure can be done by estimation without the intraoperative adjustment. I believe that the input of the patient is most important in obtaining the best result. I adjust, and then ask the patient what they see in the fields of gaze tested. When the patient says, “That’s single,” I then stop. In the patients that I have had to re-op, the tendon is attached to the sclera with the cut tendon adhering in a slanted position.
REFERENCES
- 1.Nemet P, Stolovich C. Biased resection of the medial recti; a new surgical approach to convergence insufficiency. Binocul Vis Strabismus Q. 1990;5:213. [Google Scholar]
- 2.Nemet P, Stolovich C, Lowenstein A. A new operation: slanted (reinsertion) medial rectus muscle surgery for convergence excess esotropia: Results in 12 cases. Binocul Vis Strabismus Q. 1993;8:241. [Google Scholar]
- 3.Biglan AW, Walden P. Results following management of oculomotor nerve palsy with a modified Knapp procedure. Ophthalmic Surg. 1985;16:759–764. [PubMed] [Google Scholar]
REFERENCES
- 1.von Noorden GK. Examination of the patient. II. Motor signs in heterophoria and heterotropia. In: von Noorden GK, Campos EC, eds. Binocular Vision and Ocular Motility, Theory and Management of Strabismus. Philadelphia: Mosby; 2002:202–206.
- 2.Scott AB. Graded rectus muscle tenotomy for small deviations. In: Proceedings of the Jampolsky Festschrift. San Francisco: The Smith-Kettlewell Eye Research Institute; 2000:215–216.
- 3.von Noorden GK. The history of European strabismology. In: von Noorden GK, ed. The History of Strabismology. Vol 9. Oostende, Belgium: JP Wayenborgh; 2002:40–44, 82–83.
- 4.von Noorden GK. The renaissance of ophthalmology in the eighteenth century. In: Hirschberg J, ed. The History of Ophthalmology. Berlin: Springer Verlag; 1985:319–329.
- 5.Howe L. Partial tenotomy. In: Howe L, ed. The Muscles of the Eye. London/New York: GP Putnam’s Sons/The Knickerbocker Press; 1908:304–308.
- 6.Helveston EM. Surgical Management of Strabismus: An Atlas of Strabismus Surgery. 4th ed. St Louis: Mosby; 1993:4–6.