ABSTRACT
Purpose
This was a retrospective study to compare the efficacy and efficiency of a new small anterior incision, minimal dissection ptosis procedure with that of a traditional anterior aponeurotic approach for the correction of aponeurotic ptosis.
Methods
The results of a chart and photograph review of 36 patients with 49 ptotic eyelids who had ptosis correction by a small-incision, minimal dissection procedure were compared with those of 36 patients with 49 ptotic eyelids who had ptosis correction by a traditional aponeurotic approach.
Results
The successful correction of the eyelid height and the rate of recommendation for reoperation were not significantly different for the 49 lids corrected in each arm of the study. The incidence of attaining good eyelid contour was significantly better in the small-incision group, where 41 (97.6%) of 42 lids evaluated by photographs had good contour compared with 29 (78.4%) of 37 lids in the traditional group. Operating time per lid was significantly less for the small-incision, minimal dissection group, 25.3 ± 13.0 minutes (range, 13 to 68 minutes), compared with 55.4 ± 16.6 minutes (range, 35 to 119) for the traditional group.
Conclusions
Compared with the traditional aponeurotic approach, the new small-incision, minimal dissection technique for ptosis correction is equally efficacious in correcting eyelid height, superior in producing desirable eyelid contour, and much quicker to perform.
INTRODUCTION
Shortly after the concepts of aponeurotic ptosis and aponeurotic surgery to correct it were introduced by Jones and associates1 in 1975, the concepts were accepted and surgery for acquired ptosis changed.1–3 The traditional dissection for aponeurotic ptosis correction involves a lid crease incision approximately 20 to 22 mm long. Through this, dissection is carried superiorly under the orbicularis oculi muscle across the width of the incision. When the orbital septum is identified, it is opened widely to expose the orbital fat. With the fat lifted back or excised, the levator aponeurosis is exposed. Inferiorly, the anterior surface of the upper half of the tarsal plate is cleared across the same width, by either excising overlying orbicularis oculi muscle or dissecting underneath it. The aponeurosis can then be shortened or tucked, suturing it to the exposed tarsal plate, commonly with three sutures.
We present here a small-incision, minimal dissection procedure for aponeurotic ptosis correction as originally conceived by one of the authors (H.M.). The results using the small-incision, minimal dissection approach are presented and compared with those obtained by the same surgeon (B.R.F.) using the traditional dissection procedure.
METHODS
The criteria for inclusion in this study included (1) a diagnosis of aponeurotic ptosis, (2) surgical correction either with the small-incision, minimal dissection method or by the traditional method, (3) surgery performed by one surgeon (B.R.F.) with a resident or fellow participating in the procedure, and (4) follow-up conducted by the primary surgeon. Exclusion criteria included previous surgery on the ptotic eyelid, concomitant surgery done at the time of ptosis repair, and/or a follow-up of less than 2 months.
Fifty-one charts of consecutive patients who had the small-incision, minimal dissection procedure between July 2001 and July 2003 were reviewed. Fifteen patients were excluded: six had insufficient follow-up, five had concomitant surgery, two procedures were reoperations, and two patients were determined to have had an underlying etiology other than aponeurotic ptosis. This left 36 patients for the study, 13 of whom had bilateral surgery. Sixty-three charts of nonconsecutive hapazardly chosen patients who had the traditional procedure between March 1990 and December 1996 were reviewed to come up with an equal number of patients with the same bilaterality as the small-incision, minimal dissection group. Twenty-seven were excluded: 10 had inadequate follow-up, 10 had concomitant surgery, four procedures were reoperations, and three patients were determined not to have aponeurotic ptosis. After reviewing the first 61 charts, 23 unilateral cases had been selected and 12 bilateral cases. Only bilateral cases were then reviewed to obtain the 13th bilateral case. No charts for the interval from January 1997 to June 2001 were reviewed because the surgical methodology used in that interval did not meet the selection criteria.
Information recorded for each patient in the study included age, male or female sex, ocular diseases, previous surgery on the operated side, other medical conditions, family history of ptosis, side(s) involved with ptosis, preoperative and postoperative lid excursion for each side, levator force, preoperative and postoperative distance of each lid above the center of the pupil for each side, number of sutures used, surgical time, presence of exposure keratitis postoperatively, whether the patient was clinically considered to be overcorrected or undercorrected, the lid contour judged from postoperative photographs, and whether reoperation was recommended. The study protocol was approved by the University of Michigan’s institutional review board.
Prior to data gathering, a successful outcome was defined as each lid being within 0.5 mm of the other and the operated lid being within 2 to 4 mm above the center of the pupil with the patient looking in the primary position.
Small-Incision, Minimal Dissection Procedure
The patient, in the supine position on the operating table, is asked to look straight ahead, up at the ceiling. A vertical line is drawn on the upper lid, in line with the center of the pupil. Another line is drawn in the lid crease, centered on the vertical line and about 8 to 10 mm long. Local anesthetic, an equal mixture of 1.0% Xylocaine with epinephrine 1:100,000 and 0.75% bupivacaine, is infiltrated beneath the skin of the lid crease line. The anesthetic needle is then passed vertically through the vertical line at the center of the tarsus, through the skin and orbicularis until the tarsal plate is felt but not penetrated, and additional local anesthetic is injected. A total of less than 0.6 mL of local anesthetic is used per eyelid.
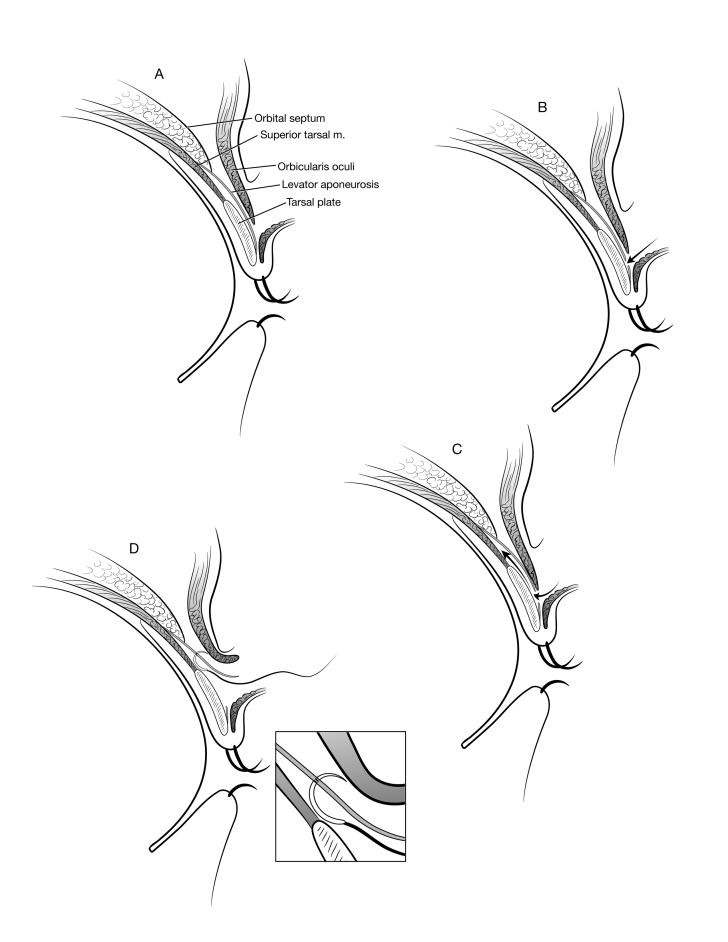
The marked lid crease is incised through the skin. A sharp scissors, aimed toward the center of the tarsal plate, is used to bluntly spread the orbicularis fibers until the tarsal plate comes into view through the semitransparent levator aponeurosis (Figure 1A). The aponeurosis is incised with sharp scissors horizontally over the tarsal plate using numerous small snips to obtain a defect that is approximately 8 mm wide (Figure 1B). The lower edge of the skin incision is pulled down, and sharp scissors are used to bluntly dissect superiorly under the cut aponeurosis until it is free from the underlying tarsal plate and Müller’s muscle, a distance of about 12 to 15 mm (Figure 1C). An 8-mm spatula needle on a permanent 6-0 suture is then passed through this space, in line with the vertical lid marking, as high as it will reach, and then curved forward and brought out the upper edge of the incision just posterior to the orbicularis oculi muscle (Figure 1D). The two ends of the suture are then grasped and held inferiorly, leaving a little slack in the suture. The lights are dimmed, and the patient is requested to open his or her eyes and look up. A firm tug should be felt on the suture if it is through the aponeurosis at the upper extent of its passage. For the infrequent times that a firm tug is not felt, the suture is repassed and the pull on upgaze rechecked. After it is ascertained that the aponeurosis has been engaged by the suture, the needle is passed horizontally through the tarsal plate in mid tarsus, centered on the vertical lid mark. The suture is tied with a surgeon’s knot to an estimate of the correct tension, and a slipknot is placed over the surgeon’s knot.
Figure 1.
Small-incision, minimal dissection procedure. The steps from dissection through the orbicularis to passing the needle through the aponeurosis, shown in cross-section. A, After incising the skin, the orbicularis is bluntly spread to expose the aponeurosis over the midtarsal plate. B, The aponeurosis is incised. C, Dissection is bluntly carried superiorly posterior to the aponeurosis. D, The suture is passed through the dissected space through the posterior surface of the aponeurosis and out the anterior surface, posterior to the orbicularis oculi muscle.
The patient is then asked to sit up and open his or her eyes. The eyelid height and contour are inspected. The suture tension is adjusted until the height seems optimal. If the eyelid cannot be elevated sufficiently with the suture tightly tied, it is removed and replaced higher in the aponeurosis. If the lid appears low medially or laterally, the dissection is extended in that direction by incising skin, extending the aponeurosis incision, and then spreading superiorly. An additional suture is similarly placed and tied. When the lid position seems optimal with the patient seated, the patient again assumes the supine position and each suture is tied permanently. The skin is closed.
Description of Patients
The average age of the patients undergoing small-incision, minimal dissection ptosis correction was 63 years, with a range of 14 to 82 years. There were nine male and 27 female patients. The average age of the patients undergoing traditional ptosis surgery was 62 years, with a range of 17 to 92 years. There were 10 male and 26 female patients.
In the small-incision, minimal dissection group, 13 patients had bilateral correction; of the 23 unilateral surgeries, 15 were on the right side and 8 were on the left side. In the traditional group, 13 patients had bilateral correction; of the 23 unilateral surgeries, 12 were on the right side and 11 were on the left side.
Nineteen of the patients in the small-incision, minimal dissection group had previous surgery in or around the eye on the ptotic side, and five had had more than one procedure. Previous surgeries included 11 cataract surgeries, three glaucoma surgeries, two corneal transplants, and two retinal surgeries. There were one each of dacryocystorhinostomy, LASIK, strabismus surgery, and removal of an orbital cavernous hemangioma. Twenty-one of the patients in the traditional group had previous surgery in or around the eye on the ptotic side, and six had more than one procedure. Previous surgeries included eight cataract surgeries, one glaucoma surgery, two corneal transplants, six retinal surgeries, three enucleations (with each of these patients having a secondary orbital implant), two punctual occlusions, one dacryocystorhinostomy, and one strabismus surgery.
In the small-incision, minimal dissection group, 24 patients had a history of other medical conditions. The most common were hypertension (14 patients), diabetes mellitus (five patients), stable thyroid abnormality (five patients), and rheumatoid arthritis (one patient). In the traditional group, 22 patients had a history of other medical conditions. The most common were hypertension (eight patients), diabetes mellitus (three patients), stable thyroid abnormality (six patients), and rheumatoid arthritis (three patients).
There was a family history of ptosis in three patients in the small-incision, minimal dissection group and in seven patients in the traditional group.
Statistical Methods
Comparison between groups of patient-level data (eg, age, sex) made use of two-sample independent statistical tests (eg, Student’s t test, chi-square test). Because lid height contrasts involved data from 26 eyelids of 13 patients who had bilateral procedures and 23 eyelids of 23 patients who had unilateral procedures in each group, comparisons of means treated subjects as a random effect and thereby adjusted for intereye dependency, using SAS Proc Mixed software. For comparisons of frequencies between groups, the generalized estimating equation was used to adjust for intereye dependency using SAS Proc Genmod software.
RESULTS
A summary of the results for each group and significance of differences is in Table 1. In the small-incision, minimal dissection group, the criteria of the lids being within 0.5 mm of each other and the operated lid being between 2 and 4 mm above the center of the pupil were met for 24 (66.7%) of the 36 patients, with both lids being low on one bilateral patient. In the traditional group, using the same criteria, criteria were met in 22 (61.1%) of 36 patients, with both lids being low on one bilateral patient.
Table 1.
Summary of results: comparing those for correcting aponeurotic ptosis with the small-incision, minimal dissection procedure and the traditional procedure
| Item | Small-incision, minimal dissection | Traditional | Significance of difference |
|---|---|---|---|
| Meets criteria of ≤0.5 mm between eyelids with operated lids being 2 to 4 mm above the center of the pupil | 66.7% | 61.1% | NSD |
| ≤0.5 mm difference in eyelid height | 75.0% | 63.9% | NSD |
| Clinical decision for reoperation | 25.0% | 31.0% | NSD |
| Satisfactory eyelid contour | 97.6% | 78.4% | P = .01 |
| Mean surgical time per lid | 26.3 minutes | 56.6 minutes | P < .0001 |
NSD, nonsignificant difference: P> .05.
The lid height difference postoperatively was ≤0.5 mm in 27 patients (75%) in the small-incision, minimal dissection group, with six of the nine failures being in the bilateral group. Of these six, one was a bilateral undercorrection, three were unilateral undercorrections (<2 mm), one was asymmetry of 1.5 mm with each lid in the acceptable range of 2 to 4 mm, and one was a unilateral overcorrection (5.0 mm above the center of the pupil). Of the three unilateral cases, two were <2 mm above the pupil, and one was 2.5 mm but 1.5 mm lower than the other side. The difference between the two sides when the difference was greater than 0.5 mm was 3.0 mm in one patient, 2.0 mm in one patient, 1.5 mm in four patients, and 1.0 mm in two patients. The lid height difference postoperatively was ≤0.5 mm in 23 patients (63.9%) in the traditional group, with four of the failures being in the bilateral group. Of these four, two were unilateral undercorrections and two had asymmetry of 1.0 mm with each lid in the acceptable range of 2 to 4 mm. For the nine unilateral cases, two were undercorrections, one was an overcorrection (5.0 mm above the center of the pupil), and six were in the range of 2.0 to 4.0 mm above the center of the pupil, but each had the operated side higher. The difference between the two sides when the difference was greater than 0.5 mm was 2.0 mm in three patients, 1.5 mm in six patients, and 1.0 mm in four patients.
The clinical decision to recommend reoperation in the small-incision, minimal dissection group was made for only the nine patients (25%) who showed >0.5 mm difference in eyelid height. There were six patients with one lid 1.5 mm above the center of the pupil and the other lid 2 mm. In two of these patients, the lowest lid was the unoperated lid, each having fallen 0.5 mm compared to the preoperative position. All six were satisfied with their lid heights, and reoperation was not recommended. In the traditional group, clinical decision for reoperation was made in 11 patients (31%), nine of whom showed >0.5 mm difference in eyelid height, one bilateral case where each lid was similarly low, and one case where the central lid height was fine but the lid was low medially. For this last patient, the medial suture was replaced in the office 1 week postoperatively. Recommendation for reoperation among patients with a lid difference of >0.5 mm was not made in four patients, three with a difference of 1.0 mm and one with a difference of 2.0 mm. Of the three with 1.0 mm difference, one patient had bilateral surgery, and in two patients the operated side was the highest and both lids were within normal range. One 70-year-old patient with the operated lid at 3.5 mm and the unoperated lid at 1.5 mm felt she could see fine and was pleased, so additional surgery was not recommended.
The frequency of a patient not meeting the criteria of the lids being within 0.5 mm of each other and the operated lid being between 2 and 4 mm above the center of the pupil and within 0.5 mm of each other was not significantly different in the two groups. The frequency of a lid being <2 mm or >4 mm above the center of the pupil when evaluated using SAS Genmod with generalized estimating equation to adjust for intereye dependency is not significantly different between the small-incision, minimal dissection group and the traditional group (P = .40). The incidence of the lids not being within 0.5 mm of each other was not significantly different in the two groups. The frequency of the clinical decision to recommend reoperation, analyzed using the chi-square test, is not significantly different in the two groups (P = .80).
Of the 49 lids operated on with the small-incision procedure, 34 received one suture, nine received two sutures, all placed laterally, and six received three sutures. Of the 49 lids operated on with the traditional procedure, two received one suture, three received two sutures, all placed medially, and 44 received three sutures.
The eyelid contour, as judged from postoperative photographs, was normal in all but one lid of the 32 patients (10 bilateral) with available postoperative photos in the small-incision, minimal dissection group. In that patient, the lid was lower laterally and had received three sutures. In the traditional group, the lid contour was normal in 29 lids of 27 patients (10 bilateral) with available postoperative photographs, with one flat centrally, three low medially, and four low laterally. The frequency of a good lid contour, 41 (97.6%) of 42 for the small-incision, minimal dissection group, is significantly greater than found for the traditional group, 29 (78.4%) of 37 by the Fisher exact test (P = .01).
The time for each procedure was obtained from the operating room records. The mean time from the beginning of the procedure to closure of the wound for the small-incision, minimal dissection group was 26.3 minutes (SE = 0.1 minute), with a range of 13 to 68 minutes. The mean operating time for the traditional group was 56.6 minutes (SE = 2.5 minutes), with a range of 35 to 119 minutes. The mean time required for the small-incision, minimal dissection group is significantly less than for the traditional group (P < .0001).
DISCUSSION
The small-incision, minimal dissection ptosis correction procedure is easy to do and to teach. The minimal dissection required means that the anatomy is less disrupted and probably explains the significantly higher rate of good eyelid contour outcome. It is a procedure that is usable usually only in eyelids that have not had previous lid surgery or trauma, because the anatomy should be in its original state to allow the blunt dissection. The first pass of the needle through the aponeurosis is nearly always effective in securing it but should always be checked by having the patient look up. One suture was sufficient in 69% of the cases, and all had a good contour outcome. The dissection to add a second suture is quick: of the patients requiring two sutures, the time of operation was less than the mean time in five, and only one of the others was an outlier, at 50 minutes. Of the six patients requiring three sutures, four were outliers, requiring 50 minutes, 68 minutes, and a bilateral case averaging 61 minutes per side. The extra time spent on these outliers suggests there was difficulty getting the contour satisfactory, although the only nonsatisfactory contour was in one lid of a bilateral patient with three sutures per side but averaging 32 minutes per side.
Use of a single suture was introduced by Liu4 in 1993. Meltzer and coworkers5 in 2001 presented excellent results with an adjustable single suture. Lucarelli and Lemke6 published the first small-incision ptosis procedure and used primarily a single suture, adding additional sutures as needed, in a similar fashion as in this report. However, their dissection was similar to the traditional dissection—finding and opening the orbital septum, retracting the fat to identify the levator aponeurosis, cutting the aponeurosis from Müller’s muscle, and then attaching it to tarsus. They state that the procedure requires less operative time than a full-incision external levator repair, but no data were provided.
Although there was no attempt to match the patients in the two groups beyond meeting the inclusion and exclusion criteria, and ensuring that the same number of bilateral cases were included in the traditional group as in the small-incision, minimal dissection group, they are remarkably similar in age, female-male mix, prior surgery on the affected side, and concomitant medical conditions. There is a preponderance of women in each group, 75% in the small-incision, minimal dissection group and 72% in the traditional group. In the failed cases of McCulley and coworkers,7 52 (72.2%) of 72 subjects were female, and in the 125 successful cases they analyzed, 72 (57.6%) were women. In the patients of Bartley and coworkers,8 9 (52.9%) of 17 were women. In the series of Lucarelli and Lemke,6 11 (64.7%) of 17 patients were female.
Although this is a retrospective study, there are complete data for every aspect studied except for postoperative photographs to judge contour. Photos were available for 89% of the small-incision, minimal dissection group and 75% of the traditional group. Looking at those for whom reoperation was recommended, seven (78%) of nine patients in the small-incision, minimal dissection group and 6 (55%) of 11 of the traditional group had photographs. Circumstance (photography department was closed) or error of omission, rather than bias, accounts for the less than 100% availability of photographs, because it is our policy to get photographs of every postoperative ptosis-correction patient at the 2-month postoperative visit. The photograph evaluator (B.R.F.) was not masked to the surgical method used; evaluation by a different, masked observer would be preferable. To comply with IRB/HIPAA regulations, and not have to contact each subject for permission, each chart and accompanying photographs were examined and the data recorded, and the records were returned, with no link remaining to connect the data collected to the patient. We believe the drawbacks of less than complete availability of photographs and nonmasked evaluation do not change the conclusion that good contour was achieved in a higher percentage of the small-incision, minimal dissection group than of the traditional group.
The ideal position of a corrected ptotic lid will depend on at least three factors: whether the patient has a dry-eye problem or even reduced tear production on Schirmer’s test; the height of the other eyelid, if the ptosis is unilateral; and the height of the patient’s lid prior to the onset of the ptosis. These are factored in and a clinical judgment is arrived at. For this reason, we did not calculate the mean elevation or the mean final position of the operated lids. Means would not convey the desired outcomes of surgery.
Whereas follow-up time was not contrasted between groups, all patients had a minimum of 2 months of follow-up. For the past 15 years, based on prior experience, when patients have adequate lid position at 2 months, they are discharged from care. This approach is supported by the data of Doxanas,9 who followed 150 patients for a minimum of 3 years and up to 5 years and reported no case of late recurrence. If patients were overcorrected or undercorrected, this was evident 1 week postoperatively in his patients. Berlin and Vestal10 did report 15 failures in 62 patients occurring after the 6-week visit when using 6-0 polyglactin suture. Use of absorbable suture in aponeurotic ptosis correction can lead to late failure, and this knowledge had led the surgeon (B.R.F.) to sole use of permanent suture for aponeurotic ptosis correction.
Table 2 shows the outcomes of 11 investigators2,4–13 in relation to meeting their criteria for successful lid position when operating for acquired ptosis. Only two7,10 of the 11 reports defining success specify not only a maximum difference in lid height but a range above the pupil that is acceptable. These two reports presented the most detailed and useful information on surgical outcome. Although Table 2 shows specific success rates for the report by McCulley and coworkers,7 these are estimates, with a range of success within a 95% confidence limit of 71% to 83% for unilateral patients and 67% to 82% for bilateral patients. The success rates in McCulley and coworkers and Berlin and Vestal10 are similar to ours, given our tighter criteria for lid difference and maximum acceptable eyelid height. It seems important that both difference in lid height and an acceptable range of lid position should be specified to truly define success. Clearly, two lids that postoperatively bisect the center of the pupil represent failed operations, although there is no difference between the height of the two lids.
Table 2.
Other reports of the results of surgery for correcting aponeurotic ptosis
| Author | Year | Criteria used, difference and range | Timing of determination | No. meeting criteria | No. done | % meeting criteria |
|---|---|---|---|---|---|---|
| Anderson et al2 | 1979 | 1.0 mm | 10 | 12 | 83.3 | |
| Older12 | 1983 | 1.0 mm | 108 | 113 | 95.6 | |
| Putterman et al11 | 1986 | 1.5 mm | 192 | 213 | 90.1 | |
| (1.0 mm) | 177 | 213 | 83.1 | |||
| (0.5 mm) | 137 | 213 | 64.3 | |||
| Berlin et al10 | 1989 | 1.0 mm and 2–4.5 mm | 6 weeks | 62 | 87 | 71.3 |
| Long term, up to 6.7 mo | 47 | 87 | 54.0 | |||
| Shore et al12 | 1990 | 1.0 mm and ≥ 3mm for bilat | 178 | 207 | 89.5 | |
| Doxanas9 | 1992 | 1.0 mm | 86 | 92 | 93.5 | |
| Liu4 | 1993 | 1.0 mm | 162 | 169 | 95.9 | |
| Bartley et al8 | 1996 | 1.0 mm | 11 | 17 | 64.7 | |
| Lucarelli et al6 | 1999 | 1.0 mm | 25 | 28 | 89.3 | |
| Meltzer et al5 | 2001 | 0.5 mm | 46 | 51 | 89.3 | |
| McCulley et al7* | 2003 | 1.0 mm and 2–4.5 mm | Unilateral | 404 | 77.0 | |
| Bilateral | 399 | 76.0 |
The success rates for McCulley and coworkers are estimates with a range, so no numbers meeting criteria are given.
The acceptable difference in lid height above the center of the pupil was 1.0 mm in most of the reports. One report11 found a difference of 1.5 mm acceptable for a successful operation. Using that criterion, 20 (28%) of our 72 patients did not need surgery in the first place. The same report had data imbedded which showed that if a 1.0-mm difference was used, the success rate dropped from 90.1% to 83.1%, and if a 0.5 mm difference was used, it dropped to 64.3%. Only one report5 mentioned success as being within 0.5 mm. Tight criteria for success in this report were chosen prior to obtaining the data: we sometimes operate for 1.0 mm of ptosis, and a normal range for lid position above the center of the pupil seemed to be 2 to 4 mm. Three (6.5%) of the 46 unilateral cases had a 1 mm difference in lid height preoperatively, confirming that judgment. Berlin and Vestal10 made an important philosophic comment: “The success rate is determined by what one is willing to accept as a good result. Expectations were less with earlier techniques and therefore, more postoperative ptosis was tolerated than would be considered cosmetically acceptable today.” This is every bit as true 15 years later.
Reoperation rate, which was not significantly different between the two groups, has a significant subjective component that does not necessarily align with the results of eyelid height. In one instance, a patient in the traditional group with 2 mm difference in lid height was satisfied, and no reoperation was recommended. There were also two patients in the traditional group with a 1.5 mm difference, and reoperation was recommended but further surgery was declined. Had those patients been listened to more carefully before surgery was recommended, those patients might well have fallen into the “no reoperation recommended” group. Objective measurements of eyelid position are a better benchmark of surgical success than reoperation rate.
While McCulley and coworkers7 found a similar success rate for unilateral and bilateral ptosis correction, 77% and 76% respectively, the reoperation rate was very different, at 5.2% for those having had unilateral surgery and 13% for those having had bilateral surgery. In our small-incision, minimal dissection group, 13% of the unilateral patients were recommended to have reoperation compared to 46% of the bilateral group. This diversion was not seen in the traditional group, where 30% of the unilateral and 31% of the bilateral patients were recommended to have reoperation. The numbers in our groups are too small to show these differences to be significant. However, on the basis of these data, we have increased our awareness of differences in bilateral cases.
Overcorrections occurred in only one patient in each of the two groups in this report, or two (7%) of the 28 that did not meet our strictest criteria. Bartley and coworkers8 reported overcorrections in four of six patients (67%) who had a difference of >1 mm between the two lids. Considering that they felt the four higher lids were each properly positioned, they had no functional overcorrections among the 17 eyelids and the likelihood of functional overcorrection was similar to ours. McCulley and coworkers7 reported overcorrections in 39 (54%) of 72 failures. These differences probably reflect the conservative bias of the surgeon (B.R.F.): an undercorrection is less onerous than a symptomatic dry eye from an upper eyelid that is too high.
In the United States, we are working at a time of decreasing surgical reimbursements. The Michigan Medicare screen for code 67904, correction of ptosis, external approach, has decreased 40% since 1995, from $942 to $554. Overhead has increased in that interval. That the small-incision, minimal dissection procedure can be done in less than half the time, on average, thus has economic significance. That the standard error is less with this procedure means there is greater predictability of the operating time, facilitating scheduling. We found no other reports of operative time to use for comparison.
In conclusion, the outcome of small-incision, minimal dissection ptosis correction in terms of eyelid height is similar to that of the traditional dissection, and success in achieving a good eyelid contour is significantly greater with the small-incision, minimal dissection procedure. The small-incision, minimal dissection procedure is significantly quicker to perform. These findings should make the small-incision, minimal dissection ptosis correction procedure the surgical procedure of choice in previously unoperated cases of aponeurotic ptosis to be corrected with aponeurotic surgery.
DISCUSSION
Dr George B. Bartley
When entering the operating room, it is useful to remember the aphorism “the longer you stay, the longer you stay”, as it reminds us to get the job done with as little invasion as possible, and then get out.
A corollary lesson from this fine study by Dr Frueh and coworkers might be: “the more you do, the more you do.” Specifically, the dissection used in the traditional approach to levator aponeurosis repair required more sutures—3 of them in 90% of cases—but yielded less favorable results in terms of eyelid contour. This has an interesting implication: given that the primary difference between the traditional “open sky” technique and the small incision/minimal dissection is maintenance of orbital septum integrity, perhaps the role of this structure in eyelid support and function is more important than is generally assumed. Sounds like a potential AOS thesis to me.
While we’re thinking about the orbital septum, two other caveats deserve mention. First, it’s critical for occasional ptosis surgeons who may wish to adopt the small incision technique to avoid snagging the septum when the levator aponeurosis is advanced, because doing so carries the risk of eyelid lag and lagophthalmos. Second, the small incision technique may not be practical in Asian eyelids that lack an eyelid crease. In such eyelids the orbital septum fuses with the aponeurosis much more inferiorly than in occidental eyelids, allowing the preaponeurotic fat to extend down over the tarsal plate. Transgression of the orbital septum is inevitable unless the incision is made just superior to the eyelash follicles.
Moving from anatomy to outcomes, Dr Frueh states “Objective measurements of eyelid position are a better benchmark of surgical success than re-operation rate.” This unquestionably is true when doing a comparative study, but the re-operation rate is a useful measure of patient satisfaction given that ptosis surgery has a significant subjective component. This is particularly true when surgery is performed to correct 1 mm of ptosis, cases that are done primarily for aesthetic improvement rather than to enlarge the superior visual field.
An editorial comment about reimbursement for CPT code 67904. Since moving to Florida, I have been surprised and dismayed by how often third-party payers deny payment for the repair of ptosis, even when the eyelid rests inferior to the pupil or is completely closed, as may occur with an oculomotor nerve palsy. Because the reimbursement for ptosis repair has dropped considerably during the past decade and may well be below cost for many practices, perhaps oculoplastic surgeons should be arguing that the operation is indeed cosmetic, as this would allow charges to be set at market rates. That might raise a few eyebrows, if not eyelids.
Dr Bartley Frueh
I thank Dr Bartley for his cogent discussion.
ACKNOWLEDGMENT
The authors thank Kenneth E. Guire, MS, Department of Biostatistics, School of Public Health, University of Michigan, for his sophisticated data analysis that enabled bilaterality of some procedures to be appropriately dealt with in outcome evaluation.
REFERENCES
- 1.Jones LT, Quickert MH, Wobig JL. The cure of ptosis by aponeurotic repair. Arch Ophthalmol. 1975;93:629–634. doi: 10.1001/archopht.1975.01010020601008. [DOI] [PubMed] [Google Scholar]
- 2.Anderson RL, Dixon RS. Aponeurotic ptosis surgery. Arch Ophthalmol. 1979;97:1123–1128. doi: 10.1001/archopht.1979.01020010577015. [DOI] [PubMed] [Google Scholar]
- 3.Older JJ. Levator aponeurosis tuck: a treatment for ptosis. Ophthalmic Surg. 1978;9:102–110. [PubMed] [Google Scholar]
- 4.Liu D. Ptosis repair by single suture aponeurotic tuck. Surgical technique and long-term results. Ophthalmology. 1993;100:251–259. doi: 10.1016/s0161-6420(93)31662-3. [DOI] [PubMed] [Google Scholar]
- 5.Meltzer MA, Elahi E, Taupeka P, et al. A simplified technique of ptosis repair using a single adjustable suture. Ophthalmology. 2001;108:1889–1892. doi: 10.1016/s0161-6420(01)00712-6. [DOI] [PubMed] [Google Scholar]
- 6.Lucarelli MJ, Lemke BN. Small incision external levator repair: technique and early results. Am J Ophthalmol. 1999;127:637–644. doi: 10.1016/s0002-9394(99)00064-1. [DOI] [PubMed] [Google Scholar]
- 7.McCulley TJ, Kersten RC, Kulwin DR, et al. Outcome and influencing factors of external levator palpebrae superioris aponeurosis advancement for blepharoptosis. Ophthal Plast Reconstr Surg. 2003;19:388–393. doi: 10.1097/01.IOP.0000087071.78407.9A. [DOI] [PubMed] [Google Scholar]
- 8.Bartley GB, Lowry JC, Hodge DO. Results of levator-advancement blepharoptosis repair using a standard protocol: effect of epinephrine-induced eyelid position change. Trans Am Ophthalmol Soc. 1996;94:165–173. [PMC free article] [PubMed] [Google Scholar]
- 9.Doxanas MT. Simplified aponeurotic ptosis surgery. Ophthalmic Surg. 1992;8:512–515. [PubMed] [Google Scholar]
- 10.Berlin AJ, Vestal KP. Levator aponeurosis surgery. A retrospective review. Ophthalmology. 1989;96:1033–1037. [PubMed] [Google Scholar]
- 11.Putterman AM, Fett DR. Muller’s muscle in the treatment of upper eyelid ptosis: a ten-year study. Ophthalmic Surg. 1986;17:354–360. [PubMed] [Google Scholar]
- 12.Older JJ. Levator aponeurosis surgery for the correction of acquired ptosis. Analysis of 113 procedures. Ophthalmology. 1983;90:1056–1059. doi: 10.1016/s0161-6420(83)80047-5. [DOI] [PubMed] [Google Scholar]
- 13.Shore JW, Bergin DJ, Garrett SN. Results of blepharoptosis surgery with early postoperative adjustment. Ophthalmology. 1990;97:1502–1511. doi: 10.1016/s0161-6420(90)32384-9. [DOI] [PubMed] [Google Scholar]