Abstract
The fitness cost of a resistance determinant is the primary parameter that determines its frequency in vivo. As a model for analysis of the impact of drug resistance mutations on the intracellular life cycle of Chlamydia spp., we studied the growth of four genetically defined spectinomycin-resistant (Spcr) clonal variants of Chlamydia psittaci 6BC isolated in the plaque assay. The development of each variant was monitored over 46 h postinfection in the absence of drug, either in pure culture or in 1:1 competition with the parent strain. Spcr mutations in the 16S rRNA gene at positions 1191 and 1193 were associated with a marked impairment of C.psittaci biological fitness, and the bacteria were severely outcompeted by the wild-type parent. In contrast, mutations at position 1192 had minor effects on the bacterial life cycle, allowing the resistant isolates to compete more efficiently with the wild-type strain. Thus, mutations with a wide range of fitness costs can be selected in the plaque assay, providing a new strategy for prediction and monitoring of the emergence of antibiotic resistance in chlamydiae. So far, drug resistance has not been a serious threat for the treatment of chlamydial infections. Tetracycline is an effective antichlamydial drug that targets 16S rRNA. Attempts to isolate spontaneous tetracycline-resistant mutants of C. psittaci 6BC revealed a frequency <3 × 10−9. We suggest that the rarity of genotypic antibiotic resistance among chlamydial clinical isolates reflects the deleterious effects of such mutations on the fitness of these obligate intracellular bacteria in the host.
Members of the genus Chlamydia are obligate intracellular gram-negative bacteria that cause a variety of diseases in animal species at virtually all phylogenic levels, from amphibians and reptiles to birds and mammals (11). Contemporary differentiation distinguishes nine species, of which three are relevant to human medicine. Chlamydia trachomatis causes trachoma and urogenital infections; C. pneumoniae is one of the most common agents of atypical community-acquired pneumonia; and C. psittaci is the etiologic agent of psittacosis, a severe zoonotic pneumonia transmitted by birds. Individuals infected with chlamydiae exhibit a wide spectrum of responses, ranging from asymptomatic or paucisymptomatic to late-stage complications (11). In addition, acute infections can progress to chronic diseases that constitute a major public health burden worldwide (1, 15).
To date, there is no vaccine against human chlamydial infections, and antibiotic therapy remains the only line of defense available. However, acute infections treated with noncidal antibiotics can lead to the development of persistent, nonreplicating bacteria, with the corollary that these persistent chlamydiae can resist eradication by further antimicrobial treatment and cause chronic disease (for reviews, see references 19 and 21). In addition, members of the family Chlamydiaceae are characterized by a biphasic developmental cycle of replication in which only one developmental form, named the reticulate body (RB), is fully metabolically active and thus sensitive to the antichlamydial antibiotics of choice, i.e., tetracycline (TET) or its derivatives, such as doxycycline, and macrolides, such as azithromycin and erythromycin. The second developmental form is the infectious but metabolically inactive elementary body (EB) that is endocytosed by a susceptible eukaryotic cell and resides within a cytoplasmic vacuole termed the inclusion, where it transforms into the RB. After replicating by binary fission, RBs transform back to the infectious form 18 to 48 h postinfection, depending on the species, before being released to the cell's exterior and starting new replicative cycles in neighboring host cells (49).
Chlamydial infections are characterized by a high recurrence rate, despite appropriate drug therapy, yet clinical failures linked to real genotypic resistance due to chromosomal mutations have rarely been reported (43, 47). This suggests that mutations that confer antibiotic resistance in chlamydiae are not selected in vivo. However, we have previously used the plaque assay to demonstrate that spontaneous mutations arise in vitro in Chlamydia spp. at a frequency similar to that in other eubacteria (8). In particular, the frequencies of rifampin resistance are in the same range for C. trachomatis L2 and C. psittaci 6BC (i.e., 10−7), whereas the frequency of resistance to the ribosome-targeting antibiotic spectinomycin is related to the number of rRNA copies present in the strains:, i.e., 5 × 10−5 for C. psittaci 6BC, which harbors a unique rRNA operon, similar to C. pneumoniae, and <2.4 × 10−8 for C. trachomatis L2, which has two rRNA chromosomal copies.
Whether drug-resistant organisms persist in nature depends on both the likelihood that they will occur and their fitness relative to that of their drug-sensitive counterparts (4, 24). One would expect a majority of rRNA mutations found in drug-resistant organisms to be associated with a biological fitness cost, as they may induce a localized conformation change inassembled ribosomes and interfere with the efficiency of protein synthesis. However, screening for spontaneous antibiotic-resistant chlamydial variants in the plaque assay should select only for the fittest bacteria, as their isolation depends on their capacity for both growth and cell-to-cell transmission. Hence, we compared the growth, in the absence of selection, of four genetically defined clonal spectinomycin (SPC)-resistant (Spcr) variants of C. psittaci 6BC originally isolated in vitro by plaque assay (8) with that of the susceptible parent strain either in pure culture or in competition. We found that the level of physiological burden on C. psittaci was dependent on the nature of the 16S allele expressed in the bacteria. Although specific mutations in 16S rRNA genes have also been associated with tetracycline resistance in Helicobacter pylori (12, 16, 45) and Propionibacterium acnes (38), we were unable to isolate spontaneous variants of C. psittaci resistant to this antibiotic in a plaque assay. The implications of these results on antibiotic treatment of chlamydial infections are discussed.
MATERIALS AND METHODS
Bacterial strains and antibiotics.
The bacterial strains used in this study are listed in Table 1. Escherichia coli strain DH5α was used for cloning purposes. E.coli strains were grown in Luria-Bertani (LB) broth with aeration or on LB agar. Antibiotics (all purchased from Sigma) were added at the following concentrations when required: 100 μg ml−1 ampicillin, 50 μg ml−1 kanamycin (KAN), 7.5μg ml−1 tetracycline (TET), and 20 μg ml−1 gentamicin. Various concentrations of SPC wereused.
TABLE 1.
Bacterial strains used in this study
| Strain | Description | Source or reference |
|---|---|---|
| C. psittaci | ||
| 6BC | C. psittaci serovar 6BC | T. Hatch |
| BC0E1 | C. psittaci serovar 6BC 16S1; Spcr | 8 |
| BC0A2 | C. psittaci serovar 6BC 16S2; Spcr | 8 |
| BCS18 | C. psittaci serovar 6BC 16S3; Spcr | 8 |
| BCS34 | C. psittaci serovar 6BC 16S4; Spcr | 8 |
| E. coli | ||
| DH5α | F−φ80Δ(lacZY-argF)U169 deoR recA1 endA1 phoA hsdR17 supE44 λ−thi-1 gyrA96 relA1 Δ(lacZ)M15 | 20 |
| JM109 | F′ Δ(lac-pro) glnV44 gyrA96 recA1 relA1 endA1 thi hsdR17 traD36 lac1q Δ(lacZ)M15 | 50 |
| ATM676 | JM109 transformed with pRAK244wt (wild-type E. coli rrnC operon in a pBR322 derivative) | This work |
| ATM680 | JM109 transformed with pRAK252mut1 (E. coli rrnC operon with 16S1 allele) | This work |
| ATM681 | JM109 transformed with pRAK253mut2 (E. coli rrnC operon with 16S2 allele) | This work |
| ATM771 | JM109 transformed with pRAK329mut5 (E. coli rrnC operon with 16S3 allele) | This work |
| ATM772 | JM109 transformed with pRAK356mut6 (E. coli rrnC operon with 16S4 allele) | This work |
| AVS69009 | E. coli Δ7 prrn strain: (ΔrrnE ΔrrnB ΔrrnA ΔrrnH ΔrrnG::lacZ ΔrrnC::cat ΔrrnD::cat ΔrecA/pTRNA66, pHKrrnC) | 34 |
| ATM692 | AVS69009 variant harboring pRAK244wt instead of pHKrrnC | This work |
| ATM693 | AVS69009 variant harboring pRAK252mut1 instead of pHKrrnC | This work |
| ATM694 | AVS69009 variant harboring pRAK253mut2 instead of pHKrrnC | This work |
| ATM773 | AVS69009 variant harboring pRAK329mut5 instead of pHKrrnC | This work |
| ATM774 | AVS69009 variant harboring pRAK356mut6 instead of pHKrrnC | This work |
Propagation of C. psittaci and L2 cells.
C. psittaci serovar 6BC was grown in mouse fibroblast L2 cells as described previously (8).
Construction and testing of E. coli rrnC plasmid derivatives.
pHKrrnC is a Kanr pBR322 derivative harboring the E. coli rrnC genomic region on a 8,465-bp PstI-BamHI fragment (5). This insert was subcloned into pBAD18, an ampicillin-resistant pBR322 derivative (18), creating pRAK244wt. To generate a C→T mutation (Mut1) or a C→G mutation (Mut5) at base 1192 of the 16S rRNA gene of the rrnC operon or a A→G mutation (Mut2) or a G→C mutation (Mut6) at base 1191 or 1193, respectively, site-directed mutagenesis was performed with pRAK248, a pBluescript II SK(+) (Stratagene) derivative harboring a 707-bp ApaI-XbaI fragment internal to the rrnC 16S rRNA gene. Complementary primers encompassing the sequence to be mutated and incorporating the required mutation (italicized) were designed for Mut1 (5′-GGAGGAAGGTGGGGA TGATGTCAAGTCATCATGG-3′ and 5′-CCATGATGACTTGACATCATC CCCACCTTCCTCC-3′), Mut2 (5′-GGAGGAAGGTGGGGATGGCGTCAAGTCATCATGG-3′ and 5′-CCATGATGACTTGACGCCATCCCCACCTTC CTCC-3′), Mut5 (5′-GGAGGAAGGTGGGGATGAGGTCAAGTCATCATGG-3′ and 5′-CCATGATGACTTGACCTCATCCCCACCTTCCTCC-3′), and Mut6 (5′-GGAGGAAGGTGGGGATGACCTCAAGTCATCATGG-3′ and 5′-CCATGATGACTTGAGGTCATCCCCACCTTCCTCC-3′). pRAK248 variants carrying these nucleotide substitutions could be selected by restriction analysis because the mutation generated destroys a unique AatII restriction site. The presence of the mutation in the selected plasmids was subsequently confirmed by DNA sequence analysis. Finally, the 16S mutant alleles were excised from the corresponding plasmids by cleavage with ApaI and XbaI and inserted into pRAK244wt, from which the ApaI-XbaI fragment was removed, resulting in plasmids pRAK252mut1, pRAK253mut2, pRAK329mut5, and pRAK356mut6.
The functionality of the 16S alleles in rrnC was studied in the E. coli strains AVS69009, in which all seven chromosomal rrn operons have been deleted (Δ7 prrn) and which expresses the plasmid-encoded E. coli rrnC operon exclusively, and JM109. Replacement of pHKrrnC in AVS69009 with pRAK244wt, pRAK252mut1, pRAK253mut2, pRAK329mut5, and pRAK356mut6 was performed as described by Asai et al. (5).
The effect of the incubation temperature on colony formation is expressed as plating efficiency, which is defined as the ratio of the colony formation at 37°C or 41°C to the colony formation at 30°C, as determined in the following way. Stationary-phase JM109 or AVS69009 transformants grown at 30°C in LB broth in the presence of the appropriate antibiotics were normalized to an optical density at 600 nm equivalent of 0.4. Bacteria were serially diluted in sterile BSG (150 mM NaCl, 2 mM KH2PO4, 4 mM Na2HPO4, 0.01% gelatin). For each dilution, aliquots of 100 μl were plated on LB agar plates with antibiotics; and two plates for each dilution were incubated at 30°C, 37°C, and 41°C for 28 h and 44 h for JM109 or AVS69009 derivatives, respectively, before the colonies were counted. The diameters of 15 random colonies were determined with a magnifying glass with graduations of 0.1 mm (7× PEAK Scale Lupe) for each strain at each temperature. Dunnett's test was performed with Prism 3.0 software (GraphPad Software, Inc., San Diego, CA) to compare the phenotypes obtained with the mutant alleles to those of the strains expressing the wild-type allele. The size index was defined as the size obtained at the same incubation temperature for each 16S allele compared to the size obtained with the wild-type allele expressed in JM109 or AVS69009. The MIC was determined by the twofold broth macrodilution method with exponential-phase cultures grown at 30°C. Each tube was inoculated with about 105 bacteria/ml in LB broth containing various concentrations of SPC. The MIC was defined as the lowest concentration where no growth was visible after an incubation of 32 h at 30°C.
Fitness costs of spectinomycin resistance in C. psittaci 6BC. (i) Determination of chlamydial growth rate by real-time quantitative PCR.
Confluent L2 monolayers in 60-mm2 dishes were infected at a multiplicity of infection (MOI) of 1 with 107 PFU of wild-type C. psittaci 6BC, BC0A2, BC0E1, BCS18, or BCS34 and incubated at 37°C in 5% CO2. After 2 h of infection, the inoculum was removed and the cells were washed twice with Dulbecco's modified Eagle medium (DMEM; GIBCO). The infected L2 cells were then incubated for up to 46 h in DMEM supplemented with 10% fetal bovine serum (FBS), 1× MEM nonessential amino acids (Sigma-Aldrich), and 2 μg of cycloheximide per ml. Total DNA was collected after RNase A treatment in 200 μl of elution buffer with DNeasy tissue kits (QIAGEN) at 2, 10, 13, 16, 19, 24, 29, 34, 37, 40, 43, and 45.5 h postinoculation (p.i.).
Real-time PCR was performed in triplicate for each time point with an ABI Prism 7000 sequence detection system (Applied Biosystems) by using 1× SYBR green PCR master mixture (Applied Biosystems) in a 25-μl reaction volume containing 300 nM of specific bacterial or eukaryotic primers. C. psittaci primers were selected from the 16S rRNA gene, primers RT1 (5′-ACCCTAAGTGTTGGCAACTAACG-3′) and RT2 (5′-TTTCCGCAAGGACAGATACACAG-3′), which amplify a 118-bp fragment only from total DNA from infected cells. Mouse-specific primers were selected from the Mus musculus hypoxanthine guanine phosphoribosyl transferase (hprt) mRNA sequence (GenBank accession number BC004686), primers RT3 (5′-TTGCTCGAGATGTCATGAAGGA-3′) and RT4 (5′-AGCAGGTCAGCAAAGAACTTATAGC-3′), which amplify a 90-bp fragment absent from the C. psittaci genome. Cycling parameters were 95°C for 10 min to activate the DNA polymerase and then 40 cycles of 95°C for 15 s and 60°C for 1 min, with a final recording step of 60°C for 20 s. Melting curve analyses were performed with Dissociation Curves software (Applied Biosystems) to ensure that only a single product was amplified.
Relative standard curves were designed by using serial dilutions of total DNA obtained from the C. psittaci wild-type strain at 43 h p.i. (linear correlation coefficient [R2] > 0.99). Each time point was consecutively reported as a fold dilution of this calibrator with Prism 3.0 software (GraphPad Software, Inc.). To compensate for any variation in the amount of starting material between the samples, the bacterial 16S rRNA gene data for each sample were normalized with the value obtained with the eukaryotic hprt gene. The normalized values were then related to the value obtained at 2 h p.i. to estimate the change in chlamydial DNA accumulation relative to the amount obtained 2 h p.i. Pearson analysis was performed with the values obtained. The correlation coefficients (r2values) were 0.8780, 0.8761, 0.8109, 0.8669, and 0.8380 for 6BC wild-type, BC0E1, BC0A2, BCS18, and BCS34, respectively. The normalized values were then fitted by using a Gompertz equation (R2 > 0.99) and the Prism 3.0 software to calculate the lag phase. The doubling time was estimated from a plot of ln (fold) = f (time) (R2 > 0.99), where the slope is ln 2/doubling time (h). The relative fitness is the ratio of doubling time for the wild type to the doubling time for the mutant (29).
(ii) Pairwise competition experiment.
C. psittaci 6BC wild-type cells and each Spcr variant were coinfected at a ratio of ∼1:1 to an MOI of 1 in 60-mm2 dishes containing confluent mouse fibroblasts and incubated at 37°C in 5% CO2. After 2 h of infection, the inoculum was removed. The cells were washed twice with DMEM and incubated in DMEM supplemented with 10% FBS, 1× MEM nonessential amino acids, and 2 μg of cycloheximide per ml. EBs were harvested in triplicate after sonication of the infected cells at 4 h p.i., 10 h p.i., and every 3 h afterwards up to 46 h p.i. and stored at −80°C in 200 μl SPG (250 mM sucrose, 10 mM sodium phosphate, 5 mM l-glutamic acid). Subsequently, EBs were harvested in duplicate after sonication of the infected cells at 19, 24, 29, 34, and 46 h p.i. Approximately 5 × 106 infectious particles from the mixed infection at 46 h p.i. were passed a second time into fresh 60-mm2 dishes, allowed to grow for another 46 h, and harvested as described above. The titers of serial dilutions of each harvest were determined in duplicate in the plaque assay in both drug-free (total PFU) and drug-containing DMEM (Spcr PFU). The plaques were counted after 10 days of incubation, as reported previously (8). The plating efficiency of each resistant mutant was unaffected by the presence of SPC. Similarly to the DNA accumulation assay, the twofold PFU increase rate was estimated from a plot of ln (PFU) = f (time), where the slope is ln 2/twofold PFU increase rate (h). The relative fitness is the ratio of the twofold PFU increase rate for the wild type to the twofold PFU increase rate for the mutant. The competition index was defined as the ratio of the output mutant-to-wild type ratio to the input mutant-to-wild type ratio (14, 26). The final competition index is the competition index determined at 46 h p.i. for each passage related to the initial input mutant-to-wild type ratio.
Titration, antimicrobial susceptibility, and isolation of chlamydial mutants by plaque assay.
The susceptibility of C. psittaci 6BC to TET was examined in a plaque assay (8). The MIC was defined as the drug concentration that inhibits the development of 105 chlamydial PFU in a confluent L2 monolayer in a 60-mm2 dish (8). To isolate spontaneous drug-resistant variants, 60-mm2 dishes were infected with 107 to 108 PFU (MOI, 1 to 10) and the drug was added at 2 h p.i. at a concentration high enough to inhibit the cytotoxicity associated with this inoculum size.
RESULTS
Phenotype conferred by the chlamydial Spcr alleles in E.coli.
In a previous study (8), we have isolated, by plaque assay in the presence of spectinomycin, 59 clonal variants of C.psittaci 6BC and characterized four independent mutations in the unique 16S rRNA gene that are associated with resistance of the organisms to the antibiotic (Table 2). Whereas the two mutations found in BC0E1 and BCS18 at position 1192 (by use of the E. coli numbering system) have been previously isolated in other Spcr bacteria, mutations at position 1091 and 1093 found in BC0A2 and in BCS34, respectively, have been described only in Spcr chloroplasts of Chlamydomonas reinhardtii (http://server1.fandm.edu/departments/Biology/Databases/16SMDBexp.html). Phylogenetic and genomic analyses have linked members of the family Chlamydiaceae with the cyanobacterial and chloroplast lineage (10). The 16S2 and 16S4 Spcr alleles in C. psittaci would strongly strengthen this proposed linkage if they did not impart the same phenotype to bacterial species that are evolutionarily distant from chloroplasts, such as E. coli. Thus, each of the four mutant 16S alleles isolated in C. psittaci was re-created by site-directed mutagenesis of the E. coli ribosomal rrnC operon present in plasmid pRAK244wt, resulting in pRAK252mut1, pRAK253mut2, pRAK329mut5, and pRAK356mut6.
TABLE 2.
Characteristics of the 16S Spcr allelesa
| Designation | Nucleotide change | Representative chlamydial mutant | Allele distribution in drug-resistant organisms | SPC MIC (μg/ml)
|
||
|---|---|---|---|---|---|---|
| C. psittaci 6BCb | E. coli JM109 variants | E. coli AVS69009 variants | ||||
| Wild type | NAc | NA | NA | 20 | 20 | 10 |
| 16S1 | C1192U | BC0E1 | E. coli, Neisseria spp. Nicotiana tabacum chloroplast | >10,000 | >5,120 | ≫5,120 |
| 16S2 | A1191G | BC0A2 | Chlamydomonas reinhardtii chloroplast | >10,000 | >5,120 | ≫5,120 |
| 16S3 | C1192G | BCS18 | E. coli | >10,000 | >5,120 | ≫5,120 |
| 16S4 | G1193C | BCS34 | Not previously reported (C. reinhardtii chloroplast for G1193A) | 5,000 | 20 | ≫5,120 |
Each distinct mutation identified was given an allele name (designation), which represents a specific change at the indicated nucleotide in the 16S rRNA sequence (E. coli numbering).
Data are from reference 8.
NA, not applicable.
The five plasmids were then separately introduced into two different E. coli strains for analysis. JM109 contains the full complement of seven rRNA operons, while AVS69009 expresses only one rRNA operon, encoded by pHKrrnC (5). All five plasmids, pRAK244wt, pRAK252mut1, pRAK253mut2, pRAK329mut5, and pRAK356mut6, displaced the kanamycin-resistant pHKrrnC, indicating that homogeneous ribosome populations containing rRNA from the mutant 16S1, 16S2, 16S3, and 16S4 alleles, respectively, were functional in E. coli. In addition, AVS69009 variants expressing each mutant allele were more than 500 times more resistant to SPC than the strain expressing the wild-type allele, with the MICs being greater than 5.12 mg/ml, whereas they were 10 μg/ml for the wild-type parent (Table 2). Similarly, each allele except 16S4 conferred a high level of SPC resistance to the wild-type E. coli strain, with the MICs being greater than 5.12 mg/ml for JM109 cells transformed with pRAK252mut1, pRAK253mut2, or pRAK329mut5, whereas the MICs were 20 μg/ml for pRAK244wt. On the other hand, pRAK356mut6 conferred spectinomycin resistance to E. coli only in the AVS69009 strain but not in the context of the seven wild-type rRNA chromosomal copies in JM109, indicating that the resistance phenotype associated with the 16S4 allele was recessive and required homogeneous populations of ribosomes for expression in organisms.
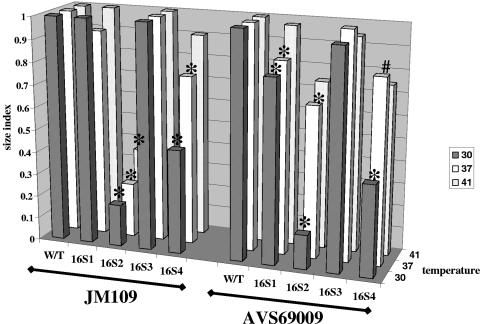
As reported earlier (28), we did not observe any serious growth defect associated with the expression of the 16S1 or the 16S3 allele in E. coli (P > 0.05). On the other hand, E. coli transformed with the 16S2 (ATM681 and ATM694) or 16S4 (ATM772 and ATM774) Spcr alleles formed much smaller colonies on nonselective agar plates, especially at 30°C (Pvalues < 0.001), indicating slower growth characteristics (Fig. 1). The plating efficiency was similar for all strains except the AVS69009 cells harboring pRAK253mut2. Indeed, the numbers of colonies for the latter variant at 41°C and 37°C were 0.36% and 5.9%, respectively, the number determined at 30°C, indicating some degree of thermosensitivity (data not shown). Interestingly, the surviving colonies appeared to be the fast growers in the ATM694 population (Fig. 1). Thus, both “chloroplastic” 16S2 and 16S4 mutant alleles were associated with reduced fitness in E. coli.
FIG. 1.
Growth of E. coli strains expressing different 16S alleles. Strain JM109 and Δ7 prrn strain AVS69009 were transformed with pBR322 derivatives harboring the E. coli rrnC operon carrying either the wild-type or mutant allele. These strains were compared for growth on nutrient agar at 30°C, 37°C, and 41°C by using Dunnett's statistical tests. Growth is expressed as colony size index (average size obtained for a strain with the Spcr 16S alleles divided by the average size obtained with the same strain expressing the wild-type allele at the same temperature). *, P < 0.001 by Dunnett's multiple-comparison test; #, P < 0.05 by Dunnett's multiple-comparison test.
Fitness of C. psittaci 6BC carrying the Spcr 16S alleles.
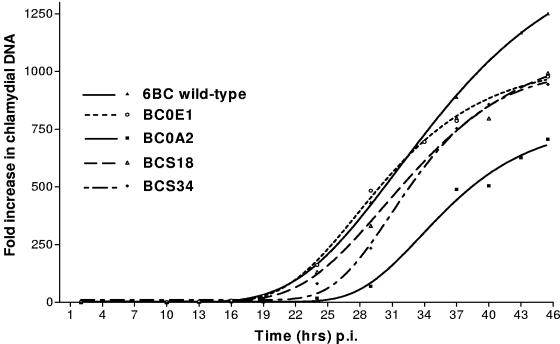
To be able to survive in a natural environment, a bacterium carrying the mutated allele must compete with the wild-type ancestor bacterial population. The outcome of the competition process depends on its relative fitness, defined as the efficiency of multiplication of the mutant cell compared with that of the wild-type ancestor strain (4). The growth of wild-type C. psittaci and the four Spcr variants, BC0E1, BC0A2, BCS18, and BCS34, was first monitored in the absence of SPC throughout one developmental cycle for 46 h by real-time PCR to determine the fold change in the amount of chlamydial DNA relative to that at a starting point of 2 h p.i. As seen in Fig. 2, all five C. psittaci 6BC strains displayed the expected sigmoid-shaped growth curves, but differences between the variants were noted. The initial lag phase of the growth curves, which corresponded to the transition phase between infectious EBs and replicating RBs, was delayed for each mutant, from about 3 h for the strains harboring the 16S1 or 16S2 alleles to more than 9 h for BC0A2 and BCS34 with the “chloroplastic” 16S2 and 16S4 alleles (Table 3). However, BCS34 growth was not as affected in the exponential phase of the curve in which the RBs both multiply by binary fission and convert to EBs. Consequently, the total DNA accumulation at the end of the cycle was in the same order for BCOE1, BCS18, and BCS34. BC0A2 DNA replication was so impaired during the entire developmental cycle that this strain accumulated less than half the amount of DNA seen for the parent strain (Fig. 2).
FIG. 2.
Relative accumulation of chlamydial DNA over time. The growth of C. psittaci 6BC carrying Spcr-associated mutations was measured as described in Materials and Methods.
TABLE 3.
Impact of mutations in the 16S rRNA gene on DNA accumulation and infectivity of C. psittaci 6BC during one developmental cycle in L2 cells
| Strain (allele) | Chlamydial DNAa
|
PFUb
|
||||
|---|---|---|---|---|---|---|
| Lag time (h) | Doubling time (h)c | Relative fitnessd | Eclipse time (h) | Time for twofold PFU increase rate (h)c | Relative fitnessd | |
| 6BC (wild type) | 6.8 | 1.77 ± 0.33 | 1 | 19 | 0.47 ± 0.03 | 1 |
| BC0E1 (16S1) | 10.1 | 1.77 ± 0.32 | 1 | 19 | 0.54 ± 0.003 | 0.87 |
| BC0A2 (16S2) | 18.3 | 2.75 ± 1.36 | 0.64 | 24 | 1 ± 0.12 | 0.47 |
| BCS18 (16S3) | 9.6 | 1.91 ± 0.57 | 0.93 | 19 | 0.51 ± 0.05 | 0.92 |
| BCS34 (16S4) | 16.1 | 2.02 ± 0.73 | 0.88 | 19-24e | 0.59 ± 0.02 | 0.79 |
Data were obtained from Fig. 1.
Data were obtained from Fig. .
The doubling time or the time required for a twofold PFU increase rate was estimated from a plot of ln (fold or PFU) = f (time), where the slope is ln 2/doubling time or twofold PFU increase rate (h). R2 was >0.99 for all curves. Data are means ± standard deviations.
The relative fitness is the ratio of the doubling time or the time required for a twofold PFU increase rate for the wild type to the doubling time or the time required for a twofold PFU increase rate for the mutant.
The lag phase lasted more than 19 h but less than 24 h.
The fitness of each mutant was calculated relative to that of the parent, for which a fitness value of 1 was assigned based on chlamydial DNA doubling time (Table 3). Interestingly, the doubling time of BC0E1 was similar to that of the wild-type strain, indicating that the C1192U mutation in the 16S rRNA was not associated with any strong growth defect in C. psittaci 6BC. Whereas the relative fitness values of BCS18 and BCS34 were about 0.90, the one for BC0A2 was 0.64, indicating that a physiological cost was associated with the A1191G mutation in the chlamydial 16S rRNA. This suggested that the chlamydial variants carrying the 16S1, 16S2, or 16S4 Spcr allele could compete more efficiently than BC0A2 (16S3) in a coinfection with the wild-type SPC-sensitive parent.
Pairwise competition between the C. psittaci 6BC wild type and the Spcr variants.
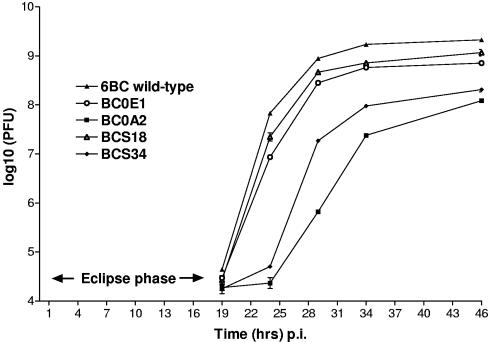
Wild-type C. psittaci 6BC and the BC0E1 variant were first coinfected at a 1:1 ratio in L2 monolayers in the absence of drug and then harvested from cells at 4 h p.i., 10 h p.i., and every 3 h afterwards up to 46 h p.i.; and titers were determined in the presence or absence of SPC by plaque assay (8). This assay uses the ability of the bacteria to lyse the host cells and form plaques resulting from the infection and spread of a single EB over several successive infection and development cycles. In some aspects, a chlamydial plaque can be seen to be similar to a bacterial colony on an agar plate in which each plaque or colony represents a clonal bacterial population that can be purified and expanded. The infectivity curve generated indicated that for up to 19 h p.i., the number of infectious particles decreased, representing the “eclipse” phase, in which infectious progeny EBs have differentiated into noninfectious RBs (data not shown). After this time, the number of infectious particles increased as RBs replicated and started differentiating back into EBs. Consequently, in subsequent competition assays the first sample was harvested at 19 h p.i. to limit our analyses to the exponential and stationary phases of the infectivity curve.
Figure 3 shows that, as seen with the lag phase on the DNA accumulation curve, the eclipse phase lasted longer for the two variants harboring the “chloroplastic” mutations, indicating a delay in the RB-to-EB transition. Yet, the twofold PFU increase rate during the exponential phase was severely affected only for BC0A2, for which it was two times slower, i.e., 1 h versus 32 min, 30 min, 35 min, and 28 min for BC0E1, BCS18, BCS34, and the wild-type strain, respectively (Table 3). Consequently, the relative fitness for BC0A2 (0.47) was also lower than those for BC0E1 (0.87), BCS18 (0.92), and BCS34 (0.79), thus following the same pattern as observed previously with the DNA accumulation curves.
FIG. 3.
Growth competition between C. psittaci 6BC wild type and the Spcr variants during one developmental cycle. Infectivity curves for the C. psittaci 6BC wild type and the BC0E1, BC0A2, BCS18, and BCS18 Spcr variants were generated by harvesting colonies at 19, 24, 29, 34, and 46 h p.i. Data are expressed as the mean ± standard deviation of duplicate determinations performed in two separate experiments.
Whereas the infectivity curves reached a plateau at 34 h p.i. for most strains, BC0A2 continued to generate EBs until late in the developmental cycle (Fig. 3). This is reflected in the competition index, defined as the ratio of the output mutant-to-wild type ratio to the input mutant-to-wild type ratio (Table 4). Whereas the wild-type strain produced as many as 1,000 times more EBs than BC0A2 at 24 and 29 h p.i., the difference was reduced to only 10-fold at 46 h p.i. However, the extended eclipse phase for both BC0A2 and BCS34 was followed by a decline in the total production of infectious particles; and although the competition index calculated during the developmental cycle for BCS34 did not fluctuate as much as that seen with the BC0A2 variant, both variants were clearly outcompeted by the wild-type strain, with final competition indices of 0.058 and 0.0096 for BCS34 after one and two developmental cycles, respectively, and competition indices of 0.067 and 0.0045 forBC0A2 after one and two developmental cycles, respectively. On the other hand, the mutations at position 1192 in the 16S rRNA were not associated with a strong growth defect in C. psittaci 6BC, as the final competition indices were 0.68 and 0.36 for BC0E1 at the end of the first and second rounds of competition with the parent strain, respectively, and 0.81 and 0.71 for BCS18 at the end of the first and second rounds of competition with the parent strain, respectively.
TABLE 4.
Growth competition between C. psittaci 6BC wild-type and Spcr variants
| Competitive strain | Input Spcr/wild type ratio | Competition index ata:
|
||||||
|---|---|---|---|---|---|---|---|---|
| 0 h | 19 h | 24 h | 29 h | 34 h | 46 h | 92 hb | ||
| BC0E1 | 0.52 | 1 | 0.96 | 0.25 | 0.73 | 0.59 | 0.68 | 0.36 |
| BC0A2 | 0.67 | 1 | 0.60 | 0.00052 | 0.00099 | 0.014 | 0.067 | 0.0045 |
| BCS18 | 0.65 | 1 | 0.89 | 0.51 | 0.83 | 0.83 | 0.81 | 0.71 |
| BCS34 | 2.08 | 1 | 0.29 | 0.29 | 0.011 | 0.036 | 0.058 | 0.0096 |
The competition index was defined as the ratio of the output mutant/wild type ratio at the indicated time p.i. to the input mutant/wild type ratio.
Determined after a second passage for another 46 h, as described in Materials and Methods.
Frequency of spontaneous mutations conferring tetracycline resistance in C. psittaci 6BC.
Chlamydial infections are often treated with tetracycline and its derivatives because these antibiotics are effective, are relatively inexpensive, and have low toxicities (37). Because mutations in the 16S rRNA have been associated with tetracycline resistance in H. pylori (12, 16, 45) as well as in cutaneous propionibacteria (38), we hypothesized that similar mutations could be selected in the unique ribosomal operon of C. psittaci 6BC. As expected, C. psittaci 6BC was very sensitive to the antibiotic, with an MIC of 40 ng/ml (Table 5). However no Tetr plaques were ever detected in the plaque assay. Therefore, the frequency of spontaneous Tetr mutation for this species was below the limit of detection, i.e., <3 × 10−9.
TABLE 5.
Effect of tetracycline on plaque formation by C. psittaci 6BC
| TET concn (ng/ml) | Input PFUa | No. of plaque |
|---|---|---|
| 20 | 137 | 77 |
| 40 | 1.3 × 105 | 0 |
| 50 | 1.4 × 107 | 0 |
| 5.8 × 107 | 0b | |
| 100 | 1.9 × 108 | 0 |
| 200 | 1.9 × 108 | 0 |
| 500 | 3 × 108 | 0 |
The largest inoculum size tested that was not cytotoxic.
Cell monolayer was unhealthy due to the large concentration of infectious particles.
DISCUSSION
At present, treatment failures following the appearance of mutations that confer antibiotic resistance have not been of great concern for chlamydial infections (43, 47). However, the acquisition of drug resistance in chlamydia by horizontal gene transfer has been suggested by the identification and characterization of a tetracycline-resistant strain of C. suis (13). In addition, studies in the laboratory have shown that mutations that result in the overexpression or alteration of the inhibitor target are associated with drug resistance in chlamydiae, similarly to other bacteria (43). Whether drug-resistant organisms persist in nature depends on their likely occurrence as well as their fitness relative to that of their drug-sensitive counterparts. We have recently shown that spontaneous mutations arise in vitro in C. psittaci 6BC and C. trachomatis L2 at frequencies similar to those in other eubacteria (8). Nevertheless, we still lack knowledge on the impact of drug-resistant mutations on the chlamydial life cycle. The objectives of the present work were to identify phenotypic changes that occur as a result of mutations in the 16S rRNA associated with Spcr in C.psittaci 6BC.
SPC resistance arose in C. psittaci 6BC from single mutations in the upper stem of the phylogenetically conserved helix 34 of 16S rRNA, mainly at position 1192 (by use of the E. coli numbering system), which has been directly implicated in the ability of the antibiotic to bind to the ribosome (8, 9). Surprisingly, alterations in the neighboring nucleotides at positions 1191 and 1193 conferred SPC resistance in C. psittaci 6BC, although similar mutations have been described previously only in Spcr chloroplasts. Introduction of the “chloroplastic” alleles in E. coli incurred a biological cost, as the recombinant bacteria formed small colonies on agar plates, possibly caused by a reduction in protein synthesis efficiency. Nevertheless, expression of the A1191G and G1193C mutations in E. coli gave rise to Spcr. This suggests that the small number of rRNA operons, i.e., one in C. psittaci and two in Chlamydomonas chloroplasts (30), rather than the proposed phylogenetic relationship between the two organisms (10) was responsible for the recovery of such mutants. In addition, expression of the SPC resistance phenotype in E. coli was codominant with the A1191G mutation, similarly to changes at position 1192, but recessive with the G1193C alteration. This explains why spectinomycin resistance due to the G-to-C mutation at position 1193 has been found only in C. psittaci so far. A similar recessivity of the phenotype has been reported for aminoglycoside resistance due to mutations in the 16S rRNA gene at position 1408 (36).
The definition of fitness includes a microorganism's ability to survive, reproduce, and be transmitted (3, 24). Chromosomal mutations that impair essential functions in bacterial physiology or that confer metabolic burdens often have deleterious effects on bacterial fitness, resulting in reduced growth, impaired virulence, and poor survival. However, one would predict that the obligate intracellular nature of an organism such as Chlamydia would impose greater restrictions on the type of mutations that can be recovered compared to those that can be recovered from free-living organisms, as isolation of chlamydial variants by plaque assay depends on both growth and cell-to-cell transmission (8). To test these predictions, we examined the growth characteristics of each chlamydial variant in pure culture and in competition with the parental SPC-sensitive strain. Because the development of chlamydiae alternates between a replicative but noninfectious form, the RBs, and the nonreplicative but infectious form, the EBs, growth curves were generated based on either the accumulation of bacterial DNA (RBs and EBs) or bacterial infectivity (EBs) over 46 h. It is worth noting that as the competition experiments were initiated at an MOI <1, each infectious particle should develop in a unique inclusion, in a unique cell. Consequently, the competing strains should not affect each other but compete only by their intrinsic growth rate and efficiency in utilizing the available nutrients.
As seen for other members of the family Chlamydiaceae, the life cycle of the C. psittaci 6BC wild-type strain was characterized by four major phases (49). The first 8 h correspond to the attachment, entry, and reorganization of EBs to RBs. Then, from 8 to 19 h p.i., RBs divide by binary fission, with a doubling every 1.8 h (Table 3). By comparison, C. trachomatis RBs divide every 2 to 3 h (41, 48), supporting our observations that C. psittaci 6BC plaques developed faster than C. trachomatis plaques. After 19 h p.i., the developmental cycle becomes asynchronous. RBs are still accumulating, but RB-to-EB conversion is observed until 34 h pi, when EB production reaches a plateau. The signals that trigger interconversion of the different chlamydial forms are unknown. Identification of temporally regulated genes and proteins suggests that the developmental cycle is regulated at the transcriptional level (6, 33, 41, 46).
Although mutations in rRNA primarily affect bacterial translational ability, indirect consequences on DNA replication can be expected. Three different growth patterns were observed among the chlamydial variants. (i) The development of both BC0E1 and BCS34, which carry a mutation at position 1192, was similar to that of the parental strain, except for an initial delay in DNA replication. (ii) The growth of BCS34, which harbored the C1193G alteration, showed an additional delay in the production of EB. (iii) The A1191G alteration in BC0A2 seriously slowed down the formation of both RBs and EBs throughout the entire developmental cycle, resulting in the production of 10 times fewer infectious particles at 46 h p.i. The 16S rRNA helix 34 appears to be involved in peptide chain termination and translation accuracy; and nucleotides at positions 1191, 1192, and 1193 interact directly with positions 1065, 1064, and 1063, respectively (9). Thus, it seems that mutations that disrupt the base pairing at position 1191 or 1193 have more severe consequences on the physiology of the bacteria, likely due to the destabilization of helix 34. This was reflected in the relative fitness and competition index, as the ranking of the strains was wild type > C1192G > C1192U > G1193C > A1191G. Interestingly, the biological costs imparted by expression of the various 16S alleles were alike in E. coli and C.psittaci, thus reflecting the similar role that nucleotides phylogenetically conserved in rRNAs play in bacterial physiology and in ribosomal function in particular.
Antibiotic-resistant mutants selected in vivo tend to be ones that display low or no fitness cost when assayed in vitro. For example, the high frequency of clinical isolates of Mycobacterium tuberculosis with the rifampin resistance-associated Ser531-to-Leu mutation in the β subunit of RNA polymerase is correlated with the low fitness cost conferred by the mutation to the bacterium, i.e., average competition index of 0.84 in vitro (7, 29). By contrast, the streptomycin resistance-associated G524C mutation in the 16S rRNA gene of mycobacteria is most frequently found in the laboratory but never in clinical isolates. This mutation results in a greater than 30% growth disadvantage per generation relative to that of the streptomycin-sensitive parental strain (40). We observed that both BCS34 and BC0A2 were severely outcompeted by the parental strain in the plaque assay, and we predict that they would not be maintained in vivo. On the other hand, BC0E1 and BCS18 were able to compete with the wild-type strain more efficiently and could likely persist longer than BCS34 and BC0A2 in the environment.
Tetracycline and its derivatives, such as doxycycline, have been some of the first drugs used for the treatment of chlamydial infections. Stable tetracycline resistance apparently acquired by horizontal gene transfer has been described only for C. suis, a pig pathogen (13). On the other hand, the tetracycline resistance reported for clinical isolates of C. trachomatis is unstable and has not been characterized at the molecular level (22, 23, 42). Tetracycline binds reversibly to the prokaryotic 30S ribosomal subunit similarly to spectinomycin. Given the conservation in structure and function of ribosomes, rRNA mutations that confer antibiotic resistance generally produce the same resistance phenotype in different bacterial species. Although C. psittaci 6BC Spcr variants arose at a frequency of 5 × 10−5 in vitro (8), the frequency of the spontaneous Tetr mutation for C. psittaci 6BC was below the limit of detection, i.e., <3 × 10−9. However, specific mutations in the 16S rRNA gene have been associated with Tetr. For example, a G-to-C mutation at E. coli equivalent base 1058 within helix 34 of the 16S rRNA has been associated with Tetr in clinical isolates of P. acnes, the causative agent of acne vulgaris. Expression of this mutation in E. coli JM109 confers a twofold increase in tetracycline resistance and is not associated with any strong growth defect (38). In clinical isolates of H. pylori, high-level tetracycline resistance has been attributed to the triple-base-pair substitution of AGA926-928 to TTC within both copies of the 16S rRNA gene, whereas low-level resistance is associated with single- and double-base-pair mutations in the exact same region (12, 16, 45). Interestingly, most eubacteria show the nucleotides TGC at the equivalent positions (positions 965 to 967 in E. coli numbering), suggesting that the G966-to-T single point mutation could confer high-level tetracycline resistance to these organisms. Our inability to isolate Tetr plaques for C.psittaci 6BC suggests either that the G1058C and G966T mutations do not confer resistance in chlamydiae or that they impose a significant burden on chlamydial fitness. Such species-specific bias for drug resistance mutations have been reported for other ribosome-targeting antibiotics, including linezolid (39) and macrolides (35).
In conclusion, the data presented in this study clearly demonstrate that Spcr-mediating mutations within the 16S rRNA cause a range of phenotypes that show from subtle to marked impairment of the biological fitness in C. psittaci 6BC and reveal distinct competitive growth disadvantages of the resistant strains compared to the growth of a clonally related susceptible strain in vitro. The fitness cost associated with resistance mutations could explain why drug resistance has not been a serious threat for the treatment of chlamydial infections so far. Nevertheless, partial azithromycin resistance resulting from alterations in the 23S rRNA has recently been reported for C. trachomatis clinical isolates. It appeared that the resistant populations were genetically heterogeneous and unstable, suggesting that the mutations incurred a strong fitness cost (32). However, the adverse effects of mutations can sometimes be reduced by the acquisition of second-site compensatory mutations (24, 27). Frequent intermittent antimicrobial treatments as a consequence of recurrent infections, repeated mass therapy currently in place to control trachoma in countries where it is endemic (31), and experimental long-term prophylactic treatment for coronary heart disease (2, 17) might select for compensatory mutations that adapt chlamydiae to the costs of chromosomal resistance. The fitness experiments reported here were performed with newly isolated organisms that had no opportunity for compensatory adaptation. We are currently investigating if mutations that ameliorate the fitness cost of the A1191G mutation can be selected in C. psittaci 6BC. This would provide additional information on the long-term stability of the resistance phenotype. Moreover, in the absence of a genetic system for chlamydiae, spontaneous antibiotic-resistant mutants presenting a high fitness cost might be our strongest candidates for a live attenuated vaccine at this time (25, 44).
Acknowledgments
This work was supported by grant AI44033 from the National Institute of Allergy and Infectious Diseases.
We thank M. O'Connor and C. L. Squires for providing E. coli strain AVS69009 along with some comments, T. Hatch for the gift of C.psittaci serovar 6BC, Nancy E. Adams for technical assistance, and Christina S. Clark for help with the statistical analysis. R.B. also gratefully acknowledges Sylvie Létoffé and Andrea J. McCoy for their stimulating comments.
REFERENCES
- 1.Adams, E. J., D. S. LaMontagne, A. R. Johnston, J. M. Pimenta, K. A. Fenton, and W. J. Edmunds. 2004. Modelling the healthcare costs of an opportunistic chlamydia screening programme. Sex. Transm. Infect. 80: 363-370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson, J. L. 2005. Infection, antibiotics, and atherothrombosis—end of the road or new beginnings? N. Engl. J. Med. 352:1706-1709. [DOI] [PubMed] [Google Scholar]
- 3.Andersson, D. I. 2003. Persistence of antibiotic resistant bacteria. Curr. Opin. Microbiol. 6:452-456. [DOI] [PubMed] [Google Scholar]
- 4.Andersson, D. I., and B. R. Levin. 1999. The biological cost of antibiotic resistance. Curr. Opin. Microbiol. 2:489-493. [DOI] [PubMed] [Google Scholar]
- 5.Asai, T., D. Zaporojets, C. Squires, and C. L. Squires. 1999. An Escherichia coli strain with all chromosomal rRNA operons inactivated: complete exchange of rRNA genes between bacteria. Proc. Natl. Acad. Sci. USA 96:1971-1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Belland, R. J., G. Zhong, D. D. Crane, D. Hogan, D. Sturdevant, J. Sharma, W. L. Beatty, and H. D. Caldwell. 2003. Genomic transcriptional profiling of the developmental cycle of Chlamydia trachomatis. Proc. Natl. Acad. Sci. USA 100:8478-8483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Billington, O. J., T. D. McHugh, and S. H. Gillespie. 1999. Physiological cost of rifampin resistance induced in vitro in Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 43:1866-1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Binet, R., and A. T. Maurelli. 2005. Frequency of spontaneous mutations that confer antibiotic resistance in Chlamydia spp. Antimicrob. Agents Chemother. 49:2865-2873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brink, M. F., G. Brink, M. P. Verbeet, and H. A. de Boer. 1994. Spectinomycin interacts specifically with the residues G1064 and C1192 in 16S rRNA, thereby potentially freezing this molecule into an inactive conformation. Nucleic Acids Res. 22:325-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brinkman, F. S., J. L. Blanchard, A. Cherkasov, Y. Av-Gay, R. C. Brunham, R. C. Fernandez, B. B. Finlay, S. P. Otto, B. F. Ouellette, P. J. Keeling, A. M. Rose, R. E. Hancock, S. J. Jones, and H. Greberg. 2002. Evidence that plant-like genes in Chlamydia species reflect an ancestral relationship between Chlamydiaceae, cyanobacteria, and the chloroplast. Genome Res. 12:1159-1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Corsaro, D., and D. Venditti. 2004. Emerging chlamydial infections. Crit. Rev. Microbiol. 30:75-106. [DOI] [PubMed] [Google Scholar]
- 12.Dailidiene, D., M. T. Bertoli, J. Miciuleviciene, A. K. Mukhopadhyay, G. Dailide, M. A. Pascasio, L. Kupcinskas, and D. E. Berg. 2002. Emergence of tetracycline resistance in Helicobacter pylori: multiple mutational changes in 16S ribosomal DNA and other genetic loci. Antimicrob. Agents Chemother. 46:3940-3946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dugan, J., D. D. Rockey, L. Jones, and A. A. Andersen. 2004. Tetracycline resistance in Chlamydia suis mediated by genomic islands inserted into the chlamydial inv-like gene. Antimicrob. Agents Chemother. 48:3989-3995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Flashner, Y., E. Mamroud, A. Tidhar, R. Ber, M. Aftalion, D. Gur, S. Lazar, A. Zvi, T. Bino, N. Ariel, B. Velan, A. Shafferman, and S. Cohen. 2004. Generation of Yersinia pestis attenuated strains by signature-tagged mutagenesis in search of novel vaccine candidates. Infect. Immun. 72:908-915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Frick, K. D., M. A. Colchero, and D. Dean. 2004. Modeling the economic net benefit of a potential vaccination program against ocular infection with Chlamydia trachomatis. Vaccine 22:689-696. [DOI] [PubMed] [Google Scholar]
- 16.Gerrits, M. M., M. Berning, A. H. van Vliet, E. J. Kuipers, and J. G. Kusters. 2003. Effects of 16S rRNA gene mutations on tetracycline resistance in Helicobacter pylori. Antimicrob. Agents Chemother. 47:2984-2986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grayston, J. T., R. A. Kronmal, L. A. Jackson, A. F. Parisi, J. B. Muhlestein, J. D. Cohen, W. J. Rogers, J. R. Crouse, S. L. Borrowdale, E. Schron, and C. Knirsch. 2005. Azithromycin for the secondary prevention of coronary events. N. Engl. J. Med. 352:1637-1645. [DOI] [PubMed] [Google Scholar]
- 18.Guzman, L. M., D. Belin, M. J. Carson, and J. Beckwith. 1995. Tight regulation, modulation, and high-level expression by vectors containing the arabinose PBAD promoter. J. Bacteriol. 177:4121-4130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hammerschlag, M. R. 2002. The intracellular life of chlamydiae. Semin. Pediatr. Infect. Dis. 13:239-248. [DOI] [PubMed] [Google Scholar]
- 20.Hanahan, D. 1983. Studies on transformation of Escherichia coli with plasmids. J. Mol. Biol. 166:557-580. [DOI] [PubMed] [Google Scholar]
- 21.Hogan, R. J., S. A. Mathews, S. Mukhopadhyay, J. T. Summersgill, and P. Timms. 2004. Chlamydial persistence: beyond the biphasic paradigm. Infect. Immun. 72:1843-1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jones, R. B., B. Van der Pol, D. H. Martin, and M. K. Shepard. 1990. Partial characterization of Chlamydia trachomatis isolates resistant to multiple antibiotics. J. Infect. Dis. 162:1309-1315. [DOI] [PubMed] [Google Scholar]
- 23.Lefevre, J. C., J. P. Lepargneur, D. Guion, and S. Bei. 1997. Tetracycline-resistant Chlamydia trachomatis in Toulouse, France. Pathol. Biol. (Paris) 45:376-378. [PubMed] [Google Scholar]
- 24.Lenski, R. E. 1998. Bacterial evolution and the cost of antibiotic resistance. Int. Microbiol. 1:265-270. [PubMed] [Google Scholar]
- 25.Linde, K., G. C. Fthenakis, and A. Fichtner. 1998. Bacterial live vaccines with graded level of attenuation achieved by antibiotic resistance mutations: transduction experiments on the functional unit of resistance, attenuation and further accompanying markers. Vet. Microbiol. 62:121-134. [DOI] [PubMed] [Google Scholar]
- 26.Macvanin, M., J. Bjorkman, S. Eriksson, M. Rhen, D. I. Andersson, and D. Hughes. 2003. Fusidic acid-resistant mutants of Salmonella enterica serovar Typhimurium with low fitness in vivo are defective in RpoS induction. Antimicrob. Agents Chemother. 47:3743-3749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maisnier-Patin, S., and D. I. Andersson. 2004. Adaptation to the deleterious effects of antimicrobial drug resistance mutations by compensatory evolution. Res. Microbiol. 155:360-369. [DOI] [PubMed] [Google Scholar]
- 28.Makosky, P. C., and A. E. Dahlberg. 1987. Spectinomycin resistance at site 1192 in 16S ribosomal RNA of E. coli: an analysis of three mutants. Biochimie 69:885-889. [DOI] [PubMed] [Google Scholar]
- 29.Mariam, D. H., Y. Mengistu, S. E. Hoffner, and D. I. Andersson. 2004. Effect of rpoB mutations conferring rifampin resistance on fitness of Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 48:1289-1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maul, J. E., J. W. Lilly, L. Cui, C. W. dePamphilis, W. Miller, E. H. Harris, and D. B. Stern. 2002. The Chlamydomonas reinhardtii plastid chromosome: islands of genes in a sea of repeats. Plant Cell 14:2659-2679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Melese, M., J. D. Chidambaram, W. Alemayehu, D. C. Lee, E. H. Yi, V. Cevallos, Z. Zhou, C. Donnellan, M. Saidel, J. P. Whitcher, B. D. Gaynor, and T. M. Lietman. 2004. Feasibility of eliminating ocular Chlamydia trachomatis with repeat mass antibiotic treatments. JAMA 292:721-725. [DOI] [PubMed] [Google Scholar]
- 32.Misyurina, O. Y., E. V. Chipitsyna, Y. P. Finashutina, V. N. Lazarev, T. A. Akopian, A. M. Savicheva, and V. M. Govorun. 2004. Mutations in a 23S rRNA gene of Chlamydia trachomatis associated with resistance to macrolides. Antimicrob. Agents Chemother. 48:1347-1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nicholson, T. L., L. Olinger, K. Chong, G. Schoolnik, and R. S. Stephens. 2003. Global stage-specific gene regulation during the developmental cycle of Chlamydia trachomatis. J. Bacteriol. 185:3179-3189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O'Connor, M., and A. E. Dahlberg. 2002. Isolation of spectinomycin resistance mutations in the 16S rRNA of Salmonella enterica serovar Typhimurium and expression in Escherichia coli and Salmonella. Curr. Microbiol. 45:429-433. [DOI] [PubMed] [Google Scholar]
- 35.Pfister, P., N. Corti, S. Hobbie, C. Bruell, R. Zarivach, A. Yonath, and E. C. Bottger. 2005. 23S rRNA base pair 2057-2611 determines ketolide susceptibility and fitness cost of the macrolide resistance mutation 2058A→G. Proc. Natl. Acad. Sci. USA 102:5180-5185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Prammananan, T., P. Sander, B. Springer, and E. C. Bottger. 1999. RecA-mediated gene conversion and aminoglycoside resistance in strains heterozygous for rRNA. Antimicrob. Agents Chemother. 43:447-453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roberts, M. C. 2003. Tetracycline therapy: update. Clin. Infect. Dis. 36: 462-467. [DOI] [PubMed] [Google Scholar]
- 38.Ross, J. I., E. A. Eady, J. H. Cove, and W. J. Cunliffe. 1998. 16S rRNA mutation associated with tetracycline resistance in a gram-positive bacterium. Antimicrob. Agents Chemother. 42:1702-1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sander, P., L. Belova, Y. G. Kidan, P. Pfister, A. S. Mankin, and E. C. Bottger. 2002. Ribosomal and non-ribosomal resistance to oxazolidinones: species-specific idiosyncrasy of ribosomal alterations. Mol. Microbiol. 46:1295-1304. [DOI] [PubMed] [Google Scholar]
- 40.Sander, P., B. Springer, T. Prammananan, A. Sturmfels, M. Kappler, M. Pletschette, and E. C. Bottger. 2002. Fitness cost of chromosomal drug resistance-conferring mutations. Antimicrob. Agents Chemother. 46: 1204-1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shaw, E. I., C. A. Dooley, E. R. Fischer, M. A. Scidmore, K. A. Fields, and T. Hackstadt. 2000. Three temporal classes of gene expression during the Chlamydia trachomatis developmental cycle. Mol. Microbiol. 37:913-925. [DOI] [PubMed] [Google Scholar]
- 42.Somani, J., V. B. Bhullar, K. A. Workowski, C. E. Farshy, and C. M. Black. 2000. Multiple drug-resistant Chlamydia trachomatis associated with clinical treatment failure. J. Infect. Dis. 181:1421-1427. [DOI] [PubMed] [Google Scholar]
- 43.Stamm, W. E. 2000. Potential for antimicrobial resistance in Chlamydia pneumoniae. J. Infect. Dis. 181(Suppl. 3):S456-S459. [DOI] [PubMed] [Google Scholar]
- 44.Su, H., R. Messer, W. Whitmire, S. Hughes, and H. D. Caldwell. 2000. Subclinical chlamydial infection of the female mouse genital tract generates a potent protective immune response: implications for development of live attenuated chlamydial vaccine strains. Infect. Immun. 68:192-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Trieber, C. A., and D. E. Taylor. 2002. Mutations in the 16S rRNA genes of Helicobacter pylori mediate resistance to tetracycline. J. Bacteriol. 184:2131-2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vandahl, B. B., S. Birkelund, and G. Christiansen. 2004. Genome and proteome analysis of Chlamydia. Proteomics 4:2831-2842. [DOI] [PubMed] [Google Scholar]
- 47.Wang, S. A., J. R. Papp, W. E. Stamm, R. W. Peeling, D. H. Martin, and K. K. Holmes. 2005. Evaluation of antimicrobial resistance and treatment failures for Chlamydia trachomatis: a meeting report. J. Infect. Dis. 191: 917-923. [DOI] [PubMed] [Google Scholar]
- 48.Wilson, D. P., S. Mathews, C. Wan, A. N. Pettitt, and D. L. McElwain. 2004. Use of a quantitative gene expression assay based on micro-array techniques and a mathematical model for the investigation of chlamydial generation time. Bull. Math. Biol. 66:523-537. [DOI] [PubMed] [Google Scholar]
- 49.Wyrick, P. B. 2000. Intracellular survival by Chlamydia. Cell Microbiol. 2:275-282. [DOI] [PubMed] [Google Scholar]
- 50.Yanisch-Perron, C., J. Vieira, and J. Messing. 1985. Improved M13 phage cloning vectors and host strains: nucleotide sequences of the M13mp18 and pUC19 vectors. Gene 33:103-119. [DOI] [PubMed] [Google Scholar]