Abstract
Recently, attention has focused on whether particulate air pollution is a specific trigger of myocardial infarction (MI). The results of several studies of single locations assessing the effects of ambient particular matter on the risk of MI have been disparate. We used a multicity case-crossover study to examine risk of emergency hospitalization associated with fine particulate matter (PM) with aerodynamic diameter < 10 μm (PM10) for > 300,000 MIs during 1985–1999 among elderly residents of 21 U.S. cities. We used time-stratified controls matched on day of the week or on temperature to detect possible residual confounding by weather. Overall, we found a 0.65% [95% confidence interval (CI), 0.3–1.0%] increased risk of hospitalization for MI per 10 μg/m3 increase in ambient PM10 concentration. Matching on apparent temperature yielded a 0.64% increase in risk (95% CI, 0.1–1.2%). We found that the effect size for PM10 doubled for subjects with a previous admission for chronic obstructive pulmonary disease or a secondary diagnosis of pneumonia, although these differences did not achieve statistical significance. There was a weaker indication of a larger effect on males but no evidence of effect modification by age or the other diagnoses. We also found that the shape of the exposure–response relationship between MI hospitalizations and PM10 is almost linear, but with a steeper slope at levels of PM10 < 50 μg/m3. We conclude that increased concentrations of ambient PM10 are associated with increased risk of MI among the elderly.
Keywords: air pollution, cardiovascular diseases, case-crossover, myocardial infarction, particulate matter
Ambient particulate matter (PM) air pollution has been repeatedly observed to be associated with increased risk of hospital admissions and deaths attributed to cardiovascular causes in studies conducted throughout the industrialized world (Anderson et al. 2003; Braga et al. 2001; Dockery 2001; Hoek et al. 2001; Katsouyanni et al. 1996; Pope et al. 2004a; Samet et al. 2000; Zanobetti et al. 2000a).
Similar relationships have been reported in locations reflecting a wide range of PM and of gaseous copollutant concentrations (Goldberg et al. 2001; Koken et al. 2003; Linn et al. 2000; Sunyer et al. 2003; Zmirou et al. 1998). Other studies have shown that these associations are not confounded by secular time trends, seasonal patterns, influenza epidemics (Braga et al. 2000), or weather (Samet et al. 1998; Schwartz 1999, 2000). In addition, a large study of essentially every U.S. city reported that airborne particles were the only air pollutant that showed an independent effect on daily deaths, and that those gaseous air pollutants did not confound the association between PM and daily deaths (Samet et al. 2000).
Although the association of airborne particles with cardiovascular events is clear, the mechanisms behind these associations are not fully understood. To further understanding of the mechanisms behind these observations, it is important to examine associations with more specific end points that may suggest specific pathways.
Recently, attention has focused on whether PM air pollution is a specific trigger of myocardial infarction (MI) [International Classification of Diseases, Revision 9 (ICD-9), code 410 (World Health Organization 1977)]. Peters et al. (2001a) conducted a case-crossover study of 772 patients presenting to Boston area hospitals with strictly defined MI and reported that elevated concentrations of ambient PM [fine PM with aerodynamic diameter < 2.5 μm (PM2.5) and < 10 μm (PM10)] were strongly associated with higher risks of MI onset in the 2-hr period, and in the 24-hr period, preceding the event.
D’Ippoliti et al. (2003) analyzed hospital admissions for MI in Rome with a case-crossover analysis and found a strong association with total suspended PM. In contrast, Sullivan et al. (2003) observed a slight effect of fine PM on onset of MI, but no association was found when stratified by those with and without heart disease. Mann et al. (2002) conducted a Poisson regression analysis of 19,460 hospital admissions for acute MI in southern California but did not observe an effect of PM10, although exposure measurements were recorded only every 6th day. Braga et al. (2001) conducted a multicity Poisson regression analysis and concluded that increased PM10 concentration increased the risk of death from MI.
To understand these disparate findings in isolated cities, a systematic approach is necessary. A systematic examination of the lag structure of the association is also needed. We therefore conducted a multicity case-crossover study of the acute effect of PM10 on the increased risk of being admitted to the hospital for MI among the elderly in 21 U.S. cities and whether that risk was modified by medical or demographic factors.
Materials and Methods
Health data.
The data on hospital admissions were extracted from the Health Care Financing Administration (Medicare; Baltimore, MD) billing records, which we obtained for the years 1985–1999. The Medicare system provides hospital coverage for all U.S. citizens ≥ 65 years of age.
We analyzed data on persons who were admitted to the hospital with a primary diagnosis of MI (ICD-9 code 410) between 1986 and 1999. Medicare data provided personal characteristics such as age, sex, and race and the type of admission. Using this information, we selected only emergency admissions to ensure that these were new events and to better ascertain the timing of the event relative to air pollution exposure.
Using a unique identifier for each subject, we traced them through Medicare records to assess whether they had any primary or secondary diagnosis of atrial fibrillation (ICD-9 code 427.3), chronic obstructive pulmonary disease (COPD; ICD-9 code 490–496, except 493), diabetes (ICD-9 code 250), congestive heart failure (CHF; ICD-9 code 428) on previous admissions, and pneumonia (ICD-9 code 480–487) as secondary diagnoses on the index admission. These characteristics were examined as effect modifiers. These diagnoses have previously been suggested as modifiers of the cardiovascular effects of particles (Sunyer et al. 2000; Zanobetti et al. 2000b). Previous admissions were traced back to 1985, ensuring at least 1 year of data before the start of the particle data.
Daily monitoring of PM10 is not done in all U.S. cities. We selected the following 21 cities with daily monitoring of PM and representing a geographic distribution across the country: Birmingham, Alabama; Boulder, Colorado; Canton, Ohio; Chicago, Illinois; Cincinnati, Ohio; Cleveland, Ohio; Colorado Springs, Colorado; Columbus, Ohio; Denver, Colorado; Detroit, Michigan; Honolulu, Hawaii; Houston, Texas; Minneapolis–St. Paul, Minnesota; Nashville, Tennessee; New Haven, Connecticut; Pittsburgh, Pennsylvania; Provo-Orem, Utah; Salt Lake City, Utah; Seattle, Washington; Steubenville, Ohio; and Youngstown, Ohio.
For most cities, the metropolitan county encompassed the city and much of its suburbs, but we used multiple counties for Minneapolis-St. Paul (Ramsey and Hennepin, MN), Birmingham (Blount, Jefferson, St. Clair, Shelby, and Walker, AL), Steubenville (Jefferson, OH, and Brooke and Hancock, WV), and Youngstown (Columbiana and Mahoning, OH).
Environmental data.
We obtained PM10 data from the U.S. Environmental Protection Agency’s Aerometric Information Retrieval System (Nehls 1973). Many of the cities have more than one monitoring location, requiring a method to average over multiple locations. We computed local daily mean PM10 concentrations using an algorithm that accounts for the different monitor-specific means and variances (Zanobetti et al. 2000a). Not all cities have daily PM10 for the full range of years from 1986 to 1999; therefore, each city was analyzed for those years when daily PM10 was available.
These PM10 series had some occasional missing observations, and we replaced the missing values with the predicted values from a regression where we controlled for season and long-term trend, weather variables, and extinction coefficient, which has been shown to be a good predictor of fine particle concentrations (Ozkaynak et al. 1985). The average percentage of observations replaced was 8.4%. We obtained local meteorologic data from the U.S. Surface Airways and Airways Solar Radiation hourly data (National Environmental Satellite Data and Information Service 2003).
Analytical strategy.
We investigated the association between daily PM10 concentrations and hospital admissions for MI using a case-crossover design. The case-crossover design was developed as a variant of the case–control design to study the effects of transient exposures on acute events (Maclure 1991). This design samples only cases and compares each subject’s exposure experience in a time period just before a case-defining event with that subject’s exposure at other times. Because there is perfect matching on all measured or unmeasured subject characteristics that do not vary over time, there can be no confounding by those characteristics. If, in addition, the control days are chosen to be close to the event day, slowly varying subject characteristics are also controlled by matching.
Bateson and Schwartz (1999, 2001) demonstrated that by choosing control days close to event days, even very strong confounding of exposure by seasonal patterns could be controlled by design in the case–control approach. This makes the approach an attractive alternative to the Poisson models. Levy et al. (2001) showed that a time-stratified approach to choosing controls, such as sampling control days from the same month of the same year, avoided some subtle selection bias issues and resulted in a proper conditional logistic likelihood. Schwartz et al. (2003) recently demonstrated with simulation studies that this approach gave unbiased effect sizes and coverage probabilities even with strong seasonal confounding. We used this same stratified approach in our analysis. Matching on day of the week as well as season also controls for the possibility that the day of the week effect varies seasonally.
We defined the hazard period—when a person is at risk for the triggering of an acute MI—as the day of the patient’s hospitalization. Air pollution has short-term serial correlation; to ensure that all of our control days were independent, we chose control days matched on day of the week, in the same month and year as the event day. The data were analyzed using a conditional logistic regression (PROC PHREG, release 8.2; SAS Institute, Cary, NC).
The analysis was conducted for each city separately, and we controlled for day of the week and weather. To control for potential impacts of weather, we used apparent temperature (AT) for the same and previous day, defined as an individual’s perceived air temperature given the humidity. AT was calculated with the following formula (Kalkstein and Valimont 1986; Steadman 1979):
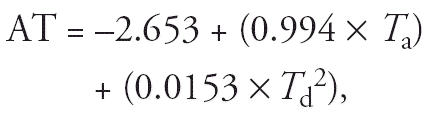 |
where Ta is air temperature and Td is dew point temperature.
Because risk may vary nonlinearly with AT, we used a regression spline (with 3 df) for both the same day and the previous day. PM10 was modeled linearly. To confirm the report of Braga et al. (2001) that the association was predominant with PM10 on the day of the event, we examined effects at exposure from lag day 0 to lag day 2. If we could confirm a primary association with lag day 0, we used this for the subsequent analysis described below.
As a sensitivity analysis, we tested an alternate referent selection scheme that matched on AT (rounded to the same degrees Celsius) and used indicator variables to control for day of the week. Because matching on two covariates controls for interactions between the covariates, this controls for the possibility that the temperature effects vary by month. It also renders moot any question of whether the nonlinear dependence of MIs with temperature was modeled correctly. Previous day’s temperature was controlled using a cubic spline in this analysis, as well.
Case-crossover analyses lend themselves to the analysis of effect modification. Factors such as sex are controlled by matching in the design of the study, but we can still test for effect modification with interaction terms or a stratified analysis. We chose stratified analyses, because if a characteristic modifies the effect of PM10, it might also modify the effect of weather or other covariates. A stratified analysis controls for this. Specifically, we conducted stratified analyses by sex, age (< 75 vs. ≥ 75), and previous admission for chronic disease such as atrial fibrillation, COPD, CHF, and diabetes, and secondary diagnosis for pneumonia as an acute modifier.
In a second stage of the analysis, the city-specific results were combined using the multivariate meta-regression technique of Berkey et al. (1998). To be conservative, we report the results incorporating a random effect, whether or not there was a significant heterogeneity.
Finally, we assessed the shape of the dose–response relationship by fitting a piecewise linear spline, with slope changes at 20 μg/m3 and 50 μg/m3. We combined these estimates using a random effect meta-analysis as well.
Results
There were 302,453 hospital admissions for MI in the 21 cities during the study period. Table 1 shows the counts for all of the cities broken into categories by age group, sex, and previous and secondary diagnosis. Table 2 shows the distribution of environmental factors by city, including the study period, the total population, PM, AT, and the counts of hospital admissions for MI. The average PM10 across all cities was 27 μg/m3.
Table 1.
Counts of hospital admissions for MI in total and by age group, sex, secondary diagnoses, and previous admissions among residents of 21 U.S. cities.
| Variable | No. of events (%) |
|---|---|
| MI | 302,453 |
| Age (years) | |
| 65–75 | 145,983 (48) |
| > 75 | 156,470 (52) |
| Sex | |
| Male | 147,246 (49) |
| Female | 155,207 (51) |
| Secondary diagnosis | |
| Pneumonia | 13,588 (4) |
| Previous admissions | |
| COPD | 32,455 (11) |
| Atrial fibrillation | 28,912 (10) |
| Diabetes | 49,732 (16) |
Table 2.
Counts of hospital admissions for MI and distribution of environmental factors.
| AT
|
PM10 |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| City | Years of study | MI events | Population (× 1,000) | 10% | 50% | 90% | 10% | 50% | 90% |
| Birmingham, AL | 1986–1993 | 14,457 | 662 | 2.9 | 17.2 | 30.5 | 13.7 | 32.3 | 63.2 |
| Boulder, CO | 1989–1996 | 1,347 | 291 | −4.3 | 8.0 | 20.9 | 10.2 | 20.3 | 37.9 |
| Canton, OH | 1989–1996 | 7,158 | 378 | −5.1 | 8.2 | 24.6 | 14.8 | 24.3 | 43.5 |
| Chicago, IL | 1986–1999 | 67,974 | 5,377 | −5.0 | 8.3 | 26.0 | 16.8 | 32.1 | 57.6 |
| Cincinnati, OH | 1989–1998 | 13,025 | 845 | −3.1 | 10.9 | 27.1 | 16.3 | 28.5 | 52.5 |
| Cleveland, OH | 1989–1999 | 27,218 | 1,394 | −4.2 | 9.1 | 25.4 | 17.0 | 34.1 | 63.4 |
| Colorado Springs, CO | 1987–1996 | 2,398 | 517 | −4.3 | 7.1 | 19.4 | 12.4 | 21.7 | 40.1 |
| Columbus, OH | 1991–1994 | 12,451 | 1,069 | −3.1 | 10.7 | 26.7 | 15.4 | 25.7 | 46.5 |
| Denver, CO | 1986–1999 | 4,755 | 555 | −4.1 | 7.6 | 21.5 | 16.7 | 28.5 | 49.2 |
| Detroit, MI | 1986–1999 | 30,793 | 2,061 | −4.8 | 8.3 | 25.4 | 13.1 | 30.5 | 59.8 |
| Honolulu, HI | 1998–1999 | 6,540 | 876 | 23.7 | 26.8 | 29.6 | 11.1 | 15.5 | 22.7 |
| Houston, TX | 1986–1987 | 15,085 | 3,401 | 7.8 | 23.2 | 34.3 | 15.9 | 29.7 | 50.0 |
| Minneapolis, MN | 1986–1999 | 14,356 | 1,627 | −8.5 | 6.4 | 24.1 | 12.0 | 23.5 | 44.4 |
| Nashville, TN | 1990–1999 | 4,740 | 570 | 0.7 | 15.3 | 30.1 | 15.7 | 28.1 | 46.5 |
| New Haven, CT | 1988–1999 | 12,807 | 824 | −3.6 | 8.6 | 25.1 | 9.9 | 22.7 | 44.8 |
| Pittsburgh, PA | 1987–1998 | 34,439 | 1,282 | −3.6 | 9.6 | 25.3 | 11.6 | 26.0 | 60.0 |
| Provo/Orem, UT | 1986–1999 | 815 | 369 | −4.1 | 7.6 | 23.9 | 14.5 | 30.5 | 66.9 |
| Salt Lake City, UT | 1986–1999 | 3,694 | 898 | −4.3 | 7.6 | 24.1 | 13.9 | 30.7 | 61.2 |
| Seattle, WA | 1986–1997 | 12,437 | 1,737 | 1.9 | 9.2 | 18.1 | 12.4 | 24.5 | 50.5 |
| Steubenville, OH | 1988–1998 | 4,185 | 132 | −3.6 | 9.5 | 25.2 | 15.4 | 30.0 | 59.7 |
| Youngstown, OH | 1989–1995 | 9,493 | 370 | −5.2 | 7.9 | 23.9 | 15.4 | 27.9 | 50.7 |
| Total | 300,167 | 25,340 | −1.70 | 11.36 | 26.55 | 14.70 | 28.35 | 53.55 | |
We first looked at the lag structure of the association between PM10 and the risk of hospitalization for MI by simultaneously estimating the effect of PM10 from lag days 0 to 2. The combined estimates of percent change in risk [and 95% confidence interval (CI)] of emergency hospitalization for MI are shown in Figure 1 together with the estimate of lag day 0 alone. The PM10 effect is mainly associated with the change in risk on the day of hospitalization; therefore, the rest of the analysis was done for lag day 0. Figure 1 also shows the percent change of the combined estimates for PM10 at lag day 0 from the sensitivity analysis, where the control periods were chosen using the same time-stratified approach but such that exposures on the case day were compared with exposures occurring on days of the same month with the same value of AT (TEMP) as the case day.
Figure 1.
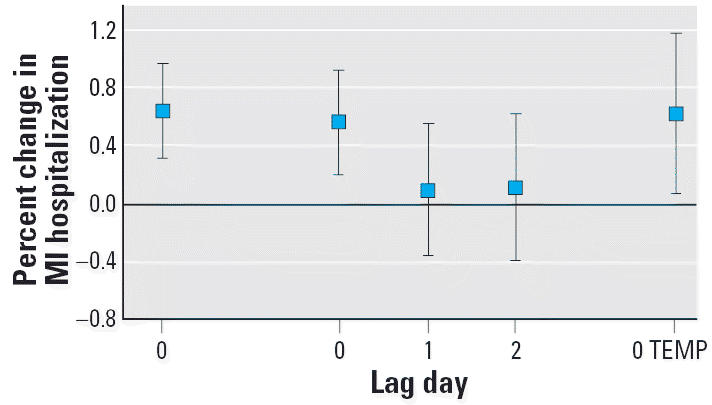
Combined random-effect estimated change in risk (and 95% CI) of hospitalization for MI associated with a 10 μg/m3 increase in daily PM10 on the same day and for lag days 0–2. Results are shown for our main model and (only for lag day 0) for the referent selection scheme that matched on AT (TEMP).
The results shown in Figure 1 using the two different referent selection schemes are consistent and show a very similar estimated effect. Overall, we found that for each 10 μg/m3 increase in the concentration of PM10, there was a 0.65% (95% CI, 0.3–1%) increase in the risk of hospitalization for an MI among the study population. When matching by AT (TEMP in Figure 1), we found a 0.64% (95% CI, 0.1–1.2%) increase. There was no evidence that the variation in effects size estimates by city was greater than would be expected giving their standard errors, with a chi-square value for heterogeneity of 17.8 (21 df, p = 0.6).
Figure 2 shows the results of the stratified analysis to examine effect modification by age group, sex, and previous admissions for atrial fibrillation, COPD, CHF, and diabetes and secondary diagnosis for pneumonia. We did not find a statistically significant modification of effect, but we found that acute or chronic lower respiratory disease had important effects on response to PM10. In subjects with a previous admission for COPD, we found a 1.3% change (95% CI, −0.1 to 2.8) for a 10 μg/m3 increase in PM10 in the risk of hospitalization for MI, whereas the risk was halved in subjects without a previous admission for COPD (0.6%, 95% CI, 0.3–1). In subjects with a secondary diagnosis of pneumonia, we found a 1.4% change (95% CI, −0.8 to 3.6) in the risk of hospitalization for MI, compared with a 0.6% change (95% CI, 0.3–1) in subjects without a secondary diagnosis of pneumonia. No significant heterogeneity was found when combining the stratified results.
Figure 2.
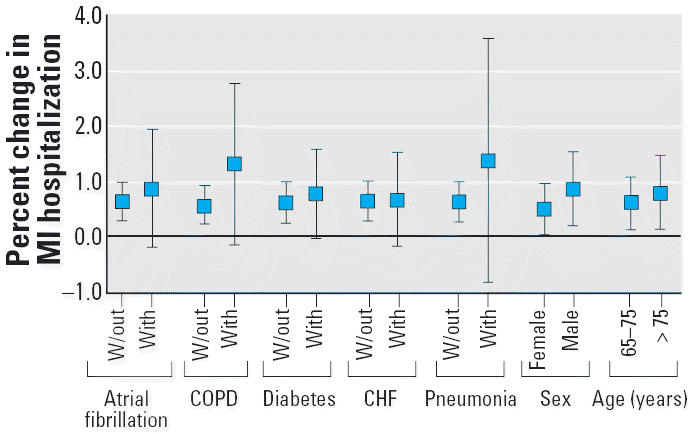
Stratified analysis for several effect modifiers: combined random-effect estimated change in risk (and 95% CI) of hospitalization for MI associated with a 10 μg/m3 increase in daily PM10 on the same day. W/out, without.
None of the other effect modifiers we examined (age, sex, CHF, atrial fibrillation, diabetes) showed much evidence for effect modification except perhaps for sex, with a suggestive difference for males (0.9%; 95% CI, 0.2–1.6) versus females (0.5%; 95% CI, 0.05–1.97).
Finally, the shape of the exposure–response relationship between MI hospitalizations and PM10 is shown in Figure 3. The exposure response is almost linear, but with a steeper slope at levels of PM10 < 50 μg/m3.
Figure 3.
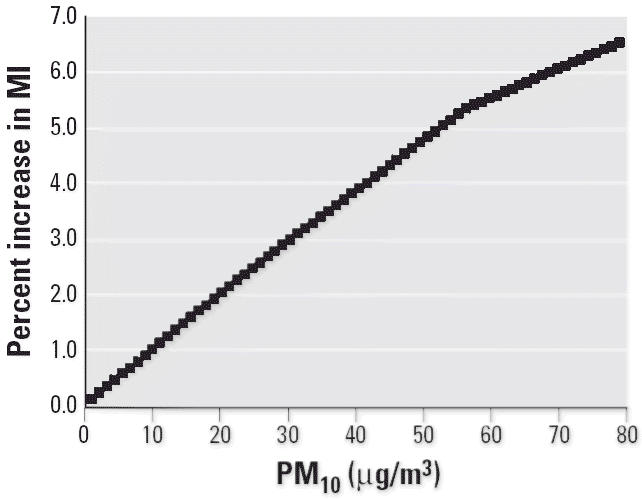
Combined random-effect estimated of the dose–response relationship between MI emergency hospital admissions and PM10, computed by fitting a piecewise linear spline, with slope changes at 20 μg/m3 and 50 μg/m3.
Discussion
We found a significant association between airborne particles and the risk of emergency MI hospitalization in a large multicity study. This association was only with PM10 on the same day, suggesting that airborne particles are acting as a trigger of an MI. We did not find evidence of effect modification by age, and weak evidence by sex, but we found a doubled risk in subjects with a secondary diagnosis of pneumonia or a previous admission for COPD. Diabetes, CHF, and atrial fibrillation did not modify the risk. These results greatly expand the number of locations in which an association between PM10 and MIs has been investigated and, by using a uniform analytical strategy, provide a clearer indication of the lag between exposure and response.
The estimated effect for a 10 μg/m3 increase in PM10 on emergency MI admissions (0.65%; 95% CI, 0.3–1.0) was higher than the estimates recently published for all-cause mortality (Schwartz et al. 2003). This suggests that MI is a more specific outcome, and the lag structure found indicates a rapid pathway. In the same article (Schwartz et al. 2003), we also showed that the effects of PM10 on hospital admissions for all other cardiovascular causes are not greatly different from the effects on MI admissions.
Recent studies of intermediate markers also provide support for a causal association. These include an observation of increased plasma viscosity (Peters et al. 1997) and increased plasma fibrinogen in a human exposure chamber study (Ghio et al. 2000). Results for C-reactive protein concentrations have been mixed (Brook et al. 2003; Donaldson et al. 2001; Peters et al. 2001b; Pope et al. 2004b), but PM exposure was associated with decreased plaque stability in an animal model for arteriosclerosis (Suwa et al. 2002). In a Los Angeles panel study in patients with COPD (Linn et al. 1999) and in a large cross-sectional German study of older adults (Ibald-Mulli et al. 2001), higher levels of air pollution were associated with higher blood pressure. Another study in Boston (Zanobetti et al. 2004) suggested that changes in PM2.5 led to within-person increases in resting and exercise blood pressure among vulnerable patients with cardiovascular disease. These studies provide a limited but growing understanding of mechanisms underlying these findings, suggesting that pollution may lead to acute or chronic vasoconstriction and/or atherosclerosis, perhaps due to systemic inflammation, changes in autonomic function, or oxidative stress.
Our finding that secondary diagnosis of pneumonia or a previous admission for COPD appears to increase the risk is consistent with previous findings. For example, cardiovascular deaths on high-pollution days have been reported to be three times as likely to include respiratory complications (Schwartz 1994b). In a study using Poisson models, we found that a secondary diagnosis for acute respiratory infection, acute bronchitis, pneumonia, and COPD modified the risk of any admission for heart disease (Zanobetti et al. 2000b). D’Ippoliti et al. (2003) also analyzed several comorbidities, and they did not find effect modification. Their study showed some indication of a higher effect for conduction disorders, a slightly higher effect in females, and a higher effect with increasing age group.
Previous studies have reported PM10 (Atkinson et al. 2001; Oftedal et al. 2003; Zanobetti et al. 2000a) effects on respiratory admissions. However, the small percentage increase in pneumonia associated with a 10 μg/m3 increase in PM10 cannot explain the doubling of the effect of PM10 on MI admissions. Persons with COPD often have underlying coronary artery disease through their joint association with smoking, and this may explain some or all of the observed effect modification. We also did not find effect modification by sex and age, even if we found a slightly higher effect in males. The weak evidence for effect modification by age groups indicates that the adverse effect of particles is not limited to the extremely elderly population.
The indication of a somewhat higher slope at PM10 concentrations < 50 μg/m3 is consistent with a previous report for all-cause mortality (Schwartz 2000). Other studies have assessed exposure response for particle using nonparametric smoothing (Schwartz 1994a; Schwartz and Zanobetti 2000) or natural spline (Daniels et al. 2000) and similarly found little evidence for a threshold and more support for steeper slopes at low concentrations.
There is a substantial body of epidemiologic literature showing a clear and consistent association between concentrations of ambient PM and negative health effects (Anderson et al. 2003; Brunekreef and Holgate 2002; Dockery 2001; Katsouyanni et al. 1996; Samet et al. 2000). Less clear is the biologic mechanism by which PM could be causing this morbidity and mortality. One avenue by which investigators can offer direction is identifying which outcomes are most strongly and consistently associated with PM10 and conditions that modify that outcome. Epidemiologic research continues to narrow the focus around specific outcomes, from mortality to cause-specific mortality and from hospitalization for cardiovascular disease to MI and examination of specific modifiers.
The further epidemiologic identification of individual traits that are associated with increased risk of mortality and morbidity from increased concentrations of PM air pollution will continue to direct ongoing research into the biologic mechanism and provide critical data for risk assessment and inform policy makers.
Footnotes
This study was funded by the U.S. Environmental Protection Agency (EPA)/Harvard Center on Ambient Particle Health Effects EPA Particulate Matter Center (EPA grant R827353 and National Institute of Environmental Health Sciences grant ES0002).
References
- Anderson HR, Atkinson RW, Bremner SA, Marston L. Particulate air pollution and hospital admissions for cardiorespiratory diseases: are the elderly at greater risk? Eur Respir J. 2003;40(suppl):39s–46s. doi: 10.1183/09031936.03.00402203. [DOI] [PubMed] [Google Scholar]
- Atkinson RW, Anderson HR, Sunyer J, Ayres J, Baccini M, Vonk JM, et al. Acute effects of particulate air pollution on respiratory admissions: results from APHEA 2 project. Air Pollution and Health: A European Approach. Am J Respir Crit Care Med. 2001;164:1860–1866. doi: 10.1164/ajrccm.164.10.2010138. [DOI] [PubMed] [Google Scholar]
- Bateson TF, Schwartz J. Control for seasonal variation and time trend in case-crossover studies of acute effects of environmental exposures. Epidemiology. 1999;10:539–544. [PubMed] [Google Scholar]
- Bateson TF, Schwartz J. Selection bias and confounding in case-crossover analyses of environmental time-series data. Epidemiology. 2001;12:654–661. doi: 10.1097/00001648-200111000-00013. [DOI] [PubMed] [Google Scholar]
- Berkey CS, Hoaglin DC, Antczak-Bouckoms A, Mosteller F, Colditz GA. Meta-analysis of multiple outcomes by regression with random effects. Stat Med. 1998;17:2537–2550. doi: 10.1002/(sici)1097-0258(19981130)17:22<2537::aid-sim953>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- Braga AL, Zanobetti A, Schwartz J. Do respiratory epidemics confound the association between air pollution and daily deaths? Eur Respir J. 2000;16:723–728. doi: 10.1034/j.1399-3003.2000.16d26.x. [DOI] [PubMed] [Google Scholar]
- Braga AL, Zanobetti A, Schwartz J. The lag structure between particulate air pollution and respiratory and cardiovascular deaths in 10 US cities. J Occup Environ Med. 2001;43:927–933. doi: 10.1097/00043764-200111000-00001. [DOI] [PubMed] [Google Scholar]
- Brook RD, Brook JR, Rajagopalan S. Air pollution: the “heart” of the problem. Curr Hypertens Rep. 2003;5:32–39. doi: 10.1007/s11906-003-0008-y. [DOI] [PubMed] [Google Scholar]
- Brunekreef B, Holgate ST. Air pollution and health. Lancet. 2002;360:1233–1242. doi: 10.1016/S0140-6736(02)11274-8. [DOI] [PubMed] [Google Scholar]
- Daniels MJ, Dominici F, Samet JM, Zeger SL. Estimating particulate matter-mortality dose-response curves and threshold levels: an analysis of daily time-series for the 20 largest US cities. Am J Epidemiol. 2000;152:397–406. doi: 10.1093/aje/152.5.397. [DOI] [PubMed] [Google Scholar]
- D’Ippoliti D, Forastiere F, Ancona C, Agabiti N, Fusco D, Michelozzi P, et al. Air pollution and myocardial infarction in Rome: a case-crossover analysis. Epidemiology. 2003;14:528–535. doi: 10.1097/01.ede.0000082046.22919.72. [DOI] [PubMed] [Google Scholar]
- Dockery DW. Epidemiologic evidence of cardiovascular effects of particulate air pollution. Environ Health Perspect. 2001;109:483–486. doi: 10.1289/ehp.01109s4483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donaldson K, Stone V, Seaton A, MacNee W. Ambient particle inhalation and the cardiovascular system: potential mechanisms. Environ Health Perspect. 2001;109:523–527. doi: 10.1289/ehp.01109s4523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghio AJ, Kim C, Devlin RB. Concentrated ambient air particles induce mild pulmonary inflammation in healthy human volunteers. Am J Respir Crit Care Med. 2000;162:981–988. doi: 10.1164/ajrccm.162.3.9911115. [DOI] [PubMed] [Google Scholar]
- Goldberg M, Burnett RT, Brook J, Bailar JC, III, Valois MF, Vincent R. Associations between daily cause-specific mortality and concentrations of ground-level ozone in Montreal, Quebec. Am J Epidemiol. 2001;154:817–826. doi: 10.1093/aje/154.9.817. [DOI] [PubMed] [Google Scholar]
- Hoek G, Brunekreef B, Fischer P, van Wijnen J. The association between air pollution and heart failure, arrhythmia, embolism, thrombosis, and other cardiovascular causes of death in a time series study. Epidemiology. 2001;12:355–357. doi: 10.1097/00001648-200105000-00017. [DOI] [PubMed] [Google Scholar]
- Ibald-Mulli A, Stieber J, Wichmann HE, Koenig W, Peters A. Effects of air pollution on blood pressure: a population-based approach. Am J Public Health. 2001;91:571–577. doi: 10.2105/ajph.91.4.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalkstein LS, Valimont KM. An evaluation of summer discomfort in the United States using a relative climatological index. Bull Am Meteorol Soc. 1986;67:842–848. [Google Scholar]
- Katsouyanni K, Schwartz J, Spix C, Touloumi G, Zmirou D, Zanobetti A, et al. Short term effects of air pollution on health: a European approach using epidemiologic time series data. The APHEA protocol. J Epidemiol Community Health. 1996;50(suppl 1):S12–S18. doi: 10.1136/jech.50.suppl_1.s12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koken PJ, Piver WT, Ye F, Elixhauser A, Olsen LM, Portier CJ. Temperature, air pollution, and hospitalization for cardiovascular diseases among elderly people in Denver. Environ Health Perspect. 2003;111:1312–1317. doi: 10.1289/ehp.5957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy D, Lumley T, Sheppard L, Kaufman J, Checkoway H. Referent selection in case-crossover analyses of acute health effects of air pollution. Epidemiology. 2001;12:186–192. doi: 10.1097/00001648-200103000-00010. [DOI] [PubMed] [Google Scholar]
- Linn WS, Gong H, Jr, Clark KW, Anderson KR. Day-to-day particulate exposures and health changes in Los Angeles area residents with severe lung disease. J Air Waste Manage Assoc. 1999;49:108–115. doi: 10.1080/10473289.1999.10463890. [DOI] [PubMed] [Google Scholar]
- Linn WS, Szlachcic Y, Gong H, Jr, Kinney PL, Berhane KT. Air pollution and daily hospital admissions in metropolitan Los Angeles. Environ Health Perspect. 2000;108:427–434. doi: 10.1289/ehp.00108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991;133:144–153. doi: 10.1093/oxfordjournals.aje.a115853. [DOI] [PubMed] [Google Scholar]
- Mann JK, Tager IB, Lurmann F, Segal M, Quesenberry CP, Jr, Lugg MM, et al. Air pollution and hospital admissions for ischemic heart disease in persons with congestive heart failure or arrhythmia. Environ Health Perspect. 2002;110:1247–1252. doi: 10.1289/ehp.021101247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Environmental Satellite, Data, and Information Service 2003. Td-3280 U.S. Surface Airways and Airways Solar Radiation Hourly. Washington, DC:U.S. Department of Commerce.
- Nehls GJ, Akland GG. Procedures for handling aerometric data. J Air Pollut Control Assoc. 1973;23:180–184. [Google Scholar]
- Oftedal B, Nafstad P, Magnus P, Bjorkly S, Skrondal A. Traffic related air pollution and acute hospital admission for respiratory diseases in Drammen, Norway 1995–2000. Eur J Epidemiol. 2003;18:671–675. doi: 10.1023/a:1024884502114. [DOI] [PubMed] [Google Scholar]
- Ozkaynak H, Schatz AD, Thurston GD. Relationships between aerosol extinction coefficients derived from airport visual range observations and alternative measures of airborne particle mass. J Air Pollut Control Assoc. 1985;35:1176–1185. [Google Scholar]
- Peters A, Dockery DW, Muller JE, Mittleman MA. Increased particulate air pollution and the triggering of myocardial infarction. Circulation. 2001a;103:2810–2815. doi: 10.1161/01.cir.103.23.2810. [DOI] [PubMed] [Google Scholar]
- Peters A, Doring A, Wichmann HE, Koenig W. Increased plasma viscosity during an air pollution episode: a link to mortality? Lancet. 1997;349:1582–1587. doi: 10.1016/S0140-6736(97)01211-7. [DOI] [PubMed] [Google Scholar]
- Peters A, Frohlich M, Doring A, Immervoll T, Wichmann HE, Hutchinson WL, et al. Particulate air pollution is associated with an acute phase response in men; results from the Monica-Augsburg study. Eur Heart J. 2001b;22:1198–1204. doi: 10.1053/euhj.2000.2483. [DOI] [PubMed] [Google Scholar]
- Pope CA, III, Burnett RTP, Thurston GDS, Thun MJMD, Calle EEP, Krewski DP, et al. Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation. 2004a;109:71–77. doi: 10.1161/01.CIR.0000108927.80044.7F. [DOI] [PubMed] [Google Scholar]
- Pope CA, III, Hansen ML, Long RW, Nielsen KR, Eatough NL, Wilson WE, et al. Ambient particulate air pollution, heart rate variability, and blood markers of inflammation in a panel of elderly subjects. Environ Health Perspect. 2004b;112:339–345. doi: 10.1289/ehp.6588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samet JM, Zeger SL, Dominici F, Curriero F, Coursac I, Dockery DW, et al. The National Morbidity, Mortality, and Air Pollution Study. Part II: morbidity and mortality from air pollution in the United States. Res Rep Health Eff Inst. 2000;94:5–70. [PubMed] [Google Scholar]
- Samet JM, Zeger SL, Kelsall J, Xu J, Kalkstein L. Does weather confound or modify the association of particulate air pollution with mortality? An analysis of the Philadelphia data, 1973–1980. Environ Res. 1998;77:9–19. doi: 10.1006/enrs.1997.3821. [DOI] [PubMed] [Google Scholar]
- Schwartz J. Total suspended particulate matter and daily mortality in Cincinnati, Ohio. Environ Health Perspect. 1994a;102:186–189. doi: 10.1289/ehp.94102186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz J. What are people dying of on high air pollution days? Environ Res. 1994b;64:26–35. doi: 10.1006/enrs.1994.1004. [DOI] [PubMed] [Google Scholar]
- Schwartz J. Air pollution and hospital admissions for heart disease in eight U.S. counties. Epidemiology. 1999;10:17–22. [PubMed] [Google Scholar]
- Schwartz J. Assessing confounding, effect modification, and thresholds in the association between ambient particles and daily deaths. Environ Health Perspect. 2000;108:563–568. doi: 10.1289/ehp.00108563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz J, Zanobetti A. Using meta-smoothing to estimate dose-response trends across multiple studies, with application to air pollution and daily death. Epidemiology. 2000;11:666–672. doi: 10.1097/00001648-200011000-00009. [DOI] [PubMed] [Google Scholar]
- Schwartz J, Zanobetti A, Bateson T. 2003. Morbidity and mortality among elderly residents in cities with daily PM measurements. In: Revised Analyses of Time-Series Studies of Air Pollution and Health. Special Report. Boston:Health Effect Institute, 25–53. Available: http://www.healtheffects.org/Pubs/TimeSeries.pdf [accessed 7 June 2005].
- Steadman RG. The assessment of sultriness. Part II: effects of wind, extra radiation and barometric pressure on apparent temperature. J Appl Meteorol. 1979;18:874–885. [Google Scholar]
- Sullivan J, Ishikawa N, Sheppard L, Kaufman J. Relation between short-term fine PM exposure and onset of myocardial infarction in a community-based myocardial infarction treatment trial [Abstract] Am J Respir Crit Care Med. 2003;167:A332. [Google Scholar]
- Sunyer J, Ballester F, Tertre AL, Atkinson R, Ayres JG, Forastiere F, et al. The association of daily sulfur dioxide air pollution levels with hospital admissions for cardiovascular diseases in Europe (the APHEA-II study) Eur Heart J. 2003;24:752–760. doi: 10.1016/s0195-668x(02)00808-4. [DOI] [PubMed] [Google Scholar]
- Sunyer J, Schwartz J, Tobias A, Macfarlane D, Garcia J, Anto JM. Patients with chronic obstructive pulmonary disease are at increased risk of death associated with urban particle air pollution: a case-crossover analysis. Am J Epidemiol. 2000;151:50–56. doi: 10.1093/oxfordjournals.aje.a010121. [DOI] [PubMed] [Google Scholar]
- Suwa T, Hogg JC, Quinlan KB, Ohgami A, Vincent R, van Eeden SF. Particulate air pollution induces progression of atherosclerosis. J Am Coll Cardiol. 2002;39:935–942. doi: 10.1016/s0735-1097(02)01715-1. [DOI] [PubMed] [Google Scholar]
- WHO 1977. Manual of the International Statistical Classification of Diseases, Injuries, and Causes of Death. 9th Revision. Geneva:World Health Organization.
- Zanobetti A, Canner MJ, Stone PH, Schwartz J, Sher D, Eagan-Bengston E, et al. Ambient pollution and blood pressure in cardiac rehabilitation patients. Circulation. 2004;110:2184–2189. doi: 10.1161/01.CIR.0000143831.33243.D8. [DOI] [PubMed] [Google Scholar]
- Zanobetti A, Schwartz J, Dockery DW. Airborne particles are a risk factor for hospital admissions for heart and lung disease. Environ Health Perspect. 2000a;108:1071–1077. doi: 10.1289/ehp.001081071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanobetti A, Schwartz J, Gold D. Are there sensitive subgroups for the effects of airborne particles? Environ Health Perspect. 2000b;108:841–845. doi: 10.1289/ehp.00108841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zmirou D, Schwartz J, Saez M, Zanobetti A, Wojtyniak B, Touloumi G, et al. Time-series analysis of air pollution and cause-specific mortality. Epidemiology. 1998;9:495–503. [PubMed] [Google Scholar]


