Abstract
Intranasal immunization of mice with purified Brucella melitensis lipopolysaccharide (LPS) as a noncovalent complex with Neisseria meningitidis group B outer membrane protein (GBOMP) elicited a high-titer anti-LPS systemic antibody response and a significant mucosal antibody response. The anti-LPS immunoglobulin G (IgG) antibody was predominantly of the IgG1 subtype, although there was some response of the IgG2a, IgG2b, and IgG3 subtypes. The antibody titer remained high for 16 weeks postimmunization. Immunized mice and sham-immunized control mice were challenged intranasally with 104 CFU of virulent B. melitensis strain 16 M 4 weeks after the second dose of vaccine. The numbers of bacteria in lungs, livers, and spleens at 3 days, 9 days, and 8 weeks postchallenge were determined. Bacteria were found in lungs of all mice on day 3, but there was no disseminated infection of liver or spleen. By day 9, 40% of the mice had infected spleens and livers. At 8 weeks postchallenge, spleens of 25 of 62 immunized mice were infected, compared to 61 of 62 control mice (P < 0.0001). The livers of 12 of 43 immunized mice were infected, compared to 22 of 36 control mice (P = 0.005). In contrast, the lungs of 26 of 46 immunized mice were still infected, compared to 27 of 44 control mice. The numbers of bacterial CFU in lungs of immunized and control animals were identical. These studies show that intranasal immunization with B. melitensis LPS-GBOMP subunit vaccine significantly protects mice against intranasal challenge with virulent B. melitensis. Vaccination reduces bacterial dissemination to spleen and liver but has no effect on the course of lung infection.
Brucellosis is a zoonosis that affects numerous species of animals, especially ruminants. Different Brucella species preferentially infect cattle (Brucella abortus), goats (B. melitensis), rodents (B. neotomae), sheep (B. ovis), dogs (B. canis), and pigs (B. suis). More recently, new species of Brucella have been isolated from marine mammals (1). Humans can acquire infection by contact with infected animals, by inhalation of aerosol, or by ingestion of contaminated animal products, such as infected milk, milk products, or meat. The most common human pathogens, B. abortus, B. melitensis, and B. suis, typically cause fever, sweats, and malaise (23, 35). Chronic infection may lead to other complications, including bone and joint infections, male genitourinary disease, meningitis, and endocarditis (19). Although Brucella vaccines are available for immunization of animals (12), there is no Brucella vaccine approved for human use in the United States. Approaches to vaccine development have included administration of live, attenuated Brucella mutants or injection of killed whole cells, antigenic fractions of cell lysates, or recombinant protein antigens administered with adjuvants. In general, successful nonliving vaccines elicit antibody directed against the surface O polysaccharide (OPS) of Brucella outer membrane lipopolysaccharide (LPS). Numerous studies have demonstrated that immunization of mice with killed smooth strains of B. abortus or B. melitensis reduces the number of B. abortus CFU in the spleen or liver when mice are challenged intravenously or intraperitoneally (i.p.) (21, 25, 26). Similarly, cell lysate fractions that induce anti-LPS antibodies also reduce the intensity of spleen and liver infection in intravenous or i.p. challenge models using either B. abortus or B. melitensis (7, 15, 28, 30-32, 34). Mice immunized with live or dead B. abortus and then challenged subcutaneously contain the organism at the site of injection or in the draining lymph node (24). This anti-Brucella effect, which can be passively transferred by immune serum, also reduces the number of bacteria in the lymph node and partially prevents dissemination. A similar localizing effect can be induced by immunization with LPS (29).
We have developed a vaccine composed of purified LPS from B. melitensis 16 M noncovalently complexed with outer membrane protein from Neisseria meningitidis group B (GBOMP). Intranasal immunization of mice and guinea pigs with this vaccine elicits both humoral and mucosal anti-LPS antibody responses (33). Here we further examine the persistence of antibody and the unique pattern of anti-LPS immunoglobulin G (IgG) subtype response elicited by the LPS-GBOMP vaccine and demonstrate protective efficacy against disseminated infection of spleen and liver following intranasal challenge of mice with 16 M.
(This work was presented in part as a poster at the 6th National Symposium on Basic Aspects of Vaccines, 3 to 5 May 2000, Bethesda, Md.)
MATERIALS AND METHODS
B. melitensis strain 16 M was obtained from Gerhardt Schurig (Virginia Polytechnic Institute, Blacksburg), and was grown in brucella broth at 37°C for 48 h. The LPS was extracted from killed B. melitensis cells and purified by a method described previously (33). N. meningitidis group B strain 8047 was from the collection of the Walter Reed Army Institute of Research. The bacteria were grown in a synthetic medium, and outer membrane protein (GBOMP) was extracted as described before (36, 37). Phosphatase-labeled goat anti-mouse IgG, IgA, IgG1, IgG2a, IgG2b, and IgG3 were purchased from Kirkegaard & Perry Laboratories (Gaithersburg, Md.). Female BALB/c mice (6 to 8 week old) were purchased from Jackson Laboratories (Bar Harbor, Maine) and were housed in the biosafety level 3 laboratory at the Armed Forces Institute of Pathology. The mice were cared for and handled in accordance with National Institutes of Health guidelines, and we adhered to the Guide for Care and Use of Laboratory Animals, Institute of Laboratory Animal Resources, National Research Council. The Institutional Animal Care and Use Committee and biosafety committee approved the study protocols. Empigen BB was obtained from Albright & Wilson (Whitehaven, United Kingdom). Yersinia enterocolitica strain O:9 was obtained from Luther Lindler of the Department of Bacterial Diseases, Walter Reed Army Institute of Research. Phenol-phase LPS of Y. enterocolitica strain O:9 was prepared by the method of Johnson and Perry (16).
Preparation of vaccine.
The B. melitensis LPS-GBOMP noncovalent complex vaccine was prepared essentially as described before (33). Briefly, purified B. melitensis LPS (51 mg) was dissolved in 42 ml of TEEN buffer (0.05 M Tris, 0.15 M NaCl, 0.005 M EDTA, 0.1% Empigen BB, pH 8.0). Purified GBOMP in TEEN buffer (8.0 ml at 6.8 mg/ml) was added to the LPS solution. The mixture (50 ml) was kept at 5°C for 30 min. The detergent (Empigen BB) was removed, and buffer was exchanged with sterile 0.9% NaCl solution by cartridge filtration (A/G Technology Corporation, Needham, Mass.), using an UFP-10-C-4A cartridge (10,000-molecular-weight cutoff), according to the manufacturer's instructions. The final product was filtered (0.20-μm-pore-size membrane) and stored at −20°C until use. The LPS content of the vaccine formulation was determined by the method of Dubois et al. (6), using purified B. melitensis LPS as a standard.
Immunization and challenge of mice.
Groups of female BALB/cJ mice (Jackson Laboratories) were immunized with the vaccine. Control mice were given sterile saline. Each mouse was given an intramuscular injection of 0.3 mg of xylazine hydrochloride (Rompun) and 1.0 mg of ketamine hydrochloride (Ketaset) in 50 μl of sterile saline, using a 1-ml syringe fitted with a 27-gauge needle. The mice were then immunized by administration of 25 μl of vaccine containing 10 μg of LPS slowly into the nostrils with a micropipette. A second dose of vaccine was given 4 weeks after the first dose. At intervals after immunization and/or challenge, blood was collected by cardiac puncture and sera were stored at −20°C until they were analyzed by enzyme-linked immunosorbent assay (ELISA). In one study, bronchoalveolar lavage (BAL) fluid was also obtained as described previously (33) and frozen at −20°C until used in ELISA.
Groups of immunized and control mice were challenged intranasally at various times (2 to 6 weeks after the second dose of vaccine), usually with 104 CFU of B. melitensis 16 M suspended in 30 μl of phosphate-buffered saline (PBS) (20). In one experiment, mice were challenged with 105 CFU. After challenge, spleens, lungs, and livers were aseptically collected at various times (typically 3 days, 9 days, and 8 weeks postchallenge). Five mice per group were used for the 3- and 9-day time points, and approximately 15 mice per group were used for the 8-week time point. Brucella CFU in organs was determined by dilution and culture on brucella agar as described before (14). For an occasional mouse, culture plates from lung or liver homogenates were unreadable due to contaminant overgrowth, so the number of these organs analyzed was less than the number of spleens analyzed.
ELISA.
ELISA was performed in 96-well flat-bottom polystyrene microtiter plates (Costar, Cambridge, Mass.) by the method of Engvall and Perlmann (9). Briefly, wells were coated with purified B. melitensis LPS at 10 μg/ml in PBS (0.01 M sodium phosphate, 0.14 M sodium chloride, 0.02% sodium azide, pH 7.4) by adding 100 μl to each well and incubating at 37°C for 3 h. The wells were washed three times with PBS. Serial twofold dilutions of primary antibodies (100 μl) were made on the plates, and the plates were kept at room temperature (25°C) for 16 h. The plates were incubated with phosphatase-labeled goat anti-mouse secondary antibodies (Kirkegaard & Perry Laboratories). The substrate used was p-nitrophenyl phosphate disodium (Sigma Chemical Co., St. Louis, Mo.) at 1 mg/ml and was incubated for 30 min at room temperature. Absorbance was read at 405 nm on a plate reader (Dynatech, Alexandria, Va.). ELISA antibody titers were calculated by using the dilution of serum or nasal wash giving an optical density (OD) at 405 nm nearest 0.5 (which falls within the linear part of the OD-dilution curve). The titer, expressed as OD units, was obtained by multiplying the reciprocal dilution of the serum or nasal wash by the OD (A405) at that dilution. ELISA was also performed with phenol-phase LPS prepared from Y. enterocolitica O:9 as the antigen for coating the plates.
Statistical methods.
Antibody titers of groups of mice were expressed as means ± standard deviations. The intensity of bacterial infection in organs was expressed as the mean log CFU ± standard deviation per infected organ. The lower limit of detection for infection of organs was 2 CFU. The significance of differences in ELISA titers and in log CFU per infected organ at different time points was determined by Student's t test. The significance of differences in percent infected spleens, livers, and lungs of immunized mice versus control mice was determined by Fisher's exact method.
Disclaimer.
The opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the U.S. Army.
RESULTS
Immune response in mice.
Two weeks after intranasal immunization with B. melitensis LPS-GBOMP vaccine, anti-B. melitensis LPS IgG titers were significantly increased (Table 1). Antibody titers rose a further fourfold at 4 weeks after the first dose of vaccine. Two weeks after the second dose of vaccine, there was another 20-fold rise. The total IgG antibody titer stayed high (approximately 25,000 OD units) until 16 weeks after the second dose and then declined to about one-third the peak level and stayed there until the study was terminated 25 weeks after the second dose of vaccine. The pattern of IgG1 response closely resembled that of total IgG. In contrast, IgG2a and IgG2b responses were blunted compared to the IgG1 response, with only a twofold rise between the first and fourth weeks after the first dose and only a further eightfold (IgG2a) or fivefold (IgG2b) rise after the second dose. The IgG3 response was also blunted compared to that of IgG1, with a fourfold rise between the first and fourth weeks after the first dose and only a further sixfold rise after the second dose.
TABLE 1.
Duration of anti-B. melitensis LPS IgG in mouse sera after intranasal immunization with B. melitensis LPS-GBOMP vaccinea
| Vaccine dose | Time (wk) after vaccine dose | OD units (mean ± SD)b
|
||||
|---|---|---|---|---|---|---|
| IgG | IgG1 | IgG2a | IgG2b | IgG3 | ||
| First | 2 | 348 ± 273 | 183 ± 197 | 30 ± 20 | 33 ± 37 | 92 ± 73 |
| 4 | 1,365 ± 464 | 988 ± 290 | 57 ± 43 | 73 ± 16 | 367 ± 143 | |
| Second | 2 | 27,332 ± 14,980 | 22,341 ± 10,983 | 217 ± 113 | 385 ± 322 | 2,111 ± 829 |
| 4 | 25,373 ± 9,477 | 23,805 ± 9,529 | 461 ± 217 | 288 ± 92 | 1,413 ± 393 | |
| 8 | 27,267 ± 13,358 | 19,620 ± 8,363 | 470 ± 412 | 274 ± 145 | 1,257 ± 494 | |
| 12 | 26,675 ± 11,290 | 21,136 ± 6,902 | 194 ± 134 | 215 ± 78 | 1,075 ± 483 | |
| 16 | 23,830 ± 13,527 | 21,756 ± 14,270 | 245 ± 179 | 318 ± 90 | 1,031 ± 450 | |
| 19 | 7,314 ± 4,801 | 6,387 ± 3,094 | 298 ± 163 | 20 ± 5 | 507 ± 163 | |
| 21 | 10,564 ± 6,439 | 11,896 ± 8,166 | 193 ± 84 | 20 ± 7 | 591 ± 266 | |
| 25 | 8,633 ± 3,723 | 7,740 ± 2,942 | 176 ± 188 | 15 ± 6 | 412 ± 267 | |
Mice were immunized twice intranasally 4 weeks apart with B. melitensis LPS-GBOMP vaccine. Sera were collected at the times indicated for ELISA.
Data are for 10 animals at each time point. Negative control sera run simultaneously in these assays had titers of less than 1 OD unit.
The B. melitensis LPS used for immunization and ELISA plate coating in these studies contained 5.5% protein. To determine whether the IgG1 responses described in Table 1 were directed against LPS determinants or protein, we selected sera obtained 2 and 4 weeks after the second dose of vaccine and repeated the ELISA using plates coated with LPS from Y. enterocolitica O:9, which has 80% structural homology with B. melitensis LPS. This Y. enterocolitica LPS preparation contained <0.1% Yersinia protein. Anti-Yersinsia O:9 LPS IgG1 titers were similar to anti-B. melitensis LPS IgG1 titers (Tables 1 and 2). Similarly, the anti-Yersinia IgG2a, IgG2b, and IgG3 titers were at least 80% lower than the IgG1 titers. These data indicated that the anti-Brucella LPS antibody elicited by vaccination consisted primarily of IgG1 directed against the O chain.
TABLE 2.
Subclasses of anti-LPS antibody after immunization with LPS-GBOMP vaccinea
| Antibody | Sera no. (wk after second dose) | ELISA antibody units (mean ± SD)b
|
|||
|---|---|---|---|---|---|
| IgG1 | IgG2a | IgG2b | IgG3 | ||
| Anti-B. melitensis LPSc | 31-40 (2) | 22,341 ± 10,983 | 217 ± 113 | 385 ± 322 | 2,111 ± 829 |
| 41-50 (4) | 23,805 ± 9,529 | 461 ± 217 | 288 ± 92 | 1,413 ± 393 | |
| Anti-Y. enterocolitica LPSd | 31-39 (2) | 19,241 ± 13,837 | 2,579 ± 4,743 | 3,900 ± 7,409 | 3,934 ± 2,348 |
| 41-49 (4) | 24,396 ± 12,904 | 770 ± 714 | 1,022 ± 1,377 | 4,456 ± 2,235 | |
Mice were immunized twice intranasally 4 weeks apart with B. melitensis LPS-GBOMP vaccine. Sera were collected 2 or 4 weeks after the second dose for ELISA.
Data are expressed in OD units. Negative control sera run simultaneously in these assays had titers of less than 1 OD unit.
The B. melitensis LPS contained 5.5% protein.
The Y. enterocolitica O:9 LPS contained 0.1% protein. At the time of running Y. enterocolitica O:9 LPS ELISA, we ran out of sera 40 and 50; therefore, there were 9 instead of 10 sera for each set.
In another experiment (Table 3), we determined the effect of challenge on IgG titers of sera from immunized or nonimmunized mice. Mice immunized with LPS-GBOMP had prechallenge titers at 4 weeks after the first and second doses of vaccine comparable to those shown in Table 1. Upon challenge, this titer did not increase. Indeed, the serum antibody titer in immunized mice dropped from 26,705 ± 17,258 OD units immediately prechallenge to 11,970 ± 10,644 OD units 3 days after challenge and stayed at that level for up to 8 weeks postchallenge. Differences between any of these postchallenge titers and the immediate prechallenge titer were not statistically significant. Sham-immunized mice given intranasal saline instead of LPS-GBOMP had negligible anti-LPS antibody (<10 OD units) at all time points before and up to 9 days after intranasal challenge with 16 M, but they developed high antibody titers at 8 weeks postchallenge (Table 3).
TABLE 3.
Anti-B. melitensis LPS serum IgG after intranasal challengea
| Vaccine | Time point | Anti-LPS IgG (mean ± SD)b |
|---|---|---|
| B. melitensis LPS- GBOMP | 4 wk after first dose | 4,421 ± 2,368 |
| 4 wk after second dose | 26,705 ± 17,258 | |
| 3 days after challenge | 11,970 ± 10,644 | |
| 9 days after challenge | 13,495 ± 5,563 | |
| 8 wk after challenge | 10,547 ± 4,810 | |
| Saline control | 4 wk after first and second doses | <10 |
| 3 and 9 days after second challenge | <10 | |
| 8 wk after challenge | 19,765 ± 11,416 |
Mice were immunized intranasally with two doses of vaccine or saline 4 weeks apart and then challenged 4 weeks after the second dose. Sera were collected for ELISA at the times indicated.
Data are expressed as OD units. n = 5 mice for all time points except 8 weeks; at 8 weeks, n = 15 mice.
Intranasal immunization also led to anti-B. melitensis LPS IgG and IgA in BAL fluid (Table 4). Both IgG and IgA antibodies were detected at 4 weeks after the first and second doses of vaccine. The titer at 4 weeks after administration of the second vaccine dose increased three- to fourfold compared to the titer at 4 weeks after administration of the first dose. BAL samples from control mice had no detectable anti-B. melitensis LPS IgG or IgA.
TABLE 4.
Anti-B. melitensis LPS IgG and IgA in BAL fluid from immunized and control micea
| Vaccine dose | Vaccine | Titer (mean ± SD)b
|
|
|---|---|---|---|
| IgG | IgA | ||
| First | B. melitensis LPS-GBOMP | 56 ± 52 | 3 ± 2 |
| Saline control | <1 | <1 | |
| Second | B. melitensis LPS-GBOMP | 202 ± 132 | 10 ± 15 |
| Saline control | <1 | <1 | |
Mice were immunized intranasally with two doses of vaccine or saline 4 weeks apart. BAL fluid was collected for ELISA 4 weeks after the indicated vaccine dose.
Mean ELISA OD units obtained from five mice per group.
Effect of immunization on infection of spleen, liver, and lung.
These strong LPS-specific antibody responses were associated with protection from disseminated infection after intranasal challenge with 16 M. Immunization did not, however, prevent pulmonary infection or enhance clearance from the lung. In four separate experiments, mice were immunized with LPS-GBOMP or sham immunized with saline in two doses intranasally 4 weeks apart and were challenged intranasally with 104 CFU of 16 M 4 weeks after the second dose. In the first of these experiments, tissues were collected at both early and late time points after challenge to determine the number of bacteria. Lungs were infected in all mice in both the immunized and sham-immunized groups at 3 days and 9 days postchallenge (Table 5). There was no difference in the number of CFU per lung among immunized or sham-immunized animals at either time point. Spleens were harvested at 8 weeks postchallenge in all four of these experiments. Spleens of 25 of 62 immunized mice were infected, compared to 61 of 62 spleens of mice sham immunized with saline (P < 0.0001). In three of these experiments, livers were also analyzed for infection at 8 weeks after challenge. Livers of 12 of 43 immunized mice were infected, compared to 22 of 36 livers of mice sham immunized with saline (P = 0.005) (Table 6). In two additional experiments, which included mice sham immunized with GBOMP alone, animals were challenged with 105 CFU and spleens were harvested 8 weeks later. In the group immunized with GBOMP alone, 17 of 18 spleens were infected, compared to 15 of 16 spleens from animals sham immunized with saline and 11 of 19 spleens from animals immunized with LPS-GBOMP (P = 0.018 versus saline and 0.011 versus GBOMP).
TABLE 5.
Spleen, liver, and lung infection 3 and 9 days after intranasal challenge with 104 CFU of 16 Ma
| Vaccine | Time after challenge (days) | No. of spleens infected/total | No. of livers infected/total | No. of lungs infected/total | Log CFU/lung (mean ± SD) |
|---|---|---|---|---|---|
| B. melitensis LPS-GBOMP | 3 | 0/5 | 0/5 | 5/5 | 3.18 ± 1.17 |
| Saline control | 3 | 0/5 | 0/5 | 5/5 | 3.95 ± 0.45 |
| B. melitensis LPS-GBOMP | 9 | 2/5 | 2/5 | 5/5 | 4.78 ± 0.36 |
| Saline control | 9 | 2/5 | 2/5 | 5/5 | 4.42 ± 0.41 |
Mice were immunized intranasally with two doses of vaccine or saline 4 weeks apart and then challenged intranasally 4 weeks after the second dose of vaccine. Bacterial CFU were determined at the indicated times after challenge by plating organ homogenates on brucella agar. The limit of detection was 2 CFU per organ.
TABLE 6.
Spleen, liver, and lung infection 8 weeks after intranasal challenge with 104 CFU of 16 Ma
| Vaccine | No. of spleens infected/totalb | Log CFU/infected spleen (mean ± SD) | No. of livers infected/totalc | Log CFU/infected liver (mean ± SD) | No. of lungs infected/totalc | Log CFU/infected lung (mean ± SD)c |
|---|---|---|---|---|---|---|
| LPS-GBOMP | 25/62d | 3.35 ± 1.44 | 12/43e | 3.4 ± 0.25 | 26/46 | 3.21 ± 0.48 |
| Saline control | 61/62 | 3.66 ± 1.13 | 22/36 | 3.2 ± 1.1 | 27/44 | 3.28 ± 1.39 |
See Table 5, footnote a.
Combined data from four experiments.
Combined data from three experiments.
P < 0.001 versus saline control (two-tailed Fisher's exact test).
P = 0.005 versus saline control (two-tailed Fisher's exact test).
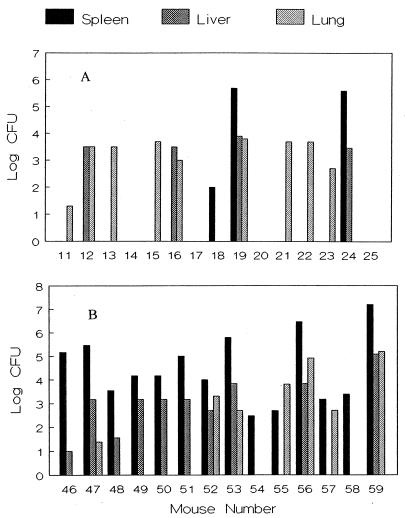
In contrast to this vaccine-induced protection of liver and spleen from disseminated infection, there was no difference in clearance of bacteria from the lungs of immunized mice at 8 weeks compared to sham-immunized controls. The lungs of 26 of 46 immunized mice and 27 of 44 control mice challenged with 104 CFU remained infected at 8 weeks postchallenge, and the numbers of CFU of lung were similar in both groups (Table 6). Figure 1 shows the relationship of lung, liver, and spleen CFU in one of these experiments. In the group sham immunized with saline (Fig. 1B), all seven animals with persistent lung infections also had spleen infection. Five of these seven animals also had liver infection. In contrast, lung infection was present in nine immunized animals, but only two of these animals had concomitant spleen and liver infection, and one additional mouse had concomitant liver infection only (Fig. 1A).
FIG. 1.
(A) Log CFU in spleens, livers, and lungs of B. melitensis LPS-GBOMP-immunized mice. Mice were given vaccine twice intranasally at 4-week intervals and challenged intranasally 4 weeks after the second dose with 104 CFU of B. melitensis 16 M. Bacterial CFU were determined 8 weeks after challenge by plating homogenates of lung, liver, and spleen on brucella agar. The limit of detection was 2 CFU per organ. Each bar represents one mouse. (B). Log CFU in spleens, livers, and lungs of sham-immunized mice. Mice were given saline twice intranasally at 4-week intervals and challenged intranasally with 104 CFU of B. melitensis 16 M 4 weeks after the second dose of saline. Bacterial CFU were determined 8 weeks after challenge by plating homogenates of lung, liver, and spleen on brucella agar. The limit of detection was 2 CFU per organ. Each bar represents one mouse.
Among infected animals, the number of CFU per organ showed substantial overlap between immunized and sham-immunized groups (Fig. 1). The spleen showed the highest intensity of infection, with ranges of 2.4 to 7.2 log CFU in sham-immunized mice and 2.0 to 5.7 log CFU in immunized animals. The number of bacteria ranged from 1.3 to 5.2 log CFU in the lungs of control mice and from 1.3 to 3.8 log CFU in the lungs of immunized mice. Similarly, the number of bacteria ranged from 1.0 to 5.1 log CFU in livers of sham-immunized mice and from 3.4 to 3.9 log CFU in livers of immunized mice. These findings were consistent in all experiments.
A single experiment was performed to determine the onset and persistence of the protective effect. Mice were challenged with 104 CFU at either 2 or 6 weeks after the second dose of vaccine, and the number of CFU in the spleens was determined 8 weeks later. For mice challenged at 2 weeks postvaccination, 12 of 15 spleens of sham-immunized mice were infected, compared to 5 of 15 spleens from immunized mice (P = 0.025). For mice challenged at 6 weeks postvaccination, 8 of 15 spleens of control mice were infected, compared to 1 of 15 spleens from immunized mice (P = 0.014). In total, these data indicated protection from 2 weeks to at least 6 weeks after administration of the second dose of vaccine.
DISCUSSION
We previously reported that intranasal immunization of mice with B. melitensis LPS-GBOMP noncovalent complex vaccine elicited both mucosal and systemic anti-LPS antibody responses (33). Anti-LPS antibodies were primarily of the IgG1 subclass, but IgG2a anti-LPS was also elicited, suggesting that this immunization route and adjuvant activated both Th2 and Th1 responses. In those studies, we also demonstrated that immune serum contained high-titer cross-reacting antibodies with LPS prepared from B. abortus 2308. In the present report, we further demonstrate that the serum anti-LPS antibody response persists at a high plateau for at least 16 weeks after the second dose of vaccine (Table 1) and is still at one-fourth of its peak level at the 25-week mark.
This prolonged, high-titer response may partially reflect the unusually prolonged persistence of Brucella LPS on the surface of antigen-presenting cells (10), but it may also reflect a contribution of the GBOMP component of the vaccine. GBOMP increases expression of costimulatory molecules on murine B cells and enhances antibody responses to polysaccharide antigens by a CD40-CD40L-mediated mechanism (27). The pattern of antibody subclass expressed by mice immunized with GBOMP-LPS is also different from the pattern evoked by immunization of mice with B. abortus LPS or infection with B. abortus (8, 18, 22). Interestingly, Kurtz and Berman (18) found that immunization with B. abortus LPS containing 5 to 6% protein by weight led to production of IgG1 antibodies directed against the protein component and IgG3 antibodies directed against the LPS component, while immunization with B. abortus LPS containing <1% protein evoked primarily IgG3 directed against LPS determinants. To confirm that the predominantly IgG1 antibodies elicited in the present study were directed against OPS, we used highly purified(<0.1% protein) LPS from Y. enterocolitica O:9 as a target antigen in the ELISA. Caroff et al. (3) have shown that the structure of the O chain of the phenol-phase-soluble LPS of Y. enterocolitica O:9 is identical to the structure of B. abortus 1119-3 LPS O chain. The B. abortus structure consists of an unbranched linear homopolymer of 1,2-linked 4,6-dideoxy-4-formamido-α-d-mannopyranosyl residues. The O chain of the B. melitensis 16 M LPS used in the present study has 80% structural homology with the homopolymeric O chain of B. abortus LPS (2), 16 M LPS differs in that, on average, every fifth sugar residue is 1,3 linked rather than 1,2 linked. Our finding of similar patterns of IgG subclass antibodies directed against O:9 LPS and 16 M LPS confirms that our LPS-based ELISA detects anti-OPS antibodies and that the majority of those antibodies in immune sera from our immunized mice are IgG1. The reasons for this difference between our studies and those of Kurtz and Berman (18) are unknown, but they could involve (i) our use of the intranasal route of immunization, (ii) adjuvant effects of GBOMP, or (iii) our use of LPS from B. melitensis as an immunogen. The last possibility is particularly interesting, since Forestier et al. (10) have recently shown that B. abortus but not B. melitensis LPS associates with major histocompatibility complex class II molecules in B cells. We are addressing these possibilities in additional studies.
The present studies also demonstrate that intranasal immunization with LPS-GBOMP significantly protects mice from dissemination of infection to the spleen and liver when animals are challenged intranasally with 16 M. The degree of protection against dissemination after intranasal challenge in the present study was similar to that previously reported with a live, attenuated vaccine administered i.p. (13). It is likely that antibody plays a major role in this protection. The role of antibody in prevention of dissemination of B. abortus from murine footpads to liver and spleen has been well documented (24, 29). The lymph node barrier effect includes prevention of dissemination of brucellae from the popliteal lymph node to the liver and spleen and reduced numbers of organisms in the node and spleen (29). We have not observed a consistent reduction of CFU in those spleens to which bacteria disseminate in our B. melitensis intranasal challenge model, whether mice were immunized i.p. with a live, attenuated bacterial strain (13) or in the present study. Whether this inability of our vaccines to inhibit bacterial growth in the spleen reflects the route of challenge, use of B. melitensis rather than B. abortus, or a requirement for a more robust immune response is unknown. The mechanism of antibody-mediated protection against brucellosis is not well understood. Complement-mediated bacterial killing (4), antibody-dependent cytotoxicity by NK cells or macrophages, and phagocytosis and subsequent killing by activated macrophages (8, 17) are potential mechanisms of protection in which antibody might play a role.
In the present study, the intranasal LPS-GBOMP vaccine failed to reduce the initial number of bacteria in the lung and did not enhance clearance of bacteria from that organ. This failure occurred despite the presence of both IgG and IgA anti-LPS in BAL fluid at 4 weeks after the second dose of vaccine, when the mice were challenged. These results are in distinct contrast to those of our previous study using a live vaccine, in which a small effect on the intensity of lung infection occurred (13). This difference suggests that the cell-mediated immunity elicited by live vaccine may play a role in reduction of the intensity of infection in the lung. Although it does not affect clearance from the lung, the LPS-based vaccine described in the present report has several attractive features. Its ability to evoke a long-lasting anti-LPS serum antibody response and to protect mice from disseminated infection, the low toxicity of Brucella LPS (11), and the safety of GBOMP in human vaccine formulations (5) indicate that it may be useful for further study as a vaccine against human brucellosis. Vaccine modifications to elicit antibodies of different subclasses or greater avidity or addition of protein antigens to enhance cell-mediated immune responses may enhance efficacy and lead to inhibition of local, as well as disseminated, infection. We are examining these possibilities in additional studies.
Acknowledgments
We thank Lynnette Young, Adrien Ravizee, Hugh Wylie, and Peter Chen for their superb technical assistance in conducting these experiments.
Editor: R. N. Moore
REFERENCES
- 1.Bricker, B. J., D. R. Ewalt, A. P. MacMillan, G. Foster, and S. Brew. 2000. Molecular characterization of Brucella strains isolated from marine mammals. J. Clin. Microbiol. 38:1258-1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bundle, D. R., J. W. Cherwonogrodzky, and M. B. Perry. 1987. Structural elucidation of the Brucella melitensis antigen by high resolution NMR at 500 MHz. Biochemistry 26:8717-8726. [DOI] [PubMed] [Google Scholar]
- 3.Caroff, M., D. R. Bundle, and M. B. Perry. 1984. Structure of the O-chain of the phenol-phase soluble cellular lipopolysaccharide of Yersinia enterocolitica serotype O:9. Eur. J. Biochem. 139:195-200. [DOI] [PubMed] [Google Scholar]
- 4.Corbeil, L. B., K. Blau, T. J. Inzana, K. H. Nielsen, R. H. Jacobson, R. R. Corbeil, and A. J. Winter. 1988. Killing of Brucella abortus by bovine serum. Infect. Immun. 56:3251-3261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Drabick, J. J., B. L. Brandt, E. E. Moran, N. B. Saunders, D. R. Shoemaker, and W. D. Zollinger. 1999. Safety and immunogenicity testing of an intranasal group B meningococcal native outer membrane vesicle vaccine in healthy volunteers. Vaccine 18:160-172. [DOI] [PubMed] [Google Scholar]
- 6.Dubois, M., K. A. Gilles, J. K. Hamilton, P. A. Rebers, and F. Smith. 1956. Colorimetric method for determination of sugars and related substances. Anal. Chem. 28:350-356. [Google Scholar]
- 7.Dubray, G., and G. Bezard. 1980. Isolation of three Brucella abortus cell-wall antigens protective in murine experimental brucellosis. Ann. Rech. Vet. 11:367-373. [PubMed] [Google Scholar]
- 8.Elzer, P. H., R. H. Jacobson, S. M. Jones, K. H. Nielsen, J. T. Douglas, and A. J. Winter. 1994. Antibody-mediated protection against Brucella abortus in Balb/c mice at successive periods after infection: variation between virulent strain 2308 and attenuated vaccine strain 19. Immunology 82:651-658. [PMC free article] [PubMed] [Google Scholar]
- 9.Engvall, E., and P. Perlmann. 1972. Enzyme-linked immunosorbent assay. ELISA III. Quantitation of specific antibodies by enzyme-labeled anti-immunoglobulin in antigen-coated tubes. J. Immunol. 109:129-135. [PubMed] [Google Scholar]
- 10.Forestier, C., E. Moreno, S. Meresse, A. Phalipon, D. Olive, P. Sansonetti, and J. P. Gorvel. 1999. Interaction of Brucella abortus lipopolysaccharide with major histocompatibility complex class II molecules in B lymphocytes. Infect. Immun. 67:4048-4054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldstein, J., T. Hoffman, C. Frasch, E. F. Lizzio, P. R. Beining, D. Hochstein, Y. L. Lee, D. R. Angus, and B. Golding. 1992. Lipopolysaccharide (LPS) from Brucella abortus is less toxic than that from Escherichia coli, suggesting the possible use of B. abortus or LPS from B. abortus as a carrier in vaccines. Infect. Immun. 60:1385-1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grillo, M. J., N. Bosseray, and J. M. Blasco. 2000. In vitro markers and biological activity in mice of seed lot strains and commercial Brucella melitensis Rev 1 and Brucella abortus B19 vaccines. Biologicals 28:119-127. [DOI] [PubMed] [Google Scholar]
- 13.Hoover, D. L., R. M. Crawford, L. L. Van De Verg, M. J. Izadjoo, A. K. Bhattacharjee, C. M. Paranavitana, R. L. Warren, M. P. Nikolich, and T. L. Hadfield. 1999. Protection of mice against brucellosis by vaccination with Brucella melitensis WR201 (16M deltapurEK). Infect. Immun. 67:5877-5884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Izadjoo, M. J., Y. Polotsky, M. G. Mense, A. K. Bhattacharjee, C. M. Paranavitana, T. L. Hadfield, and D. L. Hoover. 2000. Impaired control of Brucella melitensis infection in Rag1-deficient mice. Infect. Immun. 68:5314-5320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jacques, I., V. Olivier-Bernardin, and G. Dubray. 1991. Induction of antibody and protective responses in mice by Brucella O-polysaccharide-BSA conjugate. Vaccine 9:896-900. [DOI] [PubMed] [Google Scholar]
- 16.Johnson, K. G., and M. B. Perry. 1976. Improved techniques for the preparation of bacterial lipopolysaccharides. Can. J. Microbiol. 22:29-34. [DOI] [PubMed] [Google Scholar]
- 17.Jones, S. M., and A. J. Winter. 1992. Survival of virulent and attenuated strains of Brucella abortus in normal and gamma interferon-activated murine peritoneal macrophages. Infect. Immun. 60:3011-3014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kurtz, R. S., and D. T. Berman. 1986. Influence of endotoxin-protein in immunoglobulin G isotype responses of mice to Brucella abortus lipopolysaccharide. Infect. Immun. 54:728-734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Memish, Z., M. W. Mah, S. Al Mahmoud, M. Al Shaalan, and M. Y. Khan. 2000. Brucella bacteremia: clinical and laboratory observations in 160 patients. J. Infect. 40:59-63. [DOI] [PubMed] [Google Scholar]
- 20.Mense, M. G., L. L. Van De Verg, A. K. Bhattacharjee, J. L. Ruckert, J. A. Hart, L. E. Lindler, T. L. Hadfield, and D. L. Hoover. 2000. Bacteriological and histopathological features of a mouse model for intranasal Brucella melitensis infection. Am. J. Vet. Res. 61:715-721. [Google Scholar]
- 21.Montaraz, J. A., and A. J. Winter. 1986. Comparison of living and non-living vaccines for Brucella abortus in Balb/c mice. Infect. Immun. 53:245-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moreno, E., R. S. Kurtz, and D. T. Berman. 1984. Induction of immune and adjuvant immunoglobulin G responses in mice by Brucella lipopolysaccharide. Infect. Immun. 46:74-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mousa, A. R., K. M. Elhag, M. Khogali, and A. A. Marafie. 1988. The nature of human brucellosis in Kwait: study of 379 cases. Rev. Infect. Dis. 10:211-217. [DOI] [PubMed] [Google Scholar]
- 24.Pardon, P. 1977. Resistance against a subcutaneous Brucella challenge of mice immunized with living or dead Brucella or by transfer of immune serum. Ann. Immunol. (Paris) 128:1025-1037. [PubMed] [Google Scholar]
- 25.Pardon, P., and J. Marly. 1976. Killed vaccine in adjuvant and protection of mice against an intraperitoneal challenge of Brucella: kinetic studies. Ann. Rech. Vet. 7:297-305. [PubMed] [Google Scholar]
- 26.Pardon, P., and J. Marly. 1976. Resistance of Brucella abortus infected mice to intravenous or intraperitoneal Brucella infection. Ann. Immunol. (Paris) 127:57-70. [PubMed] [Google Scholar]
- 27.Perez-Melgosa, M., H. D. Ochs, P. S. Linsley, J. D. Laman, M. van Meurs, R. A. Flavell, R. K. Ernst, S. I. Miller, and C. B. Wilson. 2001. Carrier-mediated enhancement of cognate T cell help: the basis for enhanced immunogenicity of meningococcal outer membrane protein polysaccharide conjugate vaccine. Eur. J. Immunol. 31:2373-2381. [DOI] [PubMed] [Google Scholar]
- 28.Phillips, M., B. L. Deyoe, and P. C. Canning. 1989. Protection of mice against Brucella abortus infection by inoculation with monoclonal antibodies recognizing Brucella O-antigen. Am. J. Vet. Res. 50:2158-2161. [PubMed] [Google Scholar]
- 29.Plommet, M., and A. M. Plommet. 1983. Immune serum-mediated effects on brucellosis evolution in mice. Infect. Immun. 41:97-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Plommet, M., and A. M. Plommet. 1989. Immunity to Brucella abortus induced in mice by popliteal lymph node restricted strain 19 vaccination. Ann. Rech. Vet. 20:73-81. [PubMed] [Google Scholar]
- 31.Pugh, G. J., L. B. Tabatabai, B. J. Bricker, J. E. Mayfield, M. Phillips, E. S. Zehr, and C. A. Belzer. 1990. Immunogenicity of Brucella-extracted and recombinant protein vaccines in CD-1 and BALB/c mice. Am. J. Vet. Res. 51:1413-1420. [PubMed] [Google Scholar]
- 32.Tabatabai, L. B., G. J. Pugh, M. G. Stevens, M. Phillips, and T. J. McDonald. 1992. Monophosphoryl lipid A-induced immune enhancement of Brucella abortus salt-extractable protein and lipopolysaccharide vaccines in BALB/c mice. Am. J. Vet. Res. 53:1900-1907. [PubMed] [Google Scholar]
- 33.Van De Verg, L. L., A. B. Hartman, A. K. Bhattacharjee, B. D. Tall, L. Yuan, K. Sasala, T. L. Hadfield, W. D. Zollinger, D. L. Hoover, and R. L. Warren. 1996. Outer membrane protein of Neisseria meningitidis as a mucosal adjuvant for lipopolysaccharide of Brucella melitensis in mouse and guinea pig intranasal immunization models. Infect. Immun. 64:5263-5268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Winter, A. J., G. E. Rowe, J. R. Duncan, M. J. Eis, J. Widom, B. Ganem, and B. Morein. 1988. Effectiveness of natural and synthetic complexes of porin and O-polysaccharide as vaccine against Brucella abortus in mice. Infect. Immun. 56:2808-2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Young, E. J. 1995. An overview of human brucellosis. Clin. Infect. Dis. 21:283-289. [DOI] [PubMed] [Google Scholar]
- 36.Zollinger, W. D., J. Boslego, E. Moran, B. Brandt, H. Collins, R. Mandrell, P. Altieri, and S. Berman. November 1987. Process for the preparation of detoxified polysaccharide-outer membrane protein complexes, and their use as antibacterial vaccines. U.S. patent 4,707,543.
- 37.Zollinger, W. D., R. E. Mandrell, J. M. Grifiss, P. Altieri, and S. Berman. 1979. Complex of meningococcal group B polysaccharide and type 2 outer membrane protein immunogenic in man. J. Clin. Investig. 63:836-848. [DOI] [PMC free article] [PubMed] [Google Scholar]