Abstract
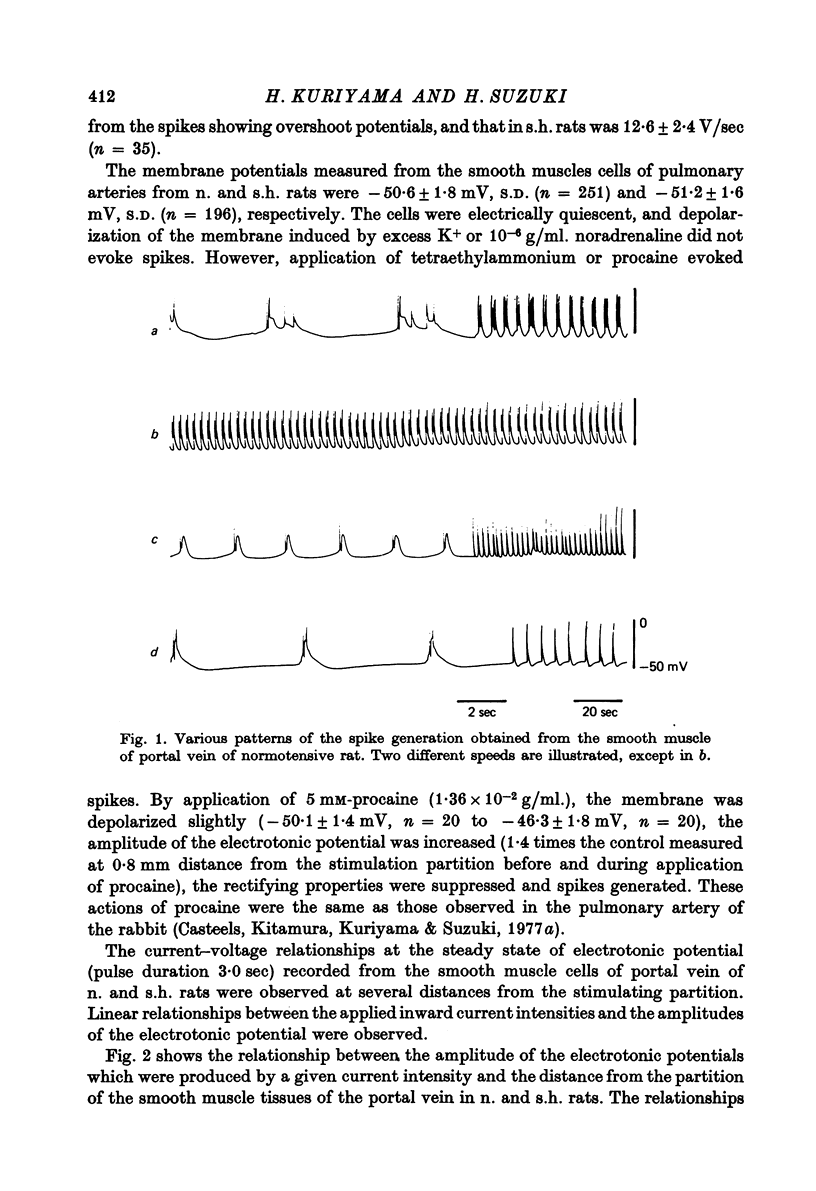
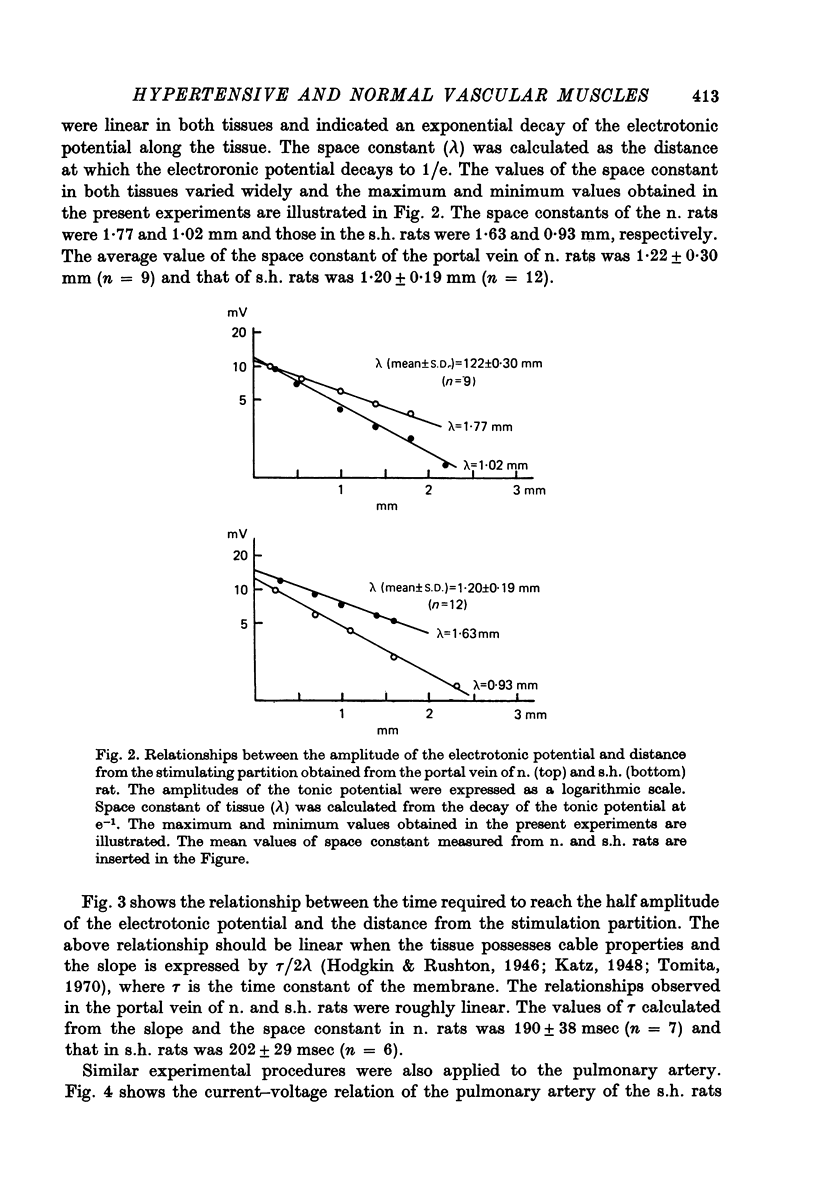
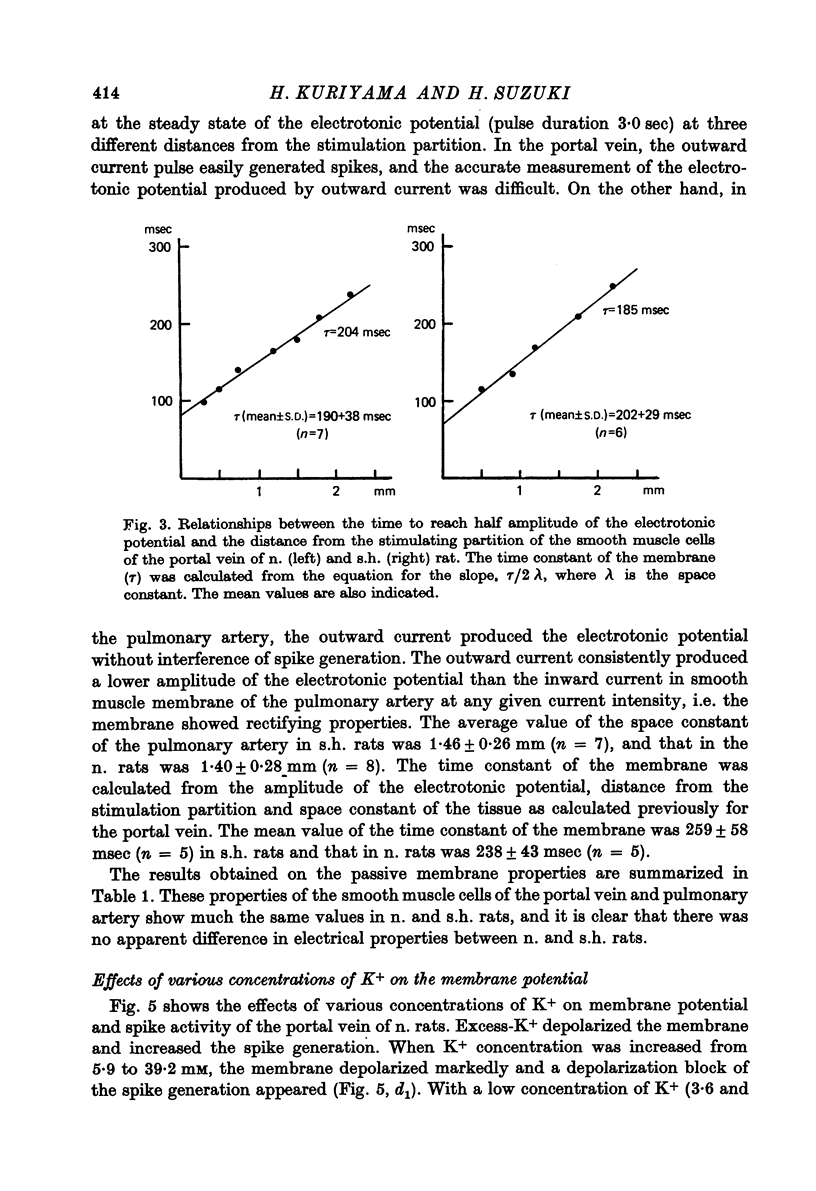
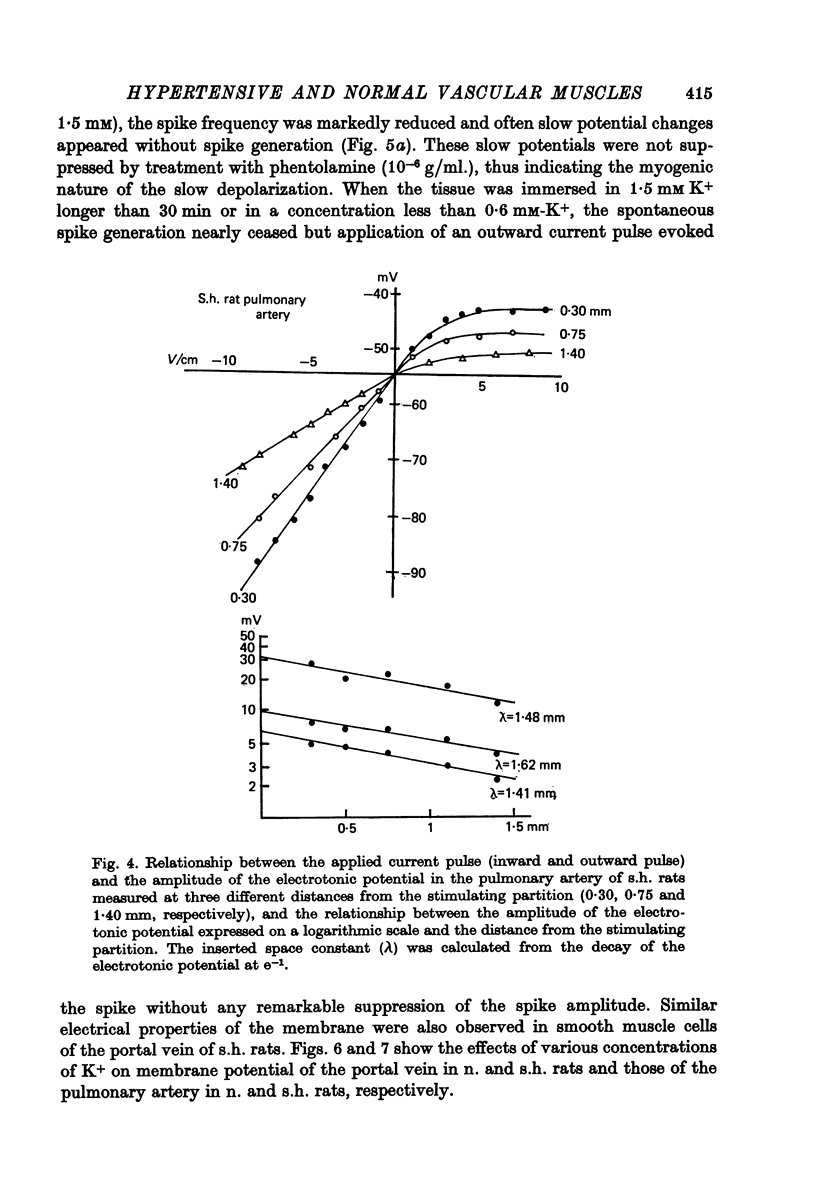
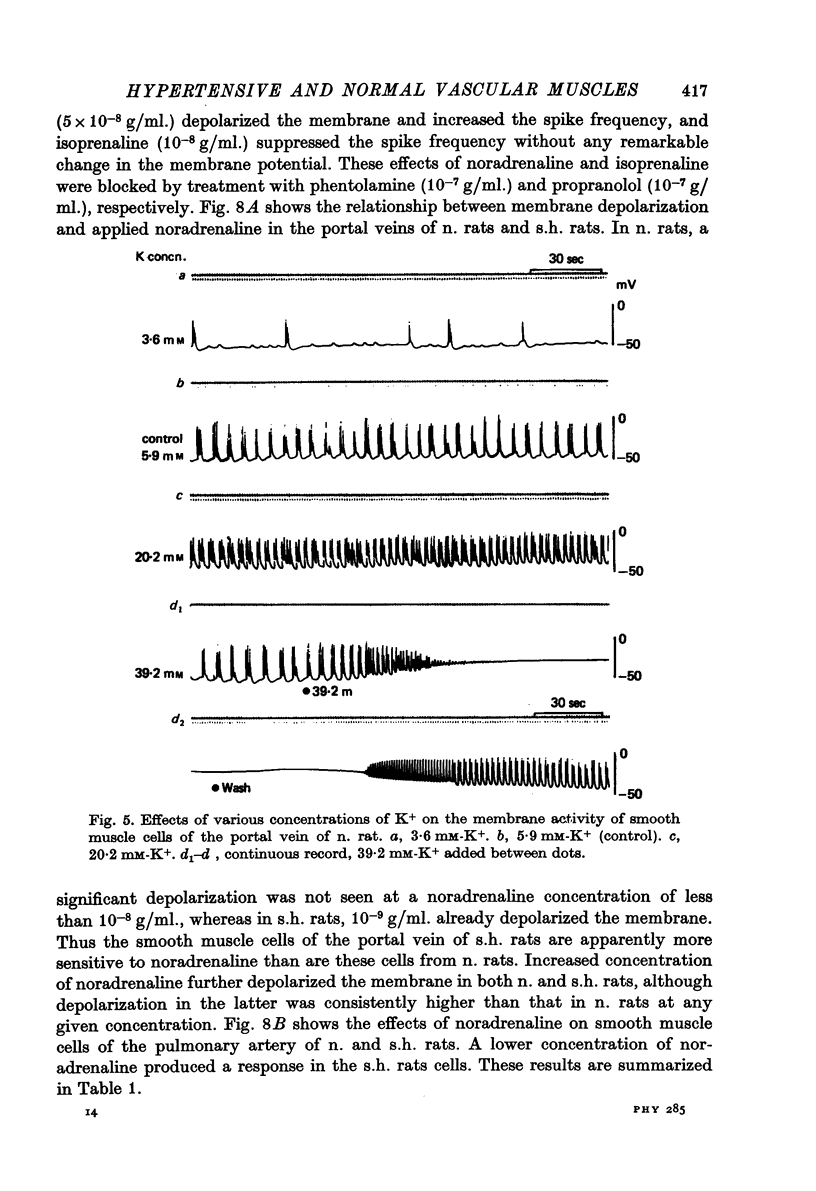
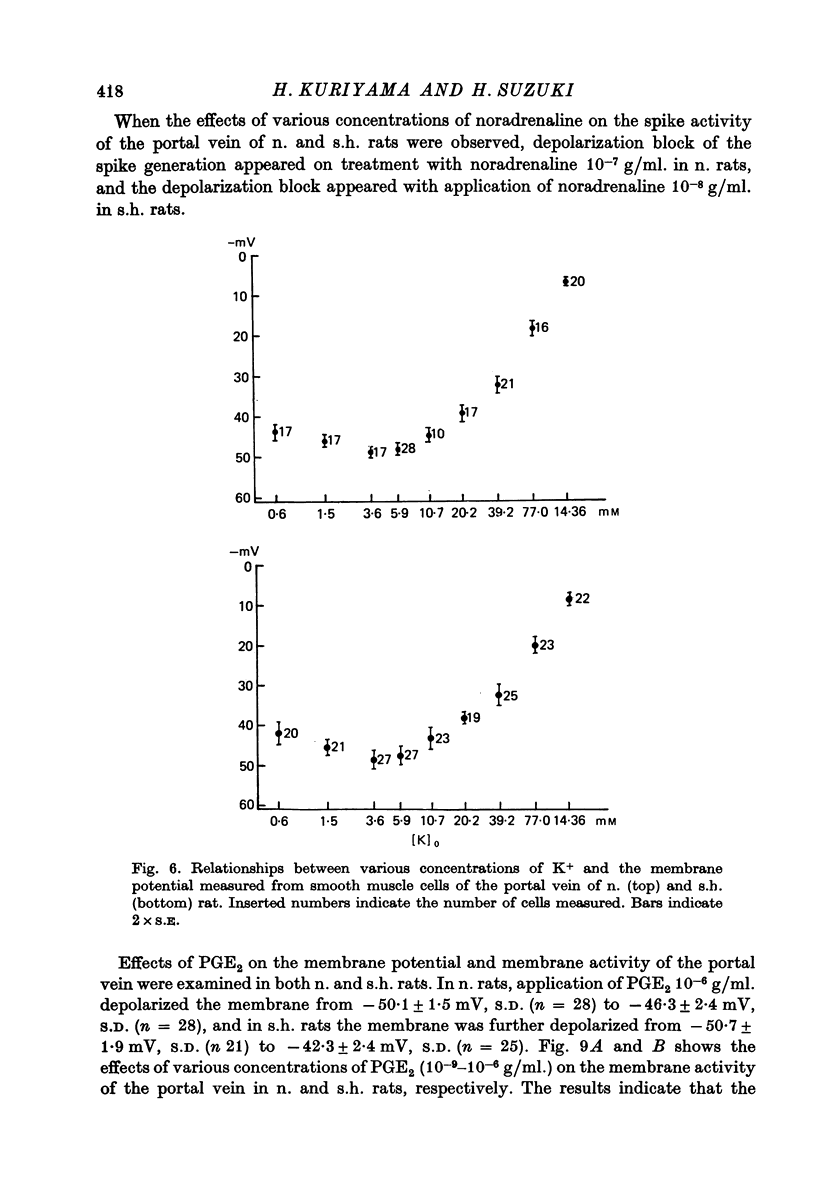
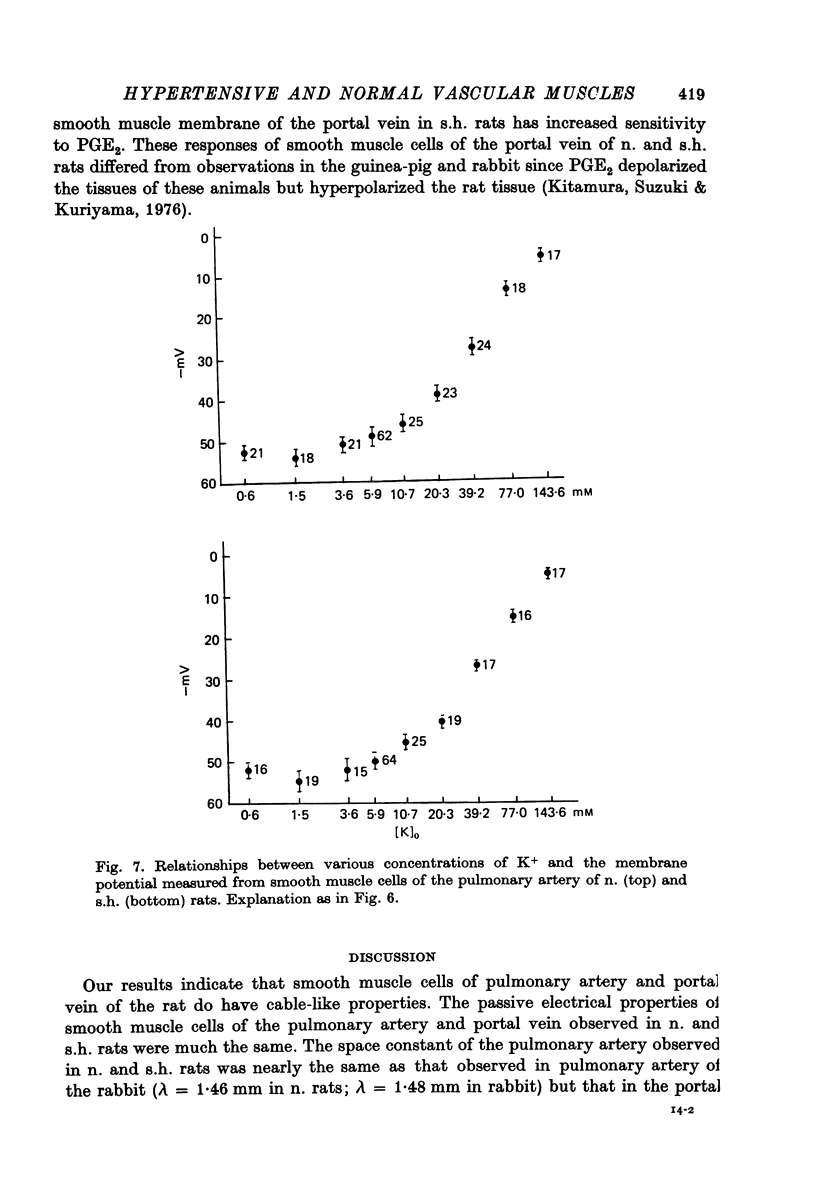
1. The membrane properties and sensitivity to chemical substances of smooth muscle cells of the portal vein and pulmonary artery were studied in normotensive rats (Wistar Kyoto) and spontaneously hypertensive rats (Okamoto & Aoki) by the micro-electrode method. 2. The parameters of the membrane, i.e. resting membrane potential, the maximum rate of rise of the spike, space constant of the tissue and time constant of the membrane measured from the portal vein were the same in normotensive rats (less than 120 mmHg) and spontaneously hypertensive rats (greater than 165 mmHg). Similar results were also obtained from the pulmonary artery. Such findings indicate that the passive electrical properties of the vascular muscle membrane are not involved in the generation mechanism of hypertension. 3. In the portal vein the maximum slope of the membrane depolarization produced by tenfold increase in external K+ concentration expressed on a logarithmic scale was the same in normal and hypertensive rats (42 and 41 mV, respectively). These observations were confirmed by the effects of application of excess K+ on the pulmonary artery (48 mV in normal and 46 mV in hypertension). With a low concentration of K+, the membrane was depolarized to a greater extent in the portal veins than in the pulmonary arteries of both types of rats. Although the response to K+ differed in vascular muscles excised from the different regions, no functional difference was apparent between normotensive and hypertensive. 4. In both portal vein and pulmonary artery, the smooth muscle membrane of spontaneously hypertensive rats proved to be more sensitive to noradrenaline, i.e. depolarization of the membrane appeared with noradrenaline 10(-9) g/ml. in hypertensive but with 10(-8)g/ml. in normotensive rats. Depolarization block of the spike generation appeared at a slower concentration of noradrenaline in hypertensive rats. Sensitivity of the smooth muscle membrane to prostaglandin E2 in the portal vein was also higher in hypertensive rats. 5. The present results indicate that the only difference between normal and spontaneously hypertensive rats regarding smooth muscle cell membrane of the pulmonary artery and portal vein is increased chemical sensitivity in hypertensive rats, and the passive electrical properties of the membrane probably does not contribute to the generation of hypertension.
Full text
PDF
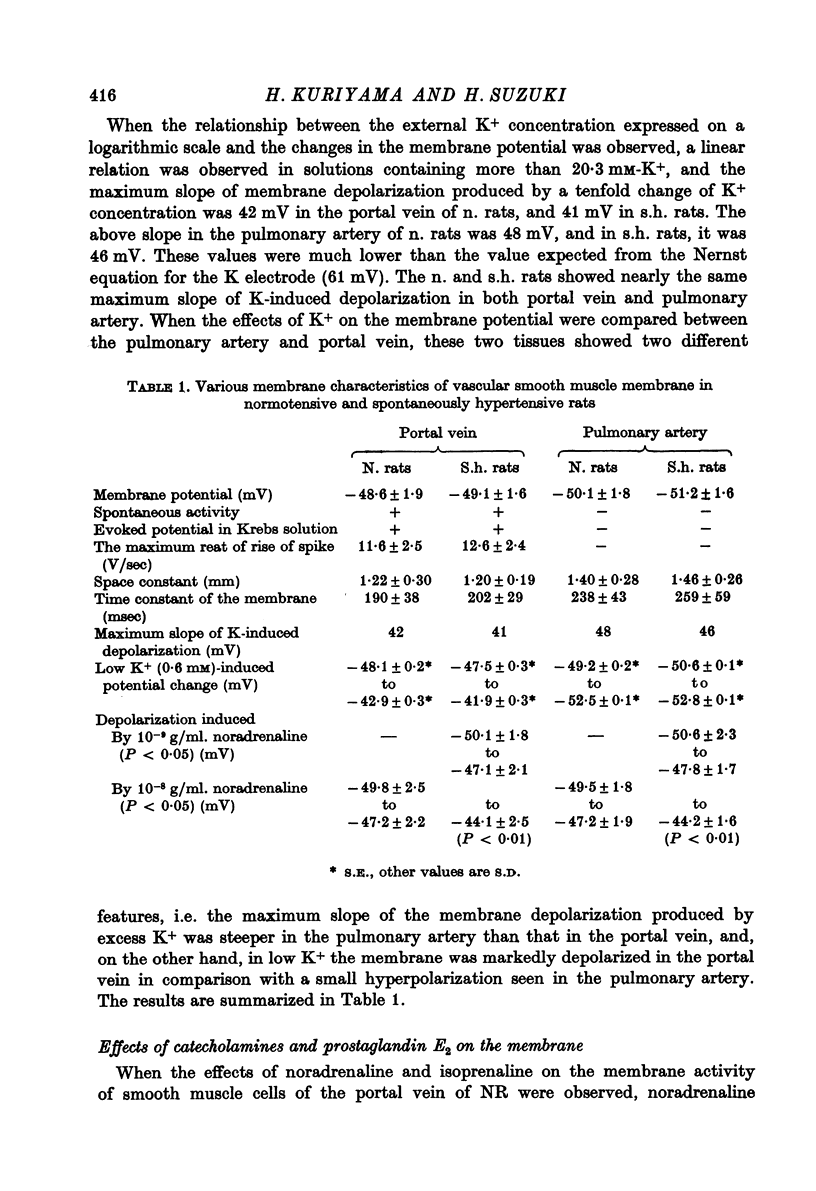
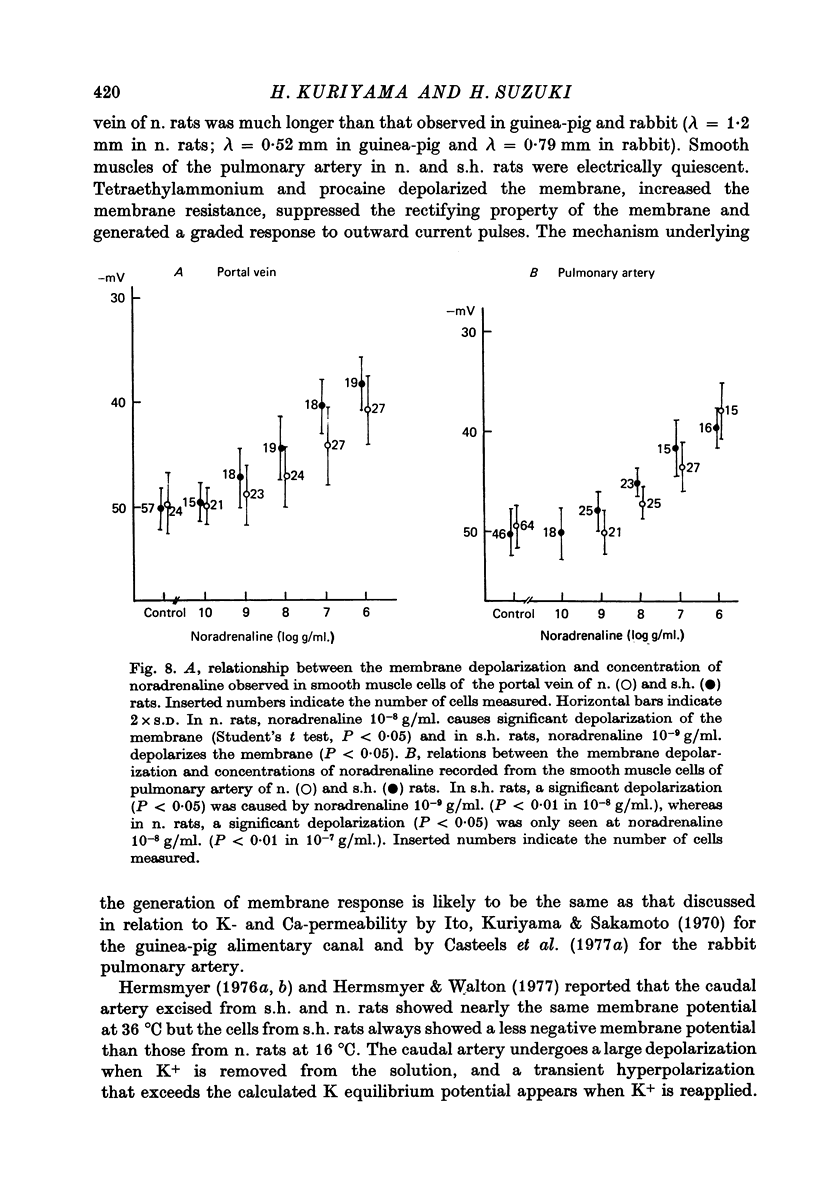
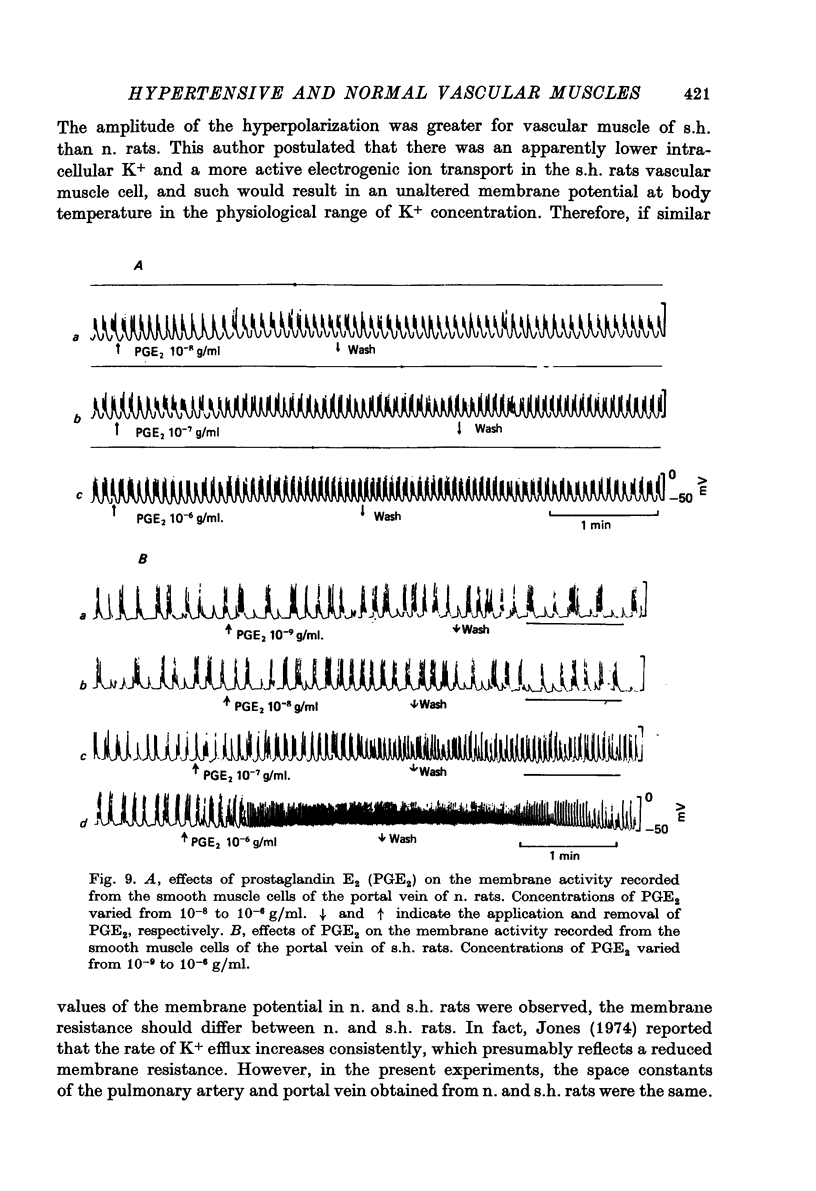
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abe Y., Tomita T. Cable properties of smooth muscle. J Physiol. 1968 May;196(1):87–100. doi: 10.1113/jphysiol.1968.sp008496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohr D. F. Reactivity of vascular smooth muscle from normal and hypertensive rats: effect of several cations. Fed Proc. 1974 Feb;33(2):127–132. [PubMed] [Google Scholar]
- Casteels R., Kitamura K., Kuriyama H., Suzuki H. Excitation-contraction coupling in the smooth muscle cells of the rabbit main pulmonary artery. J Physiol. 1977 Sep;271(1):63–79. doi: 10.1113/jphysiol.1977.sp011990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casteels R., Kitamura K., Kuriyama H., Suzuki H. The membrane properties of the smooth muscle cells of the rabbit main pulmonary artery. J Physiol. 1977 Sep;271(1):41–61. doi: 10.1113/jphysiol.1977.sp011989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkow B. The haemodynamic consequences of adaptive structural changes of the resistance vessels in hypertension. Clin Sci. 1971 Jul;41(1):1–12. doi: 10.1042/cs0410001. [DOI] [PubMed] [Google Scholar]
- Grobecker G., Roizen M. F., Weise V., Saavedra J. M., Kopin I. J. Letter: Sympathoadrenal medullary activity in young, spontaneously hypertensive rats. Nature. 1975 Nov 20;258(5532):267–268. doi: 10.1038/258267a0. [DOI] [PubMed] [Google Scholar]
- Hermsmeyer K. Electrogenesis of increased norepinephrine sensitivity of arterial vascular muscle in hypertension. Circ Res. 1976 May;38(5):362–367. doi: 10.1161/01.res.38.5.362. [DOI] [PubMed] [Google Scholar]
- Ito Y., Kuriyama H., Sakamoto Y. Effects of tetraethylammonium chloride on the membrane activity of guinea-pig stomach smooth muscle. J Physiol. 1970 Dec;211(2):445–460. doi: 10.1113/jphysiol.1970.sp009286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones A. W. Altered ion transport in vascular smooth muscle from spontaneously hypertensive rats. Influences of aldosterone, norepinephrine, and angiotensin. Circ Res. 1973 Nov;33(5):563–572. doi: 10.1161/01.res.33.5.563. [DOI] [PubMed] [Google Scholar]
- Kitamura K., Suzuki H., Kuriyama H. Prostaglandin action on the main pulmonary artery and portal vein of the rabbit. Jpn J Physiol. 1976;26(6):681–692. doi: 10.2170/jjphysiol.26.681. [DOI] [PubMed] [Google Scholar]
- Kuriyama H., Oshima K., Sakamoto Y. The membrane properties of the smooth muscle of the guinea-pig portal vein in isotonic and hypertonic solutions. J Physiol. 1971 Aug;217(1):179–199. doi: 10.1113/jphysiol.1971.sp009565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lais L. T., Brody M. J. Mechanism of vascular hyperresponsiveness in the spontaneously hypertensive rat. Circ Res. 1975 Jun;36(6 Suppl 1):216–222. doi: 10.1161/01.res.36.6.216. [DOI] [PubMed] [Google Scholar]
- Nagatsu T., Kato T., Numata Y., Ikuta K., Kuzuya H. Dopamine beta-hydroxylase and tyrosine hydroxylase activities in spontaneously hypertensive rats after NaCl administration. Experientia. 1975 Jul 15;31(7):767–768. doi: 10.1007/BF01938451. [DOI] [PubMed] [Google Scholar]
- Nakamura K., Nakamura K. Selective activation of sympathetic ganglia in young spontaneously hypertensive rats. Nature. 1977 Mar 17;266(5599):265–266. doi: 10.1038/266265a0. [DOI] [PubMed] [Google Scholar]
- OKAMOTO K., AOKI K. Development of a strain of spontaneously hypertensive rats. Jpn Circ J. 1963 Mar;27:282–293. doi: 10.1253/jcj.27.282. [DOI] [PubMed] [Google Scholar]
- Okamoto K., Nosaka S., Yamori Y., Matsumoto M. Participation of neural factor in the pathogenesis of hypertension in the spontaneously hypertensive rat. Jpn Heart J. 1967 Mar;8(2):168–180. doi: 10.1536/ihj.8.168. [DOI] [PubMed] [Google Scholar]
- Ooshima A. Enzymological studies on arteries in spontaneously hypertensive rats. Jpn Circ J. 1973 May;37(5):497–508. doi: 10.1253/jcj.37.497. [DOI] [PubMed] [Google Scholar]
- Shibata S., Kurahashi K., Kuchii M. A possible etiology of contractility impairment of vascular smooth muscle from spontaneously hypertensive rats. J Pharmacol Exp Ther. 1973 May;185(2):406–417. [PubMed] [Google Scholar]
- Somlyo A. P., Somlyo A. V. Vascular smooth muscle. II. Pharmacology of normal and hypotensive vessels. Pharmacol Rev. 1970 Jun;22(2):249–353. [PubMed] [Google Scholar]
- Spector S., Fleisch J. H., Maling H. M., Brodie B. B. Vascular smooth muscle reactivity in normotensive and hypertensive rats. Science. 1969 Dec 5;166(3910):1300–1301. doi: 10.1126/science.166.3910.1300. [DOI] [PubMed] [Google Scholar]
- Webb R. C., Bhalla R. C. Altered calcium sequestration by subcellular fractions of vascular smooth muscle from spontaneously hypertensive rats. J Mol Cell Cardiol. 1976 Aug;8(8):651–661. doi: 10.1016/0022-2828(76)90050-x. [DOI] [PubMed] [Google Scholar]
- Wei J. W., Janis R. A., Daniel E. E. Calcium accumulation and enzymatic activities of subcellular fractions from aortas and ventricles of genetically hypertensive rats. Circ Res. 1976 Jul;39(1):133–140. doi: 10.1161/01.res.39.1.133. [DOI] [PubMed] [Google Scholar]
- Wei J. W., Janis R. A., Daniel E. E. Relationship between blood pressure of spontaneously hypertensive rats and alterations in membrane properties of mesenteric arteries. Circ Res. 1977 Mar;40(3):299–305. doi: 10.1161/01.res.40.3.299. [DOI] [PubMed] [Google Scholar]


