In the presence of infection (and its treatment), anticoagulant therapy can go dangerously out of control.
CASE HISTORY
A woman aged 62 attended casualty because the vision in her only eye had suddenly deteriorated after a paroxysm of coughing. She gave a history of aortic and mitral valve replacements for rheumatic heart disease, and was taking warfarin with the aim of keeping the international normalized ratio (INR) between 2.5 and 3.5. A week before presentation she had begun a course of clarithromycin 250 mg twice daily for a chest infection. She had a complex ophthalmic history with bilateral cataract extraction in childhood and bilateral retinal detachment surgery at age 21. The left detachment repair had been successful with restoration of acuity to 6/18, but the right eye had become phthisical (blind and shrunken).
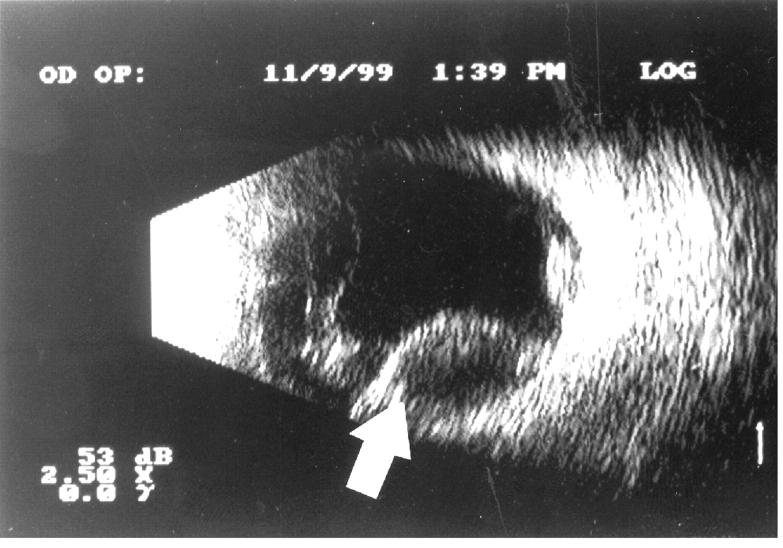
On examination she was pyrexial with signs of a resolving chest infection. There was a left hyphaema in the anterior chamber. The fundus could not be examined because of vitreous opacity. Ocular ultrasonography revealed a dense vitreous and suprachoroidal haemorrhage (Figure 1). Her INR was 8.2. Subsequent examination of the general practitioner's records showed an INR of 2.3 three days before clarithromycin and 2.9 three days into the course. The highest INR in the past four months had been 3.7.
Figure 1.
Ocular ultrasound scan showing suprachoroidal haemorrhage
The clarithromycin was stopped, the warfarin dose was adjusted and she was given 0.5 mg intravenous vitamin K. The chest infection cleared three days after admission. A vitrectomy with anterior chamber washout and partial drainage of the suprachoroidal haemorrhage was performed when her INR had fallen to 2.9. Unfortunately this did not improve her vision, which had now deteriorated to perception of light only.
COMMENT
A possible reason for the loss of anticoagulant control in this patient was the infection itself. However, we suspect that the cause was an interaction between clarithromycin and warfarin. This has been recorded in four previous case reports1,2,3. One described the interaction between clarithromycin, warfarin and digoxin in a woman with chronic atrial fibrillation1. Her INR at presentation was 7.3. She had gastrointestinal symptoms, weakness, dizziness and visual changes, but no permanent systemic or visual complications ensued. In the other three cases the INR rose to between 5.6 and >20 after taking clarithromycin and warfarin but no systemic symptoms developed2,3. Any of these patients could have suffered an intracerebral or other life-threatening bleed with an elevated INR.
The most common ocular haemorrhagic complication of warfarin is subconjunctival haemorrhage; a rarer one is spontaneous hyphaema. These almost always resolve without sequelae4. Suprachoroidal haemorrhage usually arises from intraocular surgery or trauma5; we are not aware of any previous cases resulting from drug interaction with warfarin.
Antibiotic therapy in the preceeding four weeks is one of the major risk factors for a rise in INR to above 7 (at which point the risk of bleeding increases substantially6,7), in patients taking warfarin. Clarithromycin is thought to interact with warfarin through inhibition of the cytochrome p450 drug metabolizing system7. Cephalosporins inhibit vitamin K metabolism. Sulphonamides eliminate bacterial flora with consequent vitamin K deficiency. Ciprofloxacin and tetracyclines potentiate warfarin through unknown mechanisms8.
References
- 1.Gooderham MJ, Bolli P, Fernandez PG. Concomitant digoxin toxicity and warfarin interaction in a patient receiving clarithromycin. Ann Pharmacother 1999;33: 796-9 [DOI] [PubMed] [Google Scholar]
- 2.Recker MW, Kier KL. Potential interaction between clarithromycin and warfarin. Ann Pharmacother 1997;31: 996-8 [DOI] [PubMed] [Google Scholar]
- 3.Oberg KC. Delayed elevation of international normalized ratio with concurrent clarithromycin and warfarin therapy. Pharmacotherapy 1998;18: 386-91 [PubMed] [Google Scholar]
- 4.Holden R. Spontaneous hyphaema as a result of systemic anticoagulation in previously abnormal eyes. Postgrad Med J 1991; 67: 1008-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chu TG, Green RI. Suprachoroidal haemorrhage. Surv Ophthalmol 1999; 43: 471-86 [DOI] [PubMed] [Google Scholar]
- 6.Palareti G, Leali N, Coccheri S, et al. Bleeding complications of oral anticoagulant treatment: an inception-cohort, prospective collaborative study (ISCOAT). Lancet 1996;348: 423-8 [DOI] [PubMed] [Google Scholar]
- 7.Panneerselvam S, Baglin C, Lefort W, Baglin T. Analysis of risk factors for over-anticoagulation in patients receiving long-term warfarin. Br J Haematol 1998;103: 422-4 [DOI] [PubMed] [Google Scholar]
- 8.Munckhof WJ. Concurrent prescribing. Beware of drug interactions. Aust Fam Physician 1998;27: 895-901 [PubMed] [Google Scholar]