The most important causes of spontaneous intracranial extradural haematoma are coagulation disorders, dural vascular malformations and infection1. An association with frontal sinusitis has been reported on a few occasions.
CASE HISTORY
A man aged 17 had frontal headaches for three days. He attended the emergency department and was found to be neurologically normal. Oral temperature was 37.7°C and frontal tenderness was elicited on palpation. White cell count was 7.7 × 109/L (normal 4.0-11.0), erythrocyte sedimentation rate was 44 mm/h (2-8) and coagulation screen was normal. Frontal sinusitis was diagnosed, oral amoxycillin was prescribed and he was discharged home. Three days later he was admitted to hospital after a sudden exacerbation of the headache associated with nausea and vomiting. There was no history of head injury. He remained neurologically normal. A non-enhanced computed tomogram showed a right frontal extradural haematoma (Figure 1) which was then evacuated via a frontal craniotomy. No pus was seen and there was no apparent bony or dural abnormality. Histological examination showed a blood clot containing clusters of polymorphonuclear cells. No organisms were seen on Gram staining and culture yielded no growth. The patient received a two-week course of intravenous cefotaxime and metronidazole and recovered fully. Three months later he was symptomfree and a computed tomogram showed no recurrence of the haematoma.
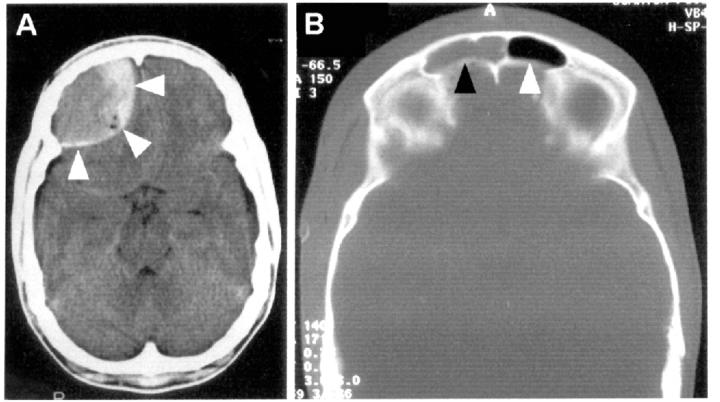
Figure 1.
Preoperative, non-enhanced, axial computed tomograms of the brain. (A) Right frontal extradural haematoma (arrows). (B) Mucosal thickening/fluid in the right (black arrow) but not the left (white arrow) frontal air sinus, consistent with right frontal sinusitis
COMMENT
Only eight cases1,2,3,4,5,6,7 of spontaneous intracranial extradural haematoma complicating infection have been recorded to date. Four patients had chronic otitis2,4,5,7, three had frontal sinusitis3,4,6 and one had orbital cellulitis7. Seven of these cases2,3,4,5,6,7 were diagnosed before the availability of computed tomography. A causal relation between infection and extradural haematoma is supported by the fact that, as in the present case, the extradural haematoma was always adjacent to the infected region.
We hypothesize that the extradural haematoma was caused by spread of inflammation beyond the confines of the sinus. This may explain the presence of clusters of neutrophils in the haematoma of our patient. The hypothesis is also supported by histological and radiological evidence of inflammation in contiguous bone and dura in patients with sinusitis7. Once the dural vessels adjacent to the infected region become inflamed, the vessel walls may weaken and the vessels may become prone to bleeding even after subclinical trauma. Progressive detachment of the dura from the inner table of the skull may also be facilitated by the accumulation in the extradural space of a sympathetic effusion, or of air through a bony defect3.
When headache develops in a patient with sinusitis, otitis or facial cellulitis, brain abscess and subdural or extradural empyema should be considered. We suggest that a sudden-onset headache in these patients might also indicate a spontaneous extradural haematoma. Computed tomography of the brain should be performed urgently: deterioration in the patient's level of consciousness reflects delay in establishing the diagnosis. Prompt evacuation of the haematoma and a course of antibiotics should lead to complete recovery.
References
- 1.Sanchis JF, Orozco M, Cabanes J. Spontaneous extradural haematomas. J Neurol Neurosurg Psychiatry 1975;38: 577-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clein LJ. Extradural haematoma associated with middle ear infection. Can Med Assoc J 1970;102: 1183-4 [PMC free article] [PubMed] [Google Scholar]
- 3.Kelly DL Jr, Smith JM. Epidural hematoma secondary to frontal sinusitis. Case report. J Neurosurg 1968;28: 67-9 [DOI] [PubMed] [Google Scholar]
- 4.Marks SM, Shaw MDM. Spontaneous intracranial extradural hematoma. J Neurosurg 1982;57: 708-9 [DOI] [PubMed] [Google Scholar]
- 5.Novaes V, Gorbitz C. Extradural hematoma complicating middle ear infection. Report of a case. J Neurosurg 1965;23: 352-3 [DOI] [PubMed] [Google Scholar]
- 6.Rajput AL, Rozdilsky B. Extradural hematoma following frontal sinusitis. Arch Otolaryngol 1971;94: 83-6 [DOI] [PubMed] [Google Scholar]
- 7.Schneider RC, Hegarty WM. Extradural hemorrhage as a complication of otological and rhinological infections. Ann Otol Rhinol Laryngol 1951;60: 197-206 [DOI] [PubMed] [Google Scholar]