Abstract
Using Benjamin’s (2000) Structural Analysis of Social Behavior, we evaluated change in "self-directed" affiliation and autonomy and prediction of treatment response and relapse/recurrence among adult outpatients with recurrent major depressive disorder consenting to acute phase cognitive therapy (A–CT; Beck, Rush, Shaw, & Emery, 1979; N = 156); A–CT responders randomized (N = 84) to 8 months of continuation phase cognitive therapy (C–CT; Jarrett, 1989; Jarrett et al., 1998; Jarrett & Kraft, 1997) or assessment-only control; and C–CT and control patients entering a 16-month, assessment-only follow-up (N = 74). Self-directed affiliation and autonomy increased after A–CT, and C–CT further increased affiliation and autonomy. Affiliation and autonomy did not predict A–CT response, but lower affiliation and higher autonomy pre-A–CT predicted relapse/recurrence post-A–CT. We discuss potential clinical implications of these results and present case examples to illustrate patterns of change.
Benjamin’s (1974, 1996, 2000) Structural Analysis of Social Behavior (SASB) provides a framework for psychological assessment highly relevant to psychotherapy process and outcome. As reviewed following, psychotherapy research using the "self-directed" domain of the SASB (the "introject") has focused on acute treatment with brief psychodynamic and experiential therapies. In this article, we extend the literature by evaluating self-directed SASB ratings in both acute phase cognitive therapy (A–CT; Beck, Rush, Shaw, & Emery, 1979), which aims to reduce depressive symptoms, and in continuation phase cognitive therapy (C–CT; Jarrett, 1989; Jarrett et al., 1998; Jarrett & Kraft, 1997), which aims to prevent relapse, using a unique clinical trial data set (Jarrett et al., 2001). The flexible SASB model allows for measurement of many different domains (e.g., thought, behavior, and emotion directed toward and in reaction to others such as parents and friends), and we focus on the self-directed domain in this article because it aligns conceptually with cognitive therapy’s focus on internal behaviors (e.g., Beck et al., 1979; Hollon & Beck, 2004; Ingram, 2003). We developed and tested hypotheses regarding change in the self-directed domain during treatment with cognitive therapy as well as prediction of treatment response and relapse/recurrence of depression posttreatment.
The self-directed domain of the SASB assesses behavior, thought, and emotion in relation to the self (Benjamin, 1974, 1996, 2000). Benjamin (1974, 1994) has hypothesized that the self-directed domain reflects "internalized" caregiver behavior, especially treatment by one’s parents during childhood. For example, demanding and critical treatment by parents in childhood might be paralleled by perfectionistic and self-critical behavior in adulthood. Limited support for this introject hypothesis has come from studies demonstrating that patients’ ratings of self-directed behavior and of therapists’ behavior toward them become more closely aligned after treatment, which is consistent with patients internalizing therapists’ behavior (Harrist, Quintana, Strupp, & Henry, 1994; Quintana & Meara, 1990). Moreover, self-reports of the SASB self-directed domain have often paralleled concurrent self-reports of treatment as a child by one’s mother (Benjamin, 1994; Benjamin & Pugh, 2001; Gurtman, 2001). Finally, affiliation was found to be higher among college students with self-reported secure, compared to fearful and preoccupied, parental attachments, although autonomy did not differ by attachment style (Pincus, Dickinson, Schut, Castonguay, & Bedics, 1999).
The self-directed domain of the SASB is usually assessed with self-report measures (Benjamin, 2000). From these measures, the self-directed domain may be partitioned into eight interrelated "clusters," described in Table 1. For example, the self-love cluster includes thought, behavior, and emotion reflecting soothing, entertaining, cherishing, seeking the best for, and nurturing oneself; whereas the self-blame cluster involves punishing, deceiving, criticizing, and doubting oneself. Scores on all eight clusters may be used to summarize a person’s functioning in the self-directed domain. However, a more efficient summary references self-directed affiliation (e.g., being pleased with and kind to vs. angry with and punishing of oneself) and autonomy (e.g., being spontaneous with and freeing of vs. restricting and controlling of oneself), two orthogonal dimensions that underlie the eight clusters and represent their factor structure (e.g., Lorr & Strack, 1999).
TABLE 1.
SASB Self-Directed ("Introject") Clusters
|
Theoretical Correlation of Cluster With Underlying Dimensions |
|||
|---|---|---|---|
| Cluster | Possible Clinical Description of High Scorers | Affiliation | Autonomy |
| Self-Love | Enjoys, cherishes, and nurtures self | + + | 0 |
| Self-Affirm | Well integrated, understands and accepts self | + | + |
| Self-Emancipate | Confident, free spirited, drifts with the moment | 0 | + + |
| Self-Neglect | A dreamer, neglects own potential, reckless | – | + |
| Self-Attack | Rejects own needs, self-destructive, overburdens self | – – | 0 |
| Self-Blame | Feels guilty, self-doubting and effacing | – | – |
| Self-Control | Restrained, proper, lives forced "ideal" identity | 0 | – – |
| Self-Protect | Self-analytical, works to improve self, takes care of self | + | – |
Note. Descriptions based on relevant SASB Intrex long-form questionnaire items (Benjamin, 2000). SASB=Structural Analysis of Social Behavior; ++=strong positive correlation; + = moderate positive correlation; 0 = zero correlation; - = moderate negative correlation; - - = strong negative correlation.
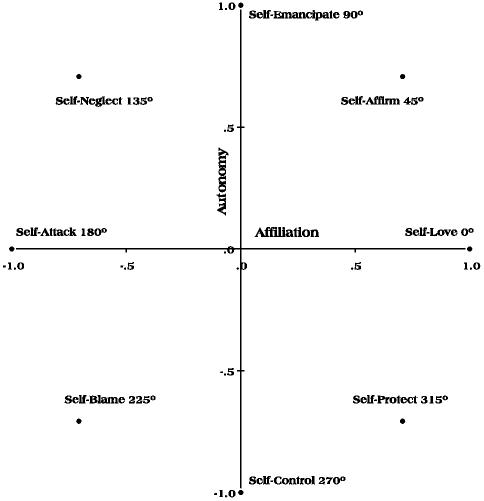
The eight clusters have different levels of association with the self-directed affiliation and autonomy dimensions, ranging from highly negative to highly positive correlations including correlations of zero (see Table 1). Using these correlations as Cartesian coordinates, the eight clusters may be plotted in a two-dimensional space with affiliation and autonomy as axes (see Figure 1). This two-dimensional, circular arrangement of clusters is often referred to as a "circumplex," and psychometric research suggests that SASB self-directed ratings typically approximate circumplex structure (e.g., Benjamin, 1994; Lorr & Strack, 1999; Pincus, Gurtman, & Ruiz, 1998). Persons’ scores on the eight clusters may be weighted by their relative associations with affiliation and autonomy and summed to derive affiliation and autonomy scores. Given circumplex structure, knowing that a patient scored high on the affiliation dimension and low on autonomy dimension, for example, we would expect the patient’s self-directed thought, behavior, and emotion to be characterized primarily by the self-protect cluster (i.e., at 315° in Figure 1) and relatively little by the self-neglect cluster (135°). In this manner, scores on the affiliation and autonomy dimensions offer a parsimonious summary of the self-directed domain.
FIGURE 1.
Theoretical circumplex structure of the self-directed domain of the Structural Analysis of Social Behavior. Eight "cluster" scales (in italics) mark equal increments (i.e., every 45°) around a two-dimensional circular space. The arrangement of clusters reflects their correlations with underlying affiliation and autonomy dimensions (in bold).
In the self-directed domain, high affiliation broadly represents psychological health (e.g., self-affirming, loving, and protecting; Henry, 1994). Conversely, psychiatric patients with a wide variety of diagnoses, such as major depressive disorder (Benjamin, 1986, 1994), bulimia nervosa (Wonderlich, Klein, & Council, 1996), dissociative disorders (Alpher, 1996), borderline personality disorder (Benjamin & Wonderlich, 1994), and alcoholism (Ichiyama, Zucker, Fitzgerald, & Bingham, 1996), often report low affiliation and so may be described as self-neglecting, blaming, or even attacking (e.g., suicidal). Self-directed autonomy may less clearly separate normal from abnormal functioning but instead partly differentiate diagnostic groups. For example, patients with relatively higher autonomy (e.g., self-neglecting) appear to include those with borderline (Benjamin & Wonderlich, 1994) and antisocial personality disorders (Benjamin, 1992) and alcoholism (Ichiyama et al., 1996), whereas patients with depression and anxiety may have relatively lower autonomy (e.g., self-blaming; Benjamin, 1986, 1994).
Assessment of the self-directed domain may be useful in tracking patient improvement during psychotherapy (Henry, 1996). For example, Paivio and Greenberg (1995) found that in outpatients (N = 34; selected for interpersonal problems and clinically judged appropriateness for psychotherapy), affiliation improved more after 3 months of experiential therapy than of psychoeducation (a control condition). In the experiential therapy group, treatment gains were maintained at a 4 month follow-up but were no longer significant at a 1-year follow-up. Moreover, in a partly overlapping sample of outpatients (N = 33; Paivio & Bahr, 1998), higher pretreatment affiliation predicted a stronger patient–therapist bond during treatment. Finally, Junkert-Tress, Schnierda, Hartkamp, Schmitz, and Tress (2001) found that affiliation improved from before to after time limited psychodynamic therapy administered to outpatients (N = 75; with personality, somatoform, or neurotic disorders of mild to moderate severity). The degree of improvement in affiliation was similar to that in measures of general symptom severity. These studies have suggested that self-directed affiliation tracks improvements in acute experiential and psychodynamic therapies. The utility of the self-directed domain could be understood better through research with different types of psychotherapy (e.g., cognitive therapy), both acute and continuation phase treatments, and evaluation of the ability of the self-directed domain to predict as well as track treatment outcomes. In this article, we offer initial data in these areas.
The controlled randomized clinical trial data set (Jarrett et al., 2001) used for these analyses included 156 adult outpatients with recurrent major depressive disorder consenting to a 20-session A–CT protocol. Consenting A–CT responders (N = 84) were randomized to 8 months of C–CT or assessment-only control. Both groups then entered a 16-month assessment-only follow-up, yielding a total of 2 years post-A–CT follow-up. This data structure allowed us to test several hypotheses regarding the SASB self-directed domain. First, we hypothesized that affiliation would increase from before to after A–CT, consistent with findings for other psychotherapies. Second, we hypothesized that higher affiliation as a marker of psychological health would predict A–CT response. Third, we hypothesized that C–CT, compared to assessment only, would produce higher affiliation. Fourth, we hypothesized that higher affiliation would predict longer survival from relapse and recurrence of major depressive disorder post-A–CT. We also planned analyses parallel to Hypotheses 1 through 4 for self-directed autonomy but did not make specific hypotheses because the literature has provided less information about the clinical implications of this construct.
This article complements previous reports using Jarrett et al.’s (2001) data set. First, Jarrett et al. (2001) found that among randomized A–CT responders, C–CT reduced relapse compared to assessment-only control over 8 months. Over 24 months, C–CT reduced relapse/recurrence among patients with early onset depression and unstable remission late in A–CT. Second, Vittengl, Clark, and Jarrett (2003) found that a measure of interpersonal problems demonstrated circumplex structure before and after A–CT, improved during A–CT, and converged regularly with measures of social adjustment and personality pathology. Third, Clark, Vittengl, Kraft, and Jarrett (2003a) partitioned state and trait variance components in dimensions of personality pathology early and late in A–CT. Both components correlated concurrently with depressive symptoms, only state variance correlated with change in depressive symptoms, and only trait variance predicted depressive symptoms forward in time. Fourth, Clark, Vittengl, Kraft, and Jarrett (2003b) partitioned shared and unique variance components among measures of interpersonal, cognitive, social, and personality functioning early and late in A–CT. Only the most general shared component predicted depressive symptoms late in A–CT. Finally, Vittengl, Clark, and Jarrett (2004) found that improvements in interpersonal problems, social adjustment, and dyadic adjustment were significant from before to after A–CT, although the improvements were smaller than and largely accounted for by the concurrent decrease in depressive symptoms. C–CT did not improve interpersonal problems, social adjustment, or dyadic adjustment compared to assessment-only control, although gains made during A–CT were maintained for 2 years post-A–CT. In this context in this article, we uniquely examine changes in the SASB with A–CT and C–CT as well as prediction of A–CT response and post-A–CT relapse/recurrence of depression from the SASB. This focus on self-directed behavior, thought, and emotion overlaps only partially with the psychosocial domains have been examined previously (i.e., personality, interpersonal problems, social adjustment, dyadic adjustment, and cognitive content; Clark et al., 2003a, 2003b; Jarrett et al., 2001; Vittengl et al., 2003, 2004) and so broadens understanding of the far-reaching effects of cognitive therapy.
METHOD
Participants
Participants were adult outpatients presenting with Diagnostic and Statistical Manual of Mental Disorders (4th ed. [DSM–IV]; American Psychiatric Association, 1994) nonpsychotic, recurrent, major depressive disorder. Inclusion criteria included clear interdepressive episode recovery (≥ 2 months of at least nearly normal functioning) and a score ≥ 16 on the 17-item Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960). Exclusion criteria included concurrent medical disorders potentially accounting for depressive symptoms, organic mental disorders, psychotic disorders, active substance abuse or dependence, primary obsessive compulsive or eating disorders, borderline personality disorder, and inability or unwillingness to complete questionnaires or to comply with the treatment protocol. Participants were recruited through media, printed announcements, and self-referral and practitioner referral. They completed telephone screening (N > 3,500) and if potentially eligible, diagnostic interviews (N = 608) at the Psychosocial Research and Depression Clinic in the Department of Psychiatry at The University of Texas Southwestern Medical Center at Dallas, which included the Structured Clinical Interview for DSM–III–R (SCID, outpatient version; Spitzer, Williams, Gibbon, & First, 1989) and supplemental interview questions to assess DSM–IV disorders. The first interview assessment was conducted by trained evaluators (described following) and resulted in 361 patients being referred for treatment elsewhere due to application of exclusion criteria. The remaining 247 patients were scheduled for reassessment by faculty level diagnosticians (described following). Among persons reassessed, 63 were excluded, 5 refused consent, and 156 consented to enter the study protocol. Jarrett et al. (2001) provides additional detail about patient inclusion and exclusion.
Similar to the full sample consenting to the protocol (N = 156), the subsample contributing SASB data (N = 148) included 75.0% women. The mean age was 41.4 years (SD = 11.1); the mean level of education was 15.4 years (SD = 2.8); and 6.0% were African American, 4.7% Hispanic, 1.4% Native American, and 87.8% White. The participants’ mean age of onset of major depressive disorder was 20.0 years (SD = 9.7), and participants had experienced a mean of 3.4 major depressive episodes (SD = 1.3). Prior treatment exposure data for participants’ first, most recent two, and current major depressive episodes indicated that 2.0% had been treated previously with electroconvulsive therapy, 58.8% with pharmacotherapy, 58.8% with psychotherapy, and 42.6% with at least two of these types of therapy. In addition to the diagnosis of recurrent major depressive disorder, the number of DSM–IV Axis I disorders pre-A–CT ranged from zero to four (M = 0.60; SD = 0.78). As is common in depressed samples, comorbid Axis I disorders included social phobia (20.3%), specific phobias (12.8%), panic disorder without agoraphobia (8.9%), posttraumatic stress disorder (7.4%), dysthymic disorder (5.4%), obsessive–compulsive disorder (1.4%), panic disorder with agoraphobia (1.3%), and 0.7% each of agoraphobia without a history of panic disorder, attention deficit hyperactivity disorder, bulimia nervosa, and hypochondriasis.
Procedure
A–CT phase. A–CT (Beck et al., l979) was conducted by five experienced therapists. A–CT was administered within a 12- to 14-week protocol including 20 individual sessions (50 to 60 min) held twice weekly for the first 8 weeks and once weekly for the last 4 weeks. No pharmacotherapy was provided. A–CT is designed to reduce depressive symptoms by eliciting thoughts associated with negative affect, teaching patients to evaluate the validity of such thoughts through logical and empirical methods, and generating more realistic alternatives when negative thoughts are not supported. Of the 156 patients who consented to A–CT, 130 (83%) completed the 20-session protocol (2 became psychotic or homicidal and were withdrawn, and 24 dropped out), and 97 (62%) met criteria for treatment response (HRSD ≤ 9 and absence of DSM–IV major depressive disorder).1
Experimental phase. The purpose of the experimental phase was to evaluate the efficacy of C–CT (Jarrett, 1989; Jarrett et al., 1998; Jarrett & Kraft, 1997). Of the 87 A–CT responders who also completed the 0-month post-A–CT assessment, 84 consented to randomization and were assigned to either C–CT (n = 41) or an assessment-only control condition (n = 43). No pharmacotherapy was provided. The C–CT protocol consisted of ten 60- to 90-min sessions of C–CT over 8 months (the first 4 sessions semimonthly and the next 6 sessions monthly) from the same therapist who had provided A–CT. C–CT is designed to prevent relapse and recurrence of depression through maintenance and generalization of skills learned in A–CT, reduction of residual depressive symptoms, and preparation for current or anticipated vulnerabilities. In C–CT, patients are taught to use emotional distress and symptoms as cues to implement skills learned in A–CT. Patients randomized to C–CT completed an average of 9.5 sessions (mode = 10). Patients in the assessment-only control were scheduled for evaluation visits at the same frequency as in C–CT and completed an average of 9.1 sessions (mode = 10). Evaluators of control patients had not provided A–CT and were prohibited from using psychosocial interventions. In both C–CT an assessment-only conditions, patients who relapsed during the experimental phase were asked to complete all sessions and were referred for extra-protocol treatment if not receiving C–CT. Data collected after relapse are utilized as available in this article to increase the generalizability of findings.
Follow-up phase. All 84 patients entering the experimental phase were eligible for, and 74 entered, the follow-up phase.2 This assessment-only period lasted 16 months beyond the experimental phase (24 months post-A–CT) and consisted of 10 sessions scheduled monthly at months 9 to 12 post-A–CT and bimonthly at months 14 to 24 post-A–CT. Evaluators were prohibited from using psychosocial interventions, and no pharmacotherapy was provided. Patients completed an average of 8.9 assessment sessions (mode = 10). Patients who experienced relapse or recurrence of depression during follow-up phase were referred for extra-protocol treatment and followed naturalistically; their data are utilized as available in this article to increase generalizability. Essential features of the study phases are depicted in Figure 2.
FIGURE 2.
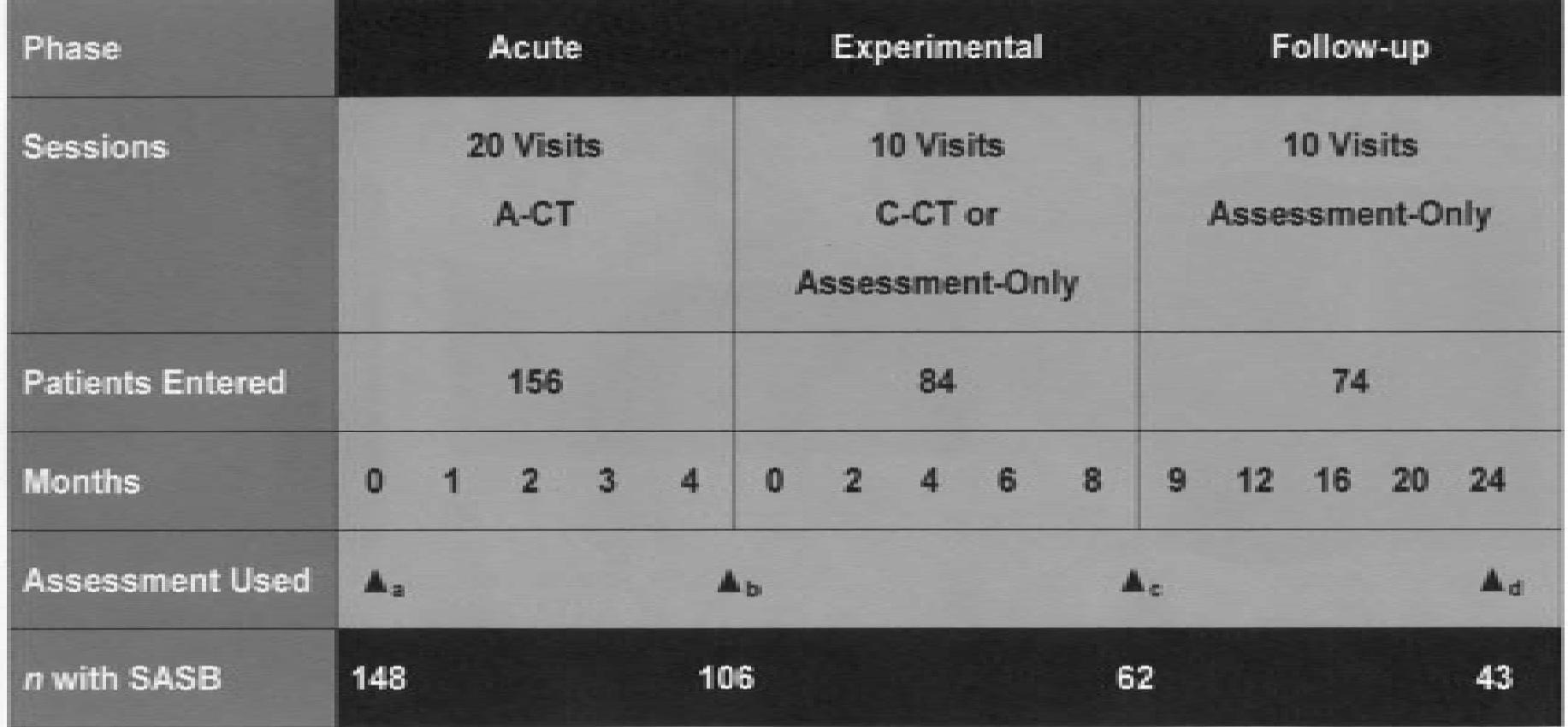
Design of randomized controlled trial and assessments used in these statistical analyses. A–CT = acute phase cognitive therapy; C–CT = continuation phase cognitive therapy. Assessment a = pre-A–CT (first therapy session); b = 0 months post-A–CT (average of 5 days after the 20th A–CT session); c = 8 months post-A–CT (end of experimental phase); d = 24 months post-A–CT (end of follow-up phase). SASB = Structural Analysis of Social Behavior.
Measures
SASB. Participants completed Intrex Long Form questionnaires (Benjamin, 2000) including 36 items describing self-directed behavior, thought, and emotion (e.g., "I just let myself go along with today as it is and don’t plan for tomorrow"; "I let myself murder, kill, destroy and reduce myself to nothing"; "I tenderly, lovingly, cherish and adore myself"). Items were rated in 10-point increments on a 0- to 100-point scale, with higher ratings reflecting more intense or frequent behavior, thought, and emotion. The items were presented twice with instructions to make ratings at one’s best and then at one’s worst. Internal consistency was computed with Benjamin’s (1974) circumplex autocorrelation method at pre-A–CT and 0, 8, and 24 months post-A–CT, yielding internal consistencies of .96, .95, .95, and .95 for the "at-best" profile and .98, .92, .91, and .86 for the "at-worst" profile, respectively. Affiliation and autonomy scores were derived by averaging the 4 to 5 relevant items to form each of eight cluster scales (see Table 1), weighting the clusters to reflect their relative loadings on affiliation and autonomy, and summing the weighted clusters (see Benjamin, 2000, and Pincus, Newes, Dickinson, & Ruiz, 1998 for more detail about scoring affiliation and autonomy scales). We chose affiliation and autonomy scales as the primary study variables because they correlate highly (negatively) with the also commonly used attack and control pattern coefficients (averaged multiple correlations of cluster profiles with theoretical curves), but the affiliation and autonomy scales have distributions closer to normal and are more nearly orthogonal (Pincus, Newes, et al., 1998).
BDI. The Beck Depression Inventory (BDI; Beck, Ward, Mendelson, Mock, & Erbaugh, 1961) is a very widely used, 21-item, self-report measure of depressive symptom severity. Beck, Steer, and Garbin (1988) reported an average internal consistency of .87, an average short-term (< 1 month) retest reliability of .60, and considerable convergence with clinical ratings of depressive symptoms, the HRSD, and other self-report measures of depressive symptoms. These analyses with the BDI focus on the first A–CT session for which the alpha internal consistency was .85.
HRSD. The HRSD (Hamilton, 1960) is a widely used, 17-item, clinician rating scale to assess severity of depressive symptoms. The scale has demonstrated good interrater reliability (r = .85; Clark & Watson, 1991), adequate internal consistency (as of .88 and .89 in two large clinic samples; Rush, Gullion, Basco, Jarrett, & Trivedi, 1996), and appropriate convergence with self-report depressive symptom measures (rs = .70 to .83; Clark & Watson, 1991). These analyses with the HRSD focus on the first A–CT session during which the HRSD was completed by the A–CT therapists. Although alpha internal consistency for the HRSD was low at this assessment (.34), the HRSD correlated highly (.72) with the clinician version of the Inventory for Depressive Symptomatology (Rush et al., 1996) in support of its validity.
LIFE. The Longitudinal Interval Follow-Up Evaluation (LIFE; Keller et al., 1987) is a semistructured interview used to rate DSM–IV Axis I psychopathology, treatment history, and psychosocial functioning, retrospectively. Interrater reliabilities for the LIFE’s numerous indexes have typically been > .70 (Keller et al., 1987). Trained independent evaluators completed LIFE ratings at 4, 8, 12, and 24 months post-A–CT; at exit; and at any time patients, therapists, or follow-up evaluators suspected relapse or recurrence of major depressive disorder. In these analyses, weekly psychiatric status ratings of major depressive disorder (on a scale ranging from 1 to 6 in which ratings 5 indicate meeting diagnostic criteria) were used assess relapse and recurrence post-A–CT. Relapse was defined as meeting criteria for DSM–IV major depressive disorder before and recurrence as meeting criteria after 8 consecutive months free of major depressive disorder (recovery). Relapse and recurrence events were collapsed for these analyses. In addition, weekly treatment history ratings were used to assess patients’ receipt of extraprotocol pharmacotherapy and psychosocial treatment (e.g., couples therapy, individual therapy, support groups) post-A–CT. Finally, monthly psychosocial functioning ratings were collected but not used in these analyses.
Clinicians
Intake evaluators. The first pretreatment assessments were conducted by a master’s level psychological associate, a psychiatric nurse, a PhD candidate in clinical psychology, and a PhD clinical psychologist. The second pretreatment assessments were conducted entirely by faculty-level diagnosticians, all holding the PhD in clinical psychology or the MD with training in psychiatry, to verify patients' study eligibility or exclusion. All interviewers had received didactic training in use of the SCID and depressive symptom severity structured interviews and were mentored by experienced interviewers during their initial (prestudy) assessments.
Psychotherapists. Five experienced psychotherapists provided A–CT and C–CT. Each therapist held the PhD in clinical psychology or the MD with training in psychiatry and had completed 1 or more years of cognitive therapy training, achieving and maintaining competency scores ≥ 40 on the Cognitive Therapy Scale (CTS; Young & Beck, 1980) before treating any study patients. During both A–CT and C–CT, therapists received weekly group supervision with a PhD clinical psychologist with extensive experience in supervising cognitive therapy and additional consultation/supervision as requested. Moreover, during both A–CT and C–CT, the fourth and an additional randomly selected therapy session were videotaped for review by an offsite consultant (a PhD clinical psychologist with extensive experience evaluating cognitive therapy) using the CTS. Therapists received timely written feedback regarding their performance in the fourth therapy session to foster increased compliance with the treatment manuals. All therapists achieved mean CTS scores > 40 during both A–CT and C–CT indicating competence in delivering the treatments.
Independent evaluators. Independent evaluators completed assessments at 0, 4, 8, 12, and 24 months post-A–CT and whenever relapse or recurrence of major depressive disorder was suspected by follow-up evaluators, patients, or therapists. Research personnel and patients concealed assignment to C–CT or assessment-only control from the independent evaluators. The independent evaluators were highly experienced clinicians trained in the application of DSM–IV criteria, depressive symptom severity measures, and the LIFE.
Extraprotocol Treatment
Participants agreed initially to postpone or to report all extraprotocol treatment throughout the study including use of psychotropic medications, psychotherapy, and other psychosocial interventions. Based on LIFE ratings, during the 104 weeks post-A–CT, patients received an average of 9.1 (SD = 19.9; median (Mdn) and mode = 0) weeks of treatment with psychotropic medication and 4.6 (SD = 12.0; Mdn and mode = 0) extraprotocol psychosocial treatment sessions (e.g., support groups, marital and family therapy, individual psychotherapy). This relatively small amount of extraprotocol treatment did not differ significantly between C–CT and assessment-only control groups by Wilcoxon or t test, ps > .13, two-tailed.
Overlap With Previous Reports Using Jarrett et al.’s (2001) Data Set
Although these hypotheses and analyses are distinct from previous reports using Jarrett et al.’s (2001) data set, there is some overlap with previous reports in participants and measures. This article focuses on patients consenting to A–CT with SASB data (N = 148), of whom 56% (83/148), 78% (115/148), 72% (107/148), 68% (100/148), and 100% (148/148) were included in other subsamples analyzed by Jarrett et al. (2001); Vittengl et al. (2003); Clark et al. (2003a, 2003b); and Vittengl et al. (2004), respectively. As in this study, all of the previous reports used the HRSD and BDI as measures of depressive symptoms (either individually or as part of a multimeasure composite), with the exception of Jarrett et al. (2001) who did not analyze BDI data. Finally, in this study, we used the LIFE to measure relapse/recurrence of depression as did Jarrett et al. (2001). None of the previous reports analyzed data from the SASB.
Effect Size Statistics
We report effect sizes computed with Cohen’s (1988) formulas to characterize the magnitude of results. Effect size statistics included (benchmarks for small, medium, and large effects) r (.10, .30, .50) and d (0.20, 0.50, 0.80).
RESULTS
Interrelations of Self-Directed Affiliation and Autonomy Before and After A–CT
Table 2 presents intercorrelations of SASB self-directed affiliation and autonomy scales in the subsample with complete at-best and at-worst data (N = 100; results using all data available pairwise were quite similar)3 pre-A–CT and 0 months post-A–CT (M = 5, range = 0 to 13 days after the 20th A–CT session). Within time (pre-A–CT and post-A–CT) and valence (best vs. worst), affiliation and autonomy were largely independent, Mdn r = .00 (range = –.24 to .13). The convergence of at-best and at-worst reports was low for affiliation (rs = .24 pre-A–CT and .07 post-A–CT), suggesting that they tap largely different aspects of the self-view, and moderate for autonomy (rs = .49 pre-A–CT and .37 post-A–CT), suggesting modest consistency of the self-view of autonomy regardless of state. Finally, within-valence re-test correlations of both scales were moderate, Mdn r = .46 (range = .24 to .49), suggesting that the scales had some cross-time consistency but did not demonstrate the strong re-test stability expected of trait measures.
TABLE 2.
Correlations Among Self-Directed Affiliation and Autonomy Pre-A–CT Phase Cognitive Therapy and 0 Months Post-A–CT
|
Correlations (r) Among Scales |
||||||||
|---|---|---|---|---|---|---|---|---|
| Scale | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| 1. Best-AFF pre-A–CT | — | |||||||
| 2. Best-AFF post-A–CT | .49 | — | ||||||
| 3. Best-AUT pre-A–CT | .13 | .03 | — | |||||
| 4. Best-AUT post-A–CT | .13 | .11 | .48 | — | ||||
| 5. Worst-AFF pre-A–CT | .24 | .11 | .02 | .03 | — | |||
| 6. Worst-AFF post-A–CT | .05 | .07 | -.04 | -.02 | .24 | — | ||
| 7. Worst-AUT pre-A–CT | .00 | -.09 | .49 | .16 | -.11 | -.07 | — | |
| 8. Worst-AUT post-A–CT | .01 | .03 | .38 | .37 | -.07 | -.24 | .44 | — |
Note. N = 100. Retest correlations underlined. Best–worst concurrent convergent correlations in italics. ǀrǀs ≥ .20, p < .05, two-tailed. Effect size ǀrǀ values ≥ .10, .30, and .50 mark small, medium, and large effects, respectively (Cohen, 1988). A–CT = acute phase cognitve therapy; best = ratings at one’s best; AFF = afilliation; AUT = autonomy; worst = ratings at one’s worst.
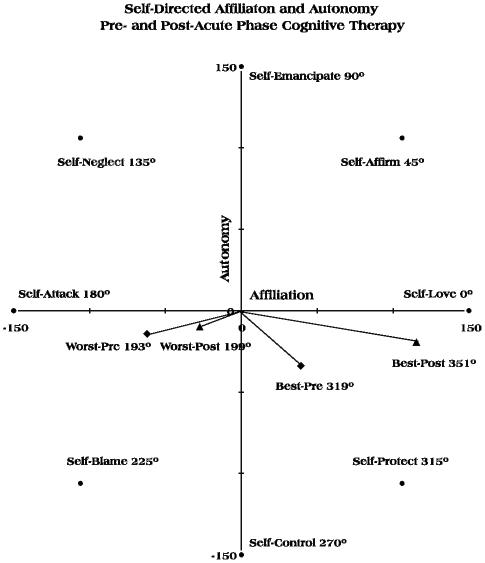
Hypothesis 1: Self-Directed Affiliation Will Increase From Before to After A–CT
Table 3 presents descriptive statistics for the affiliation and autonomy scales pre-A–CT and 0 months post-A–CT. In support of our first hypothesis, repeated measures analysis of variance (ANOVA) indicated that at-best reports, F(1, 99) = 245.78, p < .01, d = 1.57 and at-worst reports, F(1, 99) = 18.47, p < .01, d = 0.43 changed from pre- to post-A–CT. Follow-up t tests indicated that all scales except autonomy at worst changed (increased) significantly (see Table 3). To help visualize the patient self-directed functioning before and after A–CT, we plotted mean scores in self-directed circumplex space and computed angular degrees associated with at-best and at-worst functioning using standard trigonometric formulas (see Figure 3). In this plot, the length of a line from the origin (affiliation = 0, autonomy = 0) indicates the intensity, and the angular direction indicates the predominant character of self-directed thought, behavior, and emotion. Pre-A–CT, at-worst functioning was oriented closest to the self-attack cluster (180°) and was relatively intense, consistent with depression, whereas at-best functioning was oriented closest to the self-protect cluster (315°). Post-A–CT, at-worst functioning was still closest to self-attack but somewhat less intense, and at-best functioning was closest to self-love (0/360°) and somewhat more intense.
TABLE 3.
Change in Self-Directed Affiliation and Autonomy From Pre-A–CT to 0 Months Post-A–CT
| 0 Months | ||||||
|---|---|---|---|---|---|---|
|
Pre-A–CT |
Post-A–CT |
|||||
| Scale | M | SD | M | SD | Δt(99) | d |
| Best AFF | 39.3 | 84.7 | 115.4 | 61.5 | 9.98* | 1.00 |
| Best AUT | -34.0 | 38.1 | -18.7 | 29.8 | 4.30* | 0.43 |
| Worst AFF | -61.9 | 69.4 | -27.4 | 87.7 | 3.53* | 0.35 |
| Worst AUT | -14.3 | 41.1 | -9.3 | 39.9 | 1.16 | 0.12 |
Note. N = 100. Effect size d values ≥ 0.20, 0.50, and 0.80 mark small, medium, and large effects, respectively (Cohen, 1988). A–CT= acute phase cognitve therapy; best = ratings at one’s best; AFF = affiliation; AUT = autonomy; worst = ratings at one’s worst.
p < .05, two-tailed.
FIGURE 3.
Mean self-directed affiliation and autonomy scores from the Structural Analysis of Social Behavior changed from preacute phase cognitive therapy to 0 months postacute phase cognitive therapy. Best = ratings at one’s best; worst = ratings at one’s worst.
Overall, these results were consistent with A–CT improving psychological health as measured by relatively large increases in SASB self-directed affiliation. However, examination of raw score means for autonomy suggested a potential paradox: Depressed patients reported that low autonomy was better than high autonomy (pre-A–CT: at-best, M = –34.0; at-worst, M = –14.3), but when they were no longer acutely depressed, they rated themselves as somewhat more autonomous than they did when they were depressed (post-A–CT: at-best, M = –18.7; at-worst, M = –9.3). In addition, the large standard deviations for affiliation and autonomy indicated considerable variability, which limited statistical power to detect mean changes and suggested that some individuals did not fit the mean pattern.
Hypothesis 2: Higher Self-Directed Affiliation Will Predict A–CT Response
Of the 156 patients who consented to A–CT, 62% (97/156) met criteria for treatment response (HRSD ≤ 9 and absence of DSM–IV major depressive disorder). Responders’ and nonresponders’ at-best and at-worst reports were compared pre- and post-A–CT. Failing to support our second hypothesis, neither the at-best nor at-worst reports pre-A–CT predicted responder status by ANOVA (ps > .16; ds < 0.22). Post-A–CT, however, responders and nonresponders differed in both their at-best, F(1, 104) = 27.00, p < .01, d = 1.02 and at-worst, F(1, 103) = 5.32, p = .02, d = 0.45 reports. Follow-up t tests indicated that responders had higher affiliation at-best (M = 130.1, n = 79) than nonresponders (M = 67.5, n = 27), t(104) = 5.12, p < .01, two-tailed, d = 1.14; and responders had higher affiliation at-worst (M = –18.1, n = 78) than nonresponders (M = –59.3, n = 27), t(103) = 2.18, p = .03, two-tailed, d = 0.49; but responders and nonresponders did not differ significantly on autonomy at-best or at-worst (ps > .10, two-tailed; ds < 0.37). These results suggest affiliation more closely tracked the decrease in depression (as represented in treatment response vs. nonresponse) than did autonomy.
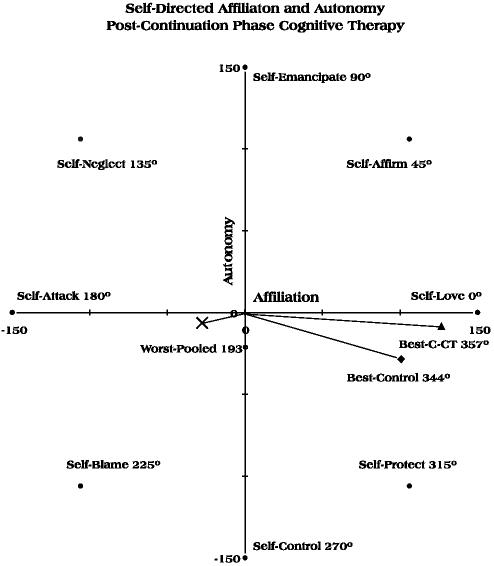
Hypothesis 3: C–CT Will Increase Self-Directed Affiliation Compared to Assessment Only
Consenting A–CT responders (N = 84) were randomized to 8 months of C–CT (n = 41) or assessment-only control (n = 43) and then assessed over an additional 16 months (total of 24 months post-A–CT). Consistent with randomization, C–CT and control groups did not differ in their at-best or at-worst reports pre-A–CT (when acutely depressed) or 0 months post-A–CT (after treatment response) by ANOVA (ps > .18; ds < 0.26). At the end of the 8-month experimental phase, the C–CT and control groups differed in their at-best report, F(1, 60) = 4.94, p = .03, d = 0.57 but did not differ significantly in their at-worst report (p = .38, d = 0.23). Similarly, 24 months post-A–CT, the C–CT and control groups differed in their at-best report, F(1, 41) = 8.45, p < .01, d = 0.91 but did not differ significantly in their at-worst report (p = .06, d = 0.61). As shown in Table 4, follow-up t tests did not support our third hypotheses at the a priori alpha level of .05, two-tailed. The overall at-best differences were due to the C–CT group having reported higher autonomy at-best scores than the control at both 8 and 24 months post-A–CT. However, at the one-tailed alpha level of .05, C–CT also produced significantly greater affiliation at-best at 8 and 24 months post-A–CT with a medium effect size, consistent with our hypothesis.
TABLE 4.
Effects of C–CT on Self-Directed Affiliation and Autonomy
|
C–CT |
Assessment Only Control |
|||||||
|---|---|---|---|---|---|---|---|---|
| Scale | n | M | SD | n | M | SD | t(N–2) | d |
| End of experimental phase (8 months post-A–CT) | ||||||||
| Best AFF | 30 | 126.7 | 52.9 | 32 | 100.7 | 68.3 | -1.67† | 0.42 |
| Best AUT | 30 | -7.7 | 32.2 | 32 | -28.5 | 31.6 | -2.57* | 0.65 |
| Worst AFF | 30 | -18.8 | 85.8 | 32 | -35.9 | 69.2 | -0.87 | 0.22 |
| Worst AUT | 30 | -5.4 | 33.0 | 32 | -7.2 | 37.7 | -0.20 | 0.05 |
| End of follow-up phase (24 months post-A–CT) | ||||||||
| Best AFF | 22 | 145.7 | 39.3 | 21 | 114.5 | 75.4 | -1.71† | 0.52 |
| Best AUT | 22 | 1.0 | 29.0 | 21 | -25.6 | 29.3 | -2.98* | 0.91 |
| Worst AFF | 22 | -3.1 | 91.3 | 21 | -48.9 | 98.1 | -1.58 | 0.48 |
| Worst AUT | 22 | -0.4 | 24.7 | 21 | -14.4 | 44.0 | -1.30 | 0.40 |
Note. Effect size d values≥ 0.20, 0.50, and 0.80 mark small, medium, and large effects, respectively (Cohen, 1988). C–CT = continuation phase cognitive therapy; A–CT = acute phase cognitve therapy; best = ratings at one’s best; AFF = afilliation; AUT = autonomy; worst = ratings at one’s worst.
p < .05, two-tailed.
p ≤ .05, one-tailed.
Means at the end of the 8-month experimental phase are plotted in Figure 4 separately for C–CT and control for the at-best report and pooled for at-worst because the groups did not differ significantly. As depicted in Figure 4, both C–CT and control groups’ at-worst functioning continued to be represented most closely by the self-attack cluster (180°), and their at-best functioning was most similar to the self-love cluster (0/360°). However, the C–CT group’s at-best functioning more closely approximated self-love in intensity (longer line length) and character (line angle).
FIGURE 4.
Mean self-directed affiliation and autonomy scores from the Structural Analysis of Social Behavior after 8 months of continuation phase cognitive therapy (C–CT) or assessment only (Control). Worst ratings pooled because C–CT and control groups did not differ significantly. Best = ratings at one’s best; worst = ratings at one’s worst.
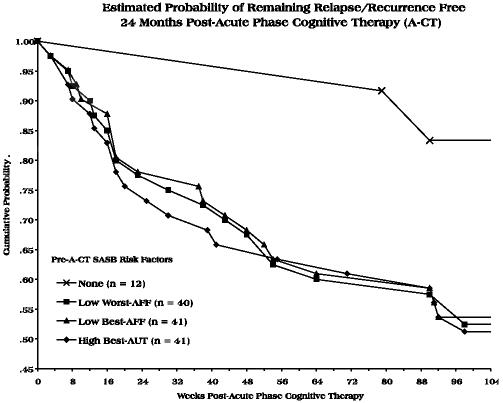
Hypothesis 4: Higher Self-Directed Affiliation Will Predict Longer Survival From Relapse/Recurrence of Depression
Cox regression analyses were used to predict time-to-relapse/recurrence of depression from self-directed affiliation and autonomy ratings. A type of survival analysis, Cox regression may be used to model time to a discrete event (e.g., relapse/recurrence) as a function of continuous predictors (e.g., affiliation and autonomy scores) while accurately accommodating "right-censored" cases (i.e., cases without target events, such as relapse/recurrence, during the observation period; see Luke & Homan, 1998, and Singer & Willett, 2003, for summaries of Cox regression analysis). In this data set, 61% (51/84) of patients did not have a recorded relapse/recurrence during the 24-months of assessment after A–CT including 15% (13/84) who attrited. Analyses were conducted first over the 8-month experimental phase and then over the entire 24-month post-A–CT period to model time-to-relapse/recurrence of DSM–IV major depressive disorder. Analyses were conducted separately for at-best and at-worst reports at pre-A–CT (when acutely depressed) and at 0 months post-A–CT (after treatment response). All models included C–CT versus control status, which is the focus of another report (Jarrett et al., 2001). C–CT is not discussed here other than to note that C–CT increased time-to-relapse/recurrence significantly over 8 months but was not significant as a main effect over the full 24 months post-A–CT (consistent with Jarrett et al., 2001; and as shown in Table 5), and C–CT did not interact significantly with self-directed affiliation or autonomy in hypothesis tests (ps > .09, rs < .19).
TABLE 5.
Prediction of Post-A–CT Relapse/Recurrence of Major Depressive Disorder From Pre-A–CT Self-Directed Affiliation and Autonomy
|
8 Months Post-A–CT |
24 Months Post-A–CT |
|||||||
|---|---|---|---|---|---|---|---|---|
| Predictor | β | SE | χ2(1) | r | β | SE | χ2(1) | r |
| At-best ratings of AFF and AUT | ||||||||
| C–CT | -1.6035 | 0.6135 | 6.83* | .29 | -0.7057 | 0.3659 | 3.72 | .21 |
| AFF | -0.0067 | 0.0032 | 4.50* | .23 | -0.0058 | 0.0023 | 6.14* | .27 |
| AUT | 0.0203 | 0.0082 | 6.16* | .27 | 0.0128 | 0.0059 | 4.81* | .24 |
| At-worst ratings of AFF and AUT | ||||||||
| C–CT | -1.2625 | 0.5919 | 4.55* | .24 | -0.5792 | 0.3636 | 2.54 | .18 |
| AFF | -0.0115 | 0.0054 | 4.53* | .24 | -0.0088 | 0.0033 | 7.16* | .30 |
| AUT | 0.0047 | 0.0058 | 0.66 | .09 | 0.0067 | 0.0046 | 2.14 | .16 |
Note. n = 81 for models with at-worst variables including 15 and 33 with relapse/recurrence events within 8 and 24 months, respectively; n = 83 for models with at-best variables including 16 and 33 with relapse/recurrence events within 8 and 24 months, respectively. C–CT coded as 1=8 months of continuation phase cognitive therapy, 0 = 8 months of assessment-only control. Negative and positive betas, respectively, mark longer and shorter estimated time-to-relapse/recurrence of major depressive disorder. Effect size r values ≥ .10, .30, and .50 mark small, medium, and large effects, respectively (Cohen, 1988). A–CT = acute phase cognitive therapy; AFF = affiliation; AUT = autonomy; C–CT = continuation phase cognitive therapy.
p < .05.
Neither the at-best nor at-worst reports at 0 months post-A–CT predicted time-to-relapse/recurrence (ps > .22, rs < .14), failing to support our hypothesis. In support of our hypothesis, however, ratings made pre-A–CT (when acutely depressed) did predict time-to-relapse/recurrence. Over both the 8- and 24-month periods, increased time-to-relapse/recurrence was predicted from higher affiliation at best and at worst, in support of our hypothesis, and also by lower autonomy at best (see Table 5). Thus, a better prognosis after A–CT response was predicted by self-reports of greater self-love and self-control at one’s best and by greater self-love at one’s worst when beginning A–CT. To better conceptualize these effects, Figure 5 depicts the cumulative probability of remaining free of major depressive disorder during 24 months post-A–CT for patients with pre-A–CT SASB scores above the median in the direction of high risk and for those with no such risk factors (all SASB scores below the median in the direction of low risk).
FIGURE 5.
Pre-A–CT ratings of self-directed affiliation (AFF) and autonomy (AUT) from the Structural Analysis of Social Behavior (SASB) predicted relapse/recurrence of major depressive disorder 24 months post-A–CT. Median splits of pre-A–CT AFF and AUT defined high-risk groups, which are not mutually exclusive. A–CT = acute phase cognitive therapy; best = ratings at one’s best; worst = ratings at one’s worst.
A potential interpretation of the prediction of relapse/recurrence post-A–CT from pre-A–CT reports is that affiliation and autonomy scores simply reflect the severity of the index episode. However, forcing pre-A–CT BDI and HRSD scores separately (to avoid estimation problems due to highly correlated predictors) into the 8- and 24-month regression models argued against this interpretation. Specifically, neither pre-A–CT BDI nor HRSD predicted relapse/recurrence (ps > .25, rs < .13), C–CT continued to predict longer time to relapse/recurrence over 8 but not over 24 months (with the exception of the at-best model including the pre-A–CT BDI in which C–CT crossed the p < .05 threshold to predict longer time-to-relapse/recurrence; r = .22), and the SASB scales remained significant predictors as previously (ps < .05, rs > .23) when these depressive symptom severity measures were included in the regressions. Furthermore, interactions of the SASB scales with the BDI and HRSD did not add incremental predictive power to equations containing SASB scale main effects for either the 8- or 24-month periods (ps > .12, rs < .18).
DISCUSSION
Summary of Results
This article provides unique data bearing on the validity of the SASB self-directed domain in A–CT and C–CT for recurrent major depressive disorder. In support of our first hypothesis, we found that self-directed affiliation at best and at worst increased over A–CT. We also found that autonomy at best increased over A–CT. Our second hypothesis that greater affiliation would predict response to A–CT was not supported with pre-A–CT reports, but responders were differentiated from nonresponders by their greater affiliation at best and at worst at 0 months post-A–CT. Our third hypothesis that C–CT would increase affiliation relative to an assessment-only control was supported with at-best reports (at the .05, one-tailed alpha level), and C–CT also increased autonomy at best. C–CT did not change at-worst affiliation and autonomy. Finally, our fourth hypothesis that greater affiliation would predict longer time to relapse/recurrence of depression was not supported with data from the post-A–CT assessment (when patients were not depressed) but was supported with the pre-ACT assessment (when patients were acutely depressed). We also found that greater autonomy at-best pre-A–CT predicted shorter time to relapse/recurrence and that prediction of relapse/recurrence from pre-A–CT affiliation and autonomy was not attributable to the severity of depressive symptoms (as measured with the BDI and HRSD).
Interpretations and Potential Clinical Implications of Results
These analyses suggest that the self-directed domain successfully tracks patient improvement in cognitive therapy. In particular, depressed patients receiving A–CT reported moderate increases in feelings, thoughts, and behaviors reflecting enjoying, cherishing, and caring for oneself and concomitant decreases in self-directed contempt and loathing. These improvements are highly congruent with goals of promoting healthy cognition and self-care in cognitive therapy (e.g., Beck et al., 1979; Hollon & Beck, 2004; Jarrett & Kraft, 1997) and extend similar findings for other forms of psychotherapy (e.g., Paivio & Bahr, 1998; Paivio & Greenberg, 1995; Junkert-Tress et al., 2001). Other psychotherapy outcome studies assessing the SASB self-directed domain, however, have not examined change in autonomy. We found that autonomy at best increased from before to after A–CT, and that among A–CT responders, C–CT increased affiliation and autonomy at best compared to assessment only. Consequently, in addition to increases in affiliation, depressed patients receiving cognitive therapy might expect increases in thoughts, behaviors, and emotions reflecting a less personally restrictive, more carefree attitude.
Our finding that greater affiliation at best and at worst predicted longer time-to-relapse/recurrence post-A–CT was not attributable to individual differences in the severity of depressive symptoms pre-A–CT. Although the mechanisms of risk were not identifiable with this design, the observed risk factors were consistent with both SASB and cognitive theory. We speculate that individuals with lower affiliation have greater negative self-referent thought and associated behavior and emotion, which may directly or indirectly increase risk of depression. Although replication and clarification of these results clearly are needed, understanding of pre-treatment risk factors for relapse/recurrence can help identify targets for improvement in treatment. For example, to the extent that affiliation confers direct relapse/recurrence risk, patients with low self-affiliation might be better served with a treatment shown to improve the self-view. On the other hand, if low self-affiliation confers risk indirectly (e.g., through less self-reward, lower perceived ability to handle stressors), treatment enhancements might also target these associated processes.
In contrast to consistent findings that higher affiliation is "good," the meaning of self-reported autonomy at best may vary by depressive state. This SASB scale increased from before to after A–CT and increased in C–CT compared to assessment only control. However, high pre-A–CT (but not post-A–CT) autonomy at best was also a risk factor for depressive relapse/recurrence, even when controlling initial depressive symptom severity. We speculate that an increase in autonomy at best during cognitive therapy marks an increase in psychological health (e.g., feeling freed from the perfectionistic need to control oneself or freedom to "be oneself"). In contrast, relatively high autonomy at best when acutely depressed may reflect feelings of lack of control over one’s thought, behavior, and emotion and so function as a risk factor for depressive relapse/recurrence (e.g., feeling overwhelmed when confronted with an external stressor that taxes efforts to implement coping strategies learned in therapy). Replication of greater relapse/recurrence risk with higher pre-treatment autonomy and additional research aimed at testing our speculation would be usefulin clarifying this possibility.
Case Examples
To illustrate changes in the SASB during cognitive therapy, we describe the progress of two patients who responded to A–CT, one randomized to C–CT and the other to assessment-only control. To support interpretations of the changes in the patients’ SASB profiles, we evaluated the significance of change in individuals’ affiliation and autonomy scores with Jacobson and Truax’s (1991) reliable change index. The reliable change index is computed as the difference between an individual’s scores at two points in time divided by the standard error of difference for a particular scale. If the resulting value is ≥ 1.96, then (assuming a normal underlying distribution) the probability that the change occurred by chance alone is < .05, two-tailed. We used data from the 12- and 24-month post-A–CT assessments in the subsample with complete data that did not relapse (n = 27; an approximation of a normal adult sample) to estimate standard errors. In the subsample, affiliation and autonomy at best (.70 and .64, respectively) and at worst (.58 and .71, respectively) had moderate retest correlations over this period and did not change significantly in mean level by dependent t tests, ps > .19, two-tailed. Reliable change thresholds (standard error × 1.96) for affiliation and autonomy at best were 81.9 and 51.5, respectively, and at-worst were 154.6 and 48.0, respectively. We compared later assessments to the pre-A–CT baseline, and differences exceeding the reliable change thresholds were considered significant.
Participant 1043. A 54-year-old woman presented with a history of five major depressive episodes, and her episode at intake was of moderate severity (HRSD = 23). Pre-A–CT, the patient’s at-best affiliation (56.1) and autonomy (–55.4) scores reflected self-protection (315°), and her at-worst affiliation (–39.8) and autonomy (3.1) scores marked self-attack (176°). Post-A–CT, the patient’s at-best affiliation had increased reliably to 146.1, but autonomy (–25.2) had not changed significantly. Together these at-best scores marked self-love (350°), suggesting some improvement in the patient’s self-directed thought, behavior, and emotion over A–CT. Her at-worst affiliation (–19.2) and autonomy (0.9) scores had not changed reliably from pre-A–CT, however. As a consenting A–CT responder, the patient was randomized to assessment only during the experimental phase. At the end of the experimental phase, her at-best affiliation remained improved (154.3), but at-best autonomy (–9.8) and at-worst affiliation (–79.6) and autonomy (5.8) remained unchanged from pre-A–CT. The failure to improve the patient’s at-worst functioning perhaps foreshadowed the recurrence of her depression at post-A–CT Week 90.
Participant 1124. A 49-year-old man presented with a history of six major depressive episodes, and his episode at in-take was of moderate severity (HRSD = 21). The patient’s pre-A–CT affiliation and autonomy scores at best were –50.9 and –33.4, respectively, and at worst were –102.6 and –3.9, respectively. Thus, his self-directed thought, behavior, and emotion were characterized primarily by self-blame at best (213°) and by self-attack at worst (182°). At the post-A–CT assessment, the patient’s at-best affiliation score had increased reliably to 118.4, and at-best autonomy changed nonsignificantly to 11.4, together marking self-love (5°). Thus, this patient made a nearly complete "turnaround" in thought, behavior, and emotion directed toward himself at best over A–CT. His at-worst affiliation and autonomy scores changed only nonsignificantly to 28.2 and 5.3, respectively. As a consenting A–CT responder, the patient was randomized to C–CT, which he completed. At the end of C–CT, the patient produced at-best affiliation and autonomy scores of 159.3 and 43.6, respectively, both scores now increased reliably from pre-A–CT. His overall at-best functioning at 15° could still be described primarily as self-love but with some movement toward the self-affirm cluster. The patient’s post-C–CT, at-worst affiliation score (108.3) also improved significantly from pre-A–CT, and his at-worst autonomy score (39.7) remained unchanged, indicating the patient’s functioning at worst was also marked by self-love and affirmation (20°) post-C–CT. Congruently, the patient remained recurrence free throughout the follow-up period with no additional significant changes in affiliation and autonomy at 24-months post-A–CT.
Limitations
These analyses involve noteworthy limitations that temper conclusions. First, the acute phase was uncontrolled, and so conclusions that A–CT improves self-directed affiliation and autonomy necessarily are tentative. A–CT research including a comparison condition could address this issue, and the brief SASB measures would represent a relatively low response burden for participants. Second, these analyses relied primarily on self-report measures. Replication with a different method (e.g., the self-directed domain also could be rated by the therapist) would be of conceptual and practical value. Finally, this focus on outpatients with recurrent major depressive disorder raises questions about the generalizability of findings to other patient diagnostic groups, especially those treated with other psychotherapies.
Conclusions
These analyses suggest that self-directed behavior, thought, and emotion as measured by the SASB change significantly with A–CT and C–CT for recurrent depression. Increases in self-directed affiliation, in particular, were congruent with the cognitive therapy model and a positive response to treatment. In addition, assessing the self-directed domain when beginning therapy may be useful in predicting post-acute-treatment relapse/recurrence of major depressive disorder, even when controlling initial depressive symptom severity. These promising findings encourage additional research with the SASB self-directed domain in cognitive therapy for depression.
ACKNOWLEDGMENTS
The clinical trial was supported in part by Grants MH–38238 and MH–01571 from the National Institute of Mental Health (Robin B. Jarrett, Principal Investigator) and was conducted at the University of Texas Southwestern Medical Center at Dallas, Department of Psychiatry, in the Psychosocial Research and Depression Clinic. We thank our colleagues for contributing to this research. Dolores Kraft coordinated the trial and provided clinical support. Jeanette Doyle, Greg Eaves, Paul Silver, Marjorie Woodruff, Bethany Hampton, Catherine Judd, Douglas Lisle, Regina Kinney, Maria Marwill-Magee, Andrew Clifford, Martin Schaffer, and Rodger Kobes, also provided clinical support. Research support was provided by Barbara Foster, Michelle White, Edna Christian, Joseph Begue, Julie Lowe, Daisha Cipher, Patricia Green, Demetria Clinton, and Paula Reese. Brian F. Shaw rated the cognitive therapists. We appreciate the administrative support of Eric J. Nestler.
Footnotes
Jarrett et al. (2001) reported n = 87 treatment responders according to ratings made by an independent evaluator at the conclusion of the A–CT protocol and consistent with the focus on participants eligible to enter C–CT (i.e., those who completed the A–CT protocol and the posttreatment assessment in addition to the absence of DSM–IV major depressive disorder and an HRSD ≤ 9). To maximize the generalizability of results in this article, we also include n = 10 patients who did not complete the A–CT protocol but met treatment response criteria as rated by their A–CT therapists in analyses of A–CT response.
Jarrett et al. (2001) reported n = 60 entering the follow-up phase because the data from 14 patients who met criteria for relapse or recurrence of DSM–IV major depressive disorder during the experimental phase were censored. In this article’s analyses, all available data, including those collected after relapse or recurrence, were utilized to maximize the generalizability of findings.
A total of 148 participants completed at-best SASB measures pre-A–CT, and 146 completed at-worst SASB measures pre-A–CT; 106 participants completed at-best measures at 0 months post-A–CT, and 105 completed at-worst measures at 0 months post-A–CT. Missing data were generated primarily by attrition from the A–CT protocol (i.e., 128 of 156 participants persisted to complete portions of the 0 month-post-A–CT assessment) but also by other processes such as patient fatigue. T tests suggested that participants with missing SASB data did not differ from those with complete SASB data on at-best and at-worst affiliation and autonomy pre-A–CT or 0 months post-A–CT, ps > .13, two-tailed. Consequently, for clarity of presentation, we focus on the subset of participants with complete SASB data (N = 100) for analysis of pre- to post-A–CT changes.
Contributor Information
Jeffrey R. Vittengl, Division of Social Science, Truman State University
Lee Anna Clark, Department of Psychology, University of Iowa.
Robin B. Jarrett, Department of Psychiatry, University of Texas Southwestern Medical Center at Dallas
REFERENCES
- Alpher VS. Identity and introject in dissociative disorders. Journal of Consulting and Clinical Psychology. 1996;64:1238–1244. doi: 10.1037//0022-006x.64.6.1238. [DOI] [PubMed] [Google Scholar]
- Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 1994. [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. Guilford; New York: 1979. [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Beck A, Ward C, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Benjamin LS. Structural analysis of social behavior. Psychological Review. 1974;81:392–425. [Google Scholar]
- Benjamin LS. Adding social and intrapsychic descriptors to Axis I of DSM–III. In: Millon T, Klerman GL, editors. Contemporary directions in psychopathology: Toward the DSM–IV. Guilford; New York: 1986. pp. 599–638. [Google Scholar]
- Benjamin LS. An interpersonal view of borderline personality disorder. In: Clarkin J, Marzialli E, Monroe-Blum H, editors. Borderline psychopathology. Guilford; New York: 1992. pp. 161–196. [Google Scholar]
- Benjamin LS. SASB: A bridge between personality theory and clinical psychology. Psychological Inquiry. 1994;5:273–316. [Google Scholar]
- Benjamin LS. A clinician-friendly version of the interpersonal circumplex: Structural Analysis of Social Behavior (SASB) Journal of Personality Assessment. 1996;66:248–266. doi: 10.1207/s15327752jpa6602_5. [DOI] [PubMed] [Google Scholar]
- Benjamin LS. SASB Intrex manual. University of Utah/Intrex; Salt Lake City: 2000. [Google Scholar]
- Benjamin LS, Pugh C. Using interpersonal theory to select effective treatment interventions. In: Livesley WJ, editor. Handbook of personality disorders: Theory, research, and treatment. Guilford; New York: 2001. pp. 414–436. [Google Scholar]
- Benjamin LS, Wonderlich SA. Social perceptions and borderline personality disorder: The relation to mood disorders. Journal of Abnormal Psychology. 1994;103:610–624. doi: 10.1037//0021-843x.103.4.610. [DOI] [PubMed] [Google Scholar]
- Clark LA, Vittengl JR, Kraft D, Jarrett RB. Separate personality traits from states to predict future depression. Journal of Personality Disorders. 2003a;17:152–172. doi: 10.1521/pedi.17.2.152.23990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, Vittengl JR, Kraft D, Jarrett RB. Shared, not unique, components of personality and psychosocial functioning predict depression severity after acute-phase cognitive therapy. Journal of Personality Disorders. 2003b;17:406–430. doi: 10.1521/pedi.17.5.406.22975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Lawrence Erlbaum Associates, Inc; Hillsdale, NJ: 1988. [Google Scholar]
- Gurtman MB. Interpersonal complementarity: Integrating interpersonal measurement with interpersonal models. Journal of Counseling Psychology. 2001;48:97–110. [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry. 1960;23:56–61. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrist RS, Quintana SM, Strupp HH, Henry WP. Internalization of interpersonal process in time-limited dynamic psychotherapy. Psychotherapy. 1994;31:49–57. [Google Scholar]
- Henry WP. Differentiating normal and abnormal personality: An interpersonal approach based on the Structural Analysis of Social Behavior. In: Stack S, Lorr M, editors. Differentiating normal and abnormal personality. Springer; New York: 1994. pp. 316–340. [Google Scholar]
- Henry WP. Structural Analysis of Social Behavior as a common metric for programmatic psychopathology and psychotherapy research. Journal of Consulting and Clinical Psychology. 1996;64:1263–1275. doi: 10.1037//0022-006x.64.6.1263. [DOI] [PubMed] [Google Scholar]
- Hollon SD, Beck AT. Cognitive and cognitive behavioral therapies. In: Lambert MJ, editor. Bergin and Garfield’s handbook of psychotherapy and behavior change. 5th ed. Wiley; New York: 2004. pp. 447–492. [Google Scholar]
- Ichiyama MA, Zucker RA, Fitzgerald HE, Bingham CR. Articulating subtype differences in self and relational experience among alcoholic men using Structural Analysis of Social Behavior. Journal of Consulting and Clinical Psychology. 1996;64:1245–1254. doi: 10.1037//0022-006x.64.6.1245. [DOI] [PubMed] [Google Scholar]
- Ingram RE. Origins of cognitive vulnerability to depression. Cognitive Therapy and Research. 2003;27:77–88. [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Jarrett RB.Cognitive therapy for recurrent unipolar depressive disorder: The continuation/maintenance phase 1989. Unpublished manuscript [Google Scholar]
- Jarrett RB, Basco MR, Risser R, Ramanan J, Marwill M, Kraft D, et al. Is there a role for continuation phase cognitive therapy for depressed outpatients? Journal of Consulting and Clinical Psychology. 1998;66:1036–1040. doi: 10.1037//0022-006x.66.6.1036. [DOI] [PubMed] [Google Scholar]
- Jarrett RB, Kraft D. Prophylactic cognitive therapy for major depressive disorder. In Session: Psychotherapy in Practice. 1997;3:65–79. [Google Scholar]
- Jarrett RB, Kraft D, Doyle J, Foster BM, Eaves GG, Silver PC. Preventing recurrent depression using cognitive therapy with and without a continuation phase: A randomized clinical trial. Archives of General Psychiatry. 2001;58:381–388. doi: 10.1001/archpsyc.58.4.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Junkert-Tress B, Schnierda U, Hartkamp N, Schmitz N, Tress W. Effects of short-term dynamic psychotherapy for neurotic, somatoform, and personality disorders: A prospective 1-year follow-up study. Psychotherapy Research. 2001;11:187–200. [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, et al. The longitudinal interval follow-up evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Lorr M, Strack S. A study of Benjamin’s eight-facet Structural Analysis of Social Behavior (SASB) model. Journal of Clinical Psychology. 1999;55:207–215. doi: 10.1002/(sici)1097-4679(199902)55:2<207::aid-jclp8>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Luke DA, Homon SM. Time and change: Using survival analysis in clinical assessment and treatment evaluation. Psychological Assessment. 1998;10:360–378. [Google Scholar]
- Paivio SC, Bahr LM. Interpersonal problems, working alliance, and outcome in short-term experiential therapy. Psychotherapy Research. 1998;8:392–407. [Google Scholar]
- Paivio SC, Greenberg LS. Resolving "unfinished business": Efficacy of experiential therapy using empty-chair dialogue. Journal of Consulting and Clinical Psychology. 1995;63:419–425. doi: 10.1037//0022-006x.63.3.419. [DOI] [PubMed] [Google Scholar]
- Pincus AL, Dickinson KA, Schut AJ, Castonguay LG, Bedics J. Integrating interpersonal assessment and adult attachment using SASB. European Journal of Psychological Assessment. 1999;15:206–220. [Google Scholar]
- Pincus AL, Gurtman MB, Ruiz MA. Structural Analysis of Social Behavior (SASB): Circumplex analyses and structural relations with the Interpersonal Circle and the Five-Factor Model of personality. Journal of Personality and Social Psychology. 1998;74:1629–1645. [Google Scholar]
- Pincus AL, Newes SL, Dickinson KA, Ruiz MA. A comparison of three indexes to assess the dimensions of Structural Analysis of Social Behavior. Journal of Personality Assessment. 1998;70:145–170. doi: 10.1207/s15327752jpa7001_10. [DOI] [PubMed] [Google Scholar]
- Quintana SM, Meara NM. Internalization of therapeutic relationships in short-term psychotherapy. Journal of Counseling Psychology. 1990;37:123–130. [Google Scholar]
- Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH. The Inventory of Depressive Symptomatology (IDS): Psychometric properties. Psychological Medicine. 1996;26:477–486. doi: 10.1017/s0033291700035558. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Survival analysis. In: Schinka JA, Velicer WF, editors. Handbook of psychology: Research methods in psychology. Vol. 2. Wiley; New York: 2003. pp. 555–580. [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First MB. Structured Clinical Interview for DSM–III–R outpatient version (with psychotic screen) New York State Psychiatric Institute; New York: 1989. [Google Scholar]
- Vittengl JR, Clark LA, Jarrett RB. Interpersonal problems, personality pathology, and social adjustment after cognitive therapy for depression. Psychological Assessment. 2003;15:29–40. doi: 10.1037/1040-3590.15.1.29. [DOI] [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Jarrett RB. Improvement in social-interpersonal functioning after cognitive therapy for recurrent depression. Psychological Medicine. 2004;34:643–658. doi: 10.1017/S0033291703001478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wonderlich S, Klein MH, Council JR. Relationship of social perceptions and self-concept in bulimia nervosa. Journal of Consulting and Clinical Psychology. 1996;64:1231–1237. doi: 10.1037//0022-006x.64.6.1231. [DOI] [PubMed] [Google Scholar]
- Young J, Beck AT. Cognitive Therapy Scale: Rating manual. Center for Cognitive Therapy; Philadelphia: 1980. [Google Scholar]