Abstract
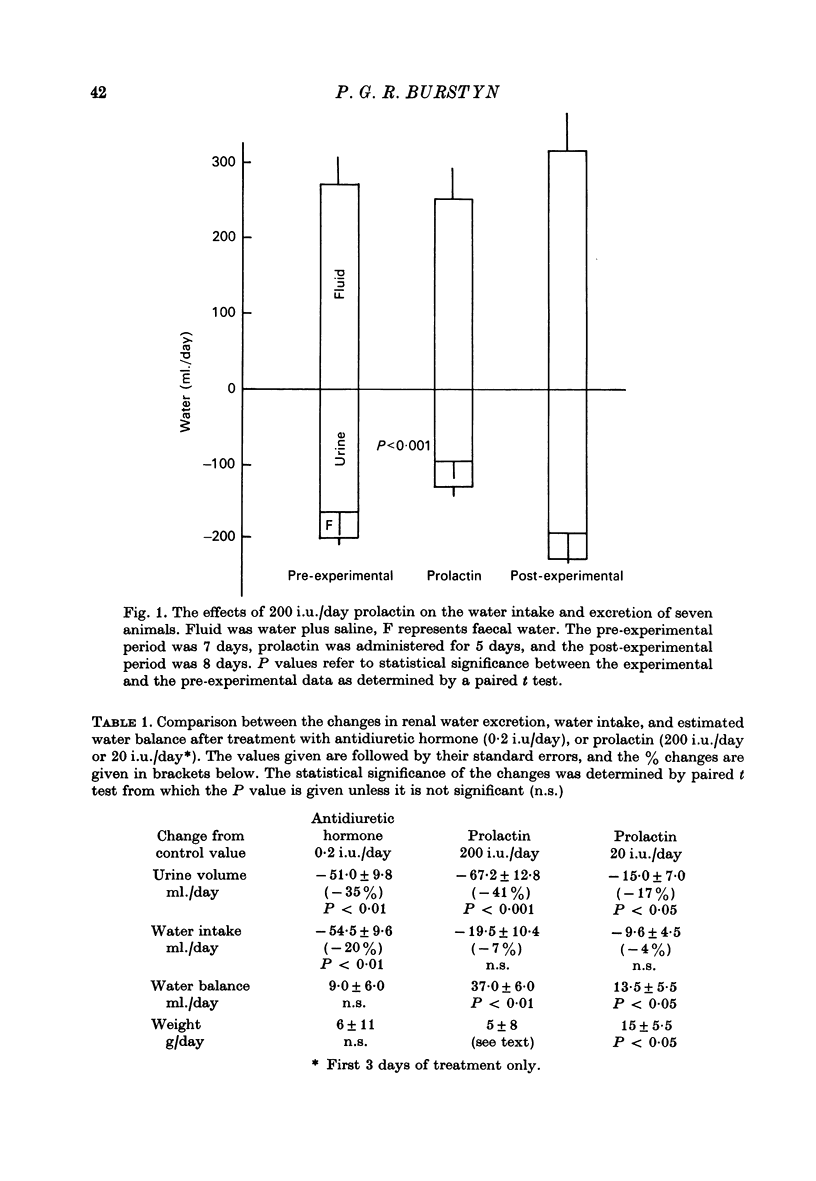
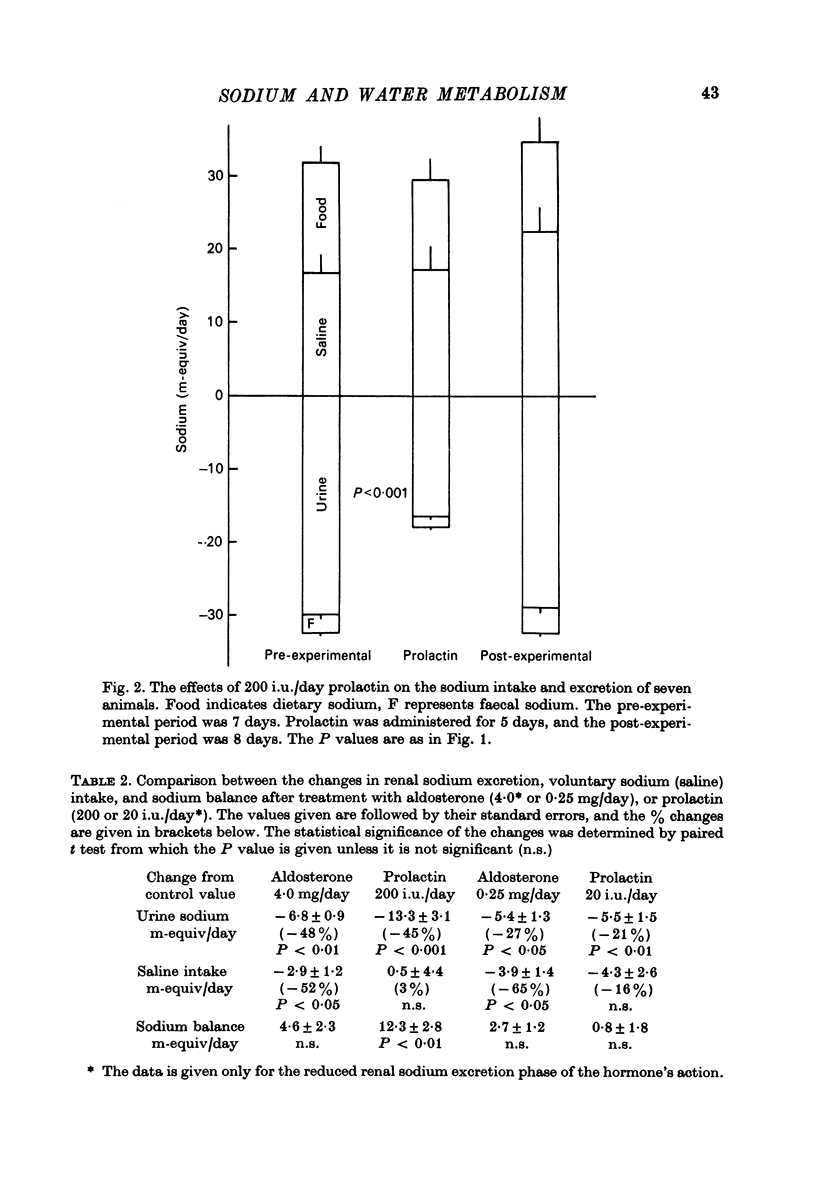
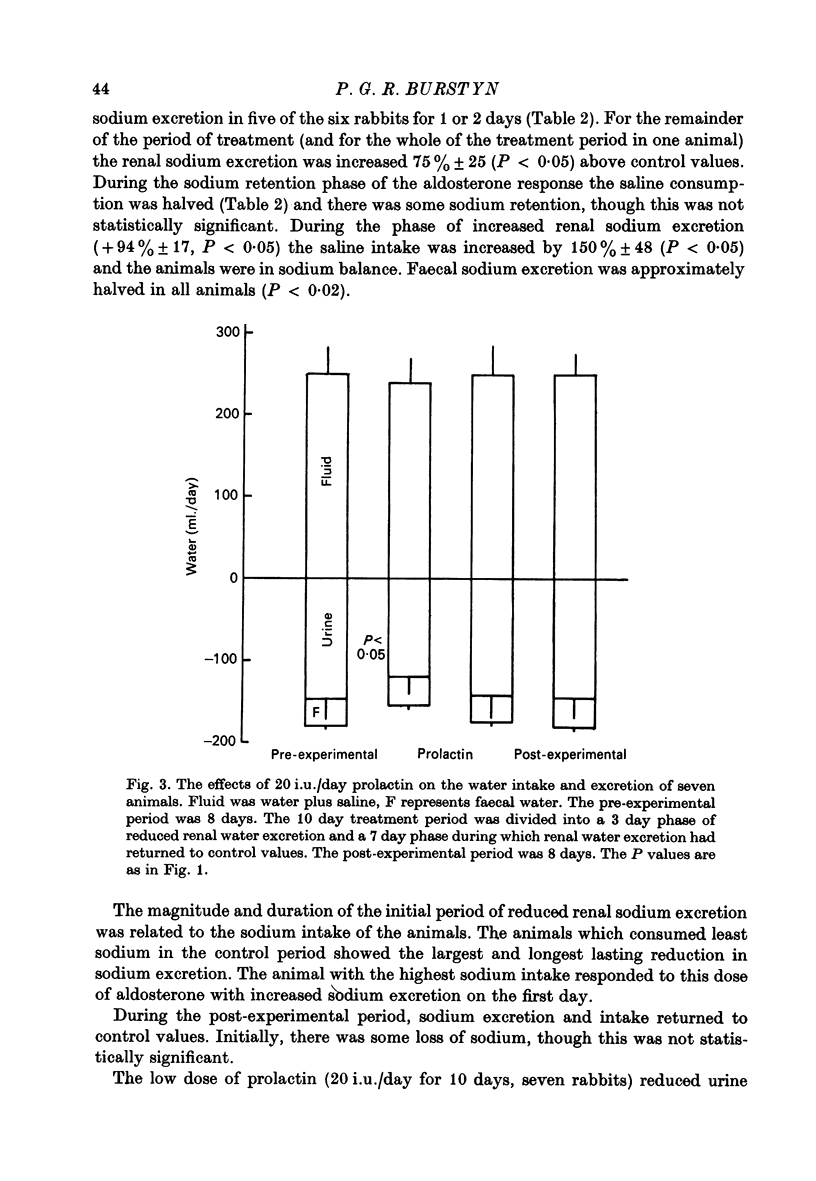
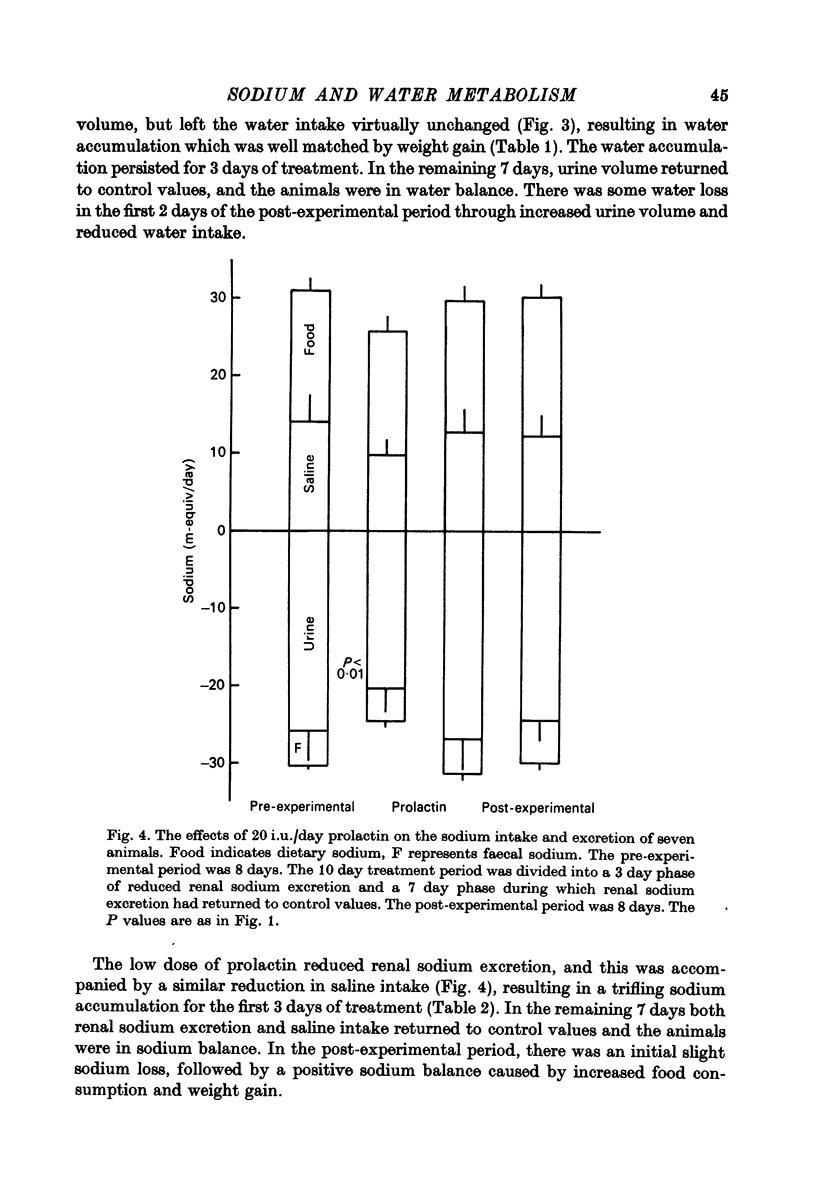
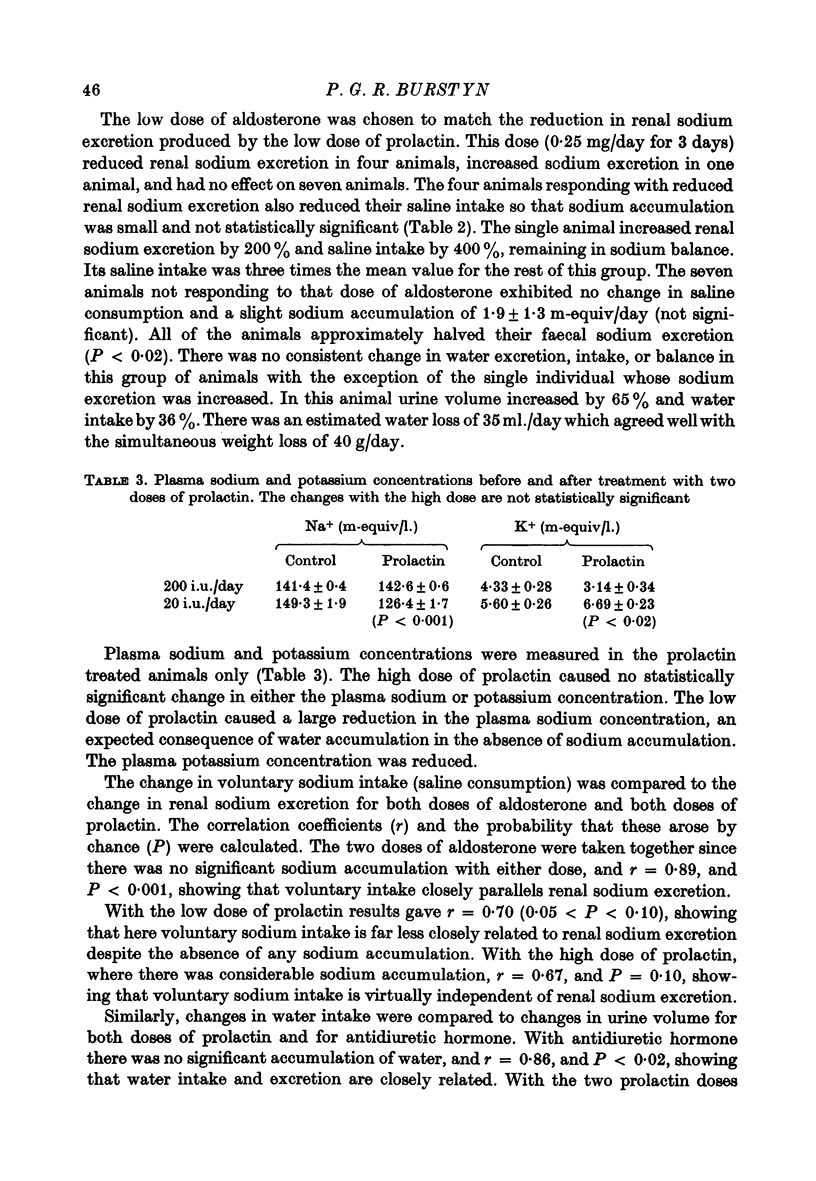
1. Rabbits were placed in metabolism cages in order to measure their intakes of food, water, and sodium chloride (as 1% saline solution), and to measure urinary and faecal excretion of sodium, potassium, and water. 2. Antidiuretic hormone (0.2 i.u./day) caused a reduction in urine volume and no change in sodium excretion. There was full compensatory reduction in water intake so that no accumulation of water occurred. 3. Aldosterone (4 mg/da) caused a reduction in renal sodium excretion for 1--2 days. The saline intake was reduced, though this was insufficient to prevent some sodium accumulation. 4. Renal mineralocorticoid 'escape' resulted in a large increase in sodium excretion at the end of the aldosterone treatment period. This was fully compensated through increased saline intake, and balance was maintained. 5. Prolactin (200 i.u./day) caused a reduction in urine volume and in renal sodium excretion and since there were no compensatory changes in water and sodium intake, this led to substantial accumulation of both water and sodium. 6. The effects of smaller doses of both aldosterone and prolactin were investigated and found to be similar but smaller. 7. It is suggested that whereas prolactin may have little or no role to play in the sodium homoeostasis of the normal animal, the hormone may well be responsible for the substantial increase in body fluids in pregnancy.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- AUGUST J. T., NELSON D. H., THORN G. W. Response of normal subjects to large amounts of aldosterone. J Clin Invest. 1958 Nov;37(11):1549–1555. doi: 10.1172/JCI103747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adler R. A., Noel G. L., Wartofsky L., Frantz A. G. Failure of oral water loading and intravenous hypotonic saline to suppress plasma prolactin in man. J Clin Endocrinol Metab. 1975 Aug;41(2):383–389. doi: 10.1210/jcem-41-2-383. [DOI] [PubMed] [Google Scholar]
- Berl T., Brautbar N., Ben-David M., Czaczkes W., Kleeman C. Osmotic control of prolactin release and its effect on renal water excretion in man. Kidney Int. 1976 Aug;10(2):158–163. doi: 10.1038/ki.1976.90. [DOI] [PubMed] [Google Scholar]
- Berle P., Apostolakis M. Prolaktin-konzentrationen im menschlichen Plasma während Schwangerschaft und Wochenbett. Acta Endocrinol (Copenh) 1971 May;67(1):63–72. [PubMed] [Google Scholar]
- Buckman M. T., Kaminsky N., Conway M., Peake G. T. Utility of L-dopa and water loading in evaluation of hyperprolactinemia. J Clin Endocrinol Metab. 1973 May;36(5):911–919. doi: 10.1210/jcem-36-5-911. [DOI] [PubMed] [Google Scholar]
- Buckman M. T., Peake G. T. Osmolar control of prolactin secretion in man. Science. 1973 Aug 24;181(4101):755–757. doi: 10.1126/science.181.4101.755. [DOI] [PubMed] [Google Scholar]
- Burstyn P. G., Horrobin D. F., Manku M. S. Saluretic action of aldosterone in the presence of increased salt intake and restoration of normal action by prolactin or by oxytocin. J Endocrinol. 1972 Nov;55(2):369–376. doi: 10.1677/joe.0.0550369. [DOI] [PubMed] [Google Scholar]
- Burstyn P. G., McKillop W., Lloyd I. J. The effects of prolactin on the renal excretion of water, sodium, potassium and calcium in the rabbit. ICRS J Int Res Commun. 1974 Aug;2(8):1474–1474. [PubMed] [Google Scholar]
- Campbell D. M., MacGillivray I. Comparison of maternal response in first and second pregnancies in relation to baby weight. J Obstet Gynaecol Br Commonw. 1972 Aug;79(8):684–693. doi: 10.1111/j.1471-0528.1972.tb12901.x. [DOI] [PubMed] [Google Scholar]
- GRAY M. J., MUNRO A. B., SIMS E. A., MEEKER C. I., SOLOMON S., WATANABE M. REGULATION OF SODIUM AND TOTAL BODY WATER METABOLISM IN PREGNANCY. Am J Obstet Gynecol. 1964 Jul 15;89:760–765. doi: 10.1016/0002-9378(64)90179-6. [DOI] [PubMed] [Google Scholar]
- GROSS F., SCHMIDT H. Aldosterone overdosage in the rabbit. Acta Endocrinol (Copenh) 1958 Aug;28(4):467–478. doi: 10.1530/acta.0.0280467. [DOI] [PubMed] [Google Scholar]
- HERXHEIMER A., WOODBURY D. M. The effect of deoxycorticosterone on salt and sucrose taste preference thresholds and drinking behaviour in rats. J Physiol. 1960 May;151:253–260. doi: 10.1113/jphysiol.1960.sp006435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall C. E., Hall O. Interaction between desoxycorticosterone treatment, fluid intake, sodium consumption, blood pressure, and organ changes in rats drinking water, saline, or surcose solution. Can J Physiol Pharmacol. 1969 Jan;47(1):81–86. doi: 10.1139/y69-013. [DOI] [PubMed] [Google Scholar]
- Horrobin D. F., Lloyd I. J., Lipton A., Burstyn P. G., Durkin N., Muiruri K. L. Actions of prolactin on human renal function. Lancet. 1971 Aug 14;2(7720):352–354. doi: 10.1016/s0140-6736(71)90065-1. [DOI] [PubMed] [Google Scholar]
- Lockett M. F. A comparison of the direct renal actions of pituitary growth and lactogenic hormones. J Physiol. 1965 Nov;181(1):192–199. doi: 10.1113/jphysiol.1965.sp007754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lockett M. F., Nail B. A comparative study of the renal actions of growth and lactogenic hormones in rats. J Physiol. 1965 Sep;180(1):147–156. [PMC free article] [PubMed] [Google Scholar]
- NEWMAN R. L. Serum electrolytes in pregnancy, parturition, and puerperium. Obstet Gynecol. 1957 Jul;10(1):51–55. [PubMed] [Google Scholar]
- Shulkes A. A., Covelli M. D., Denton D. A., Nelson J. F. Hormonal factors influencing salt appetite in lactation. Aust J Exp Biol Med Sci. 1972 Dec;50(7):819–826. doi: 10.1038/icb.1972.79. [DOI] [PubMed] [Google Scholar]
- TATUM H. J. Blood volume variation during labor and early puerperium. Am J Obstet Gynecol. 1953 Jul;66(1):27–35. doi: 10.1016/0002-9378(53)90282-8. [DOI] [PubMed] [Google Scholar]
- Tyson J. E., Hwang P., Guyda H., Friesen H. G. Studies of prolactin secretion in human pregnancy. Am J Obstet Gynecol. 1972 May 1;113(1):14–20. doi: 10.1016/0002-9378(72)90446-2. [DOI] [PubMed] [Google Scholar]
- Weisinger R. S., Woods S. C. Aldosterone-elicited sodium appetite. Endocrinology. 1971 Aug;89(2):538–544. doi: 10.1210/endo-89-2-538. [DOI] [PubMed] [Google Scholar]
- Wolf G., Handal P. J. Aldosterone-induced sodium appetite: dose-response and specificity. Endocrinology. 1966 Jun;78(6):1120–1124. doi: 10.1210/endo-78-6-1120. [DOI] [PubMed] [Google Scholar]


