Abstract
Objective To test whether improvement in household coal stoves affected the incidence of chronic obstructive pulmonary disease (COPD) in Xuanwei County, China.
Design Retrospective cohort study (follow-up 1976-92) comparing incidence of COPD between groups with and without chimneys.
Participants 20 453 people born into homes with unvented coal stoves;16 606 (81.2%) subsequently changed to stoves with chimneys.
Intervention Installation of a chimney in households in which unvented stoves had been used previously.
Results Installation of a chimney was associated with distinct reduction in the incidence of COPD. Compared with people who did not have chimneys, the Cox-modelled risk ratio (relative risk) was 0.58 (95% confidence interval 0.49 to 0.70, P < 0.001) in men and 0.75 (0.62 to 0.92, P = 0.005) in women. Modelled risk ratios were robust to different Cox model specifications. Relative risks decreased with time since stove improvement. In both sexes, the reduction in risk became unequivocal about 10 years after stove improvement.
Conclusions In Xuanwei, incidence of COPD decreased markedly after household coal stoves were improved.
Introduction
Burning coal and biomass fuels on unvented stoves causes much disease in developing countries. Such fuel is the domestic energy source for almost 3 billion people,1 and the resulting smoke contributes importantly to the global burden of mortality, accounting for about 1.6 million of the 59 million deaths annually.2,3 Indoor smoke is estimated as the eighth largest risk factor for global disease, accounting for 2.7% of disability adjusted life years lost (DALYs).2,3 Chronic obstructive pulmonary disease (COPD) is a major component of global disease, and the World Health Organization estimated that COPD was the sixth leading contributor to worldwide mortality in 1990. By 2020 they estimate that it will be the third leading contributor.4 Exposure to smoke from solid fuel burned indoors is strongly associated with an increased risk of COPD and other respiratory disorders.5-13
In Xuanwei County, Yunnan Province, China, rates of lung cancer were among the highest in China,14 and rates of COPD were over twice the national average.15 In Xuanwei > 90% of residents are farmers.16 Most men, but few women, smoke. Nearly all women, and some men, cook food on the household stove. For cooking and heating, residents usually burned smoky coal (bituminous coal), smokeless coal (anthracite), or wood in unvented stoves. Unvented burning of smoky coal generates high concentrations of indoor air pollution.14,17 In Xuanwei, rates of lung cancer14,16 and COPD15 are strongly associated with household use of smoky coal.
Most Xuanwei residents have changed from unvented stoves to stoves with chimneys. This greatly reduces indoor air pollution and was associated with a reduction in risk of lung cancer.16 To the best of our knowledge, the effects on risk of COPD have not previously been documented, though we would expect that the incidence would decrease.18 We therefore compared incidence of COPD between people who installed chimneys and those who used only unvented stoves.
Methods
Data collection
We searched administrative records to identify all farmers born 1917-51 who were living in Xuanwei's three central communes (the study area) on 1 January 1976 (31 364 farmers in all). From 1976-92, 1215 (3.9%) moved away and were not included in analysis. From March-November 1992, trained interviewers administered a standardised questionnaire to the 30 149 remaining. They determined history of household stove and fuel use, diagnosed illnesses, smoking, cooking food, time spent indoors and outdoors, education, and residence. Participants were asked whether they had ever been diagnosed with chronic bronchitis or emphysema and, if so, the age and place of diagnosis (hospitals at the province, district, county, or commune level). Chronic bronchitis and emphysema were combined into a single category of COPD. Dates of all deaths from 1976-92 were taken from death certificates. Written informed consent was obtained from all literate respondents. Study goals and procedures were explained orally to each eligible illiterate person, in the presence of a literate relative. If this person gave oral consent, the relative signed the consent form for that person.
Data analysis
We restricted analysis to lifelong users of smoky coal (causing 2836 exclusions) and those who had used unvented stoves throughout their lives or who changed from unvented stoves to stoves with chimneys (5861 exclusions). We also excluded eight people because of coding errors on the questionnaire, 217 patients with COPD who did not specify a place of diagnosis (n = 189) or who had both COPD and lung cancer and in whom COPD was diagnosed after lung cancer (n = 28). Follow-up started on 1 January 1976, resulting in exclusion of 774 COPD patients diagnosed before that date. Thus the final dataset included 20 453 subjects (10 785 men and 9668 women), of whom 1487 (7.3%) had COPD and 16 606 (81.2%) had installed chimneys.
We counted age at entry into follow-up as the number of days from birth date to 1 January 1976, divided by 365.25. People left follow-up by reporting they had received a diagnosis of COPD (integer age at diagnosis +0.5), if they died without COPD during follow-up (number of days from birth date to death date, divided by 365.25), or if they were alive and free of COPD at interview in 1992 (number of days from birth date to interview date, divided by 365.25).
There were 298 378 person years during follow-up (116 221 before installing a chimney and 182 157 after). We calculated incidence rates of COPD adjusted for age before and after installation. Product-limit survival curves, with incident COPD as outcome, were plotted by age for men and women with and without a chimney (SAS, SAS Institute, Cary, NC).
We used sex specific multivariable Cox models, with incident COPD as outcome. The time axis was age. Stove improvement was assessed with a time dependent variable that switched from zero to one when the person changed to a stove with chimney. This gave a modelled overall risk ratio (relative risk) for COPD of stove improvement compared with no improvement. The models also used various dummy variables: having ≥5 people in the household at exit from follow-up; spending ≥7 daily waking hours indoors up to age 20; using an annual average of > 3 tonnes of coal in the household; being born outside the study area; having any education; having ≥3 rooms in the home at exit from follow-up; and six dummies for the birth cohorts of 1922-6, 1927-31, 1932-6, 1937-41, 1942-6, and 1947-51 (compared with 1917-21). These variables were constructed exactly as in our previous analysis16 to enable comparison of their effects on incidence of lung cancer and COPD.
The men's model included three time dependent variables for pack years of smoking (20-29, 30-39, and ≥40 pack years, relative to < 20 pack years); a time dependent variable for cooking food for ≥20 years, relative to < 20 years; and a dummy for ever being a coal miner. The women's model included three time dependent variables for how long they had been cooking food (20-29, 30-39, and ≥40 years of cooking, relative to < 20 years). Few of the women (< 1%) had ever smoked, so we did not adjust the women's model for smoking. During this study, rural Chinese communes were typically subdivided into “large teams.” Extended families were generally concentrated in single teams. To control for potential non-independence from family related clustering we stratified models on large teams.
We used additional Cox models for sensitivity analyses. One model included a dummy for history of lung cancer. Another included all the covariates in the main model plus dummies for history of lung cancer, questionnaire respondent (1 if answered for self, 0 if surrogate respondent), and digit preference in reported age at COPD diagnosis (1 if a multiple of 10, 0 otherwise). The main model was run after we excluded patients with lung cancer and replaced several categorical covariates with continuous ones. An additional model used a time axis of calendar time (not age), with adjustment for age at entry. To evaluate potential effects of error in recall of age at installation of a chimney, we ran the main model after addition and subtraction of 5 years from this age as reported.
We also used Cox models to assess the change in incidence of COPD over time after installation of a chimney. We assigned people who changed to a stove with a chimney < 10 years, 10-19 years, and ≥20 years before leaving follow-up to separate groups. For each group we entered a time dependent variable that switched from zero to one at stove improvement. This gave a modelled relative risk for stove improvement in each group compared with 1 for no improvement. These models were run on the entire cohort, then with successive exclusion of those who left follow-up within one year, two years, three years, and four years after improvement.
Results
Table 1 summarises details of the participants. The age adjusted incidence rate of COPD was distinctly higher in people without chimneys than in those with chimneys, as was the overall mortality and mortality from COPD. Mean educational attainment was at the level of primary school (up to the age of about 11 years). Men were better educated than women, as were people who had chimneys. Smoking was similar in men with and without chimneys. Prevalence of cooking was higher in men without chimneys. Among men who cooked, how long they had been cooking and at what age they started to cook were similar in those with and without chimneys. Only 10 people were born outside Xuanwei.
Table 1.
Characteristics of participants by history of stove use, Xuanwei, 1976-92. Figures are numbers (percentages) or means (95% confidence intervals)
| No stove improvement | Changed to stove with chimney | Total | |
|---|---|---|---|
| Men and women combined | |||
| Total | 3847 | 16 606 | 20 453 |
| Age on 1 January 1976 | 41.8 (41.4 to 42.1) | 37.9 (37.7 to 38.0) | 38.6 (38.5 to 38.8) |
| Age at exit from follow-up | 52.5 (52.2 to 52.9) | 53.3 (53.2 to 53.5) | 53.2 (53.1 to 53.3) |
| Diagnosis of COPD, 1976-92 | 746 (19.4) | 741 (4.5) | 1487 (7.3) |
| Age adjusted incidence of COPD/100 000 person years | 767 | 367 | 498 |
| Chronic bronchitis, no emphysema (% of all COPD) | 574 (76.9) | 536 (72.3) | 1110 (74.6) |
| Emphysema, no chronic bronchitis (% of all COPD) | 86 (11.5) | 154 (20.8) | 240 (16.1) |
| Chronic bronchitis and emphysema (% of all COPD) | 86 (11.5) | 51 (6.9) | 137 (9.2) |
| Died with COPD during follow-up | 437 (11.4) | 433 (2.6) | 870 (4.3) |
| Died without COPD during follow-up | 1383 (36.0) | 2093 (12.6) | 3476 (17.0) |
| Alive and free of COPD in 1992 | 1718 (44.7) | 13 772 (82.9) | 15 490 (75.7) |
| Age at diagnosis of COPD | 49.7 (48.9 to 50.4) | 53.6 (52.9 to 54.3) | 51.6 (51.1 to 52.1) |
| Age at stove improvement | — | 41.6 (41.4 to 41.7) | 41.6 (41.4 to 41.7) |
| Time from stove improvement until exit from follow-up | — | 11.8 (11.7 to 11.8) | 11.8 (11.7 to 11.8) |
| No of people in household | 5.3 (5.3 to 5.4) | 5.1 (5.1 to 5.1) | 5.2 (5.1 to 5.2) |
| Born in 1937-51 | 1675 (43.5) | 9654 (58.1) | 11 329 (55.4) |
| History of lung cancer | 607 (15.8) | 740 (4.5) | 1347 (6.6) |
| Spent ≥7 waking hours indoors/day up to age 20 | 2388 (62.1) | 10 945 (65.9) | 13 333 (65.2) |
| Used average >3 tonnes of fuel/year | 1625 (42.2) | 11 331 (68.2) | 12 956 (63.3) |
| No of rooms in home | 1.8 (1.8 to 1.9) | 1.7 (1.70 to 1.73) | 1.7 (1.7 to 1.8) |
| Men only | |||
| Total | 2047 (100.0)‡ | 8738 (100.0) | 10 785 (100.0) |
| Diagnosis of COPD, 1976-92 | 421 (20.6) | 371 (4.2) | 792 (7.3) |
| Had any education | 826 (40.4) | 4286 (49.1) | 5112 (47.4) |
| Born outside study area | 18 (0.9) | 80 (0.9) | 98 (0.9) |
| Ever been a coal miner | 154 (7.5) | 860 (9.8) | 1014 (9.4) |
| Ever smoked tobacco | 1805 (88.2) | 8107 (92.3) | 9912 (91.9) |
| Years of smoking in smokers | 32.3 (31.8 to 32.8) | 31.9 (31.6 to 32.1) | 31.9 (31.7 to 32.2) |
| Age at starting to smoke (years) | 21.3 (21.1 to 21.5) | 21.6 (21.5 to 21.7) | 21.5 (21.5 to 21.6) |
| Total pack years | 29.7 (28.7 to 30.7) | 31.9 (31.5 to 32.4) | 31.5 (31.1 to 31.9) |
| No of cigarettes (+ tobacco equivalents) smoked/day | 17.7 (17.3 to 18.2) | 19.3 (19.1 to 19.5) | 19.0 (18.8 to 19.2) |
| Ever quit smoking | 33 (1.6) | 118 (1.4) | 151 (1.4) |
| Ever cooked food | 313 (15.3) | 644 (7.4) | 957 (8.9) |
| Years of cooking in men who cooked | 28.2 (26.7 to 29.8) | 27.3 (26.2 to 28.4) | 27.6 (26.7 to 28.5) |
| Age at starting to cook | 25.8 (24.2 to 27.4) | 28.0 (26.8 to 29.2) | 27.3 (26.3 to 28.3) |
| Women only | |||
| Total | 1800 (100.0)‡ | 7868 (100.0) | 9668 (100.0) |
| Diagnosis of COPD, 1976-92 | 325 (18.1) | 370 (4.7) | 695 (7.2) |
| Had any education | 375 (20.8) | 1971 (25.1) | 2346 (24.3) |
| Born outside study area | 241 (13.4) | 1023 (13.0) | 1264 (13.1) |
| Ever smoked tobacco | 22 (1.2) | 61 (0.8) | 83 (0.9) |
| Ever cooked food | 1744 (96.9) | 7696 (97.8) | 9440 (97.6) |
| Years of cooking in women who cooked | 36.6 (36.1 to 37.1) | 34.5 (34.3 to 34.8) | 34.9 (34.7 to 35.1) |
| Age at starting to cook | 17.0 (16.8 to 17.2) | 18.1 (18.1 to 18.2) | 17.9 (17.9 to 18.0) |
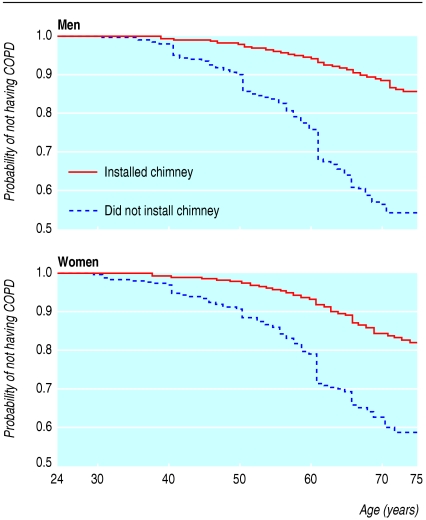
The figure shows product limit curves of incidence of COPD in men and women according to stove improvement. Age specific proportions of people without COPD were consistently higher in those with chimneys than in those without. In both sexes, differences between curves were highly significant (P < 0.001 in Wilcoxon, log rank, and likelihood ratio χ2 tests). Among all those with COPD, 514 (34.6%) reported age at diagnosis as an exact multiple of 10, whereas only 1791 without COPD (9.4%) left follow-up at such an age.
Figure 1.
Product limit survival plots showing probability of not having chronic obstructive pulmonary disease (COPD) by age in years in men and women according to whether they had a chimney, Xuanwei, 1976-92
Tables 2 and 3 show the risk ratios (with 95% confidence intervals and P values) from the main Cox model for overall incidence rate of COPD. In both men and women, using a stove with a chimney was distinctly and significantly associated with a reduction in the incidence of COPD. This reduction was more pronounced in men (42% reduction, P < 0.001) than in women (25% reduction, P = 0.005). In both sexes, living in a household of ≥5 people and spending ≥7 daily waking hours indoors up to the age of 20 were significantly associated with increased incidence of COPD. Using > 3 tonnes of fuel annually, being born outside the study area, and having ≥3 rooms in the home were not appreciably associated with the incidence. In men, smoking was significantly associated with increased incidence (1.45 for ≥40 pack years, P = 0.007 overall, table 3). In women, duration of cooking was not significantly associated with incidence (table 3).
Table 2.
Stratified main Cox model risk ratios (relative risks) for chronic obstructive pulmonary disease (COPD) incidence rate, by sex, Xuanwei, 1976-92
|
Men*
|
Women*
|
|||
|---|---|---|---|---|
| Independent variables | Relative risk (95% CI)† | P value | Relative risk (95% CI)† | P value |
| No stove improvement‡v changed to stove with chimney | 0.58 (0.49 to 0.70) | <0.001 | 0.75 (0.62 to 0.92) | 0.005 |
| <5‡v ≥5 people in household | 1.58 (1.33 to 1.88) | <0.001 | 1.57 (1.31 to 1.88) | <0.001 |
| <7‡v ≥7 waking hours/day indoors to age 20 | 1.34 (1.12 to 1.59) | 0.001 | 1.82 (1.49 to 2.22) | <0.001 |
| Used annual average ≤3‡v >3 tonnes of fuel | 1.14 (0.96 to 1.35) | 0.136 | 1.01 (0.83 to 1.21) | 0.960 |
| Born in study area‡v born outside study area | 1.27 (0.62 to 2.59) | 0.508 | 1.16 (0.92 to 1.47) | 0.203 |
| No education‡v education | 0.87 (0.74 to 1.02) | 0.089 | 0.93 (0.74 to 1.18) | 0.564 |
| <3 rooms‡v ≥3 rooms in home | 1.01 (0.82 to 1.26) | 0.901 | 0.93 (0.73 to 1.18) | 0.527 |
| Birth cohort effects (born in 1917-21‡v all others): | ||||
| 1922-6
|
0.73 (0.56 to 0.95)
|
<0.001 | 0.71 (0.54 to 0.94)
|
<0.001 |
| 1927-31
|
0.57 (0.42 to 0.78)
|
0.49 (0.36 to 0.67)
|
||
| 1932-6
|
0.50 (0.34 to 0.72)
|
0.53 (0.36 to 0.78)
|
||
| 1937-41
|
0.43 (0.28 to 0.66)
|
0.41 (0.26 to 0.64)
|
||
| 1942-6
|
0.30 (0.18 to 0.49)
|
0.26 (0.15 to 0.44)
|
||
| 1947-51 | 0.41 (0.24 to 0.69) | 0.26 (0.14 to 0.46) | ||
Men: 157 239.4 person years during follow-up (61 543.6 before stove improvement and 95 695.9 after it). Women: 141 138.1 person years (54 677.0 before stove improvement and 86 461.1 after it). Among the 116 220.6 person years before improvement, 41 466.4 (35.7%) were in people who never had improved stoves, and 74 754.2 (64.3%) were in people with improved stoves, but before they were improved.
Likelihood ratio χ2 statistics for both models were 157.2 (18 df, P<0.001) for men and 129.8 (16 df, P<0.001) for women. There were 792 diagnosed COPD cases in men (7.3%) and 695 in women (7.2%).
Reference category (relative risk=1).
Table 3.
Stratified main Cox model risk ratios (relative risks) for incidence rate of chronic obstructive pulmonary disease (COPD), for smoking, occupation, and cooking Xuanwei, 1976-92
| Independent variables | Relative risk (95% CI) | P value |
|---|---|---|
| Men only | ||
| Amount of smoking (<20*†‡ pack years v all others): | ||
| 20-29‡
|
1.16 (0.93 to 1.44)
|
0.007 |
| 30-39‡
|
0.97 (0.73 to 1.29)
|
|
| ≥40‡ | 1.45 (1.14 to 1.86) | |
| Cooked food <20 years*‡§v ≥20 years | 0.95 (0.72 to 1.27) | 0.748 |
| Never a coal miner*v ever a coal miner | 1.22 (0.93 to 1.61) | 0.160 |
| Women only | ||
| Amount of cooking (cooked food <20 years*‡§v all others): | ||
| 20-29‡
|
1.07 (0.74 to 1.55)
|
0.602 |
| 30-39‡
|
1.09 (0.73 to 1.62)
|
|
| ≥40‡ | 1.31 (0.83 to 2.07) |
Reference category (relative risk=1).
Includes non-smokers.
Time dependent number of pack years of men's smoking, duration of men's cooking, and duration of women's cooking, from age at starting to smoke or cook to age at each successive risk set comparison.
Includes people who did not cook food.
Table 4 shows modelled risk ratios of stove improvement for incidence of COPD in alternative Cox models. In both sexes, the risk ratios were stable with different model specifications, and relative risks, confidence intervals, and P values were similar when we excluded all patients with lung cancer.
Table 4.
Cox model risk ratios (relative risks) of stove improvement (v no stove improvement*) for incidence rate of chronic obstructive pulmonary disease (COPD), with different model specifications, by sex, Xuanwei, 1976-92
|
Men
|
Women
|
|||
|---|---|---|---|---|
| Model specification | Relative risk (95% CI) | P value | Relative risk (95% CI) | P value |
| Main model with additional covariate for lung cancer† | 0.59 (0.49 to 0.70) | <0.001 | 0.76 (0.62 to 0.92) | 0.005 |
| Expanded model‡ | 0.58 (0.49 to 0.70) | <0.001 | 0.79 (0.65 to 0.97) | 0.021 |
| Time axis=calendar time, not age§ | 0.56 (0.46 to 0.68) | <0.001 | 0.76 (0.62 to 0.92) | 0.006 |
| Main model, excluding all lung cancer patients | 0.60 (0.50 to 0.73) | <0.001 | 0.80 (0.65 to 0.98) | 0.032 |
| Main model, substituting continuous for categorical covariates¶ | 0.59 (0.49 to 0.71) | <0.001 | 0.77 (0.64 to 0.94) | 0.010 |
| Main model, +5 years to reported age at stove improvement | 0.65 (0.53 to 0.78) | <0.001 | 0.80 (0.65 to 0.97) | 0.025 |
| Main model, −5 years from reported age at stove improvement | 0.50 (0.41 to 0.60) | <0.001 | 0.62 (0.51 to 0.77) | <0.001 |
Reference category, relative risk=1.
Dummy variable, equals 1 when subject had lung cancer, 0 otherwise.
Main model plus dummy variables for lung cancer, questionnaire respondent status (equals 1 when responded for self, 0 otherwise), and digit preference for reported age at COPD diagnosis (equals 1 when integer age at exit from follow-up was an exact multiple of 10, 0 otherwise).
Adjusted for age at entry into follow-up, no covariates for birth cohorts, otherwise same as main model.
Models included continuous covariates for years of cooking, average daily waking hours spent indoors before age 20, average tonnes of fuel used annually, numbers of rooms and people in home, year of birth, and pack years of smoking (men only).
Table 5 shows the analyses of the reduction in the risk of COPD over time after installation of a chimney. Risks consistently decreased with length of time since installation. In men and women who left follow-up within 10 years after installation, modelled relative risks were significantly higher than 1. This was observed until we excluded from analysis men and women who left follow-up within three and four years, respectively, after installation. Stove improvement was consistently associated with highly significant reduction in incidence of COPD in people who left follow-up ≥10 years after improvement (P < 0.001).
Table 5.
Cox model risk ratios (relative risks) for incidence rate of COPD, by time from stove improvement until leaving follow-up, when excluding subjects with successively longer times after improvement, Xuanwei, 1976-92
|
Men
|
Women
|
|||
|---|---|---|---|---|
| Exclusions | Relative risk (95% CI)* | Person years | Relative risk (95% CI)* | Person years |
| None (all subjects analysed) | ||||
| No stove improvement | 1 | 61 544* | 1 | 54 677* |
| 0-10 years after improvement | 1.89 (1.56 to 2.29) | 21 777† | 2.37 (1.93 to 2.92) | 19 802† |
| 10-19 years after improvement | 0.20 (0.16 to 0.26) | 65 409† | 0.26 (0.20 to 0.34) | 58 457† |
| ≥20 years after improvement | 0.10 (0.05 to 0.20) | 8 509† | 0.13 (0.07 to 0.26) | 8 202† |
| Left follow-up ≤1 year after stove improvement | ||||
| No stove improvement | 1 | 60 905* | 1 | 54 103* |
| 0-10 years after improvement | 1.47 (1.20 to 1.81) | 21 723† | 1.75 (1.41 to 2.18) | 19 754† |
| 10-19 years after improvement | 0.19 (0.15 to 0.25) | 65 409† | 0.23 (0.18 to 0.31) | 58 457† |
| ≥20 years after improvement | 0.09 (0.04 to 0.18) | 8 509† | 0.12 (0.06 to 0.23) | 8 202† |
| Left follow-up ≤2 years after stove improvement | ||||
| No stove improvement | 1 | 60 092* | 1 | 53 253* |
| 0-10 years after improvement | 1.28 (1.03 to 1.58) | 21 559† | 1.55 (1.24 to 1.95) | 19 603† |
| 10-19 years after improvement | 0.18 (0.14 to 0.24) | 65 409† | 0.23 (0.17 to 0.30) | 58 457† |
| ≥20 years after improvement | 0.08 (0.04 to 0.17) | 8 509† | 0.11 (0.06 to 0.22) | 8 202† |
| Left follow-up ≤3 years after stove improvement | ||||
| No stove improvement | 1 | 58 867* | 1 | 52 224* |
| 0-10 years after improvement | 1.10 (0.88 to 1.37) | 21 155† | 1.31 (1.04 to 1.66) | 19 278† |
| 10-19 years after improvement | 0.18 (0.14 to 0.23) | 65 409† | 0.21 (0.16 to 0.28) | 58 457† |
| ≥20 years after improvement | 0.08 (0.04 to 0.17) | 8 509† | 0.10 (0.05 to 0.21) | 8 202† |
| Left follow-up ≤4 years after stove improvement | ||||
| No stove improvement | 1 | 57 448* | 1 | 50 930* |
| 0-10 years after improvement | 0.81 (0.64 to 1.03) | 20 530† | 1.02 (0.80 to 1.32) | 18 710† |
| 10-19 years after improvement | 0.17 (0.13 to 0.22) | 65 409† | 0.21 (0.16 to 0.27) | 58 457† |
| ≥20 years after improvement | 0.08 (0.04 to 0.16) | 8 509† | 0.10 (0.05 to 0.20) | 8 202† |
Includes person years in people who never had improved stoves and in people with improved stoves, but before they were improved.
Person years after stoves improved.
Discussion
We observed a substantial reduction in the incidence rate of COPD after installation of chimneys on household coal stoves in a rural province of China. The reduction in incidence was lower in women than in men, probably because a much higher proportion of women cook food and they start to cook at a much younger age and cook for longer, thus being exposed to more long term indoor air pollution at higher doses, both before and after installation of a chimney. Furthermore, even after installation, the average concentration of airborne particles ≤10 μm in diameter was still quite high near the stove (710 μg/m3).16
Possible limitations
Our outcome variable was incidence rate of self reported diagnosis of COPD, and we did not compare these self reports with physicians' records. Though self reporting creates some uncertainty in the outcome and might bias results, we doubt this for two reasons. Firstly, we excluded people who reported COPD but did not specify the place of diagnosis. Secondly, presence of chronic bronchitis was strongly positively associated with presence of lung cancer (P < 0.001 by χ2 test) but presence of emphysema was not (P = 0.649). This is consistent with the findings of Kishi et al, who observed a positive and significant association of the risk of lung cancer with airways obstruction but no such association with emphysema.19
Lung cancer could be misclassified as COPD, but we doubt whether appreciable misclassification occurred in this study. As expected, mortality was lower in people with COPD than in people with lung cancer (58.5% (870/1487) v 97.8% (1317/1347). Also, the mean time from diagnosis to death or the end of the study was 6.04 years in patients with COPD but only 1.53 years in patients with lung cancer. Additionally, in Cox models that included a covariate for lung cancer, and that excluded patients with lung cancer, modelled effects of stove improvement were similar to those in the main models (table 4).
There was a long average interval of 12.8 years between reported age at installation of a chimney and the questionnaire interview. This is a source of uncertainty in data analysis. We emphasise, however, that the modelled overall effect would have been beneficial even in the presence of substantial error in reported age at installation. For example, across an error range of -5 years to +5 years (table 4), the modelled relative risk of improvement for overall incidence of COPD would have ranged from 0.50 to 0.65 in men (P < 0.001) and from 0.62 to 0.80 in women (P ≤ 0.025).
COPD risk reduction over time
Risk of COPD was reduced unequivocally about 10 years after installation of a chimney but was higher just after improvement (table 5). The risk of COPD also tends to be higher just after smoking cessation, presumably because some smokers quit only after becoming ill.20-23 Similarly, some Xuanwei residents may have installed chimneys after the onset of respiratory symptoms. Also, it is conceivable that people who sought a physician's advice may have been more likely than others both to be diagnosed with COPD and to install chimneys. If so, people with chimneys could have been more likely to have had a diagnosis of COPD, and the present results could be conservative. In any event, the increase in risk just after improvement remains to be fully explained.
Summary and recommendations
In summary, we found a substantial reduction in the risk of COPD after installation of chimneys on coal stoves in Xuanwei. This has broad implications because unvented burning of coal and biomass fuels is widespread.1 Findings may be especially important regarding biomass burning, which is more common than coal burning, because it is strongly associated with COPD5-13 and because COPD accounts for more DALYs than lung cancer.24 We expect that installation of chimneys would greatly benefit public health, especially in developing countries. These findings should stimulate further stove improvement, research into its health benefits, and introduction of clean burning household fuels.
What is already known on this topic
Chronic obstructive pulmonary disease (COPD) is a major component of the global burden of disease
Coal and biomass fuels are used for household cooking and heating by almost 3 billion people worldwide
Unvented burning of these solid fuels generates high levels of indoor air pollution and is strongly associated with increased risk of COPD and other diseases
What this study adds
In Xuanwei, China, the incidence of COPD decreased substantially after installation of chimneys on formerly unvented coal stoves (and consequent reduction of exposure to coal smoke)
We gratefully acknowledge the contributions of Rudao Yang and Chaofu Huang.
Contributors: XH and QL designed this study, managed data collection, and participated in data processing. RSC participated in data processing, conducted most of the analyses, and was primarily responsible for writing the paper. The analysis incorporated suggestions by AEB, XH, and QL. All authors contributed to draft manuscripts and the final version. RSC is the guarantor.
Funding: Chinese Academy of Preventive Medicine, Beijing, China; Yunnan Province Antiepidemic Station, Kunming, China; US Environmental Protection Agency (contract No 5D2290NFFX); and intramural research programme of the NIH, National Cancer Institute. This report does not necessarily reflect US Environmental Protection Agency policy or Depart-ment of Health and Human Services policy. Mention of commercial products does not constitute endorsement for use.
Competing interests: None declared.
Ethical approval: Institutional review board of the Chinese Academy of Preventive Medicine.
References
- 1.Ezzati M, Kammen DM. The health impacts of exposure to indoor air pollution from solid fuels in developing countries: knowledge, gaps, and data needs. Environ Health Perspect 2002;110: 1057-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ. Selected major risk factors and global and regional burden of disease. Lancet 2002;360: 1347-60. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. World health report: 2002: reducing risks, promoting healthy life. Geneva: WHO; 2002. www.who.int/whr/2002/en (accessed 29 July 2005).
- 4.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: global burden of disease study. Lancet 1997;349: 1498-504. [DOI] [PubMed] [Google Scholar]
- 5.Bruce N, Perez-Padilla R, Albalak R. Indoor air pollution in developing countries: a major environmental and public health challenge. Bull World Health Organ 2000;78: 1078-92. [PMC free article] [PubMed] [Google Scholar]
- 6.Smith KR, Mehta S, Maeusezahl-Feuz M. Indoor air pollution from household use of solid fuels. In: Ezzati M, Lopez AD, Rodgers A, Murray CJL, eds. Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors. Geneva: World Health Organization, 2004: 1435-93.
- 7.Pandey MR. Domestic smoke pollution and chronic bronchitis in a rural community of the hill region of Nepal. Thorax 1984;39: 337-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Malik SK. Exposure to domestic cooking fuels and chronic bronchitis. Indian J Chest Dis Allied Sciences 1985;27: 171-4. [PubMed] [Google Scholar]
- 9.Døssing M, Khan J, al-Rabiah F. Risk factors for chronic obstructive lung disease in Saudi Arabia. Respir Med 1994;88: 519-22. [DOI] [PubMed] [Google Scholar]
- 10.Dennis RJ, Maldonado D, Norman S, Baena E, Martinez G. Woodsmoke exposure and risk for obstructive airways disease among women. Chest 1996;109: 115-9. [DOI] [PubMed] [Google Scholar]
- 11.Perez-Padilla R, Regalado J, Vedal S, Pare P, Chapela R, Sansores R, et al. Exposure to biomass smoke and chronic airway disease in Mexican women. A case-control study. Am J Respir Crit Care Med 1996;154: 701-6. [DOI] [PubMed] [Google Scholar]
- 12.Gupta BN, Mathur N. A study of household environmental risk factors pertaining to respiratory diseases. Energy Environ Monitor 1997;13: 61-7. [Google Scholar]
- 13.Albalak R, Frisancho AR, Keeler GJ. Domestic biomass fuel combustion and chronic bronchitis in two rural Bolivian villages. Thorax 1999;54: 1004-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mumford JL, He XZ, Chapman RS, Cao SR, Harris DB, Li XM, et al. Lung cancer and indoor air pollution in Xuan Wei, China. Science 1987;235: 217-20. [DOI] [PubMed] [Google Scholar]
- 15.Zhou X, Jin Y, He X. [A study on the relationship between indoor air pollution and chronic obstructive pulmonary disease in Xuanwei County]. Zhonghua Yu Fang Yi Xue Za Zhi 1995;29: 38-40 (in Chinese). [PubMed] [Google Scholar]
- 16.Lan Q, Chapman RS, Schreinemachers DM, Tian L, He X. Household stove improvement and risk of lung cancer in Xuanwei, China. J Natl Cancer Inst 2002;94: 826-35. [DOI] [PubMed] [Google Scholar]
- 17.Mumford JL, Chapman RS, Harris DB. Indoor air exposure to coal and wood combustion emissions associated with a high lung cancer rate in Xuan Wei, China. Environ Int 1989;15: 315-20. [Google Scholar]
- 18.Ezzati M, Vander Hoorn S, Rodgers A, Lopez AD, Mathers CD, Murray CJ. Estimates of global and regional potential health gains from reducing multiple major risk factors. Lancet 2003;362: 271-80. [DOI] [PubMed] [Google Scholar]
- 19.Kishi K, Gurney JW, Schroeder DR, Scanlon PD, Swensen SJ, Jett JR. The correlation of emphysema or airway obstruction with the risk of lung cancer: a matched case-controlled study. Eur Respir J 2002;19: 1093-8. [DOI] [PubMed] [Google Scholar]
- 20.Doll R, Peto R. Mortality in relation to smoking: 20 years' observations on male British doctors. BMJ 1976;2: 1525-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.US Department of Health and Human Services. The health benefits of smoking cessation. Rockville, MD: US Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1990. (DHHS Publication No (CDC) 90-8416.)
- 22.Yang G, Ma J, Chen A, Zhang Y, Samet JM, Taylor CE, et al. Smoking cessation in China: findings from the 1996 national prevalence survey. Tob Control 2001;10: 170-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lam TH, He Y, Shi QL, Huang JY, Zhang F, Wan ZH, et al. Smoking, quitting, and mortality in a Chinese cohort of retired men. Ann Epidemiol 2002;12: 316-20. [DOI] [PubMed] [Google Scholar]
- 24.Murray CJ, Lopez AD. Evidence-based health policy—lessons from the global burden of disease study. Science 1996;274: 740-3. [DOI] [PubMed] [Google Scholar]