Abstract
Germination of Bacillus anthracis Sterne and plasmidless Δ-Sterne endospores was dramatically enhanced in RAW264.7 macrophage-like cells, while germination of nonpathogenic Bacillus endospores was not. Elimination of gerS, a germinant receptor locus, caused a complete loss of cell-enhanced germination, implicating gerS in the breaking of endospore dormancy in vivo.
The endospores of Bacillus anthracis ensure its prolonged persistence in the environment and are the infectious particles during anthrax infections. Upon entering the body, endospores are engulfed by regional phagocytes, germinate, and begin a vegetative, often lethal, growth cycle (3, 7, 10, 12, 14, 16). Work with nonpathogenic Bacillus subtilis and Bacillus megaterium endospores indicates that small molecules from the environment specifically bind to germinant receptors, encoded by tricistronic operons and localized to the plasma membrane of the endospore (5). Receptor occupancy results in rapid hydration, breakdown of spore structures, and bacilli outgrowth (5). The chemical germinant profiles vary among Bacillus species. B. anthracis endospores are capable of rapid germination and outgrowth in certain animal and macrophage (Mφ) culture models (2, 9, 12, 16, 21, 22,), but they do not germinate or outgrow effectively in rats (10). In vivo studies indicate that endospores are rapidly (within minutes) associated with regional Mφ, with no obvious involvement of polymorphonuclear cells (9, 16, 24). During inhalation anthrax, endospores germinate while associated with alveolar Mφ traveling en route to regional lymph nodes (9, 10, 12, 16). Since B. anthracis endospores interact with phagocytic cells during early infection, we examined these initial interactions in cultured RAW 264.7 Mφ cultures.
The parental strain of B. anthracis used for this experimentation is Sterne 34F2, containing one of the two virulence plasmids, toxin plasmid pXO1. The strain Δ-Sterne 34F2 is a plasmidless variant of Sterne 34F2, derived by temperature curing pXO1. Construction and growth of B. anthracis ΔgerS strains is described for Δ-Sterne 34F2, and an analogous allelic-exchange procedure was used for the Sterne 34F2 construct (14). B. subtilis and B. megaterium were manipulated and stored according to accepted protocols. B. anthracis endospores were prepared and stored as described elsewhere (14). The murine peritoneal cell line RAW 264.7 (ATCC TIB-71) used in this study maintains most, if not all, markers and functions common to primary Mφ (13). Mφ were grown at 37°C (humidified, 5% CO2) in minimal essential media (MEM; Gibco-BRL) supplemented with 10% (vol/vol) animal sera. Sera used included fetal bovine (Gibco-BRL), equine (HyClone), rabbit, porcine, goat, and rat (Sigma). Mφ were grown to 80% confluence, washed twice with fresh media, recovered by scraping, and suspended in fresh media at a density of 106 Mφ/ml. The degree of endospore germination and germination kinetics calculations were obtained through measurements of release of 45Ca from prelabeled endospores as recently described (14). 45Ca-labeled endospores were mixed at the indicated multiplicities of infection (MOIs) and incubated at room temperature, and the percent germination was scored (14). Endospore uptake measurement was as described in previous studies (2).
The behavior of B. anthracis endospores in a controlled cell culture microenvironment was investigated as a model to study early germination events. First, virtually no germination of B. anthracis endospores occurred in MEM culture medium alone or MEM supplemented with horse, rat, porcine, or rabbit serum. Only limited germination was observed in MEM with fetal bovine serum, while goat serum permitted robust germination of endospores (Table 1). These data are in agreement with findings indicating that serum is not the sole germination factor in susceptible animals, nor the sole reason for animal resistance (10, 18, 23). Second, B. anthracis endospores also rapidly and efficiently associated with RAW 264.7 Mφ-like cells (10, 18, 23). By microscopic visualization and plating assays, >90% of endospores, independent of species or MOI (up to 20:1 endospore/Mφ ratio), were found Mφ associated within 10 min (data not shown).
TABLE 1.
Rate and Extent of B. anthracis Sterne 34F2 germination in MEM with animal sera
| Serum or additivea | Max. germination rate (% germination/min)b,c | Total germination (%)c in 1 h |
|---|---|---|
| BHI | 17.7 ± 4.0 | 99.2 ± 2.3 |
| Water | <0.1 | 2.0 ± 0.3 |
| Rat serum | <0.1 | 4.7 ± 0.5 |
| Horse serum | <0.1 | 5.4 ± 0.5 |
| Rabbit serum | <0.1 | 4.9 ± 0.3 |
| Goat serum | 8.3 ± 1.2 | 89.4 ± 0.9 |
| Fetal bovine serum | 4.0 ± 1.0 | 36.6 ± 1.8 |
| Pig serum | <0.1 | 9.6 ± 0.8 |
All serum or additives are at 10% (vol/vol) with MEM (Gibco-BRL).
Rates marked as <0.1 showed no significant germination in 60 min.
Values reported are the average and one standard deviation for three independent replicates on each of two independent endospore samples.
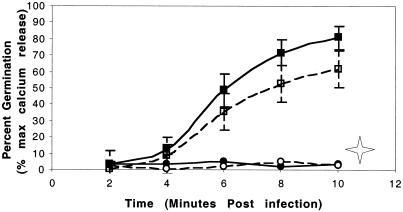
A dramatic increase in germination was seen when anthrax endospores were exposed to Mφ cultures, increasing from nearly 0 to 80% in the presence of Mφ in 10 min (Fig. 1). This increase in germination was independent of input MOI (up to 20:1), of species of animal sera used, or of heat inactivation of sera. Additional requirements for both serum and, to a lesser extent, MEM were also seen, as germination increases were not as robust when either was substituted with phosphate-buffered saline (Table 2). The possibility that endospore uptake by phagocytes could be mimicked by other conditions and cell types was also addressed. Endospores separated physically from Mφ cultures by use of Transwell membranes still germinated (35 to 50% in 1 h), indicating that neither phagocytosis nor direct contact with the Mφ is an absolute requirement for the germination event but that these cells condition the medium to become germination competent, likely by contributing required germinant molecules, perhaps including some known to stimulate through the gerS-dependent pathway in vitro (14). NIH 3T3 fibroblasts were also competent to induce germination (30 to 40% in 1 h), indicating the possibility that non-Mφ cells can also supply germinants. Although germination of B. anthracis endospores in various tissue culture systems remains a formal possibility, all prior work indicates that Mφ are the de facto site for germination within the animal host (3, 7, 9, 12), and direct observations in animal studies are required before assigning a role for other cells in vivo.
FIG. 1.
Germination kinetics for B. anthracis endospores in Mφ cultures. gerS, but not gerX, is required for Mφ-induced germination. Mφ were infected (MOI of 10:1) with B. anthracis strains Sterne (gerS+, gerX+) ▪, Sterne ΔgerS (gerS-deficient, gerX+) •, Δ-Sterne (gerS+, gerX-deficient) □, or Δ-Sterne ΔgerS (gerS and gerX deficient) ○. Germination was monitored by release of 45Ca from prelabeled endospores. Both ΔgerS mutant strains (circles) did not germinate out to 4 h, and only limited germination was seen after 16 h, while the ΔgerX mutant containing wild-type gerS (open squares) was capable of significant Mφ germination. Endospores recovered from Mφ 16 h postinfection (open star symbol) were capable of fully germinating on BHI agar plates, indicating no loss of viability (see text). All cultures were in MEM with 10% (vol/vol) horse serum. The mean of triplicate experiments of each of two endospore preparations with one standard deviation is shown (standard deviations in mutant gerS samples were too small to depict).
TABLE 2.
Role of Mφ, serum, culture medium, and the gerS and gerX loci in B. anthracis germination kinetics
| B. anthracis strain (genotype) | Maximum germination rate (% germination/min)a for germination condition:
|
|||
|---|---|---|---|---|
| + MEM,b + serum, −Mφ | + MEM, − serum, + Mφ | − MEM, + serum, + Mφ | + MEM, + serum, + Mφ | |
| Sterne (gerS+ gerX+) | <0.1 | 0.7 ± 0.2 | 1.4 ± 0.5 | 11.0 ± 2.0 |
| Δ-Sterne (gerS+, gerX deficient) | <0.1 | 0.5 ± 0.3 | 1.2 ± 0.5 | 9.0 ± 1.1 |
| Sterne ΔgerS (gerS deficient, gerX+) | <0.1 | <0.1 | <0.1 | <0.1 |
| Δ-Sterne ΔgerS (gerS and gerX deficient) | <0.1 | <0.1 | <0.1 | <0.1 |
Values reported are the experimental mean, and one standard deviation, for three independent replicates each of two independent endospore samples.
+ or − symbols indicate presence or absence of MEM, 10% (vol/vol) horse serum, and 105 Mφ. Equivalent volumes of phosphate-buffered saline were used to replace the missing ingredient.
We next examined whether the effect of Mφ on germination was unique to B. anthracis, as it was possible that host-associated germination of endospores might be a general response common to many Bacillus species, pathogen and nonpathogen alike. To test this, the nonpathogenic species B. subtilis and B. megaterium were compared to B. anthracis (Table 3). Both B. anthracis and B. subtilis exhibited extremely limited baseline germination in complete culture medium in the absence of Mφ. B. subtilis and B. megaterium endospores showed no increase in germination in the presence of Mφ, even at extended times, while B. anthracis showed a large and rapid increase in germination. The background response of B. megaterium to medium alone is likely due to the proline in MEM, a powerful B. megaterium germinant (5). Therefore, while a limited germination can occur with all three Bacillus species tested, only the pathogen B. anthracis exhibited a rapid host cell-specific response.
TABLE 3.
Germination of B. anthracis, B. subtilis, and B. megaterium in Mφ cell culture
| Bacterial species and strain | % Germination in 30 mina
|
|||
|---|---|---|---|---|
| MEM + horse serumb | Macrophage culturec | Water | BHI | |
| B. anthracis Sterne 34F2 | 2.0 ± 0.3 | 75.0 ± 2.0 | 1.0 ± 0.4 | 100 ± 0.3 |
| B. subtilis BD170 | 7.0 ± 1.0 | 7.0 ± 2.0 | 2.0 ± 1.0 | 95.0 ± 2.0 |
| B. megaterium QMD1551 | 45.0 ± 3.0 | 47.0 ± 4.0 | 3.0 ± 2.0 | 100.0 ± 2.0 |
Values reported are the experimental mean, and one standard deviation, for three independent replicates each of two independent endospore samples.
Horse serum is at 10% (vol/vol).
MEM, 10% (vol/vol) horse serum, and 105 Mφ.
Experiments were conducted to compare the roles of the chromosomal locus gerS to those of the plasmid-encoded gerX locus with respect to the rapid germination seen in Mφ cultures. The gerS locus was recently shown to act as a B. anthracis germinant receptor recognizing aromatic ring-like germinant signals (14). No germinants are yet known to be associated with gerX receptor activity. The ΔgerS mutant was severely attenuated in Mφ germination. Compared to parental cells, ΔgerS mutants were incapable of germination in Mφ (Fig. 1 and Table 2), with a severely limited germination at 16 h (<4% [data not shown]). Endospore strains that did not readily germinate in Mφ did not lose viability after 16 h and were fully able to germinate when removed from cultures and plated on brain heart infusion (BHI) agar plates (Fig. 1). Collectively, these results indicate that gerS is important for cell-associated germination and suggest a role for aromatic amino acids and purines as potential host-supplied germinants (14). In contrast, B. anthracis strains not containing the pXO1-encoded germinant receptor operon gerX (Δ-Sterne strains) showed only a minor defect in Mφ-associated germination extents or rates (Fig. 1 and Table 2). This gerX observation differs with earlier reports by Guidi-Rontani et al. (7-8) in that we found only a slight germination defect in pXO1− (gerX-deficient) strains. Our assay conditions, however, diverge in three important ways from the previous works. First, gentamicin was not used in our assays, as gentamicin has a severe inhibitory effect on the germination and outgrowth of Bacillus endospores, even at low concentrations, and gentamicin can be internalized or concentrated into the phagolysosomes of Mφ (4, 11, 15, 19, 20). Second, all assays were done in the presence of serum, while the earlier work utilized serum-free conditions that we found severely limited endospore uptake and slowed germination rates. Third, our germination assay is based on the release of radioactive calcium ions from prelabeled endospores (14, 17), allowing direct measurement of germination without the need for survival of the newly vegetative bacilli.
Data presented here indicate that the B. anthracis endospore responds dramatically to the microenvironment of eukaryotic cells, reaching >80% germination after as little as 10 min coincubation with Mφ. This is consistent with these phagocytes serving as the relevant site of germination during infections (2-3, 7, 9-10, 12, 16, 18, 22-24). Furthermore, host cell-associated germination was not seen with nonpathogenic Bacillus species, implying that the pathogen B. anthracis has evolved specialized abilities to sense its entry into a host and initiate vegetative growth. These data and previous work also support a model where in vivo germination is controlled by combinations of a number of discrete germinant signals (1) and multiple receptors, including gerS encoded on the chromosome and perhaps, to a lesser degree, the gerX encoded on pXO1 (8). However, since B. anthracis strains (Δ-Sterne) cured of all plasmids also exhibit significant germination in the presence of Mφ (Fig. 1 and Table 2), our data contradict the notion that host-dependent germination is strictly controlled by elements on the virulence plasmid pXO1. Additionally, since defined chemical triggers for the gerS germination locus are also known (14), we hypothesize that these molecules may be utilized as signals for germination in vivo. Work presented here supports a model where rapid and strong germination responses greatly influence the early stages of Mφ-endospore interactions. The combinations of multiple host-supplied germinant molecules, recognized by multiple endospore ger receptors, are likely requirements for a successful infection. Knowledge of the specific germinant molecules and their receptors allows further mechanistic studies of the germination process and for the development of compounds useful for blocking, or stimulating, the germination state of the anthrax endospore.
Acknowledgments
We appreciate the comments of T. Read, M. Weiner, J. Crosno, B. Thomason, S. Cendrowski, and T. Dixon.
This work was supported in part by grants from the National Institutes of Health (AI45740) and the Office of Naval Research (14001-0422, 14011-1044, and 14021-0061).
Editor: J. T. Barbieri
REFERENCES
- 1.Clements, M., and A. Moir. 1998. Role of the gerI operon of Bacillus cereus 569 in the response of spores to germinant. J. Bacteriol. 180:6729-6735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dixon, T., A. Fadl, T. Koehler, J. Swanson, and P. Hanna. 2000. Early Bacillus anthracis-macrophage interactions: intracellular survival and escape. Cell. Microbiol. 2:453-463. [DOI] [PubMed] [Google Scholar]
- 3.Dixon, T. C., M. Meselson, J. Guillemin, and P. C. Hanna. 1999. Anthrax. N. Engl. J. Med. 341:815-826. [DOI] [PubMed] [Google Scholar]
- 4.Drevets, D., B. Canono, P. Leenen, and P. Campbell. 1994. Gentamicin kills intracellular Listeria monocytogenes. Infect. Immun. 62:2222-2228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Foster, S. J., and K. Johnstone. 1990. Pulling the trigger: the mechanism of bacterial spore germination. Mol. Microbiol. 4:137-141. [DOI] [PubMed] [Google Scholar]
- 6.Guerout-Fleury, A., K. Hazand, N. Frandsen, and P. Stragier. 1995. Antibiotic-resistance cassettes for Bacillus subtilis. Gene 167:335-336. [DOI] [PubMed] [Google Scholar]
- 7.Guidi-Rontani, C., M. Levy, H. Ohayon, and M. Mock. 2001. Fate of germinated Bacillus anthracis spores in primary murine macrophages. Mol. Microbiol. 42:931-938. [DOI] [PubMed] [Google Scholar]
- 8.Guidi-Rontani, C., Y. Pereira, S. Ruffie, J. C. Sirard, M. Weber-Levy, and M. Mock. 1999. Identification and characterization of a germination operon on the virulence plasmid pXO1 of Bacillus anthracis. Mol. Microbiol. 33:407-414. [DOI] [PubMed] [Google Scholar]
- 9.Guidi-Rontani, C., M. Weber-Levy, E. Labruyere, and M. Mock. 1999. Germination of Bacillus anthracis spores within alveolar macrophages. Mol. Microbiol. 31:9-17. [DOI] [PubMed] [Google Scholar]
- 10.Hachisuka, Y. 1969. Germination of B. anthracis spores in the peritoneal cavity of rats and establishment of anthrax. Jpn. J. Microbiol. 13:199-207. [DOI] [PubMed] [Google Scholar]
- 11.Hand, W., R. W. Corwin, T. H. Steinberg, and G. D. Grossman. 1984. Uptake of antibiotics by human alveolar macrophages. Am. Rev. Respir. Dis. 129:933-937. [DOI] [PubMed] [Google Scholar]
- 12.Hanna, P., and J. Ireland. 1999. Understanding Bacillus anthracis pathogenesis. Trends Microbiol. 7:180-182. [DOI] [PubMed] [Google Scholar]
- 13.Hanna, P., B. Kruskal, R. Ezekowitz, B. Bloom, and J. Collier. 1994. Role of macrophage oxidative burst in the action of anthrax lethal toxin. Mol. Med. 1:7-18. [PMC free article] [PubMed] [Google Scholar]
- 14.Ireland, J. A. W., and P. C. Hanna. 2002. Amino acid- and purine ribonucleoside-induced germination of Bacillus anthracis Δ-Sterne endospores: gerS mediates responses to aromatic ring structures. J. Bacteriol. 184:1296-1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mayorga, L. S., F. Bertini, and P. Stahl. 1991. Fusion of newly formed phagosomes with endosomes in intact cells and in a cell-free system. J. Biol. Chem. 266:6511-6517. [PubMed] [Google Scholar]
- 16.Ross, J. M. 1957. The pathogenesis of anthrax following the administration of spores by the respiratory route. J. Pathol. Bacteriol. 73:485-494. [Google Scholar]
- 17.Suzuki, J. B., R. Booth, and N. Grecz. 1971. In vivo and in vitro release of 45Ca from spores of Clostridium botulinum type A as further evidence for spore germination. Res. Commun. Chem. Pathol. Pharmacol. 2:16-23. [PubMed] [Google Scholar]
- 18.Titball, R. W., and R. J. Manchee. 1987. Factors affecting the germination of spores of Bacillus anthracis. J. Appl. Bacteriol. 62:269-273. [DOI] [PubMed] [Google Scholar]
- 19.Tochikubo, K., Y. Hayakawa, and K. Kojima. 1981. Mutual relationship between antibiotics and resting spores of Bacillus subtilis: binding of cyclic polypeptide and aminoglycoside antibiotics to spores and their inhibitory effect on outgrowth and vegetative growth. Microbiol. Immunol. 25:113-126. [DOI] [PubMed] [Google Scholar]
- 20.van den Broek, P. J. 1989. Antimicrobial drugs, microorganisms, and phagocytes. Rev. Infect. Dis. 11:213-245. [DOI] [PubMed] [Google Scholar]
- 21.Welkos, S. 1991. Plasmid-associated virulence factors of non-toxigenic (pXO1−) Bacillus anthracis. Microb. Pathog. 10:183-198. [DOI] [PubMed] [Google Scholar]
- 22.Welkos, S., and A. Friedlander. 1988. Pathogenesis and genetic control of resistance to the Sterne strain of Bacillus anthracis. Microb. Pathog. 4:53-69. [DOI] [PubMed] [Google Scholar]
- 23.Welkos, S., S. Little, A. Friedlander, D. Fritz, and P. Fellows. 2001. The role of antibodies to Bacillus anthracis and anthrax toxin components in inhibiting the early stages of infection by anthrax spores. Microbiology 147:1677-1685. [DOI] [PubMed] [Google Scholar]
- 24.Welkos, S. L., R. W. Trotter, D. M. Becker, and G. O. Nelson. 1989. Resistance to the Sterne strain of B. anthracis: phagocytic cell responses of resistant and susceptible mice. Microb. Pathog. 7:15-35. [DOI] [PubMed] [Google Scholar]