Abstract
Objectives
To determine whether a home based exercise programme can improve outcomes in patients with knee pain.
Design
Pragmatic, factorial randomised controlled trial of two years' duration.
Setting
Two general practices in Nottingham.
Participants
786 men and women aged ⩾45 years with self reported knee pain.
Interventions
Participants were randomised to four groups to receive exercise therapy, monthly telephone contact, exercise therapy plus telephone contact, or no intervention. Patients in the no intervention and combined exercise and telephone groups were randomised to receive or not receive a placebo health food tablet.
Main outcome measures
Primary outcome was self reported score for knee pain on the Western Ontario and McMaster universities (WOMAC) osteoarthritis index at two years. Secondary outcomes included knee specific physical function and stiffness (scored on WOMAC index), general physical function (scored on SF-36 questionnaire), psychological outlook (scored on hospital anxiety and depression scale), and isometric muscle strength.
Results
600 (76.3%) participants completed the study. At 24 months, highly significant reductions in knee pain were apparent for the pooled exercise groups compared with the non-exercise groups (mean difference –0.82, 95% confidence interval –1.3 to –0.3). Similar improvements were observed at 6, 12, and 18 months. Regular telephone contact alone did not reduce pain. The reduction in pain was greater the closer patients adhered to the exercise plan.
Conclusions
A simple home based exercise programme can significantly reduce knee pain. The lack of improvement in patients who received only telephone contact suggests that improvements are not just due to psychosocial effects because of contact with the therapist.
What is already known on this topic
Physiotherapy is often prescribed for the treatment of knee pain
Previous trials have usually been short and used intensive supervision and sophisticated equipment
The impact of psychological factors in reducing pain is unclear
What this study adds
Home based programmes involving exercise for up to 30 minutes a day significantly reduce self reported knee pain
Social support alone does not improve health outcomes
Reductions in pain are greater for patients the closer they adhere to exercise programmes
Introduction
Knee osteoarthritis contributes greatly to disability in the general population, particularly in the elderly.1,2 Pain is the principal feature of knee osteoarthritis, but it is well recognised that severity of pain equates poorly with radiographic and structural change.3,4 Drug treatments aimed at relieving pain are often limited by side effects. Physiotherapy is often recommended, although until recently relatively few studies confirmed its efficacy. Most successful physiotherapy approaches incorporate exercises to strengthen quadriceps. Many of these programmes, however, have employed intensive supervision and sophisticated equipment.5,6 Since knee osteoarthritis is a considerable public health issue, a less expensive community based approach would be desirable. Previous studies have focused on radiographically defined knee osteoarthritis rather than knee pain.7,8 In the early stages of disease, when exercise intervention may be most appropriate, however, radiographs may be normal. We have shown previously that a simple six month exercise programme can reduce knee pain.9 This study assessed relatively short term outcomes, however, and it did not control for social contact from the therapist, which may itself have a positive effect on pain reporting.10
We aimed to assess whether a home based exercise programme lasting two years could reduce knee pain and improve physical function in people with knee pain. We also aimed to determine the relative contribution of contact with a therapist in explaining these health outcomes.
Methods
Participants
A postal survey was sent to 9296 patients aged 45 and over registered at two general practices in Nottingham. Patients were defined as having knee pain if they responded “yes” to both of the following questions: “Have you ever had pain in or around the knee on most days for at least a month?” and “If so, have you experienced any pain during the last year?”11 Participants with knee pain were invited to an initial assessment. The following exclusion criteria were applied: total knee replacement, lower limb amputation, permanent cardiac pacemaker, unable to give informed consent, and no knee pain within the last week.
The protocol was approved by local hospital research ethics committees, and all participants provided written informed consent.
Interventions
The two year exercise programme was simple to use and applicable for all age groups. It was designed to maintain and improve the strength of muscles acting around the knee, the range of motion at the knee joint, and locomotor function. The programme was self paced but became progressively more challenging. Graded elastic bands were used to increase the resistance against which the muscles worked. The programme was taught in the participants' homes by a trained researcher. The initial training phase consisted of four visits lasting approximately 30 minutes in the first two months, with follow up visits scheduled at six monthly intervals. Participants were encouraged to perform the programme with both legs for 20-30 minutes a day. They were instructed to increase the number of repetitions up to a maximum of 20 per leg. Adherence was assessed by means of self completed diaries, which were collected every six months.
Telephone contact consisted of monthly calls all made by the same researcher. The principal aim of the calls was to monitor symptoms and to offer simple advice on the management of knee pain. This intervention provided a control for the psychosocial contact inherent in delivery of the exercise programme. For those participants who received telephone contact and exercise therapy, discussion of the exercise programme was discouraged and specific problems were referred back to the therapist responsible for teaching the programme. Calls typically lasted about two minutes.
Participants in the control group (no intervention) received no contact between assessment visits.
Outcome measures
The primary outcome measure was self reported knee pain at two years. This was measured using the knee specific questionnaire of the Western Ontario and McMaster universities (WOMAC) osteoarthritis index. This has three domains: pain, stiffness, and physical function.12 The pain domain produces a score of 0-20, with higher scores indicating more pain.
Secondary measures consisted of change in knee specific stiffness (0-8) and disability (0-68) (WOMAC), general physical function (anglicised SF-36),13 psychological score (hospital anxiety and depression scale),14 and isometric quadriceps muscle strength (measured with a modified Tornvall chair in participants from one practice).15 Economic data were also collected and will be reported separately.
Radiographic osteoarthritis was defined by the presence of definite osteophyte in either compartment of at least one knee, as determined with a standard atlas.16
Randomisation and blinding
Participants were randomised with a factorial design based around the two main factors for evaluation—exercise and contact with a therapist. They were allocated to one of four groups: exercise therapy, monthly telephone contact, exercise therapy plus telephone contact, or no intervention. As this was a long term study, we were concerned that some patients in the no intervention control group would lack motivation to remain in the study. As a result, participants allocated to the no intervention and combined exercise and telephone groups were further randomised to receive or not receive a placebo tablet (dolomite) twice a week. Dolomite is a health food product containing calcium and magnesium and is normally taken at a dose of three tablets per day. Even at its full dose, no benefit in arthritis has been proved.
Randomisation was achieved by means of computer generated lists in permuted blocks of 10, stratified by sex and age. As participants were enrolled in the study, the study administrator added them to the list in sequential order. More participants were randomised to the groups involving exercise to allow for a predicted high dropout rate in these groups. Participants were assessed every six months for two years. The assessor was blinded to the intervention group and was the same for each assessment.
Statistical analysis
We aimed to recruit 800 participants—the number calculated to detect a 20% change in the primary outcome measure with greater than 90% power at the 5% significance level. Analysis was performed on an intention to treat basis, with data carried forward from the last available assessment unless values were missing at the first assessment.
All analyses were performed with SPSS version 9.0.0. We used a factorial analysis of variance model to assess changes in self reported knee pain at two years and number needed to treat to assess the clinical significance of these findings.17,18 A clinically significant improvement was defined as a reduction in pain ⩾50%. As number needed to treat is known to be highly sensitive to baseline values, the odds ratio is also presented.
Results
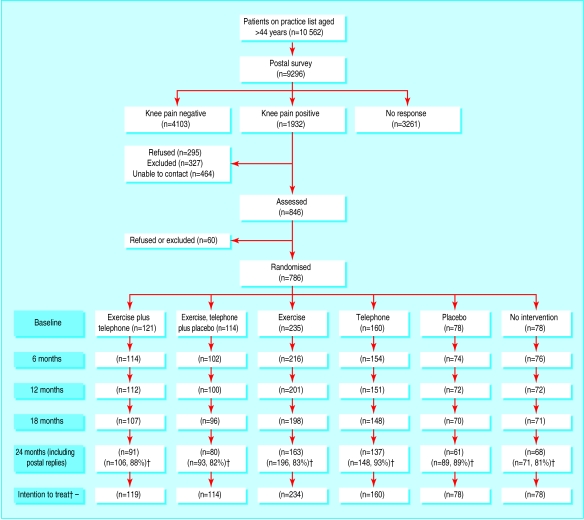
In total, 786 participants were recruited between January 1996 and January 1997. Follow up was completed in January 1999. Recruitment and progress through the study are summarised in the figure. Characteristics and baseline measures are shown in table 1; no statistically significant differences were seen between the groups.
Table 1.
Characteristics of treatment groups
| Characteristic
|
Exercise and telephone
|
Exercise, telephone, and dolomite
|
Exercise
|
Telephone
|
Dolomite
|
No intervention
|
|---|---|---|---|---|---|---|
| No of participants | 121 | 114 | 235 | 160 | 78 | 78 |
| Mean (SD) age | 62.6 (9.36) | 62.5 (8.86) | 61.5 (9.58) | 61.5 (9.02) | 61.9 (9.84) | 61.9 (9.39) |
| Mean (SD) body mass index | 27.58 (3.93) | 28.19 (4.76) | 28.02 (4.18) | 28.24 (4.93) | 27.87 (5.53) | 28.14 (4.81) |
| Mean (SD) WOMAC pain score | 6.96 (3.54) | 7.82 (3.61) | 6.93 (3.55) | 7.43 (3.48) | 7.49 (3.63) | 7.04 (3.67) |
| Mean (SD) strength of left quadriceps | 204.61 (133.22) (n=74) |
207.62 (109.96) (n=64) |
218.16 (117.96) (n=141) |
221.24 (127.14) (n=94) |
213.46 (117.99) (n=45) |
205.31 (99.96) (n=49) |
| Sex ratio (male:female) | 39:61 | 38:62 | 36:64 | 34:66 | 35:65 | 35:65 |
| No (%) with bilateral pain | 89 (74) | 79 (69) | 161 (69) | 102 (64) | 50 (64) | 48 (62) |
| No (%) with radiograph showing definite osteophyte present | 61/112 (54) | 42/100 (42) | 87/206 (42) | 78/139 (56) | 29/71 (41) | 33/72 (46) |
Overall, 600 (76.3%) participants completed the study and returned for final assessment at 24 months (figure). A further 83 (10.6%) participants who withdrew from the interventions completed a postal questionnaire at 24 months. These participants were more likely to be aged over 75, have higher baseline pain scores, and be randomised to one of the groups involving exercise.
Factorial analysis
No significant differences were found between the groups that did and did not receive the placebo intervention (no intervention v placebo, P=0.66; exercise plus telephone v exercise, telephone, and placebo, P=0.94). These subgroups were therefore merged, and the analysis performed on the original four groups. The validity of this decision was tested with a sensitivity analysis.
Primary outcome
At 24 months, the exercise groups differed significantly from the non-exercise groups (table 2). Similar improvements were not observed for the telephone groups compared with the non-telephone groups or for the interaction of the exercise and telephone groups.
Table 2.
Change in WOMAC pain scores at 6, 12, 18 and 24 months† and knee related physical function and stiffness at 24 months
| Outcome
|
No of participants
|
Baseline
|
Mean difference at 24 months†
|
95% confidence interval for mean difference
|
df
|
F
|
P
|
Effect size
|
|---|---|---|---|---|---|---|---|---|
| Primary | ||||||||
| Knee pain at 24 months*: | ||||||||
| Exercise | 467 | 7.15 | −0.82 | −1.3 to −0.3 | 1 and 779 | 11.14 | 0.001 | 0.25 |
| Non-exercise | 316 | 7.35 | ||||||
| Telephone | 393 | 7.10 | −0.16 | −0.6 to 0.3 | 1 and 779 | 0.45 | 0.50 | 0.05 |
| Non-telephone | 390 | 7.40 | ||||||
| Knee pain at 6 months: | ||||||||
| Exercise | 467 | 7.15 | −0.61 | −1.0 to −0.2 | 1 and 779 | 8.64 | 0.003 | 0.21 |
| Non-exercise | 316 | 7.35 | ||||||
| Knee pain at 12 months: | ||||||||
| Exercise | 467 | 7.15 | −0.61 | −1.0 to −0.2 | 1 and 779 | 7.80 | 0.005 | 0.20 |
| Non-exercise | 316 | 7.35 | ||||||
| Knee pain at 18 months: | ||||||||
| Exercise | 467 | 7.15 | −0.69 | −1.1 to −0.2 | 1 and 779 | 9.10 | 0.003 | 0.22 |
| Non-exercise | 316 | 7.35 | ||||||
| Secondary | ||||||||
| Physical function: | ||||||||
| Exercise | 466 | 23.15 | −2.57 | −4.1 to −1.1 | 1 and 778 | 11.44 | 0.001 | 0.25 |
| Non-exercise | 316 | 22.97 | ||||||
| Stiffness: | ||||||||
| Exercise | 470 | 3.42 | −0.29 | −0.5 to −0.1 | 1 and 782 | 6.44 | 0.01 | 0.18 |
| Non-exercise | 316 | 3.46 | ||||||
Interaction of exercise and telephone (P=0.54).
Negative values for mean differences reflect improvements in knee symptoms compared with baseline.
Sensitivity analysis excluding those patients who received the placebo tablet did not change our conclusions. Mean differences were –1.12 (95% confidence interval –1.71 to –0.54) for exercise versus non-exercise and –0.44 (–1.02 to 0.13) for telephone versus non-telephone.
On the basis of a the comparison of the exercise group with the non-exercise group, the number needed to treat to achieve a >50% improvement in knee pain in 13.0 (6 to 20). This equates to an odds ratio of 1.5.
Exercise was consistently better at reducing pain at 6, 12, and 18 months than no exercise (table 2). A significant interaction was observed between exercise and telephone contact at 6 months (P=0.001). This effect was not observed at any of the other time points. As exercise was associated with an improvement in the telephone and non-telephone groups, we decided to present results of the main effect rather than the simple main effects (table 2). Our interpretation is that this interaction occurred by chance.
Secondary outcomes
At two years, 226 (48.1%) of those allocated to receive exercise therapy completed the programme. The most common reasons for failing to adhere to the programme were related to health problems (back and hip pain) and lack of time. Fifty two (11%) of those exercising reported side effects, but these were generally minor (for example, the exercise band was painful around their ankle). Self reported adherence to the exercise programme was crudely graded as high (n=128), medium (n=32), or low (n=307). The impact of exercise adherence on self reported pain at 24 months suggested a dose-response effect, with effect sizes of 0.42, 0.34, and 0.16 for the three grades of adherence, respectively.
Scores for stiffness and physical function on the WOMAC index both showed significant improvements for the exercise groups compared with the non-exercise groups (table 2). Isometric muscle strength was higher in the exercise groups than in the non-exercise groups (mean difference 18.4 N (95% confidence interval 7.0 to 29.8); P=0.002), but general physical function (indicated by score on the SF-36), anxiety, and depression at 24 months were not significantly altered by any of the study interventions (data not shown).
Discussion
This study shows that simple home based exercise therapy over two years can produce small but significant reductions in knee pain. Improvements in pain were achieved by six months and sustained throughout the study period; this suggests that follow up at six monthly intervals may be enough to ensure adherence to exercise programmes. Compared with the non-exercise groups, groups that performed exercise had an average reduction in knee pain of 12%. This effect was incremental to benefits resulting from normal care and is of some clinical relevance. In addition to improvements in pain, the exercise programme also produced significant improvements in knee stiffness and physical function.
The exercise programme was generally well tolerated, although adherence was moderate. The introduction of telephone support contributed little to observed reductions in knee pain. It is reasonable to attribute the beneficial effects primarily to the exercise intervention rather than to secondary effects because of improved psychosocial contact.
Comparison with other studies
That this was a pragmatic study is important when comparing it with other studies. In addition to using an intention to treat analysis, we used a practical intervention that involved limited input from health professionals, a long period of follow up, and entry criteria based upon knee pain rather than radiographic status. We anticipated that these factors would improve the generalisability of our study findings, but that effect sizes would be smaller than those reported by other exploratory trials. For example, a large study comparing exercise therapy with education reported effect sizes of 0.3-0.6 for pain and function.7 It was based in primary care, it involved contact with a physiotherapist one to three times per week, and outcomes were assessed after 12 weeks. Follow up data show that these improvements were not sustained at nine months.19
A more comparable 18 month study compared aerobic exercise and resistance exercise with an education programme.20 This study reported 12% and 8% reductions in pain and effect sizes of 0.5 and 0.3 in the aerobic and resistance exercise groups, respectively. Again this involved an element of supervised therapy, and patients were included on the basis of both radiographic evidence of osteoarthritis and difficulty with activities of daily living, in addition to self reported knee pain.
Limitations
Despite a highly significant difference between the exercise and non-exercise groups, some patients may consider the effect (a reduction in pain of 12%) to be too small to be worth the effort of half an hour of daily exercise for two years. Future work should focus on establishing which patients are likely to benefit most from an intervention of this kind.
Adherence to treatment may be higher in a trial setting than in routine clinical practice. Nevertheless, participants for this study were approached directly in the community rather than through general practices. Patients who contact their general practitioner may be more inclined to adhere to a treatment programme.
More importantly, patients with pain referred from sites such as the back or hips may have been included in this study on the basis of self reported knee pain. Such individuals are unlikely to benefit from the study interventions. Nevertheless, 740 (94.5%) of the participants had signs suggesting pain originating in the knee (localised pain and tenderness or pain on movement, or both) rather than referred pain (diffuse pain involving the thighs with no pain on knee movement).
Conclusion
Simple home based exercise programmes can produce significant reductions in knee pain over two years. Such programmes are ideally suited for primary care.
Figure.
Progress of participants through the trial. †Includes participants who dropped out but still returned the final questionnaire. ‡Data were missing for three participants at baseline; they were not included in the intention to treat analysis at 24 months
Acknowledgments
We thank Cliniband and Dynaband for providing the exercise bands and Sarah Pacey, senior pharmacist, Nottingham City Hospital, for organising supplies of dolomite tablets. We are indebted to the doctors and staff of Torkard Medical Centre, Hucknall, and Arnold Health Centre. We are particularly grateful to the patients who took part in the study.
Footnotes
Funding: Department of Health.
Competing interests: None declared.
References
- 1.Felson DT, Naimark A, Anderson JJ, Kazis L, Castelli W, Meenan RF. The prevalence of knee osteoarthritis in the elderly: the Framingham osteoarthritis study. Arthritis Rheum. 1987;30:914–918. doi: 10.1002/art.1780300811. [DOI] [PubMed] [Google Scholar]
- 2.Badley EM, Tennant A. Disablement associated with rheumatic disorders in a British population: problems with activities of daily living and level of support. Br J Rheumatol. 1993;32:601–608. doi: 10.1093/rheumatology/32.7.601. [DOI] [PubMed] [Google Scholar]
- 3.Lawrence JS, Bremner JM, Bier F. Osteoarthrosis. Prevalence in the population and relationship between symptoms and X-ray changes. Ann Rheum Dis. 1966;25:1–23. [PMC free article] [PubMed] [Google Scholar]
- 4.Davis MA, Ettinger WH, Neuhaus JM, Barclay JD, Segal MR. Correlates of knee pain among US adults with and without radiographic knee osteoarthritis. J Rheumatol. 1992;19:1943–1949. [PubMed] [Google Scholar]
- 5.Fisher NM, Prendergast DR, Gresham GE, Calkins E. Muscle rehabilitation: its effect on muscular and functional performance of patients with knee osteoarthritis. Arch Phys Med Rehabil. 1991;72:367–374. [PubMed] [Google Scholar]
- 6.Deyle GD, Henderson NE, Matekel MP, Ryder MG, Garber MB, Allison SC. Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee. A randomized, controlled trial. Ann Intern Med. 2000;132:173–181. doi: 10.7326/0003-4819-132-3-200002010-00002. [DOI] [PubMed] [Google Scholar]
- 7.Van Barr ME, Dekker J, Oostendorp RA, Bijl D, Voorn TB, Lemmens JA. The effectiveness of exercise therapy in patients with osteoarthritis of hip or knee: a randomised clinical trial. J Rheumatol. 1998;25:2432–2439. [PubMed] [Google Scholar]
- 8.Maurer BT, Stern AG, Kinossian B, Cook KD, Schumacher HR. Osteoarthritis of the knee: isokinetic quadriceps exercise versus an educational intervention. Arch Phys Med Rehabil. 1999;80:1293–1299. doi: 10.1016/s0003-9993(99)90032-1. [DOI] [PubMed] [Google Scholar]
- 9.O'Reilly SC, Muir KR, Doherty M. The effectiveness of home exercise on pain and disability from osteoarthritis of the knee: a randomised controlled trial. Ann Rheum Dis. 1999;58:15–19. doi: 10.1136/ard.58.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weinberger M, Tierney WM, Booher P, Katz BP. Can the provision of information to patients with osteoarthritis improve functional status? A randomized, controlled trial. Arthritis Rheum. 1989;32:1577–1583. doi: 10.1002/anr.1780321212. [DOI] [PubMed] [Google Scholar]
- 11.O'Reilly SC, Muir KR, Doherty M. Screening for knee pain in osteoarthritis: which question? Ann Rheum Dis. 1996;55:931–933. doi: 10.1136/ard.55.12.931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J. Validation study of WOMAC: a health status instrument for measuring clinically-important patient-relevant outcomes following total hip or knee arthroplasty in osteoarthritis. J Ortho Rheumatol. 1988;1:95–108. [PubMed] [Google Scholar]
- 13.Brazier JE, Harper R, Jones NM, O'Cathain A, Thomas KJ, Usherwood T, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992;305:160–165. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 15.Tornvall G. Assessment of physical capabilities with special reference to the evaluation of maximum voluntary isometric muscle strength. Acta Physiol Scand. 1963;58(suppl 201):1–102. [Google Scholar]
- 16.Altman RD, Hochberg MC, Murphy WA, Wolfe F. Atlas of individual radiographic features in osteoarthritis. Osteoarthritis Cart. 1995;3(suppl A):3–70. [PubMed] [Google Scholar]
- 17.Altman DG. Confidence intervals for the number needed to treat. BMJ. 1998;317:1309–1312. doi: 10.1136/bmj.317.7168.1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cook RJ, Sackett DL. The number needed to treat: a clinically useful measure of treatment effect. BMJ. 1995;310:452–454. doi: 10.1136/bmj.310.6977.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Baar ME, Dekker J, Oostendorp RA, Bijl D, Voom TB, Bijlsma JW, et al. Effectiveness of exercise in patients with osteoarthritis of hip or knee: nine months' follow up. Ann Rheum Dis. 2001;60:1123–1130. doi: 10.1136/ard.60.12.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ettinger WH, Burns R, Messier SP, Applegate W, Rejeski WR, Morgan T, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. JAMA. 1997;277:25–31. [PubMed] [Google Scholar]